Abstract
EMBO J 32: 2920–2937 ; DOI: 10.1038/emboj.2013.207; published online September 24 2013
Microtubule loss from axons and dendrites is a key contributor to nervous system degeneration during Alzheimer disease. Previous evidence suggested a simple pathway by which tau dissociation from microtubules in the axon allows excess severing of microtubules by katanin. Now, new evidence has emerged for a more complex pathway by which abnormal tau invasion into dendrites, triggered by Aβ oligomers, results in excess severing of microtubules by spastin.
Alzheimer disease (AD) is a member of a category of neurodegenerative disorders called tauopathies (Wang and Liu, 2008). These are diseases of the nervous system in which tau becomes abnormally phosphorylated, and thereby detaches from microtubules. As the microtubules lose tau, they diminish in number and density, and this loss of microtubule mass negatively impacts the capacity of the neuron to maintain axonal transport and synaptic connections. Terms such as disintegrate or ‘fall apart’ are often used to describe the effect on the microtubules as they lose tau, but to date there has been very little information on how this happens. There is no mechanistic evidence to support the view that the microtubules become less stable and simply disassemble by their normal dynamic properties.
One possibility is that tau normally protects microtubules from being destroyed by various proteins in the axon that would otherwise cut them into pieces or in some other way break them down. This presumably reflects a physiological mechanism wherein the regulation of tau dissociation from the microtubule via signalling pathways controls when and where microtubule breakage normally occurs. When a pathological condition causes tau to detach from microtubules, they become extremely sensitive to such factors. In addition, there is strong evidence that the abnormal tau, whether soluble or filamentous, can elicit toxic gain-of-function effects on the axon (Wang and Liu, 2008).
To make matters even more complex, AD is not a pure tauopathy. Beta amyloid (Aβ) accumulates abnormally in the brain during AD, and this prompts tau to become hyperphosphorylated and lose association with microtubules. However, the Aβ can also elicit microtubule loss, independent of tau dissociation from the microtubules. In AD, there is also a loss of microtubules from dendrites, and this introduces an additional degree of complexity. Tau is normally less enriched in dendrites than axons. In AD, tau invades dendrites abnormally through deregulation of its normal sorting mechanism, and this somehow leads to microtubule loss from dendrites (Zempel et al, 2010).
Microtubule loss is a common end point of multiple pathways, some involving loss of tau function, others involving gain-of-function effects of abnormal tau, and still others working through tau-dependent Aβ toxicity. All of this is not to say that the effects on microtubules are the only reason or even the principal explanation for axonal degeneration in AD, but the loss of microtubules is an important contributor to nervous system degeneration. Preventing or reversing the effects on microtubules could help stave off degeneration and hence provide patients with additional years of cognitive health and better quality of life.
Microtubule assembly and disassembly occur from the ends of a microtubule, mainly (and often exclusively) at the plus end of the microtubule in living cells. Proteins that regulate microtubule stability affect the rate of these dynamics at microtubule ends. In recent years, a great deal of attention has focused on a category of proteins, termed microtubule-severing proteins. These proteins are enzymes that yank at the microtubule anywhere along its length to pull out a tubulin subunit, and thereby ‘cut’ the microtubule by causing it to break into pieces (Roll-Mecak and Vale, 2008). If the microtubule is sufficiently stable in the region of the break, the parent microtubule is cut into two shorter microtubules that persist, with minimal disassembly of either of the two pieces. If a microtubule is severed in its more labile region, the breakage could cause a great deal of disassembly. If the tubulin being yanked is situated at one of the ends of a microtubule, the result would be a shortening of the microtubule from that end; that is, disassembly. Thus, microtubule severing in the axon can certainly lead to microtubule loss, either by cutting the polymer all the way to subunits, inducing disassembly directly from microtubule ends or promoting disassembly as a secondary effect to the cutting.
To date, the AAA enzymes katanin and spastin are the best studied of the microtubule-severing proteins (Yu et al, 2008). Spastin was originally identified as the product of the gene whose mutations are the chief cause of hereditary spastic paraplegia. Curiously, neurons express levels of spastin and katanin that are theoretically high enough to completely sever all of the microtubules in the neuron to subunits (Solowska et al, 2008), and yet this does not happen. Various regulatory mechanisms presumably keep the activities of the severing proteins in check. One of these mechanisms, in the case of katanin, is microtubule-bound tau, which protects the microtubule from being accessed by katanin (Qiang et al, 2006).
Could microtubule loss in AD be due, at least in part, to excess microtubule severing due to deregulation of microtubule-severing proteins? We have posited that heightened severing of the microtubules by katanin, as the microtubules lose association with tau, is a contributing factor to the degradation of microtubules in the axons of AD patients (Sudo and Baas, 2011). A role for spastin in this pathway is questionable, because tau does not appear to protect microtubules against spastin as effectively as it does against katanin (Qiang et al, 2006). However, we now know that spastin is far from irrelevant to AD, as an exciting new article from the Mandelkow and Dawson laboratories implicates spastin in an entirely different pathway for microtubule loss in AD (Zempel et al, 2013). Whereas the katanin pathway is more relevant to axons, this new spastin pathway is more relevant to dendrites.
In this new work, Zempel et al (2013) exposed mature primary neurons to oligomers of Aβ and observed microtubule breakdown in dendrites that had been invaded by tau. They found that the missorting of tau leads to an elevation of TTLL6 (Tubulin-Tyrosine-Ligase-Like-6) in dendrites, and this results in a marked increase in the polyglutamylation status of the microtubules. Because spastin has a strong preference for polyglutamylated microtubules, the microtubules become more sensitive to spastin-induced severing. Exactly why katanin is not a factor remains unclear, as polyglutamylation renders microtubules more sensitive to both of the severing proteins, not just spastin (Lacroix et al, 2010). Perhaps some of the tau that invades the dendrite is able to bind to microtubules and protect them from katanin, or perhaps katanin is less potent in dendrites because their microtubules are poorly acetylated, as katanin prefers acetylated microtubules to unacetylated ones (Sudo and Baas, 2011). Whatever the case, these new studies suggest that spastin, a protein whose mutations cause an entirely different neurodegenerative disease, is also a major factor in AD.
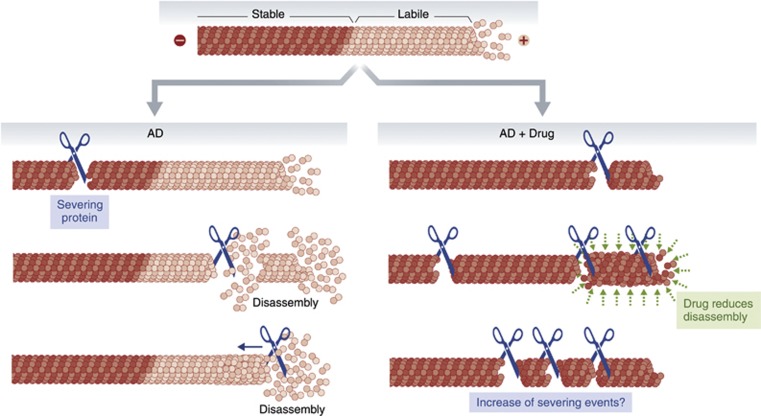
What are the implications of these findings for AD treatment? In recent years, there have been encouraging results on rodent models for AD, in which behavioural improvement and enhanced neuronal vitality were observed when the animals were treated with drugs that stabilize microtubules against disassembly (Zhang et al, 2012). Such drugs are currently in clinical trials for AD (Barten et al, 2012). This strategy is based on the presumption that the microtubule loss that occurs in AD is due to destabilization of the microtubules. However, the results discussed here suggest that the primary cause of the microtubule loss could be something quite different, namely excess severing of microtubules. In this regard, it is relevant that both katanin and spastin seem to have a preference for severing stable microtubules (Lacroix et al, 2010; Sudo and Baas, 2011). Therefore, while treatment with a microtubule-stabilizing drug would mitigate disassembly that occurs as an aftereffect of microtubule severing, the severing events themselves would likely be increased (Figure 1). Heightened microtubule severing in axons and dendrites, even if the total levels of microtubule mass are preserved, could result in a gradual shift from a normal distribution of long and short microtubules to a predominance of microtubules too short to support sustained excursions of organelle transport. Long microtubules are also necessary as compression-bearing struts that prevent axons and dendrites from collapsing on themselves. We suspect that appropriate treatment regimes can be devised to prevent such dire consequences from happening, but we would advocate for the development of new drugs that inhibit microtubule-severing proteins. Such drugs may prove to be a better approach (on their own or in combination with a stabilizing drug) for preserving the fidelity of axonal and dendritic microtubules in AD patients. Given that the structure of the severing proteins is known, it may be straightforward to develop inhibitors, especially to their ATPase domains.
Figure 1.
Microtubules in axons and dendrites consist of a stable region towards the minus end of the microtubule and a labile region towards the plus end, as well as a pool of free tubulin subunits. Microtubule severing is a normal event in the neuron, when tightly regulated. Abnormal (deregulated) microtubule severing is posited to account for microtubule loss in AD. Severing in the stable region of the microtubule would create two new microtubules, with fairly minimal disassembly of either one. Severing in the labile region of the microtubule would result in notably more disassembly. Severing at the end of the microtubule would result in disassembly. Because known microtubule-severing proteins favour the stable region of the microtubule, treatment of AD with a microtubule-stabilizing drug may mitigate disassembly that occurs as an aftereffect of the severing, but the severing events themselves would likely increase.
Footnotes
The authors declare that they have no conflict of interest.
References
- Barten DM, Fanara P, Andorfer C, Hoque N, Wong PY, Husted KH, Cadelina GW, Decarr LB, Yang L, Liu V, Fessler C, Protassio J, Riff T, Turner H, Janus CG, Sankaranarayanan S, Polson C, Meredith JE, Gray G, Hanna A et al. (2012) Hyperdynamic microtubules, cognitive deficits, and pathology are improved in tau transgenic mice with low doses of the microtubule-stabilizing agent BMS-241027. J Neurosci 32: 7137–7145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacroix B, van Dijk J, Gold ND, Guizetti J, Aldrian-Herrada G, Rogowski K, Gerlich DW, Janke. C (2010) Tubulin polyglutamylation stimulates spastin-mediated microtubule severing. J Cell Biol 189: 945–954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiang L, Yu W, Andreadis A, Luo M, Baas PW (2006) Tau protects microtubules in the axon from severing by katanin. J Neurosci 26: 3120–3129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roll-Mecak A, Vale RD (2008) Structural basis of microtubule severing by the hereditary spastic paraplegia protein spastin. Nature 451: 363–367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solowska JM, Morfini G, Falnikar A, Himes BT, Brady ST, Huang D, Baas PW (2008) Quantitative and functional analyses of spastin in the nervous system: implications for hereditary spastic paraplegia. J Neurosci 28: 2147–2157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudo H, Baas PW (2011) Strategies for diminishing katanin-based loss of microtubules in tauopathic neurodegenerative diseases. Human Molec Genetics 20: 763–778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu W, Qiang L, Solowska JM, Karabay A, Korulu S, Baas PW (2008) The microtubule-severing proteins spastin and katanin participate differently in the formation of axonal branches. Mol Biol Cell 19: 1485–1498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang JZ, Liu F (2008) Microtubule-associated protein tau in development, degeneration and protection of neurons. Prog Neurobiol 85: 148–175 [DOI] [PubMed] [Google Scholar]
- Zempel H, Thies E, Mandelkow E, Mandelkow EM (2010) Abeta oligomers cause localized Ca(2+) elevation, missorting of endogenous Tau into dendrites, Tau phosphorylation, and destruction of microtubules and spines. J Neurosci 30: 11938–11950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zempel H, Luedtke J, Kumar Y, Biernat J, Dawson H, Mandelkow E, Mandelkow E-M (2013) Amyloid-β oligomers induce synaptic damage via Tau-dependent microtubule severing by TTLL6 and spastin. EMBO J 32: 2920–2937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang B, Carroll J, Trojanowski JQ, Yao Y, Iba M, Potuzak JS, Hogan AM, Xie SX, Ballatore C, Smith AB 3rd, Lee VM, Brunden KR (2012) The microtubule-stabilizing agent, epothilone D, reduces axonal dysfunction, neurotoxicity, cognitive deficits, and Alzheimer-like pathology in an interventional study with aged tau transgenic mice. J Neurosci 32: 3601–3611 [DOI] [PMC free article] [PubMed] [Google Scholar]