Abstract
Objective. To improve pharmacy and nursing students’ competency in collaborative practice by having them participate in an interprofessional diabetes experience involving social networking.
Design. An existing elective course on diabetes management was modified to include interprofessional content based on Interprofessional Education Collaborative (IPEC) competency domains. Web-based collaborative tools (social networking and video chat) were used to allow nursing and pharmacy students located on 2 different campuses to apply diabetes management content as an interprofessional team.
Assessment. Mixed-method analyses demonstrated an increase in students’ knowledge of the roles and responsibilities of the other profession and developed an understanding of interprofessional communication strategies and their central role in effective teamwork.
Conclusion. Interprofessional content and activities can be effectively integrated into an existing course and offered successfully to students from other professional programs and on remote campuses.
Keywords: interprofessional education, social networking, diabetes, pharmacy students, nursing
INTRODUCTION
The “medical homelessness” experienced by many patients with complex and chronic illnesses is an all too common occurrence.1 Prevention of “medical homelessness” requires a team of healthcare professionals who know how to work together to optimize each member’s skills, which means health professional students must learn and practice collaborative patient care prior to entering practice. Diabetes patients are an excellent example of a population with complex medical needs that require the coordinated efforts of a team of health professionals.
To prepare pharmacists (and other health professionals such as nurses) to effectively contribute to a primary care team devoted to diabetes care, practice opportunities working within a coordinated team should be incorporated within core patient-care courses. Health professions students are busy; the demands of each professional program can be intense and create competing schedules. To expect students from different professional programs to meet face-to-face outside of their classrooms may not be reasonable; educators must consider multiple strategies to connect health professions students, including social networking. Social networking platforms offer a unique space where people can interact in a meaningful manner, even if separated by time and distance.2,3
In this project, we evaluated the feasibility and effectiveness of integrating interprofessional education into an elective advanced diabetes course through the use of an online social networking platform, Ning (www.ning.com), as well as other distance education strategies. We chose Ning because of its focus on group collaboration and it allowed us to control access and membership to the site. The design of this course incorporated a social networking tool for a variety of reasons: educational literature supports the use of asynchronous tools for fostering more complete and diplomatic participation of students; students can interact at any time/place; students can self-construct the interprofessional discussion environment (students created their own rules with regard to posting and self-rated their participation, with instructional team oversight); and students at a distant campus can participate.
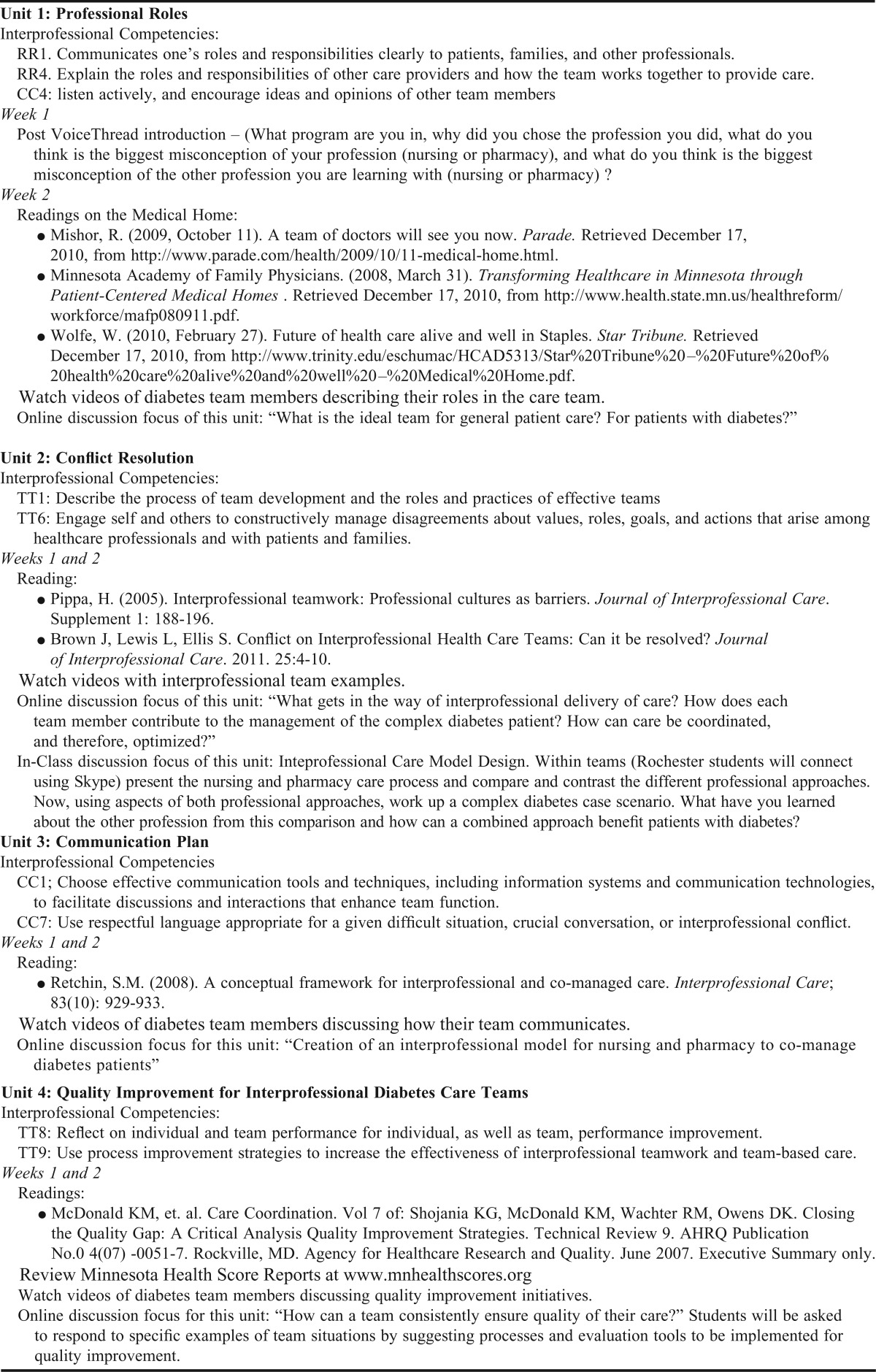
Based on findings from a previous study evaluating the use of social networking for interprofessional education, we used a facilitated pedagogical structure to guide interprofessional awareness and respect among students in this interprofessional diabetes course. For the design of this course, the instructors focused on 3 interprofessional competency domains outlined by the Interprofessional Education Collaborative (IPEC)4: roles and responsibilities, interprofessional communication, and teams and teamwork. The primary research questions we intended to answer were whether pharmacy and nursing students who were learning together: (1) increased their knowledge of roles and responsibilities with respect to the other profession, and (2) developed an understanding of interprofessional communication and its central role in effective teamwork.
DESIGN
The diabetes course was designed to provide students the opportunity to acquire in-depth knowledge of diabetes mellitus through active, hands-on learning in an interprofessional environment. As a required part of this course, students participated in a week-long experience of living with diabetes, during which they gave themselves simulated insulin injections (normal saline) and checked their blood glucose levels 4 times daily. The basic design of this course, prior to becoming an interprofessional course, has been described.5 In addition, students participated in activities primarily within a social networking space centered around interprofessional teams and how a team of nurses and pharmacists can provide optimal care to patients with diabetes.
To evaluate the research questions, students were divided into 9 groups. Each group initially was comprised of 4 pharmacy students and 3 nursing students who interacted for the entire 15-week semester. Groups met “in person” on the first day of class with students located on a remote campus meeting their other group members via interactive television. For the remainder of the semester, the groups worked together on Ning as well as in groups for in-class interprofessional face-to-face sessions (distant students used Skype during these sessions).
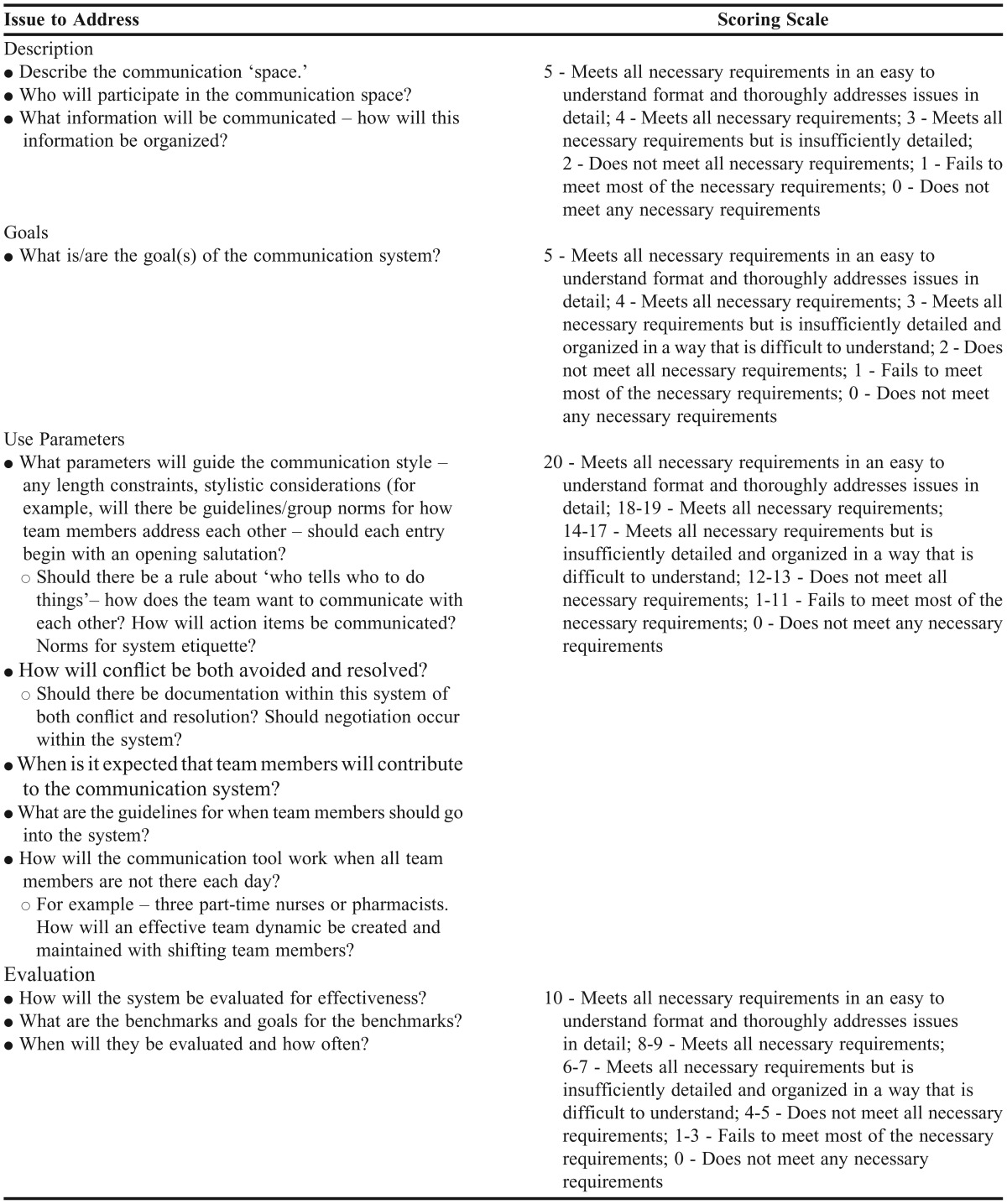
On the first day of class, students were asked to draft their group’s ground rules, which included expected participation levels in the online space, appropriate etiquette rules, and timeliness for completing assignments. Groups created a team name and logo and participated in an interprofessional “ice breaker” game. Four times during the semester students self-scored their participation and adherence to their group’s ground rules on a scale of 1 to 5, and submitted their score and a brief justification of why they deserved the score to the instructor. The course instructors developed the interprofessional content and activities to address the 3 IPEC domains and coordinate with the diabetes content and activities (Appendix 1). As a final team project, groups co-created a communication plan for coordinating and collaborating on the care of diabetes patients in an ambulatory setting (Table 1). During the last class period, groups gave a brief presentation of their plan and how they developed it. This study along with all associated study materials, assessments, and procedures, was deemed exempt from review by the University of Minnesota Institutional Review Board on January 9, 2012.
Table 1.
Grading Rubric for Pharmacy and Nursing Students’ Communication Plan for Coordinating and Collaborating on the Care of Diabetes Patients in an Ambulatory Setting
EVALUATION AND ASSESSMENT
Total final enrollment for this course was 34 pharmacy students (4 third-year and 30 second-year students) and 17 undergraduate nursing students (9 third-year and 8 fourth-year students). Thirty-four pharmacy students and 17 nursing students (14 in Minneapolis and 3 in Rochester) completed the course.
Two interprofessional survey instruments were used in this study: the Interdisciplinary Education Perception Scale (IEPS)6 and the Readiness for Interprofessional Learning Scale (RIPLS).7 Both surveys were administered at baseline (beginning of course) and at the end of the study (following the completion of the course). These tools measure student perceptions and attitudes related to interprofessional collaboration and are the standard found in the interprofessional education literature. Using the guidelines described by Gaddis8 and Dillman, Tortora, and Bowker,9 an additional pre- and post-experience survey instrument was developed to ask students about their experiences in this course. The IEPS, the RIPLS, and the survey items about the course were formatted as one continuous instrument and administered pre- and post-course. Online survey data were aggregated and described. Because of the repeated measures of the RIPLS and IEPS, the pre- and post-course scores were compared using a paired t test, and means were compared to other reports in the literature. No significant differences were noted in the pre- and post-course RIPLS and IEPS scores (p>0.1 for all subgroup pairings).
Almost all students indicated on the pre-course survey that they had experience with a social networking Web site (98%), and all except 2 students were active on at least 1 social networking Web site. Of those students active with a social networking site, 82% stated that they log into a social networking site at least once a day for approximately 30 minutes or less. Most students had taken an online course before (84%) and stated that they agreed or strongly agreed that meaningful learning can occur online (95%). Students were asked to list past participation with interprofessional experience, and 80% were able to list at least 1 past interprofessional course or activity. When students were asked to state their expectations for this interprofessional education social networking experience, most students said they wanted to learn more about the management of diabetes from the perspective of both professions in order to optimize care for patients. There were also many (79%) comments about better understanding the role of the other profession represented in the class, as well as being able to communicate the important role of their own profession. Two students stated that they had no expectations at all. When asked how they would know if their expectations were met, most students stated that gaining some new knowledge about the other profession would be an indicator. A few expanded to say that their expectations would be met if they appreciated the role of the other profession in a clinical setting in a new way because of the knowledge gained from the course.
All students (100%) who completed the course completed the post-experience survey instrument. From the course evaluations, 100% of students stated that the course workload was within what was expected for a 2-credit course. Students were asked to describe their experience using Ning, indicate whether interprofessional education expectations were met in this course, describe how this experience impacted their knowledge of the other profession represented, and describe the role of the “other” profession related to the care of patient with diabetes (this same question was asked on the pre-experience survey instrument).
The success of the social networking tool, Ning, was mixed. Overall, students were fairly split about whether this strategy should be used again (42% agreed or strongly agreed, 58% disagreed or strongly disagreed). When asked to explain the answer given in regard to use of a social networking tool for interprofessional education, the students’ explanations were positive, mixed, or negative. Students who responded positively liked the flexibility to contribute to the conversation outside of class and stated that Ning was easier and more interesting to use than Moodle. Some students in this cohort stated that Ning seemed less academic so the discussion felt more “laidback.” Another theme within the positive comments was the advantage of everyone in the group contributing to the discussion within the Ning site (as this was an expectation) versus in a classroom setting when at times only a few contribute. The comments of students who had mixed feelings about the use of social networking were consistent. These students encouraged the instructors to maintain an out-of-class discussion portion to the course but suggested that they just use Moodle (which was the course learning management system) rather than Ning. Although they liked Ning, they felt its advantages did not overcome the hassle of having to go to 2 different sites (Ning and Moodle) to complete course activities and assignments. The students with negative comments argued strongly against requiring any out-of-class discussion because they believed that interprofessional education must occur face-to-face.
Seventy-seven percent of all students stated that their expectations for the interprofessional component of the course were met. All students who stated their expectations were NOT met were pharmacy students, with the exception of 1 nursing student. Students who stated their expectations were met more often described getting to know the students representing the other professional role better and that learning about another profession within a specific patient context was helpful. These students felt that learning with other health professions students had enhanced their knowledge of and confidence in treating patients with diabetes. These students also stated that they felt better able to work with other health professionals in the care of patients in general and more “competent” to deliver interprofessional care. Those students who felt their needs were not met stated that using the Ning site as the predominant interprofessional discussion space was not effective.
The qualitative analysis consisted of content analysis and discourse analysis to examine if the postings within each group were qualitatively different. Content analysis of both the Ning postings and open-ended survey responses used the Classic Analysis Strategy, a constant comparison-like approach,10 to reveal what participants said within their groups.11 All transcripts of Ning postings and open-ended survey responses were first reviewed for emerging themes; after several passes over the postings and open-ended survey responses, themes were combined when appropriate and compared across groups.
Students who answered positively to the question of whether their expectations were met also had positive responses to the question of how participating in the course impacted their knowledge of the other profession. These students consistently mentioned that they felt much more knowledgeable and skilled at collaborating with students representing the other profession (ie, nursing or pharmacy students). Understanding the other profession’s care plan approach and then collaborating to create a plan for a patient with diabetes solidified the important role of each profession. These students felt confident that they could effectively work with the other profession and understood how to best use each other’s skills/areas of expertise to optimize patient care. All of the negative comments were from pharmacy students and centered on not having enough “real” collaboration within the course and nursing students not contributing enough in the group activities and assignments.
On the entrance and exit survey instruments, we asked students to comment on the roles of the nurse and pharmacist in taking care of patients with diabetes. At the beginning of the course, about a third of students representing each profession responded that they were not really sure what the role of the other profession was. Another third characterized the role superficially and stereotypically, stating that it had something to do with education (pharmacy students commenting on nursing) or medications (nursing students commenting on pharmacy). In the exit survey, overwhelmingly, both nursing and pharmacy students used terms like holistic, whole-person and advocacy to describe the nurse’s role, and phrases like optimizing medication therapy/medication management and ensuring safe and effective medication use to describe the pharmacist’s role.
DISCUSSION
This project evaluated the feasibility and effectiveness of integrating interprofessional education into an advanced diabetes content course using the online social networking platform, Ning, as well as other distance education strategies. The social networking strategy was important for connecting students from a remote campus and also allowing students to extend classroom interaction and foster interaction across professional programs. In a previous study evaluating social networking for interprofessional education, students were positive about the integration of a social networking tool such as Ning and recommended it be used within a core patient care course. Although the social networking tool was a feasible option, the student response was mixed. As expected and documented in many other places in the interprofessional literature, it is difficult to demonstrate significant increases in RIPLS or IEPS scores among highly motivated, self-selected students who enter interprofessional experiences with positive attitudes regarding interprofessional collaboration. Fortunately, attitudes did not decline as a result of this experience, as has been documented in other examples. Nonetheless, qualitative data demonstrates the success of integrating interprofessional educational content and pedagogy. Students demonstrated increased knowledge of roles and responsibilities with respect to the other profession, and they developed an understanding of interprofessional communication strategies and its central role in effective teamwork. In the exit survey, all students were able to characterize the role of the other profession and, interestingly, the phrasing used by pharmacy and nursing students merged. It is as though they began to take on a common language.
The authors and instructors attribute the in-class activity of comparing professional care processes as marking a critical moment in the interprofessional educational success for this course and redesign. During this class activity the nursing and pharmacy students seemed to have a collective understanding and to finally grasp the important differences and similarities of the 2 roles, and therefore the benefits of an interprofessional collaboration between the 2 professions.
The placement of the diabetes activity at the end of the interprofessional unit 2 on professional roles and conflict resolution and just prior to unit 3 on creating a communication plan, also may have been a reason for the course’s success. At this point in the course, students had been grappling with the concepts of interprofessional collaboration for some time and were comfortable within their interprofessional small groups. The authors and instructors believe that if the activity had been placed earlier in the semester it would not have had the same impact, and also argue that the integration of interprofessional activities within a core clinical context was essential to the overall success. In the original project design, a focus group session at the end of the semester was planned. With many nursing students graduating at the end of the semester and pharmacy students transitioning into other summer activities, the instructional team was unsuccessful with getting any volunteers to participate in the follow-up focus group session.
The course has been revised to reflect what was learned from this project. Although Ning was not used in the subsequent semester, students on the distant campus were still connected to small groups through Skype (Microsoft Redmond, WA) and the course content and schedule were similar. All classes were conducted face to face, so out-of-class interprofessional discussions were not required. Future evaluation of these changes is planned.
The original enrollment numbers for the class were 39 pharmacy students and 29 nursing students. Initial assigned groups typically had 4 pharmacy students and 3 nursing students. At approximately the 3-week point, a number of junior and senior nursing students dropped the course. By the middle of the semester, most groups had only 1 or 2 nursing students. The most common explanation given by the nursing students for dropping the course was concern regarding managing the time commitment with their assigned clinical experiences. The authors and instructors have tried to understand and address the large number of nursing students who withdraw from this course. The nursing faculty member on the instructional team felt that the quiz structure used at the beginning of the classes may have intimidated the nursing students, who were already busy with finishing up clinical experiences for graduation. The authors and instructors have addressed this potential barrier by explaining more extensively the role of the quizzes at the beginning of the semester and minimizing the point allocation, with the hope that we can retain more nursing students. The end of the semester focus group was also unsuccessful, and while it would have been helpful to get additional feedback from students, we did have 100% completion rates for the postcourse survey instrument and received a lot of helpful information from students through both the closed and open-ended questions.
SUMMARY
Integrating interprofessional educational content and activities into a diabetes management course was feasible and effective in achieving both interprofessional and clinical-learning outcomes. Using IPEC competency domains to guide the interprofessional content development was an important educational design strategy to ensure purposeful integration of interprofessional concepts within the clinical course context. The use of Web-based collaborative tools (Ning and Skype) was also feasible and allowed students at a remote campus to participate but with mixed educational results. It is important to continue to leverage evolving and improving learning technologies to connect interprofessional students to facilitate learning about, from, and with each other.
Appendix 1.
REFERENCES
- 1.Colwill JM. A case of ‘medical homelessness.’. Health Aff. 2010;29(5):1067–1070. doi: 10.1377/hlthaff.2009.0224. [DOI] [PubMed] [Google Scholar]
- 2.Shen D, Nuankhieo P, Huang X, Amelung C, Laffey J. Using social network analysis to understand sense of community in an online learning environment. J Educ Comput Res. 2008;39(1):17–36. [Google Scholar]
- 3.Zhu E. Interaction and cognitive engagement: an analysis of four asynchronous online discussions. Instr Sci. 2006;34(6):451–480. [Google Scholar]
- 4.Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice. report of an expert panel; Washington, DC: 2011. [Google Scholar]
- 5.Westberg SM, Bumgardner MA, Brown MC, Frueh J. Impact of an elective diabetes course on student pharmacists’ skills and attitudes. Am J Pharm Educ. 2010;(3):74. Article 49. doi: 10.5688/aj740349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McFadyen AK, Maclaren WM, Webster VS. The interdisciplinary education perception scale (IEPS): an alternative remodeled sub-scale structure and its reliability. J Interprof Care. 2007;21(4):433–443. doi: 10.1080/13561820701352531. [DOI] [PubMed] [Google Scholar]
- 7.McFadyen AK, Webster V, Strachan K, Figgins E, Brown H, McKechnie J. The Readiness for interprofessional learning scale: a possible more stable sub-scale model for the original version of RIPLS. J Interprof Care. 2005;19(6):595–603. doi: 10.1080/13561820500430157. [DOI] [PubMed] [Google Scholar]
- 8.Gaddis SE. How to design online surveys. Train Dev. 1998;52(6):67–71. [Google Scholar]
- 9.Dillman DA, Tortora RD, Bowker D. Principles for constructing web surveys (Technical Report 98-50) Pullman, Washington: Social and Economic Sciences Research Center, Washington State University; 1998. http://survey.sesrc.wsu.edu/dillman/papers/websurveyppr.pdf. Accessed April 29, 2009.
- 10.Krueger RA, Casey MA. Focus Groups: A Practical Guide for Applied Research, 4th ed. Thousand Oaks, CA: Sage Publishing, Inc; 2009. [Google Scholar]
- 11.Paulus TM. Challenge or connect? Dialogue in online learning environments. J Comput High Educ. 2006;18(1):3–29. [Google Scholar]


