Abstract
Context
Although pressure ulcers may negatively influence quality of life (QoL) post-spinal cord injury (SCI), our understanding of how to assess their impact is confounded by conceptual and measurement issues. To ensure that descriptions of pressure ulcer impact are appropriately characterized, measures should be selected according to the domains that they evaluate and the population and pathologies for which they are designed.
Objective
To conduct a systematic literature review to identify and classify outcome measures used to assess the impact of pressure ulcers on QoL after SCI.
Methods
Electronic databases (Medline/PubMed, CINAHL, and PsycInfo) were searched for studies published between 1975 and 2011. Identified outcome measures were classified as being either subjective or objective using a QoL model.
Results
Fourteen studies were identified. The majority of tools identified in these studies did not have psychometric evidence supporting their use in the SCI population with the exception of two objective measures, the Short-Form 36 and the Craig Handicap Assessment and Reporting Technique, and two subjective measures, the Life Situation Questionnaire-Revised and the Ferrans and Powers Quality of Life Index SCI-Version.
Conclusion
Many QoL outcome tools showed promise in being sensitive to the presence of pressure ulcers, but few of them have been validated for use with SCI. Prospective studies should employ more rigorous methods for collecting data on pressure ulcer severity and location to improve the quality of findings with regard to their impact on QoL. The Cardiff Wound Impact Schedule is a potential tool for assessing impact of pressure ulcers-post SCI.
Keywords: Spinal cord injuries, Quality of life, Pressure ulcers, Outcome assessment, Cardiff wound impact schedule
Introduction
Pressure ulcers are a frequently reported secondary health condition following spinal cord injury (SCI),1 with an estimated annual prevalence rate of approximately 30%.2 A pressure ulcer is a soft tissue lesion that typically results from pressure, friction, or shear forces. The most common places for these lesions occur over bony prominences, such as the sacrum, greater trochanters (hips), ankles, and heels. People with SCI have lifelong increased risk of pressure ulcers due to impaired skin sensation, reduced mobility, and other factors such as spasticity and incontinence.3 This devastating secondary health condition may affect 95% of persons with SCI over the course of their lifetime.4 Less severe ulcers (Stages I and II) comprise about 75% of those observed, while more severe ulcers (Stages III and IV) have a prevalence of about 25%.5 Although preventable, the consequences of having a pressure ulcer can be grave and, in rare cases, result in death.6
Pressure ulcers have been estimated to account for approximately one-fourth of the cost of care post-SCI, but the most important impact is their potential to interfere in a number of physical, psychological, and social domains, which subsequently affect quality of life (QoL).7 Recurring and/or severe pressure ulcers might disrupt the rehabilitation process, prevent individuals with SCI from working or attending school, and interfere with community reintegration and participation.8 One study9 reported that prescribed bed rest, a common practice to foster pressure ulcer healing, prevented individuals with SCI from participating in rehabilitation for 5–32, 12–120, and 26–282 days for Stages II, III, and IV ulcers, respectively. Prescribed bed rest for weeks or months may also negatively affect one's self-esteem and mood.10
Although the presence of a pressure ulcer is largely assumed to negatively influence QoL, our understanding of how to assess QoL post-SCI is confounded by a number of issues.11 For instance, concurrent secondary health conditions post-SCI (e.g. pain, spasticity, depression, etc.) may minimize the sensitivity of the QoL outcome tool to measure pressure ulcer impact. To ensure that descriptions of pressure ulcer impact are appropriately characterized, measures should be selected according to the domains that they evaluate and the population and pathologies for which they are designed.12 In order to achieve this goal, it is imperative that investigators have a clear understanding of conceptual and measurement issues related to QoL.
QoL can be defined as having one's individual needs and desires fulfilled within reason; a belief that life is offering the appropriate balance of challenges and successes in particular areas of personal salience; and happiness and satisfaction that life is delivering all or most of what is expected or desired.13 A related construct that has received much attention with regard to SCI outcomes is participation, which is defined as “involvement in life situations” and includes social functioning, and physical and emotional role limitations.14 Despite being distinct, albeit related, constructs, QoL and participation are frequently confounded and/or used interchangeably with health-related QoL, which focuses more on the consequences of illness and disability.
An emerging issue in the field is the notion that QoL can be measured from a subjective and/or objective perspective.15 An objective perspective refers to observable life conditions or physical functioning that are often determined by societal norms that can be operationalized by tests, which obtain a total score by assessing various indicators of “the good life” (i.e. possessions, achievements, statuses, etc.)16 Conversely, a subjective viewpoint of QoL accounts for the respondents' perception.17 With subjective instruments, QoL can be determined (1) by the person who lives it or (2) by the discrepancy between a person's standards, goals, values, and his/her actual situation, accomplishments, etc.18 Objective and subjective approaches to assessing QoL have their respective strengths and weaknesses.15 These issues should be taken into account to ensure that the measures employed are (1) congruent with the intended goals and outcomes of the project, and (2) are meaningful to the target audience to whom the results will be delivered (e.g. decision makers, advocacy groups, etc.).
To date, no systematic reviews on the influence of pressure ulcers on QoL or on the appropriateness of QoL measures for assessing pressure ulcers have been conducted. Given the substantial influence pressure ulcers have on QoL, there is a need to improve conceptual understandings of QoL to ensure that investigators employ appropriate research designs as well as suitable outcome measures to assess this serious secondary health condition associated with SCI. Hence, the purpose of this systematic literature review was to classify and evaluate outcome measures used to assess the influence of pressure ulcers on QoL (and other related constructs, such as participation, social support, etc.) post-SCI. An evaluation of this nature could lead to a better understanding of QoL in the field and contribute to improved practices for identifying better tools for ascribing the burden of pressure ulcers in persons with SCI. It also may promote a greater understanding of issues surrounding pressure ulcer management and care.
Materials and methods
A systematic review of all relevant literature published from 1975 to 2011 was conducted using multiple databases (MEDLINE/PubMed, CINAHL, and PsycINFO). A broad time range was selected to ensure that the maximum number of studies could be included in this review. The key word “spinal cord injuries” and its variants were used in combination with the following terms: pressure ulcers, pressure sores, decubitus ulcers, as well as quality of life, participation, and activities of daily living. Reference lists of articles were also reviewed to identify additional relevant publications. Articles considered for review were studies published in English with adult (>18 years) SCI participants comprising at least 50% of the sample. Abstracts were verified by two reviewers and relevant articles were extracted. Studies examining global constructs of QoL or participation after SCI and studies of paediatric populations or paediatric-onset SCI were excluded. In order to maximize the identification of potential domains for investigation, qualitative studies were included for review as well.
Information from the studies was extracted into summary tables (Table 1), and the QoL measures used in the studies were categorized within Dijkers' QoL theoretical model (Table 2).15,18 This model enables classification of the construct of QoL into different perspectives (objective vs. subjective), and provides operationally defined categories of QoL. Although not explicitly described in the model, related constructs, such as participation and social support, could also be categorized using the existing framework proposed by Dijkers.
Table 1.
Identified studies on pressure ulcers and QoL post-SCI
| Reference | Research design/population/objective/QoL outcome measures | Findings |
|---|---|---|
| Sapountzi-Krepia et al.24 |
Design: Cross-sectional survey Population: 98 persons with post-traumatic paraplegia (62% male), mean age 31.4 yrs Objective: To measure the impact of pressure sores and urinary tract infections (UTI) on the everyday life activities of persons with post-traumatic paraplegia QoL outcome measures: Sarno Functional Life Scale (SFLS) |
|
| Fuhrer et al.5 |
Design: Cross-sectional survey Population: 140 (100 men) persons with SCI, mean age 36.2 yrs (±11.5), mean YPI 10.6 yrs (±7.8) Objective: To examine the prevalence and correlates of pressure ulcers in terms of their number, severity, and anatomical location were studied in community-dwelling persons with SCI QoL outcome measures: Craig Handicap Assessment and Reporting Technique (CHART) |
1. 33% of their sample had at least one Stage I pressure ulcer, and within that group, persons with more severe ulcers (Stage III or IV) had significantly ↓ means scores on the Occupation (P < 0.001) and Mobility (P < 0.05) dimensions of CHART than those with less severe pressure ulcers (Stage I or II) |
| Westgren and Levi25 |
Design: Cross-sectional survey Population: 320 persons (261 men) with SCI, mean age 42 (17–78 yrs), YPI ≤4 yrs and ≥4 yrs Objective: To determine associations between major outcome variables after SCI and QoL QoL outcome measures: Short Form Health Survey (SF-36) |
1. Pressure ulcers yielded a strong effect size with ↓ scores on the physical functioning (P = 0.001) sub-scale of SF-36 |
| Krause53 |
Design: Cross-sectional survey Population: 1017 (69% male) persons with SCI, mean age at onset 29.1, mean YPI 13.3 yrs Objective: To identify the relationship between two skin sores related variables and multiple indicators of life adjustment after SCI QoL outcome measures: Life Situation Questionnaire-Revised (LSQ-R) |
|
| Saladin and Krause52 |
Design: Cross-sectional survey Population: 475 (60% male) consumers with SCI, approx. equal distributions of Caucasians, African-Americans, Hispanics, and American-Indians, mean age at onset 29.3 yrs, mean YPI 12.8 yrs Objective: Compare the prevalence of pressure ulcer and barriers to treatment in the event of ulcer development as a function of race-ethnicity in persons with SCI QoL outcome measures: Sections of the Life Situation Questionnaire-Revised (LSQ-R); Reciprocal Social Support Scale (RSS) |
1. Individuals with higher levels of social support scores were less likely to report a current pressure ulcer (P = 0.033) |
| Anson et al.41 |
Design: Cross-sectional survey and longitudinal survey Population: 125 persons with SCI, 18 yrs+ and YPI > 1 yr Objective: (1) To explore relationships among social support, adjustment, and secondary complications in persons with SCI; and (2) to investigate the potential effects of persons' perceptions that they contribute to the social support of others as well as received social support from others QoL outcome measures: Reciprocal Social Support (RSS) scale |
|
| Krause et al.63* |
Design: Cross-sectional survey Population: 97 (78% males) American-Indians with SCI, mean age 40.4 yrs, YPI 12.4 yrs Objective: To identify factors related to risk for poor health outcomes and secondary in a sample of American-Indians with SCI QoL outcome measures: Reciprocal Social Support (RSS) scale |
|
| Anderson and Andberg47 |
Design: Cross-sectional survey Population: 141 (114 males) subjects with spinal cord dysfunction with motor and sensory deficits, mean age 34 yrs, YPI 10.5 yrs. The sample was divided into: Group 1 – 58 persons with paraplegia; Group 2 – 83 persons with tetraplegia; The groups were further sub-divided into: Group A – individuals with no time lost because of pressure sores in the last 2 yrs; Group B – individuals who lost time. Objective: To determine if psychosocial factors, not purely mechanical aspects, play an important role in the incidence of pressure sores QoL outcome measures: Satisfaction with Activities of Life (SATIS) and Responsibility in Skin Care (RESPON); Tennessee Self-Concept Scale (TSCS) |
|
| Harding-Okimoto64 |
Design: Qualitative study and cross-sectional survey Population: 5 persons with SCI and pressure ulcers, mean age 49.6 yrs, mean YPI 18.6; 5 persons with SCI without pressure ulcers, mean age 47.6, mean YPI 23.8 Objective: To determine if there is any difference in self-concept and body-image between persons with SCI and pressure ulcers and those with SCI and no pressure ulcers QoL outcome measures: Body Cathexis-Self-Cathexis Scale; Qualitative interviews |
|
| Gordon et al.75 |
Design: Cross-sectional and Retrospective survey; Population: 566 persons (79.4% male) with SCI, mean age 26.1 ± 10.4, YPI range 1–4 yrs Objective: To examine the occurrence of pressure sores during inpatient rehabilitation and scores on personal adjustment QoL outcome measures: Human Service Scale (HSS) |
|
| Lyons and Sorenson62 |
Design: Cross-sectional survey Population: 36 (27 males) persons with SCI, mean age 42 yrs, YPI range 2–46 yrs Objective: To describe subject perceptions related to the presence of a pressure ulcer & to compare QoL with those without an ulcer QoL outcome measures: Ferrans & Powers Quality of Life Index Spinal Cord Injury Version-III (QLI) |
|
| Singh et al.76 |
Design: Prospective clinical study Population: 30 patients with traumatic SCI resulting in pressure ulcers (stages III and IV). Eligibility criteria included: failure of conservative treatment to heal pressure ulcers, minimum regular follow up of 6 months, and injury below C4 Objective: To evaluate the effect of surgery for pressure ulcers on general health and quality of life in patients with SCI QoL outcome measures: Patient satisfaction questionnaire; Visual Analog Scale |
|
| Langemo et al.79 |
Design: Phenomenological qualitative study Population: 8 respondents (4 with SCI), mean age 35.75 yrs. Objective: To explore the phenomena of the lived experience of having a pressure ulcer to determine the essential structure of the experience QoL outcome measures: N/A; Qualitative interviews |
|
| Jackson et al.80 |
Design: Qualitative study Population: 20 persons with SCI and a history of pressure ulcers Objective: To identify overarching principles that explain how daily lifestyle considerations affect pressure ulcer development in adults with SCI QoL outcome measures: N/A; Qualitative interviews |
1. The study led to identification of 8 interrelated daily lifestyle principles: perpetual danger, change/disruption of routine, decay of prevention behaviors, lifestyle risk ratio, individualization, simultaneous presence of prevention awareness and motivation, lifestyle trade-off, and access to needed care, services, and supports. |
yrs, years; YPI, years post-injury; N/A, not applicable.
*Krause et al.63 also used the Craig Handicap Assessment Reporting Technique (CHART), but only used a few items. Based on this issue, and the lack of association with pressure ulcers, it was decided to exclude this part of the study from the present review.
Table 2.
Summary of outcome measures
| Measure | O vs S | QoL category/construct | SCI psychometrics | Format/scoring | Administrative burden | Sensitive to pressure ulcers |
|---|---|---|---|---|---|---|
| Body Cathexis Self-Cathexis Scale (BCSC) | S | SWB; Self-esteem | N/A | 46 items; Each item ranked on a five-point scale: 1 = Have strong feelings and wish change could somehow be made 2 = Don't like but can put up with 3 = Have no particular feelings one way or the other 4 = Am satisfied 5 = Consider myself fortunate Higher scores indicate greater body satisfaction; an overall score is achieved by summing the items and dividing the total score by 46 |
∼15–20 minutes | +Harding-Okimoto64 |
| Craig Handicap Assessment and Reporting Technique (CHART) | O | A; Disability; Proxy for Community Reintegration | Established reliability and validity for SCI See Noonan et al.91 for full details. |
32 items that are combined to provide sub-scale scores; Scoring scale has been calibrated to yield 100 for non-disabled respondents and 0 for persons with maximal handicap Each domain can receive a maximum score of 100. Domain scores also can be combined to form a total score Higher scores correspond to a role fulfillment equivalent to that of most individuals without disabilities |
∼15 minutes | +Fuhrer et al.5 |
| Ferrans and Powers Quality of Life Index – Spinal Cord Injury Version-III (QLI-SCI) | S | SWB | Cronbach's α = 0.73–0.99 Validity established for SCI See Hill et al.38 for full details. |
74 items divided into two parts: Part 1 (Satisfaction; 37 items) and Part 2 (Importance; 37 items). Each item for both parts is ranked on a six-point scale, with 1 = very dissatisfied or unimportant, and 6 = very satisfied or important Scores range from 0 to 30, with higher scores indicating better QoL |
∼10 minutes | +Lyons and Sorenson62 |
| Human Service Scale (HSS) | S | SWB | N/A | 80 items (unemployed individuals only complete questions 1–63); Likert-Scale; For each sub-scale, the maximum points are as follows: physiological (110), emotional security (152), economic security (41), family (69), social (65), economic self-vocational self-actualization (114) Scores for each scale are obtained by calculating a percentage of the total points for that scale, and based upon that determining the amount of need fulfillment an individual is experiencing (75% = high, 50% = average, 25% = low) |
∼20 minutes | +Gordon et al.75 |
| Life Situation Questionnaire – Revised (LSQ-R) | S | SWB | Cronbach's α = 0.76–0.86 | 50 items divided into two parts: Part 1 (Satisfaction; 20 items) on a five-point scale, with 1 = very dissatisfied and 5 = very satisfied; Part 2 (Problems; 30 items) on a five-point scale anchored by two statements (1 = No Problem; 5 = Major Problem) Eight subjective well-being scales are embedded into LSQ-R derived from the two major parts of the scale (Satisfaction and Problems) |
∼10 minutes | +Krause53 +Saladin and Krause52 |
| Patient Satisfaction Questionnaire | S | SWB | N/A | 4 open-ended questions No scoring, descriptive measure |
∼5 minutes | +Singh et al.76 |
| Reciprocal Social Support (RSS) Scale | S | SWB | Cronbach's α = 0.73 | Eight questions rating each type of support received from their families, friends, and community; Responses are ranked on a seven point scale, with 1= never and 7= always. Higher scores indicated greater levels of support |
∼20 minutes | +Anson et al.41 −Krause et al.63 +Saladin and Krause52 |
| Sarno Functional Life Scale (SFLS) | O | A | N/A | 44 items designed to measure the five elements of performance on four qualities of performance (self-initiation, frequency, speed, and overall efficiency) that are ranked on a five point scale: 0 = Does not perform the activity at all 1 = Very poor 2 = Deficient 3 = Approaches normal 4 = Normal The scoring of SFLS is a matter of finding the proportion of the patient's scores with respect to his/her maximum score. Scores are obtained for each category and each quality of performance being measured. The overall score obtained is the proportion of the patient's total score in all five categories compared to his/her maximum possible total |
∼15–20 minutes | +Sapountzi-Krepia et al.24 |
| Satisfaction with Activities of Life (SATIS) | S | SWB | N/A | 6 domains of activities rated on a continuum with three levels: dissatisfaction (1.00); neutral (2.00); and satisfaction (3.00). Higher scores indicate greater satisfaction |
+Anderson and Andberg47 | |
| Short-Form Health Survey (SF-36) | O | A; HRQoL | Established reliability & validity for SCI See Noonan et al.91 for full details. |
36 items covering eight domains related to functioning and health The scoring is norm-based, with a general population mean score of 50 and a standard deviation of 10 Higher scores indicate higher levels of health |
∼5–10 minutes | +Westgren and Levi25 |
| Tennessee Self-Concept Scale (TSCS) | S | SWB; Self-concept | N/A | 100 items ranked on a five-point scale: 1 = Always False 2 = Mostly False 3 = Partly False and Partly True 4 = Mostly True 5 = Always True The clinical and research form yields 29 profiled scores |
∼15–20 minutes | −Anderson and Andberg47 |
| Visual analog scale (VAS) | S | SWB | N/A | A 100 mm visual analog scale ranging from 0 (very low) to 100 (very high) on which respondents record their perception of QoL Higher scores indicate higher levels of QoL |
∼5 minutes | +Singh et al.76 |
A, Achievement; HRQoL, Health-related quality of life; O, Objective; N/A, Not available; S, Subjective; SCI, Spinal cord injury; SWB, Subjective well-being; + Sensitive to pressure ulcer impact; − Not sensitive to pressure ulcer impact.
According to Dijkers'18 conceptualization, the construct of QoL can be divided into three main concepts, which include QoL as “Utility”, QoL as “Achievements”, and QoL as “Subjective Well-Being”. Qol as “Utility” (box A in Fig. 1), is defined as preference-based health state valuations such as those used in cost evaluations in health care. Achievements and statuses are evaluated in terms of societal norms and standards (box B in Fig. 1), and the resulting assessments (box A in Fig. 1) “reflect the desirability of, relative preference for, or even value of life” (ref.18, p. 89) that can be measured across several domains (box C in Fig. 1). This type of analysis often yields a health utility (or health preference) score, which relates to a person's state of well-being. It is a single metric anchored at 0 (death) and 1 (perfect health) that represents a preference for a health state.19 These health state morbidities are measured across a group of individuals and aggregated into a utility score, which can then be used as quality weight for calculating the number of quality-adjusted life-years gained in cost-utility analyses.20 Hence, this perspective considers only the outsider's viewpoint when determining QoL.
Figure 1.
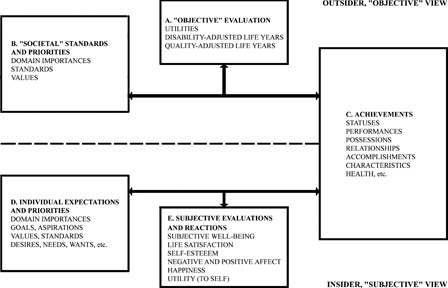
Three conceptualizations of QoL and their interrelations (Adapted, with permission, from Dijkers15).
Qol as “Achievements” places emphasis on people's possessions, statuses, relationships, accomplishments, etc. (box C in Fig. 1). Some examples of major domains include “employment and education, marriage and spousal relations, sexuality, other major social relations (e.g. friendships), leisure activities, spirituality and religion, healthcare, equipment and accessibility, and personal caregivers”. [ref.17, p. 99] Health-related QoL is often included within this category of achievements.
QoL as “Subjective Well-Being” is typically represented as the sum total of the cognitive and emotional reactions that people experience (box E in Fig. 1) when they compare what they have and do in life (box C in Fig. 1) with their aspirations, needs, and other expectations (box D in Fig. 1).18 QoL can therefore be expressed as the discrepancy between an individuals' actual status and the one he/she desires or expects.
Results
The initial search strategy yielded a total of 71 studies. After reviewing the abstracts, most of the studies did not meet the inclusion criteria (i.e. did not explicitly link pressure ulcers and QoL in their assessments and/or only discussed implications of pressure ulcers to QoL, etc.). Fourteen studies remained (see Table 1). There were nine cross-sectional observational studies, one study with a combined cross-sectional and longitudinal design, one prospective study, one mixed methods (quantitative and qualitative) study, and two qualitative studies.
Applicability of objective QoL measures on assessing pressure ulcers
With regard to objective measures of QoL, Sarno Functional Life Scale (SFLS),21 Craig Handicap Assessment and Reporting Technique (CHART),22 and Short-Form 36 (SF-36)23 have been used to assess the influence of pressure ulcers (see Table 2). SFLS (boxes B and C, see Fig. 1) assesses cognition, activities of daily living, activities in the home, outside activities, and social interaction.21 CHART (boxes B and C, see Fig. 1) quantifies handicap (loss or limitation of opportunities to take part in the life of the community on an equal level with others)14 by evaluating five domains: “Physical Independence”, “Mobility”, “Occupation”, “Social Integration”, and “Economic Self-Sufficiency”. SF-36 (boxes B and C, see Fig. 1) is a generic health status measure that covers eight domains: physical functioning, role limitations due to physical health problems, bodily pain, general health, vitality, social functioning, role limitations due to emotional problems, and mental health.23
Of the three studies that used objective measures,5,24,25 the study by Fuhrer et al.5 is the only one that provides a clear depiction of the influence of pressure ulcers on community reintegration by correlating pressure ulcer severity with scores on CHART. Fuhrer et al.5 found that persons with more severe pressure ulcers had significantly lower scores on the Occupation and Mobility sub-scores than those with less severe ulcers. A benefit of CHART is that it is a valid and reliable measure for the SCI population.22,26 As well, the “Spinal Cord Outcomes Partnership Endeavor” (SCOPE), which is a broad-based international consortium of scientists and clinical researchers representing various bodies (academic institutions, industry, government agencies, not-for-profit organizations and foundations) has endorsed CHART,27 although not specifically for measuring the impact of pressure ulcers. It should be noted that CHART is not considered a QoL measure, but rather a measure of handicap often used to assess participation.14
Although sensitive to the presence of pressure ulcers, both the SLFS and SF-36 instruments have some issues with regard to their applicability to SCI. An issue with the SLFS is that it appears to have been used only in the one study24 identified for this review. No SCI studies on other topics (general QoL, other SCI health conditions, etc.) were found to include this scale. As well, SFLS has served as the basis for the Level of Rehabilitation Scale (LORS)28 (boxes B and C, see Fig. 1), which is a rehabilitation functional outcome measure, and subsequent derivatives (i.e. LORS-II and III). It is arguable that SFLS items of social relations and everyday life activities could be construed as assessing participation or community integration, but the scale appears to be closer to that of a functional status measure that is generic in nature, and not condition-specific.29 Thus, caution is warranted with using SFLS as the psychometric properties of this scale for SCI are not established, partly due to its limited use in the field of SCI, and the scale has questionable value for assessing QoL or participation due to its basis for a subsequent functional outcome measure (i.e. LORS).
Conversely, SF-36 is one of the most commonly used measures of health-related QoL,30 with well-established psychometric properties for multiple health conditions,31 which allows for the evaluation of various patient populations. SF-36 has been validated in multiple SCI studies. The reliability of the scale has been shown to be moderate to high (α = 0.72–0.98), with the exception of the general health item.32,33 However, there is some controversy surrounding this measure cannot be disregarded. For instance, respondents who use wheelchairs have found the wording of certain SF-36 items to be offensive,34,35 since five of its ten items refer to climbing or walking. One study dropped these questions from the scale because of a perception they were derogatory to persons with SCI.36 Some people with disabilities also perceive that the underlying assumptions of SF-36 are flawed regarding their QoL,37 with one issue being that persons with disabilities do not equate disability with health.35
Despite these controversies and problems, SF-36 has been widely used to assess health-related QoL in persons with SCI, and its limitations may be minimized by using it in conjunction with condition-specific tools.35 As well, the development of SF-36V has addressed some of the noted problems of SF-36 with SCI, but this scale has not yet been validated for this population.38 Similar to CHART, SF-36 has been endorsed by SCOPE,27 but again, not specifically to assess the impact of pressure ulcers.
In summary, the objective measures identified were all sensitive to the presence of pressure ulcers (lower QoL/participation associated with pressure ulcers), and fall into QoL as “Achievements” category of Dijker's model.18 However, these measures were not originally intended to assess QoL per se (i.e. CHART and SFLS) and/or are limited in terms of their applicability for SCI (i.e. SF-36, SFLS). Further work examining the applicability of SF-36V for investigating the influence of pressure ulcers might be warranted, since it appears to have qualities that are more appropriate to studying SCI-related outcomes than does its predecessor.
Applicability of subjective QoL measures on assessing pressure ulcers
The use of subjective measures of QoL has been more widely applied to the study of pressure ulcers (see Table 2). Identified measures include Life Situation Questionnaire-Revised (LSQ-R),39,40 Reciprocal Social Support Scale (RSS),41 Tennessee Self-Concept Scale (TSCS),42 Body Cathexis-Self Cathexis (BCSC) scale,43 Human Service Scale (HSS),44 Ferrans and Powers,45 Quality of Life Index (QLI) SCI Version III,46 Satisfaction with Activities of Life (SATIS),47 and a QoL visual analog scale (VAS).48
LSQ-R (boxes C–E, see Fig. 1) measures a broad range of long-term SCI outcomes, including those related to employment, medical treatments, social activities, and subjective well-being,49,50 and has undergone major revisions to increase its core content coverage, particularly for items relating to subjective well-being.41,51 LSQ-R contains seven factor scales, including: “Engagement”, “Negative Emotions”, “Health Problems”, “Career Opportunities”, “Finances”, “Living Circumstances”, and “Inter-Personal Relations”. In addition, LSQ-R consists of several sets of items that were designed to measure objectively verifiable information, such as pressure ulcer outcomes,52 rather than psychometric scales of underlying theoretical constructs (e.g. efficacy). Each set of items was designed to be measured independently of other sets of items, without compromising validity. In other words, each set of items on LSQ-R could be considered a separate instrument. In the study by Saladin and Krause,52 two additional item sets were included: the first had five questions identifying barriers to maintaining bed rest after getting an open sore, and the second identified barriers to seeing a physician in the event of a pressure sore (described as an open sore on the questionnaire). As well, Krause53 supplemented LSQ-R with an “Adjustment”, “Medical Instability”, and “Fitness” factor scales.
LSQ-R is a condition-specific instrument that appears appropriate and valid for the SCI population,54,55–58 and has items sensitive to the presence of pressure ulcers and other health conditions (i.e. urinary tract infections). Hallin et al.58 noted that the LSQ or its revised form have not been used consistently, with discrepancies found in the number of items used and scale developed. The scale employs a mix of both objective and subjective items, although later versions emphasize the items that affect subjective well being.18 Despite the variety in its application, Hallin et al.58 found in their meta-analysis of QoL measures used in SCI research that LSQ-R has high levels of reliability (Cronbach's α = 0.76–0.86). A strength of the study by Saladin and Krause52 was that each added item set was developed using a combination of consumer input and expert judgment. However, the emphasis in their study52 was on identifying the prevalence of pressure ulcers and barriers to treatment, and thus used LSQ-R to independently measure this issue, rather than the underlying construct of well-being. Nevertheless, the items used were sensitive to barriers that were societal in nature. Based on the evidence, LSQ-R is suitable for assessing the impact of pressure ulcers, but it may be warranted to use it in combination with global measures of subjective well-being given the issues noted above in the study by Saladin and Krause.52
QLI (boxes C–E, see Fig. 1) measures satisfaction in and the relative importance of the following domains: Health and Functioning, Socioeconomic Status, Psychological and Spiritual Well-Being, and Family Relationships. QLI has been used in other QoL SCI-related studies59,60 and can be administered by client self-report or via interview. There is support for the homogeneity reliability with Cronbach's alpha scores of 0.73–0.99.46,61 However, factorial analysis of the scale revealed that the domain structure did not fit with subject interpretations.46 Further, the correlation of the importance of scores was very low (r = 0.47). Despite these issues with the scale, QLI appears to be sensitive to the presence of pressure ulcers,62 with persons with SCI and pressure ulcers having lower scores on QLI than those without, except for the “Family” sub-score, which yielded no differences. Overall, QLI seems well suited to assessing the impact of pressure ulcers post-SCI, but it has been suggested38 that QLI may require alteration to the structure of the importance scale scoring. As well, Hill and colleagues38 suggest that the scale may require domain rearrangement.
RSS (boxes C and E, see Fig. 1) was designed to “measure the amount of support given to and received from family members, friends, and the community” (ref.63, p. 926). Individuals rate the frequency with which they receive four types of support: social interaction, material assistance, emotional support, and non-paid personal assistance. RSS appears to be a suitable measure of social support for use in SCI, but its findings regarding pressure ulcer impact are mixed.41,52,63 One study63 investigating how QoL is influenced by pressure ulcers in an American-Indian population provided alpha coefficients for RSS, which ranged from 0.70 to 0.76 for the four types of support, with an average of 0.73. The alpha for the upsets scale was 0.55; however, low internal consistency is expected given that the scale sums evaluations were made by three groups: family, friends, and community.63 As well, the lack of significant findings in this study63 may be attributable to using RSS in a sample of American-Indians. RSS has not been validated for use in this minority group, which may have contributed to the lack of an effect. As well, findings reported from homogenous samples lack generalizability.
Some studies that did not detect an effect only used some of the sub-scales of RSS.52,63 It may be that the other sub-scales have greater sensitivity to the presence of pressure ulcers. Based on the evidence, further work is needed to better elucidate the relationships between pressure ulcers and social adjustment and support factors.
Self-esteem appears to be a promising construct for investigation of QoL, but the measures identified (BCSC, TSCS, and HSS) have no psychometric evidence to support their use in SCI. Further, some of the measures showed only a trend towards significance (BCSC and TSCS), with self-esteem scores being negatively influenced by having a pressure ulcer. This lack of an effect could be partly attributed to small sample size in one case.64 It should be noted that TSCS (boxes C and E, Fig. 1), a measure of total self-concept (sub-scales include physical, moral, personal, family, social, and academic work), has been used in other SCI studies,65,66 and has good psychometric properties with use in other populations, with a reported test–retest reliability of 0.92 and Cronbach's α = 0.94.67 Similarly, the BSCS (boxes C and E, Fig. 1), which assesses the degree of a person's satisfaction with the various parts or processes of the body, is a valid and reliable measure used in the body image literature,68 and has been used with clinical populations.69–71 Future studies considering these measures should pair either TSCS or BCSC with instruments with better psychometric evidence for use in persons with SCI, such as the Rosenberg Self-Esteem Scale,72 which has good internal consistency (α = 0.82)73 and reproducibility (good to excellent; 92%)61 in this population.
HSS (boxes C and E, Fig. 1) assesses psychosocial adjustment, which is determined by scores on seven scales (Physiological, Emotional Security, Social, Family, Economic Security, Economic Self-Esteem, and Vocational Self-Actualization), and is based on Maslow's theory of needs.74 In particular, the Economic Self-Esteem and Social sub-scales of HSS may be sensitive to the influence of pressure ulcers, which showed negative correlations to one another.75 However, the Economic Self-Esteem scale was also related to other independent factors (i.e. sex, race, impairment, and occupation). Further, the relationships and effect sizes detected were not straightforward or as strong as expected.75 This suggested that the association between pressure ulcers and social adjustment is complex, and mediated by other factors.
Anderson and Andberg47 developed their own surveys to examine factors related to QoL and psychological well-being and how these related to pressure ulcer development and maintenance in persons post-SCI. With regard to QoL, one survey assessed perceived satisfaction in various domains (SATIS; boxes C and E, Fig. 1). SATIS assessed satisfaction with six groups of activities: education classes, employment, avocational activities, group activities, living arrangements, and sexual activity.
Singh et al.76 used a VAS (boxes C and E, Fig. 1) to evaluate the effect of surgery for pressure ulcers on QoL in patients with SCI. They also used the following questions to assess patient satisfaction: (1) Had surgery resulted in improvement in subjective well-being? (2) Was the patient satisfied with ultimate rehabilitation outcome after surgery? (3) Had surgery led to improvement in QoL? and (4) In what areas of life had QoL improved after surgery?
The use of study specific measures (i.e. SATIS) or global ratings of QoL using a VAS have value for studying pressure ulcer impact but are problematic. The main problems with study-specific questionnaires are that they are not comparable to questionnaires designed for the general population, effect sizes are not calculated, information on cross-cultural applications is not available, and the instruments assess different dimensions.58 Similarly, VAS may best represent an individual's global QoL without the constraints of predetermined domains.77 At this time, use of VAS in SCI has only been strongly recommended to assess SCI-related pain,78 and its applicability to pressure ulcers is unknown but likely to be somewhat insensitive for identifying particular domains of impact (e.g. relationships, vocation, etc.).
Overall, the majority of measures of QoL as “Subjective Well-being” appear to be sensitive to pressure ulcer impact with some mixed findings regarding the applicability of RSS and measures of self-esteem (TSCS, BCSC, and HSS). Only two measures (LSQ-R and QLI SCI Version III) have adequate psychometric evidence for use with the SCI population. Given their established appropriateness for SCI, further work utilizing LSQ-R and QLI SCI Version III to assess the influence of pressure ulcers is recommended. Self-esteem appears to be a promising construct for investigation, but as noted above, future studies using TSCS or BCSC might benefit by pairing it with the Rosenberg Self-Esteem Scale.
Qualitative reports
The qualitative findings reviewed identify many QoL domains assessed in the quantitative studies (i.e. self-esteem), as well as highlight other areas that are affected when one sustains a pressure ulcer.
Lyons and Sorenson62 investigated the impact of pressure ulcers in 36 persons with SCI by using content analysis on the responses by participants to four open-ended questions on a survey. Findings demonstrated themes reflecting: (1) loss of independence, (2) fear and frustration, (3) pain and discomfort, and (4) decreased social interaction. As well, Harding-Okimoto64 conducted semi-structured interviews regarding self-concept and body image with 10 persons with SCI (50% with pressure ulcers). Those with ulcers reported being influenced by others' perceptions of them, and had negative perceptions of their physical appearance and did not check their skin regularly, while persons without pressure ulcers did not report the same issues of influence on physical appearance, and conducted regular skin checks. Further, persons with ulcers reported that perceptions of others had changed when they developed their ulcers, with some reporting their parents becoming more “smothering” and “intense”, and two reported feeling as a “burden to their caregiving wives” (ref.64, p. 115). The findings are echoed in the phenomenological study by Langemo et al.,79 who explored the phenomena of the lived experience of having a pressure ulcer (N = 8) to determine the essential structure of the experience in persons with various impairments (50% of the sample was SCI). They found that having a pressure ulcer negatively impacted their life in that it required prolonged periods of being immobilized (i.e. due to bed rest) and social isolation during healing. It also negatively influenced body image perception, and persons struggled to regain control and independence over their lives while dealing with their pressure ulcer. The pain associated with the wound and dealing with difficult treatment regimens were issues that affected their lives.
Jackson et al.80 conducted interviews with persons with SCI (N = 20) that had a history of pressure ulcers. Eight life principles, describing reasons for which pressure ulcers develop in adults with SCI, were identified: perpetual danger (of incurring a pressure ulcer), change/disruption of routine (as a result of a pressure ulcer), decay of prevention behaviours over time, lifestyle risk ratio, individualization (i.e. differences in pressure ulcer effects from person to person), simultaneous presence of awareness and motivation (to avoid pressure ulcers), lifestyle trade-off (between the need to avoid pressure ulcers and the need to live a fulfilling life), and access to needed care, services, and supports.
The qualitative reports highlight that sustaining a pressure ulcer negatively influences social interactions by contributing to situations that strain relationships with significant others or causes isolation due to treatments (i.e. bed rest) and/or reduces social activities/roles that may contribute to the development/worsening of pressure ulcers (i.e. employment).62,64,79,80 One salient area noted by some of the qualitative reports, but not assessed by the quantitative studies in the review, was the issue of pain stemming from the pressure ulcer.62,79,80 Overall, the studies described above might serve as a starting point for supplementing existing QoL measures with additional questions to better assess the influence of pressure ulcers, and/or to develop a condition-specific QoL measure of pressure ulcers post-SCI.
Discussion
The purpose of this review was to identify and classify outcome measures used to assess the influence of pressure ulcers on QoL post-SCI in order to improve the QoL outcome tool selection process for describing the burden of pressure ulcers. From this review, the identified measures were only representative of two of the three major domains of Dijker's18 model, which included QoL as “Achievements” and QoL as “Subjective Well-Being”. Under QoL as “Achievements” category, objective measures of community participation (CHART and SFLS) and health-related QoL (SF-36) were assessed. Under QoL as “Subjective Well-Being” category, measures of global subjective well-being (VAS) were assessed as well of measures of subjective well-being that assess specific domains of life (SATIS, LSQ-R, QLI SCI Version III, and HSS), such as self-esteem (BCSC and TSCS), and social support (RSS). Many of the measures (objective and subjective) used appear to be sensitive to the presence of pressure ulcers, but only a few have sufficient psychometric evidence for use in the SCI population (CHART, SF-36, LSQ-R, and QLI SCI Version III). The lack of psychometric data for some of the measures does not negate future use for investigating pressure ulcers, but they should be paired with complementary measures validated for SCI to help advance their applicability. As well, when surveys designed specifically for a study are employed, their contents should be well described to facilitate replication and assessment. In general, using study-specific questionnaires is not highly recommended unless there are no appropriate measures available to investigate the construct of interest. Further, the development of instruments would benefit by being structured within a theoretical framework or informed by a qualitative process. Qualitative findings reinforced the notion that measures collecting information on related QoL constructs, such as social support and body self-esteem, may be pertinent domains that are negatively influenced by pressure ulcers post-SCI.
As noted, objective and subjective measures have their respective strengths and weaknesses. Objective measures have the advantage of capturing important qualities of the society that subjective measures may not take into account. For instance, subjective measures only take into account the person's perception on a particular domain, while ignoring those that are based on widely shared values.81 As a result of this issue, subjective measures are sometimes “criticized as ‘soft measures’, someone's feelings about a condition within the environment, and not the condition itself” (ref.82, p. 47). Conversely, objective measures are criticized for failing to consider the individual's perception. Not surprisingly, objective measures of QoL are often poorly correlated with perception and satisfaction with life.81,82
Within the context of the current review, it is interesting to note that the social integration sub-scale of CHART (an objective measure) was insensitive to pressure ulcer severity whereas other reports using subjective measures or qualitative approaches found that social support was a domain negatively influenced by pressure ulcers.41,52,79 CHART is limited to assessing only the extent of an individual's social network.83 It does not assess important aspects such as the frequency of supportive behaviours offered by the support network, or the individual's personal evaluation of how they view the quality of their social support.83 Although CHART is a validated and widely used measure in the field of SCI, its objective perspective limits its suitability for a study if the main outcome of interest is social support. In addition to its psychometric properties, the theoretical underpinnings of an outcome tool should be considered to determine if it would best answer a research question. Given that objective and subjective measures offer contrasting perspectives on what constitutes QoL that are of value to different stakeholders (i.e. objective measures valued by health policy decision makers), it might be a good practice to use (where possible) both an objective and a subjective measure. Doing so may allow for a broader perspective on the impact of a condition (e.g. pressure ulcers) on QoL post-SCI.
A significant limitation across the majority of studies is that they utilized self-report data on current or past pressure ulcer occurrence, severity, and/or location (e.g. hospitalization, number of pressure ulcers, days impacted by pressure ulcers). In addition, information on the categorization of the pressure ulcer severity using the stages, such as the ones as defined by the National Pressure Ulcer Advisory Panel (Grade I, II, III, or IV),84 was lacking. The only exceptions were the studies by Fuhrer et al.,5 Langemo et al.,79 Harding-Okimoto,64 and Singh et al.,76 all of whom used clinical data (e.g. hospital records and direct assessment) to describe pressure ulcer location and severity. Lyons and Sorenson62 collected self-report data on pressure ulcer severity, and only included persons with grade III or grade IV ulcers. Overall, future studies should employ more rigorous means of pressure ulcer categorization to help improve the quality of findings regarding their impact on QoL.
Another issue related to evidence reviewed is that most of the studies employed a cross-sectional design, which makes it difficult to ascribe the direction of the relationship between QoL and pressure ulcers. For instance, in the study by Harding-Okimoto64 examining self-esteem and body image in persons with and without pressure ulcers, the pressure ulcer group may have had pre-existing body image and self-esteem issues that decreased their likelihood of performing skin checks. More research studies that examine associations between QoL and changes in wound status over time (open versus healed; severity) would help to clarify this matter since it would inform investigators if QoL changes in persons as their pressure ulcers heal.
One area that would help to better attribute the causality and impact of pressure ulcers on QoL is to develop a condition-specific (pressure ulcer) measure of QoL to ascribe burden. Measures for use exist for other SCI-related secondary health conditions, such as spasticity (i.e. Spinal Cord Injury Spasticity Evaluation Test),85 bladder dysfunction (i.e. Qualiveen),86 neurogenic bowel (i.e. Neurogenic Bowel Dysfunction Score),87 etc. The advantage of having a condition-specific measure is that it may quantify impact of a pressure ulcer on domains deemed relevant to the person with SCI, while not being overshadowed by general issues affecting QoL (e.g. employment, marital status, etc.). As well, it may be useful to identify specific factors related to pressure ulcers that negatively influence QoL (i.e. pain stemming from the pressure ulcer). At this time, there are no SCI-specific pressure ulcer QoL measures.
One potential measure that is specific to assessing the influence of pressure ulcers on QoL, and that addresses some of the qualitative themes raised across studies in the review64,79,80 is Cardiff Wound Impact Schedule (CWIS) (boxes C and E, Fig. 1).88 The CWIS assesses the impact of chronic wounds and has three scales: (1) Physical Symptoms and Daily Living; (2) Social Life; and (3) Well-being. The “Physical Symptoms and Daily Living” and “Social Life” sub-scales assess both the experience of a given symptom/problem and the associated stress experienced with those symptoms/problems. The “Well-being” scale assessed the respondent's well-being in relation to the wound, such as anxieties about outcome. The CWIS has undergone extensive piloting on persons with leg ulcers and diabetic foot ulcers to establish its psychometric properties by comparing it to SF-36.88 Factor analysis from the development study found that internal consistency was good (α = 0.77–0.96) and reproducible.88 The CWIS discriminated between persons with healed ulcers and those with open ulcers. Construct validity was demonstrated by strong correlations between related items on CWIS and SF-36. Although there are no published studies on the applicability of the CWIS to persons with SCI, there are currently several on-going Canadian clinical SCI-related research studies using this tool.89 Some modifications are likely needed to account for the impact of sacral/coccygeal wounds. However, the CWIS may be an ideal tool to use in conjunction with other health-related QoL measures, and may be of use to clinicians wishing to assess the effectiveness of various interventions. Within the SCI literature there is limited evidence25 that pressure ulcers affect “Physical Functioning” on SF-36. As such, it is reasonable to assume that the CWIS may be appropriate for persons with SCI, but it may be prudent to use it alongside SF-36 at this time to help validate it for this population.
Conclusion
Pressure ulcers are a significant issue for persons with SCI, and accurately ascribing their burden is important for ensuring that adequate resources can be obtained to help successfully manage them and prevent their occurrence. Although their significance is well recognized, it is surprising to learn that the majority of identified studies used self-report for describing the location and/or severity of ulcers. Further, the lack of validated QoL outcome measures or QoL measures specific to pressure ulcer impact is problematic. More work is required to properly describe the impact of pressure ulcers from both an objective and subjective perspective using suitable measures for the SCI population. In particular, the lack of research using measures that quantify QoL as “Utility” are sorely needed to inform cost-effectiveness models of emerging treatments for pressure ulcers. Given the high cost of pressure ulcers to the health care system,90 ascribing burden of ulcers from this perspective might help justify the need to key decision makers for additional resources to manage this serious secondary health condition. The use of robust research designs that lend themselves to inferring causation of pressure ulcers to negatively affect QoL is also warranted. Improving practices in these domains may lead to a greater understanding of issues surrounding pressure ulcer management and care.
Acknowledgment
This project was supported by the Ontario Neurotrauma Foundation and the Réseau provincial de recherche en adaptation-réadaptation (REPAR) (Grant nos 2010-KM-SCI-QOL-825; 2008-ONF-REPAR-601; 2007-ONF-REPAR-518); Salary support to Dr SL Hitzig is provided by the Ontario Neurotrauma Foundation and the Rick Hansen Institute (Grant no. 2010-RHI-MTNI-836); Additional support was provided by the Toronto Rehabilitation Institute, which receives funding under the Provincial Rehabilitation Research Program from the Ministry of Health and Long-Term Care in Ontario. The views expressed do not necessarily reflect those of the Ministry.
References
- 1.Byrne DW, Salzberg CA. Major risk factors for pressure ulcers in the spinal cord disabled: a literature review. Spinal Cord 1996;34(5):255–63 [DOI] [PubMed] [Google Scholar]
- 2.Hitzig SL, Tonack M, Campbell KA, McGillivray CF, Boschen KA, Richards K, et al. Secondary health complications in an aging Canadian spinal cord injury sample. Am J Phys Med Rehabil 2008;87(7):545–55 [DOI] [PubMed] [Google Scholar]
- 3.Niezgoda JA, Mendez-Eastman S. The effective management of pressure ulcers. Adv Skin Wound Care 2006;19(Suppl 1):3–15 [DOI] [PubMed] [Google Scholar]
- 4.Krause JS, Saunders LL. Health, secondary conditions and life expectancy after spinal cord injury. Arch Phys Med Rehabil 2011;92(11):1770–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fuhrer MJ, Garber SL, Rintala DH, Clearman R, Hart KA. Pressure ulcers in community-resident persons with spinal cord injury: Prevalence and risk factors. Arch Phys Med Rehabil 1993;74(11);1172–7 [PubMed] [Google Scholar]
- 6.Richards JS, Waites K, Chen YY, Kogos K, Schumitt MM. The epidemiology of secondary conditions following spinal cord injury. Top Spinal Cord Inj Rehabil 2004;10(1):15–29 [Google Scholar]
- 7.Consortium for Spinal Cord Medicine Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health care professionals. J Spinal Cord Med 2001. Spring;24(Suppl 1):S40–101 [DOI] [PubMed] [Google Scholar]
- 8.Regan M, Teasell RW, Keast D, Abut JL, Foulon Bl, Mehta S. Pressure ulcers following spinal cord injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, et al., eds. Spinal cord injury rehabilitation evidence. Version 4.0, 2012. Available at: http://www.scribd.com/doc/8951639/Spinal-Cord-Injury-Rehabilitation-Evidence [Google Scholar]
- 9.New PW, Rawicki HB, Bailey MJ. Nontraumatic spinal cord injury rehabilitation: pressure ulcer patterns, prediction, and impact. Arch Phys Med Rehabil 2004;85(1):87–93 [DOI] [PubMed] [Google Scholar]
- 10.Jones ML, Mathewson CS, Adkins VL, Ayllon T. Use of behavioral contingencies to promote prevention of recurrent pressure ulcers. Arch Phys Med Rehabil 2005;84(6):796–802 [DOI] [PubMed] [Google Scholar]
- 11.Dijkers M. “What's in a name?” The indiscriminate use of the “Quality of life” label, and the need to bring about clarity in conceptualizations. Int J Nurs Stud 2007;44(1):153–5 [DOI] [PubMed] [Google Scholar]
- 12.Emery MP, Perrier L, Acquadro C. Patient-Reported Outcome and Quality of Life Instruments Database (PROQOLID): Frequently asked questions. Health Qual Life Outcomes 2005;8(3):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kemoun G, Benaim C, Thevenon A. Une approache de la qualité de vie: l'évaluation individualisée. Ann Réadaption Méd Phys 1996;39(3):171–7 [Google Scholar]
- 14.WHO ICF: International classification of functioning, disability and health. Geneva: World Health Organization; 2002 [Google Scholar]
- 15.Dijkers MP. Individualization in quality of life measurement: instruments and approaches. Arch Phys Med Rehabil 2003;84(4 Suppl 2):S3–14 [DOI] [PubMed] [Google Scholar]
- 16.Browne JP, O'Boyle CA, McGee HM, McDonald NJ, Joyce CR. Development of a direct weighting procedure for quality of life domains. Qual Life Res 1997;6(4):301–9 [DOI] [PubMed] [Google Scholar]
- 17.Moons P, Budts W, de Geest S. Critique on the conceptualisation of quality of life: A review and evaluation of different conceptual approaches. Int J Nurs Stud 2006;43(7):891–901 [DOI] [PubMed] [Google Scholar]
- 18.Dijkers MP. Quality of life of individuals with spinal cord injury: A review of conceptualization, measurement, and research findings. J Rehabil Res Dev 2005;42(3 Suppl 1):87–110 [DOI] [PubMed] [Google Scholar]
- 19.Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI®): concepts, measurement properties and applications. Health Qual Life Outcomes 2003;16(1):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Torrance GW. Measurement of health state utilities for economic appraisal: a review. J Heath Econ 1986;5(1):1–30 [DOI] [PubMed] [Google Scholar]
- 21.Sarno JE, Sarno MT, Levita E. The Functional Life Scale. Arch Phys Med Rehabil 1973;54(5):220. [PubMed] [Google Scholar]
- 22.Whiteneck G, Charlifue SW, Gerhart KA, Overholser JD, Richardson GN. Quantifying handicap: a new measure of long-term rehabilitation outcomes. Arch Phys Med Rehab 1992;73(6):519–26 [PubMed] [Google Scholar]
- 23.Ware JEJ, Kosinski M, Gandek B. SF-36 health survey: manual and interpretation guide. Lincoln: QualityMetric; 2001 [Google Scholar]
- 24.Sapountzi-Krepia D, Soumilas A, Papadakis N, Sapkas G, Nomicos J, Theodossopoulou E, et al. Post traumatic paraplegics living in Athens: the impact of pressure sores and UTIs on everyday life activities. Spinal Cord 1998;36(6):432–7 [DOI] [PubMed] [Google Scholar]
- 25.Westgren N, Levi R. Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil 1998;79(11):1433–9 [DOI] [PubMed] [Google Scholar]
- 26.Hall KM, Dijkers M, Whiteneck G, Brooks CA, Krause JS. The Craig Handicap Assessment and Reporting Technique (CHART): Metric properties and scoring. Top Spinal Cord Inj Rehabil 1998;4(1):16–30 [Google Scholar]
- 27.Alexander MS, Anderson KD, Biering-Sorenson F, Blight AR, Brannon R, Bryce TN, et al. Outcome measures in spinal cord injury: Recent assessments and recommendations for future directions. Spinal Cord 2009;47(8):582–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carey RG, Posavac EJ. Program of a physical medicine and rehabilitation unit: a new approach. Arch Phys Med Rehabil 1978;59(7):330–7 [PubMed] [Google Scholar]
- 29.Cohen ME, Marino RJ. The tools of disability outcomes research functional status measures. Arch Phys Med Rehabil 2000;81(12 Suppl 2):S21–29 [DOI] [PubMed] [Google Scholar]
- 30.McHorney C, Ware JJ, Lu R, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care 1994;32(1):40–66 [DOI] [PubMed] [Google Scholar]
- 31.Ware J, Kosinski M, Keller S. SF-36 Physical and mental health summary scales: A user's manual. Boston, MA: The Health Institute; 1994 [Google Scholar]
- 32.Forchheimer M, McAweeney M, Tate DG. Use of the SF-36 among persons with spinal cord injury. Am J Phys Med Rehabil 2004;83(5):390–5 [DOI] [PubMed] [Google Scholar]
- 33.Lin MR, Hwang HF, Chen CY, Chiu WT. Comparisons of the brief form of the World Health Organization Quality of Life and Short-Form 36 for persons with spinal cord injuries. Am J Phys Med Rehabil 2007;86(2):104–13 [DOI] [PubMed] [Google Scholar]
- 34.Andresen EM, Fouts BS, Romeis JC, Brownson CA. Performance of health-related quality-of-life instruments in a spinal cord injured population. Arch Phys Med Rehabil 1999;80(8):877–84 [DOI] [PubMed] [Google Scholar]
- 35.Andresen EM, Meyers AR. Health-related quality of life outcomes measures. Arch Phys Med Rehabil 2000;81(12 Suppl 2):S30–45 [DOI] [PubMed] [Google Scholar]
- 36.Mattson-Prince J. A rational approach to long-term care: comparing the independent living model with agency-based care for persons with high spinal cord injuries. Spinal Cord 1997;35(5):326–31 [DOI] [PubMed] [Google Scholar]
- 37.Hays RD, Hahn H, Marshall G. Use of the SF-36 and other health-related quality of life measures to assess persons with disabilities. Arch Phys Med Rehabil 2002;83(12 Suppl 2):S4–9 [DOI] [PubMed] [Google Scholar]
- 38.Hill MR, Noonan VK, Sakakibara BM, Miller WC, SCIRE Research Team Quality of life instruments and definitions in individuals with spinal cord injury: a systematic review. Spinal Cord 2010;48(6):438–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krause JS. Dimensions of subjective well-being after spinal cord injury: an empirical analysis by gender and race/ethnicity. Arch Phys Med Rehabil 1998;79(8):900–9 [DOI] [PubMed] [Google Scholar]
- 40.Krause JS. Subjective well being after spinal cord injury: relationships to gender, race/ethnicity, and chronological age. Rehabil Psychol 1998;43(4):282–96 [Google Scholar]
- 41.Anson CA, Stanwyck DJ, Krause JS. Social support and health status in spinal cord injury. Int J Paraplegia 1993;31(10):632–8 [DOI] [PubMed] [Google Scholar]
- 42.Fitts WH. Manual for the Tennesse self concept scale. Nashville, TN: Counselor Recordings and Tests; 1965 [Google Scholar]
- 43.Secord P, Jourard S. The appraisal of body cathexis: body cathexis and the self. J Consult Psychol 1953;17(5):343–7 [DOI] [PubMed] [Google Scholar]
- 44.Reagles KW, Butler AS. The Human Service Scale: A new measure for evaluation. J Rehabil 1976;42(3):34–48 [PubMed] [Google Scholar]
- 45.Ferrans CE, Powers MJ. Psychometric assessment of the Quality of Life Index. Res Nurs Health 1992;15(1):29–38 [DOI] [PubMed] [Google Scholar]
- 46.May L, Warren S. Measuring quality of life of persons with spinal cord injury: substantive and structural validation. Qual Life Res 2001;10(6):503–15 [DOI] [PubMed] [Google Scholar]
- 47.Anderson TP, Andberg MM. Psychosocial factors in pressure sores. Arch Phys Med Rehabil 1979;60(8):341–6 [PubMed] [Google Scholar]
- 48.Carlsson AM. Assessment of chronic pain. I: aspects of the reliability and validity of the visual analogue scale. Pain 1983;16(1):87–101 [DOI] [PubMed] [Google Scholar]
- 49.Crewe NM, Athelstan GT, Krumberger J. Spinal cord injury: a comparison of pre-injury and post-injury marriages. Arch Phys Med Rehabil 1979;60(6):252–6 [PubMed] [Google Scholar]
- 50.Crewe NM, Krause JS. An eleven year follow-up of adjustment to spinal cord injury. Rehabil Psychol 1990;35(4):205–10 [Google Scholar]
- 51.Krause JS, Crewe NM. Long-term prediction of self-reported problems following spinal cord injury. Paraplegia 1990;28(3):186–202 [Google Scholar]
- 52.Saladin LK, Krause JS. Pressure ulcer prevalence and barriers to treatment after spinal cord injury: Comparisons of four groups based on race-ethnicity. NeuroRehabil 2009;24(1):57–66 [DOI] [PubMed] [Google Scholar]
- 53.Krause JS. Skin sores after spinal cord injury: relationship to life adjustment. Spinal Cord 1998;36(1):51–6 [DOI] [PubMed] [Google Scholar]
- 54.Krause JS. Life satisfaction after spinal cord injury: a descriptive study. Rehabil Psychol 1992;37(1):61–70 [Google Scholar]
- 55.Krause JS. Aging and life adjustment after spinal cord injury. Spinal Cord 1998;36(5):320–8 [DOI] [PubMed] [Google Scholar]
- 56.Krause JS, Anson CA. Adjustment after spinal cord injury: relationship to participation in employment or educational activities. Rehabil Couns Bull 1997;40(3):202–14 [Google Scholar]
- 57.Krause JS. Adjustment after spinal cord injury: a 9-year longitudinal study. Arch Phys Med Rehabil 1997;78:651–7 [DOI] [PubMed] [Google Scholar]
- 58.Hallin P, Sullivan M, Kreuter M. Spinal cord injury and quality of life measures: a review of instrument psychometric quality. Spinal Cord 2000;38(9):509–23 [DOI] [PubMed] [Google Scholar]
- 59.Lin KH, Chuang CC, Kao MJ, Lien IN, Tsauo JY. Quality of life of spinal cord injured patients in Taiwan: a subgroup study. Spinal Cord 1997;35(12):841–9 [DOI] [PubMed] [Google Scholar]
- 60.Gianino JM, York MM, Paice JA, Shott S. Quality of life: effect of reduced spasticity from intrathecal baclofen. J Neurosci Nurs 1998;30(1):47–54 [DOI] [PubMed] [Google Scholar]
- 61.May LA, Warren S. Measuring quality of life of persons with spinal cord injury: external and structural validity. Spinal Cord 2002;40(7):341–50 [DOI] [PubMed] [Google Scholar]
- 62.Lyons S, Sorenson M. Quality of life in spinal cord injury patients with pressure ulcers. SCI Nurs 2009;26:13–8 [Google Scholar]
- 63.Krause JS, Coker JL, Charlifue S, Whiteneck GG. Health outcomes among American Indians with spinal cord injury. Arch Phys Med Rehabil 2000;81(7):924–31 [DOI] [PubMed] [Google Scholar]
- 64.Harding-Okimoto MB. Pressure ulcers, self-concept and body image in spinal cord injury patients. SCI Nurs 1997;14(4):111–7 [PubMed] [Google Scholar]
- 65.Green BC, Pratt CC, Grigsby TE. Self-concept among persons with long-term spinal cord injury. Arch Phys Med Rehabil 1984;65(12):751–4 [PubMed] [Google Scholar]
- 66.Yetzer EA, Schandler S, Root TL, Turnbaugh K. Self-concept and body image in persons who are spinal cord injured with and without lower limb amputation. SCI Nurs 2003;20(1):18–23 [PubMed] [Google Scholar]
- 67.Roid G, Fitts W. The Tennessee self-concept scale. Los Angeles: Western Psychological Services; 1988 [Google Scholar]
- 68.Hammond SM, O'Rourke MM. A psychometric investigation into the body-cathexis scale. Personality Ind Diff 1984;5(5):603–5 [Google Scholar]
- 69.Taleporos G, McCabe MP. The impact of physical disability on body esteem. Sexuality Disabil 2001;19(4):1573–6717 [Google Scholar]
- 70.Limb M. An examination of the relationships between body image, self-esteem and behaviour in adult clients undergoing limb reconstruction procedures. J Orthop Nurs 2003;8(3):164–70 [Google Scholar]
- 71.Samonds RJ, Cammermeyer M. Perceptions of body image in subjects with multiple sclerosis: a pilot study. J Neurosci Nurs 1989;21(3):190–4 [DOI] [PubMed] [Google Scholar]
- 72.Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965 [Google Scholar]
- 73.Coyle CP, Lesnik-Emas S, Kinney WB. Predicting life satisfaction among adults with spinal cord injuries. Rehabil Psychol 1994;39(2):95–111 [Google Scholar]
- 74.Maslow AH. Toward a psychology of being. New York: Van Nostrand Reinhold; 1968 [Google Scholar]
- 75.Gordon WA, Harasymiw S, Bellile S, Lehman L, Sherman B. The relationship between pressure sores and psychosocial adjustment in persons with spinal cord injury. Rehabil Psychol 1982;27(3):185–91 [Google Scholar]
- 76.Singh R, Singh R, Rohilla RK, Siwach R, Verma V, Kaur K. Surgery for pressure ulcers improves general health and quality of life in patients with spinal cord injury. J Spinal Cord Med 2010;33(4):396–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hauser K, Walsh D. Visual analogue scales and assessment of quality of life in cancer. J Support Oncol 2008;6(6):277–82 [PubMed] [Google Scholar]
- 78.Wood-Dauphinée S, Exner G, Bostanci B, Exner G, Glass C, Jochheim KA, et al. Quality of life in patients with spinal cord injury—basic issues, assessment, and recommendations. Restor Neurol Neurosci 2002;20(3–4):135–49 [PubMed] [Google Scholar]
- 79.Langemo DK, Melland H, Hanson D, Olson B, Hunter S. The lived experience of having a pressure ulcer: a qualitative analysis. Adv Skin Wound 2000;13(5):225–35 [PubMed] [Google Scholar]
- 80.Jackson J, Carlson M, Rubayi S, Scott MD, Atkins MS, Blanche EI, et al. Qualitative study of principles pertaining to lifestyle and pressure ulcer risk in adults with spinal cord injury. Disabil Rehabil 2010;32(7):567–78 [DOI] [PubMed] [Google Scholar]
- 81.Diener E, Suh E. Measuring quality of life: economic, social, and subjective indicators. Soc Indicators Res 1997;40(1):189–216 [Google Scholar]
- 82.Angur MG, Widgery R, Angur SG. Congruence among objective and subjective quality-of-life (QOL) indicators. AJBR. Accessed at: http://ajbr.org/Archives/Congruence%20among%20Objective%20and%20Subjective%20Quality-of-Life%20(QOL. )%20indicators.pdf [accessed 2012 September 4].
- 83.Hicken BL, Putzke JD, Richards JS. Bladder management and quality of life after spinal cord injury. Am J Phys Med Rehabil 2001;80(12):916–22 [DOI] [PubMed] [Google Scholar]
- 84.National Pressure Ulcer Advisory Panel. Pressure Ulcer Stages Revised by NPUAP. NPUAP http://www.npuap.org/pr2.htm . 2007 [accessed 2012 December 8].
- 85.Adams MM, Martin Ginis KA, Hicks AL. The Spinal Cord Injury Spasticity Evaluation Tool: development and evaluation. Arch Phys Med Rehabil 2007;88(9):1185–92 [DOI] [PubMed] [Google Scholar]
- 86.Costa P, Perrouin-Verbe B, Colvez A, Didier J, Marquis P, Marrel A, et al. Quality of life in spinal cord injury patients with urinary difficulties. Development and validation of qualiveen. Eur Urol 2001;39(1):107–13 [DOI] [PubMed] [Google Scholar]
- 87.Krogh K, Christensen P, Sabroe S, Laurberg S. Neurogenic bowel dysfunction score. Spinal Cord 2006;44(10):625–31 [DOI] [PubMed] [Google Scholar]
- 88.Price P, Harding K. Cardiff Wound Impact Schedule: the development of a condition-specific questionnaire to assess health-related quality of life in patients with chronic wounds of the lower limb. Int Wound J 2004;1(1):10–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nussbaum EL, Flett H, Hitzig SL, McGillivray C, Leber D, Morris H, et al. Ultraviolet-C irradiation in the management of pressure ulcers in people with spinal cord injury: A randomized, placebo-controlled trial. Arch Phys Med Rehabil 2013;94(4):650–9 [DOI] [PubMed] [Google Scholar]
- 90.Stroupe KT, Manheim L, Evans CT, Guihan M, Ho C, Li K, et al. Cost of treating pressure ulcers for veterans with spinal cord injury. Top Spinal Cord Inju Rehabil 2011;16(4):62–73 [Google Scholar]
- 91.Noonan VK, Miller WC, Noreau L, SCIRE Research Team A review of instruments assessing participation in persons with spinal cord injury. Spinal Cord 2009;47(6):435–46 [DOI] [PMC free article] [PubMed] [Google Scholar]


