Abstract
Background: Collecting a 24-h urine sample is recommended for monitoring the mean population sodium intake, but implementation can be difficult.
Objective: The objective was to assess the validity of published equations by using spot urinary sodium concentrations to predict 24-h sodium excretion.
Design: This was a cross-sectional study, conducted from June to August 2011 in metropolitan Washington, DC, of 407 adults aged 18–39 y, 48% black, who collected each urine void in a separate container for 24 h. Four timed voids (morning, afternoon, evening, and overnight) were selected from each 24-h collection. Published equations were used to predict 24-h sodium excretion with spot urine by specimen timing and race-sex subgroups. We examined mean differences with measured 24-h sodium excretion (bias) and individual differences with the use of Bland-Altman plots.
Results: Across equations and specimens, mean bias in predicting 24-h sodium excretion for all participants ranged from −267 to 1300 mg (Kawasaki equation). Bias was least with International Cooperative Study on Salt, Other Factors, and Blood Pressure (INTERSALT) equations with morning (−165 mg; 95% CI: −295, 36 mg), afternoon (−90 mg; −208, 28 mg), and evening (−120 mg; −230, −11 mg) specimens. With overnight specimens, mean bias was least when the Tanaka (−23 mg; 95% CI: −141, 95 mg) or Mage (−145 mg; −314, 25 mg) equations were used but was statistically significant when using the Tanaka equations among females (216 to 243 mg) and the Mage equations among races other than black (−554 to −372 mg). Significant over- and underprediction occurred across individual sodium excretion concentrations.
Conclusions: Using a single spot urine, INTERSALT equations may provide the least biased information about population mean sodium intakes among young US adults. None of the equations evaluated provided unbiased estimates of individual 24-h sodium excretion. This trial was registered at clinicaltrials.gov as NCT01631240.
INTRODUCTION
Excess sodium intake is projected to cause an estimated 50,000 heart attacks and 30,000 strokes in the United States every year (1). Accurate monitoring of intake is essential to support public health efforts to reduce excess intakes (2–5). Twenty-four–hour urinary sodium excretion is recommended for monitoring sodium intake (2, 6). When collection is complete and sodium intake is held constant for several days, 24-h urinary sodium excretion reflects ∼90% of sodium intake (7–9) on that day. In adults, the half-life required to establish homeostasis in sodium excretion is ∼24 h (10–12). Because participation in a 24-h urine collection can be low and some voids missed or spilled, according to the Institute of Medicine (2), “Research is needed to develop a marker of sodium intake other than 24-hour urine collection that is reliable, economical, and easy to administer in population surveys.”
Collecting a spot or casual urine specimen is feasible and low cost but is currently not recommended for monitoring sodium intake because of the large diurnal variation in sodium excretion (2, 6, 13–18). This excretion pattern is reversed for individuals with hypertension, and diurnal variation may be less among blacks or African Americans (14–19). Despite these issues, predictive equations were developed in previous studies and used with spot urine specimens to estimate population mean and individual 24-h urinary sodium excretion (20–30). The 2 major approaches for developing these equations are as follows: 1) direct regression of sodium concentration from spot urine specimens on 24-h urinary sodium excretion (20, 21) and 2) multiplication of the spot urinary sodium-to-creatinine ratio by the predicted or actual 24-h urinary creatinine concentration (22, 23, 29). Some equations (22), but not others (20, 21, 23), were developed to estimate 24-h urinary sodium excretion based on urine collected at a specific time of day. The most frequently used prediction equations were developed in Asian populations (22, 23, 25–28), and their applicability to US adults is unclear. Newly published equations developed among North American and European adults appear promising for monitoring population mean 24-h sodium excretion, but are not yet validated in an external sample (20). Furthermore, information is limited on the validity of predicted 24-h urinary sodium excretion among African Americans and by the timing of spot urine collection.
Current and past NHANES include a spot urine specimen collected in person (31) used to estimate 24-h excretion of pesticides and chemicals (32, 33), but not sodium. Starting in 2009, a urine specimen was collected at home after the longest period of sleep (34). To inform the use of a single spot urine specimen to assess sodium intake in NHANES and other surveys, here we assessed the validity of published equations for predicting 24-h sodium excretion at a population level and at an individual level by timing of spot urine collection among adults aged 18–39 y who participated in a urine calibration study (35), among all participants and within sex and race subgroups.
SUBJECTS AND METHODS
During June–August 2011, 500 volunteers aged 18–39 y living in the Washington, DC, metropolitan area underwent a screening process to determine their willingness and eligibility to participate in a study requiring the collection of urine over a 24-h period. Of them, 481 were scheduled for an initial visit; 441 completed the visit and were enrolled in the study. The study design, methods, and descriptive data are presented in detail elsewhere (35). Briefly, participant recruitment was stratified by sex and race, and questions were asked in an attempt to recruit an enhanced sample of 50 participants with a low and 50 with a high sodium intake. Pregnant women or women trying to get pregnant, persons who reported taking loop diuretics, persons with self-reported chronic kidney disease, or persons with reported new or modified hypertension treatment in the past 2 wk were excluded from participation.
Data collection for all participants relevant to this analysis, included questions related to sociodemographic characteristics, use of hypertensive medications, measured weight and height, and a fractional 24-h urine collection (35). For the fractional 24-h urine collection, each void was collected and stored in a separate container, and the participant recorded the time of the collection. Participants returned the urine collection on the day of completion. Urine was kept cold (with ice packs or in the refrigerator) until portioned into aliquots. One-third of the participants were invited to collect a second fractional 24-h urine specimen 4–11 d later. In this study we included 407 participants who completed one 24-h urine collection. Completion was defined as having urinated ≥500 mL as measured by a technician, a recorded collection of ≥20 h, and reports of spilling urine or missing a void no more than once in 24 h (35). Seven persons missed (n = 6) or spilled (n = 1) 1 void in the initial 24-h urine collection, but were kept in the sample because their urine volumes and 24-h sodium and creatinine excretions did not differ from those of the remaining participants, and their exclusion did not affect the results (35). Collections from female participants were excluded if they were menstruating. Questions regarding spilling urine, missing a void, or menstruation were determined via standard questions. The study protocol was approved by the National Center for Health Statistics, CDC, ethics review board, and written informed consent was obtained from all participants.
The timing of urine specimens was as follows: morning (the second void on rising in the morning), 0830–1230; afternoon, 1231–1730; evening, 1731–2359; and overnight (the first void after the longest period of sleep), 0400–1200 the next morning.
A composite 24-h urine specimen was prepared by taking a proportional aliquot from each void (fractional specimen). In addition, 4 spot urine specimens were selected in accordance with the method of urine collection currently used in NHANES (31, 34): the first specimen collected in the morning after discarding the first void (0830–1230), the afternoon (1231–1730), and evening (1731–2359) and the overnight specimen, which was the first void collected the next morning after the longest period of sleep (0400–1200). A 1-mL aliquot was taken from the composite 24-h urine sample and each of the 4 spot urine specimens. All vials were shipped frozen on dry ice within 7 d of collection to CDC's National Center for Environmental Health for analysis. For analysis of sodium and other electrolytes (potassium and chloride), ion-selective electrodes (ISEs) and the Cobas ISE/Na+, K+, Cl− assay were used on the Hitachi Modular P clinical analyzer (Roche Diagnostics) (36). For analysis of urine creatinine, the Roche Creatinine Plus enzymatic assay was used on the Hitachi Modular P clinical analyzer (37). Each analytic run included 2 levels of urine quality-control samples measured in duplicate at the beginning and end of the run bracketing the study samples. The between-run measurement imprecision was ≤3% for each analyte and is reported in detail elsewhere (35).
Participants who self-identified their race by a “yes” response to the following question during screening, “Do you consider yourself to be Black or African American?”, were grouped as “black” in the analyses. Participants who answered “no” were grouped into “other races.” Information on the race or ethnicity of this group was not collected (35) because previous studies do not suggest variations in the diurnal pattern of urine electrolyte excretion within ethnic groups other than African Americans (15, 38). BMI was calculated as weight (in kg) divided by height (in m) squared.
Estimation of 24-h sodium excretion from spot specimens
The volume of the measured 24-h urine sample was adjusted for self-reported collection time as follows: (total volume collected/self-reported collection time) × 24. The total amount of sodium excreted in each spot urine specimen (measured spot urinary sodium) and 24-h urine specimen (measured 24-h sodium excretion) was calculated by multiplying the sodium concentration by the corresponding volume of the sample. In addition, we used 4 previously published equations to predicted 24-h urinary sodium excretion from spot urinary sodium concentrations (Table 1): 1 direct approach using the Western INTERSALT (International Cooperative Study on Salt, Other Factors, and Blood Pressure) samples (20) and 3 indirect approaches based on spot urinary sodium-to-creatinine ratios multiplied by predicted 24-h creatinine excretion [Tanaka (23), Kawasaki (22), and Mage (32, 33)]. The Tanaka equation was based on the Japanese INTERSALT population, the Kawasaki equation also was developed in a Japanese population, but has been applied to Western populations (25), and the Mage equation was used to estimate urine pesticide and chemical exposure with NHANES urine specimens. Prediction of 24-h creatinine concentrations varied in these equations. All of these 3 equations (Tanaka, Kawasaki, and Mage) took age, weight, and height into account in their prediction of creatinine. However, only the Kawasaki and Mage equations have sex-specific predictions of creatinine. With Mage, we used a creatinine correction for differences in muscle mass by race (33). Because, the Kawasaki equation was specifically developed for use with a second morning urine specimen collected after the first void in the morning, we only evaluated its use with our “morning” specimen.
TABLE 1.
Predictive equations for 24-h sodium excretion based on single spot urinary sodium concentrations1
| Equation | Age range | Low to high group mean observed 24-h sodium excretion | Predictive equation for 24-h sodium excretion | Reference |
| y | mg | mg | ||
| Developed in North American and European populations | ||||
| INTERSALT | ||||
| Male (n = 2841) | 20–59 | 3386–55202 | = 23 × {25.46 + [0.46 × spot Na (mmol/L)] – [2.75 × spot Cr (mmol/L)] − [0.13 × spot K (mmol/L)] + [4.10 × BMI (kg/m2)] + [0.26 × age (y)]} | (20) |
| Female (n = 2852) | 20–59 | 2709–38523 | = 23 × {5.07 + [0.34 × spot Na (mmol/L)] − [2.16 × spot Cr (mmol/L)] − [0.09 × spot K (mmol/L)] + [2.39 × BMI (kg/m2)] + [2.35 × age (y)] – [0.03 × age2 (y)]} | (20) |
| Developed in Japanese populations | ||||
| Tanaka | ||||
| Male and female (n = 591) | 20–59 | 3337–51504 | = 23 × (21.98 × XNa0.392), where XNa = [spot Na (mmol/L)/spot creatinine (mg/dL) × 10] × [Pr24hCr (mg/d)]5 | (23) |
| Kawasaki | ||||
| Male and female (n = 159) | 20–79 | 4287–53506 | = 23 × (16.3 × XNa0.5), where XNa = [spot Na (mmol/L)/spot Cr (mg/dL) × 10] × [Pr24hCr (mg/d)]7 | (22) |
| Theoretical equation developed for use with NHANES | ||||
| Mage | ||||
| Male and female8 | NA | NA | = {[23 × spot Na (mmol/L)]/[spot Cr (mg/dL) × 10]} × [Pr24hCr (mg/d)]9 | (32, 33) |
Cr, creatinine; INTERSALT, International Cooperative Study on Salt and Blood Pressure; spot, spot urine; NA, not applicable; Pr24hCr, predicted 24-h urine creatinine excretion.
Low (Charleroi, Belgium) to high (Krakow, Poland) mean sodium intake among women enrolled in the INTERSALT study in Western populations.
Low (Cottbus, Germany) to high (Bassiano, Italy) mean sodium intake among men enrolled in the INTERSALT study in Western populations.
Low (among women in Osaka, Japan) to high (among men in Toyama, Japan) mean sodium content in persons enrolled in the INTERSALT study in Japan.
Pr24hCr (mg/d) = [−2.04 × age (y)] + [14.89 × weight (kg)] + [16.14 × height (cm)] − 2244.45.
Low (women) to high (men) mean sodium intake among persons living in Japan (location not specified).
Equation for predicted 24-h urine creatinine excretion developed in a separate study of 256 male and 231 female participants and validated in 20 male and 27 female Japanese and foreign (including 16 American) subjects (39). Pr24hCr (mg/d) for men = [−12.63 × age (y)] + [15.12 × weight (kg)] + [7.39 × height (cm)] - 79.9; Pr24hCr (mg/d) for women = [−4.72 × age (y)] + [8.58 × weight (kg)] + [5.09 × height (cm)] − 74.5.
The Mage equation was developed to predict urine pesticide and chemical exposure with NHANES urine specimens and was not calibrated or validated against measured 24-h urine excretion.
Equation for predicted 24-h urine creatinine excretion developed in a separate study of 249 men in Canada (40) with corrections based on the relative amounts of fat and muscle mass in women and in later publications (32, 33) on differences in muscle mass by race (black compared with other) and BMI (20, 21): Pr24hCr (mg/d) for men = 0.00179 × [140 − age (y)] × [weight (kg)1.5 × height (cm)0.5] × [1 + 0.18 × A × [1.366–0.0159 × BMI (kg/m2)]. Pr24hCr (mg/d) for women = 0.00163 × [140 − age (y)] × [weight (kg)1.5 × height (cm)0.5] × [1 + 0.18 × A × [1.429–0.0198 × BMI (kg/m2)], where A is African American or black race = 1, other race = 0.
Statistical analysis
First we examined the means and SDs for measured 24-h urinary sodium excretion and predicted 24-h urinary sodium excretion using each of the 4 predictive equations with each of the 4 single spot urine collections among all participants and among 4 race and sex subgroups (black men, black women, other race men, and other race women). Because not all participants voided during each of the 4 time periods examined, we predicted mean measured 24-h urinary sodium excretion based on the same sample of participants who voided during the specified time period (eg, morning). To evaluate whether a spot urine collection can be used with predictive equations to estimate population mean 24-h urinary sodium excretion measured on the same day, we examined bias between predicted and measured 24-h urine collections for each of the 4 published equations (INTERSALT, Tanaka, Kawasaki, and Mage) by the timing (morning, afternoon, evening, and overnight) of spot urine collections (except for the Kawasaki equation, which was only evaluated with the morning sample) for all participants and also among race and sex subgroups.
We evaluated the group mean bias in predicted 24-h urine excretion by calculating the difference (predicted – measured) in 24-h urine excretion for each participant and calculating the mean of these differences. Paired t tests were used to assess the statistical significance of differences in predicted-measured 24-h excretion. The 95% CIs were calculated as ± 1.96 × SE of the mean differences.
Because the distribution of the individual biases (predicted – measured) were somewhat skewed, to evaluate the individual differences over the distribution of 24-h sodium excretion, we also calculated the mean and individual relative bias from Bland-Altman plots (41, 42). The Bland-Altman relative bias is the individual difference between the predicted and measured sodium excretion divided by the mean of the predicted and measured excretions. We examined whether individual bias differed across the range of 24-h urinary sodium excretion by plotting the relative bias for each individual against the mean of the predicted and measured for that individual and determined the 95% limits of agreement (relative bias ± 1.96 × SD). We also calculated the Spearman correlation coefficients to examine the relation between individual measured 24-h urinary sodium excretion and individual predicted 24-h urine excretion for the total sample and by race-sex subgroup.
To address potential bias related to potential incomplete 24-h urine collection, we replicated our analyses 1) after excluding individuals who were missing one void and 2) after excluding individuals with potential incomplete urine samples. For 2), we used an alternative marker of completeness of urine collection (43–47), measured-to-expected 24-h urine creatinine ratio excluding participants with a 24-h urine creatinine ratio <0.6 based on equations for expected (predicted) creatinine by using age, weight, height, and race (32). To address potential bias due to inclusion of individuals with hypertension, we also replicated our analyses excluding participants who reported that they had ever been told by a doctor or other health professional that they had hypertension (high blood pressure) or reported currently taking one or more antihypertensive medications. All the statistical analyses were conducted by using SAS version 9.3 (SAS Institute). Statistical significance was defined as P < 0.05. No adjustment was made for multiple comparisons.
RESULTS
Mean measured and predicted 24-h urinary sodium excretions
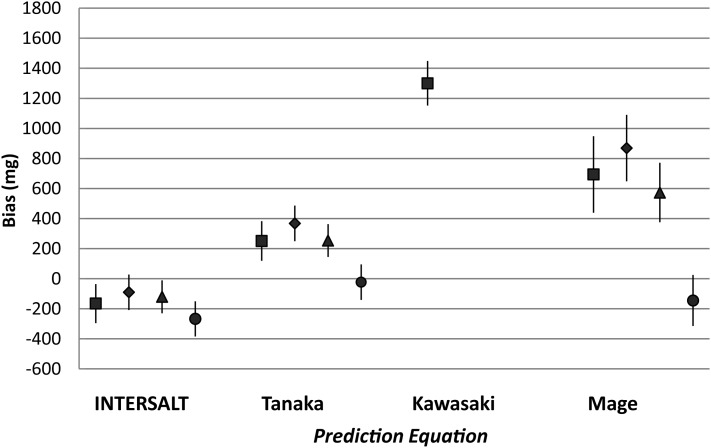
Not all participants voided urine during each time period. Mean predicted 24-h urinary sodium excretion varied by prediction equation, the timing of the spot urine collection, race, and sex (Table 2). Mean biases (predicted minus observed 24-h sodium excretion) with the INTERSALT equations were −165 mg (95% CI: −295, −36 mg) with the morning specimen, −90 mg (95% CI: −208, 28 mg) with the afternoon specimen, −120 mg (95% CI: −230, −11 mg) with the evening specimen (Figure 1), and −267 (−384, −151 mg) with the overnight specimen. With the Tanaka equations, the mean bias was small and not statistically significant with the overnight specimen (−23 mg; 95% CI: −141, 95 mg), but positive and statistically significant with the morning (251 mg), afternoon (368 mg), and evening (255 mg) specimens. Using Kawasaki equations with the morning specimen, mean bias was 1300 mg (95% CI: 1152, 1300 mg) (Table 2 and Figure 1). With the Mage equations, mean bias was not statistically significant with overnight specimens (−145 mg; 95% CI: −314, 25 mg), but was positive and statistically significant with the morning (693 mg), afternoon (869 mg), and evening (574 mg) specimens.
TABLE 2.
Measured and predicted 24-h urinary sodium excretion by population subgroup and the timing of spot urine collection in adults aged 18–39 y1
| Predicted 24-h urinary sodium excretion |
||||||
| No. of subjects | Measured 24-h sodium excretion | INTERSALT2 | Tanaka3 | Kawasaki4 | Mage5 | |
| mg/d | mg/d | mg/d | mg/d | mg/d | ||
| All | ||||||
| Morning | 339 | 3323 ± 14376 | 3157 ± 8917 | 3574 ± 8937 | 4623 ± 14717 | 4016 ± 27957 |
| Afternoon | 389 | 3287 ± 1408 | 3197 ± 824 | 3655 ± 8707 | NA8 | 4156 ± 27177 |
| Evening | 402 | 3298 ± 1399 | 3178 ± 8467 | 3553 ± 8207 | NA8 | 3872 ± 25307 |
| Overnight | 406 | 3295 ± 1400 | 3028 ± 8097 | 3272 ± 779 | NA8 | 3150 ± 2002 |
| Black men | ||||||
| Morning | 76 | 3536 ± 1608 | 3569 ± 1131 | 3554 ± 899 | 4943 ± 15367 | 4723 ± 33827 |
| Afternoon | 85 | 3508 ± 1640 | 3630 ± 1029 | 3584 ± 864 | NA8 | 4748 ± 30207 |
| Evening | 88 | 3529 ± 1617 | 3616 ± 1058 | 3543 ± 914 | NA8 | 4686 ± 33917 |
| Overnight | 89 | 3524 ± 1608 | 3411 ± 952 | 3254 ± 724 | NA8 | 3664 ± 2247 |
| Black women | ||||||
| Morning | 90 | 3195 ± 1344 | 3010 ± 642 | 3655 ± 8197 | 4347 ± 11697 | 4113 ± 24727 |
| Afternoon | 102 | 3219 ± 1331 | 3030 ± 712 | 3655 ± 9017 | NA8 | 4142 ± 27657 |
| Evening | 107 | 3177 ± 1317 | 2917 ± 6887 | 3517 ± 7957 | NA8 | 3725 ± 22577 |
| Overnight | 107 | 3177 ± 1317 | 2884 ± 657 | 3420 ± 7677 | NA8 | 3407 ± 1940 |
| Other men | ||||||
| Morning | 77 | 3600 ± 1514 | 3433 ± 843 | 3598 ± 932 | 5111 ± 16417 | 4169 ± 28857 |
| Afternoon | 90 | 3529 ± 1430 | 3432 ± 738 | 3588 ± 794 | NA8 | 4013 ± 25527 |
| Evening | 94 | 3559 ± 1427 | 3494 ± 784 | 3593 ± 788 | NA8 | 3999 ± 23697 |
| Overnight | 97 | 3555 ± 1427 | 3269 ± 7537 | 3185 ± 7337 | NA8 | 3000 ± 18187 |
| Other women | ||||||
| Morning | 96 | 3051 ± 1259 | 2747 ± 6877 | 3494 ± 9307 | 4236 ± 13787 | 3243 ± 2311 |
| Afternoon | 112 | 2986 ± 1207 | 2831 ± 571 | 3761 ± 9067 | NA8 | 3834 ± 25187 |
| Evening | 113 | 3017 ± 1206 | 2822 ± 5557 | 3560 ± 8027 | NA8 | 3271 ± 1892 |
| Overnight | 113 | 3004 ± 1213 | 2656 ± 6617 | 3220 ± 8567 | NA8 | 2632 ± 18877 |
All values are means ± SDs of measured 24-h urinary sodium excretion and or predicted 24-h urinary sodium excretion based on 1 of the 4 estimation equations (in single spot urine specimens): INTERSALT, Tanaka, Kawasaki, and Mage. The timing of urine specimens was as follows: morning (the second void on rising in the morning), 0830–1230; afternoon, 1231–1730; evening, 1731–2359; and overnight (the first void after the longest period of sleep), 0400–1200 the next morning. INTERSALT, International Cooperative Study on Salt and Blood Pressure.
Reference 20. For men: predicted 24-h urinary sodium excretion (mg/d) = 23 × {25.46 + [0.46 × timed-spot sodium concentration (mmol/L)] − [2.75 × timed-spot creatinine concentration (mmol/L)] − [0.13 × timed-spot potassium concentration (mmol/L)] + [4.10 × BMI (kg/m2)] + [0.26 × age (y)]}. For women: predicted 24-h urinary sodium excretion (mg/d) = 23 × {5.07 + [0.34 × timed-spot sodium concentration (mmol/L)] − [2.16 × timed-spot creatinine concentration (mmol/L)] − [0.09 × timed-spot potassium concentration (mmol/L)] + [2.39 × BMI (kg/m2)] + [2.35 × age (y)] – [0.03× age2 (y)]}.
Reference 23. Predicted 24-h urinary sodium excretion (mg/d) = 23 × (21.98 × XNa0.392), where XNa = [spot sodium concentration (mmol/L)/spot creatinine concentration (mg/dL) × 10] × [predicted 24-h creatinine (mg/d)]. Predicted 24-h creatinine (mg/d) = [−2.04 × age (y)] + [14.89 × weight (kg)] + [16.14 × height (cm)] − 2244.45.
Reference 22. Predicted 24-h urinary sodium excretion (mg/d) = 23 × (16.3 × XNa0.5). For men: predicted 24-h creatinine (mg/d) = [−12.63 × age (y)] + [15.12 × weight (kg)] + [7.39 × height (cm)] − 79.9. For women: predicted 24-h creatinine (mg/d) = [−4.72 × age (y)] + [8.58 × weight (kg)] + [5.09 × height (cm)] − 74.5.
References 32 and 33. Predicted 24-h sodium excretion (mg/d) = {[23 × spot sodium concentration (mmol/L)]/[spot creatinine concentration (mg/dL) × 10]} × [predicted 24-h creatinine (mg/d)]. For men: predicted 24-h creatinine (mg/d) = 0.00179 × [140 − age (y)] × [weight1.5 (kg) × height0.5 (cm)] × [1 + 0.18 × (black = 1, non-black = 0)] × [1.366–0.0159 × BMI (kg/m2)]. For women: predicted 24-h creatinine (mg/d) = 0.00163 × [140 − age (y)] × [weight1.5 (kg) × height0.5 (cm)] × [1 + 0.18 × (black = 1, nonblack = 0)] × [1.429–0.0198 × BMI (kg/m2)].
The mean measured sodium excretion within each race-sex group differs slightly because of the inclusion of only those participants who had a urine sample during the same time period.
Significantly different from measured 24-h urinary sodium excretion, P < 0.05 (paired t test).
Not applicable because the Kawasaki equation was developed to estimate 24-h urinary sodium excretion based on the second morning void only.
FIGURE 1.
Mean bias in predicted minus measured 24-h urinary sodium excretion based on the same day by prediction equation and by timing of the spot urine collection in adults aged 18–39 y. The mean bias in predicted 24-h sodium excretion by using each equation is shown for a single urine specimen collected in the morning (▪), in the afternoon (◆), in the evening (▴), and overnight (•). The 95% CIs for the mean bias are shown by the vertical lines surrounding each mean. INTERSALT, International Cooperative Study on Salt and Blood Pressure.
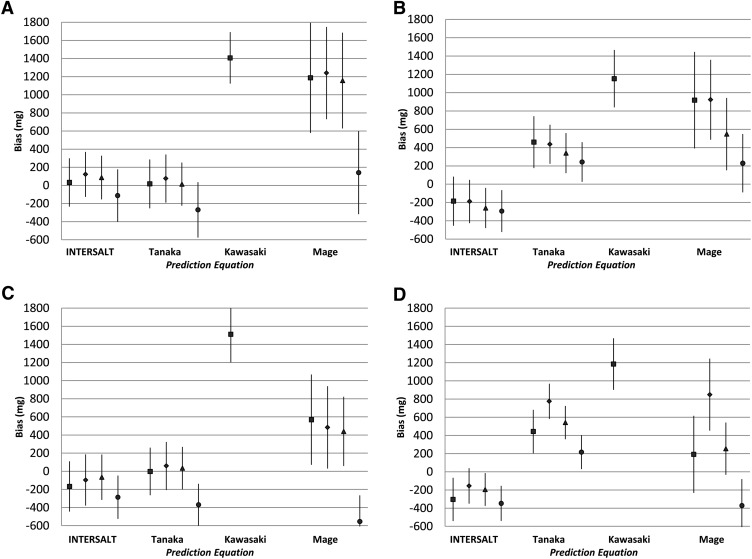
Within race and sex subgroups, mean bias was not significant and of similar magnitude when the INTERSALT (<±200 mg) equations were used with the morning, afternoon, or evening specimen, with a few exceptions (Table 2). The mean bias when the INTERSALT equations were used with the evening spot urine specimens from black women was −260 mg (95% CI: −479, −41 mg) and with the morning specimens in other race women was −304 mg (95% CI: −542, −66 mg) (Table 2, Figure 2). In women, the mean bias when the Tanaka equation was used with the overnight specimen was 243 mg (95% CI: 26, 459 mg) for blacks and 216 mg (95% CI: 30, 402 mg) for other races (Table 2, Figure 2). In contrast, the mean bias when the Tanaka equation was used with the overnight specimen was in the opposite direction among men and statistically significant among other race men (−370 mg; 95% CI: −601, −138 mg) (Table 2, Figure 2). Within race and sex subgroups, mean biases were in the same direction and of similar magnitude when the Kawasaki equations (>1000 mg) were used with morning specimens (Table 2, Figure 2). In races other than black, the mean bias when the Mage equation was used with the overnight specimen was −555 mg (95% CI: −843, −265 mg) for men and −372 mg (95% CI: −664, −81 mg) for women (Table 2, Figure 2), but among black men and women was positive, although not statistically significant.
FIGURE 2.
Mean bias in predicted minus measured 24-h urinary sodium excretion based on the same day by prediction equation and by timing of the spot urine collection in adults aged 18–39 y within the following race-sex subgroups: black men (A), black women (B), other race men (C), and other race women (D). The mean bias in predicted 24-h sodium excretion by using each equation is shown for a single urine specimen collected in the morning (▪), in the afternoon (◆), in the evening (▴), and overnight (•). The 95% CIs of the mean bias are shown by the vertical lines surrounding each mean. Among other race men, the lower limit of the 95% CI of the mean bias in predicted 24-h sodium excretion with the use of Mage equations with overnight specimens was −843 mg. INTERSALT, International Cooperative Study on Salt and Blood Pressure.
Relative individual differences in predicted and measured 24-h urinary sodium excretion
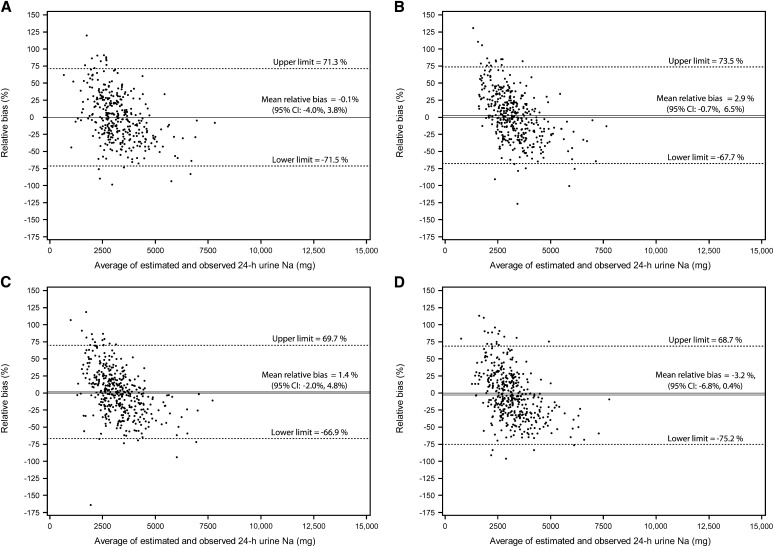
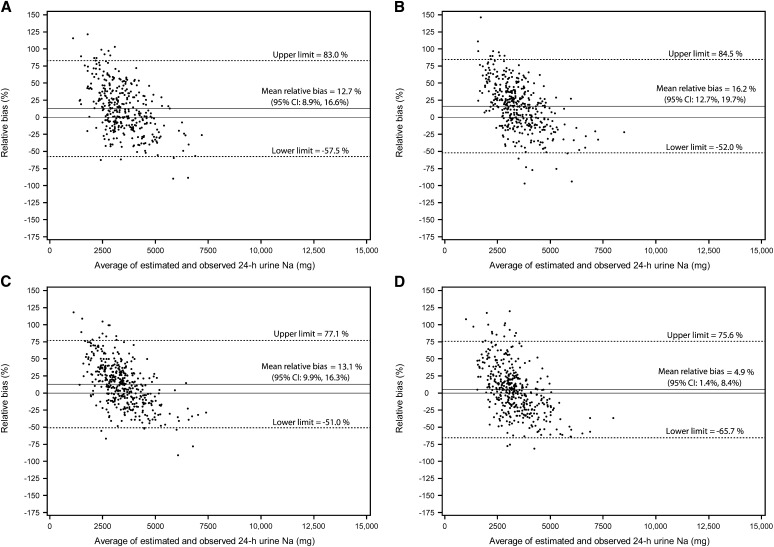
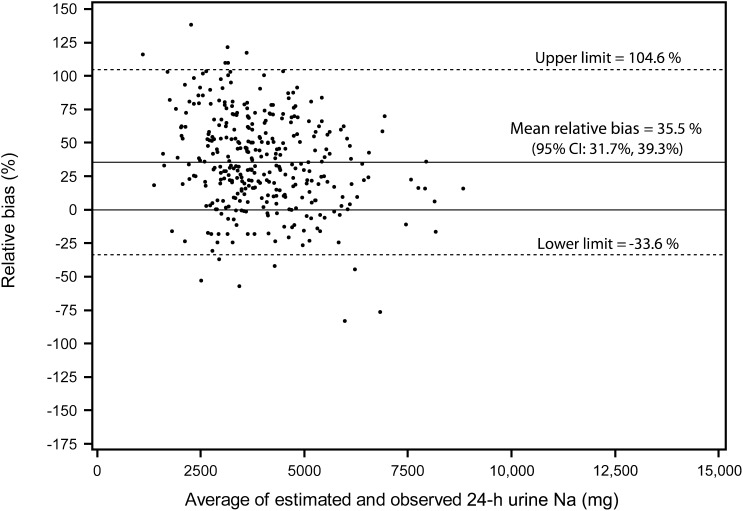
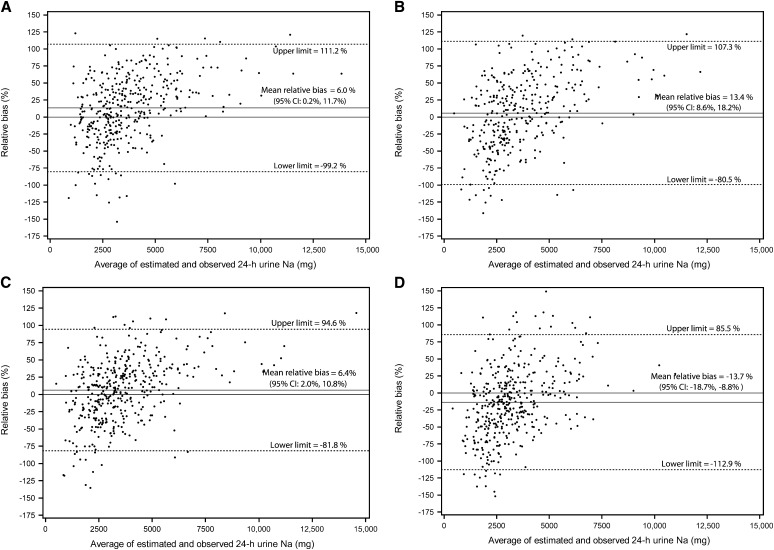
For individuals, the difference in predicted and measured 24-h urine excretions was not consistent across low to high levels of 24-h sodium excretion. With the INTERSALT and Tanaka equations, overestimation occurred at the low levels of 24-h sodium excretion and underestimation at the high levels (Figures 3 and 4). When the Kawasaki equation was used with the morning specimen, overestimation appeared to occur across low to high levels of 24-h urinary sodium excretions (Figure 5). With the Mage equation, underestimation occurred at low levels and overestimation at high levels of sodium excretion (Figure 6). Although mean relative differences could be small, the 95% limits of agreement were wide for predicted 24-h sodium excretions. When the INTERSALT equation was used with the morning void as an example, the mean relative difference was 0.1% and the upper and lower limits of agreement were −71.3% and 71.5%, respectively (Figure 3). Similar patterns were observed among sex and race subgroups (data not shown).
FIGURE 3.
Bland-Altman plots of the relative bias (difference in agreement) between measured 24-h urinary sodium excretion on one day and predicted 24-h urinary sodium excretion on the same day based on the INTERSALT equation (27) and spot urinary sodium collected in the morning (A), in the afternoon (B), in the evening (C), and overnight (D). The relative bias for each individual is the predicted minus the measured 24-h urinary sodium excretion divided by the mean of the predicted and measured 24-h urinary sodium multiplied by 100 and is plotted against the mean of the predicted and measured 24-h urinary sodium excretion. The solid black line represents the mean relative difference (bias). The dashed lines represent the 95% limits of agreement of the mean relative difference ± 1.96 × SD. INTERSALT, International Cooperative Study on Salt and Blood Pressure.
FIGURE 4.
Bland-Altman plots of the relative bias (difference in agreement) between measured 24-h urinary sodium excretion on one day and predicted 24-h urinary sodium excretion on the same day based on the Tanaka equation (30) and spot urinary sodium collected in the morning (A), in the afternoon (B), in the evening (C), and overnight (D). The relative bias for each individual is the predicted minus the measured 24-h urinary sodium excretion divided by the mean of the predicted and measured 24-h urinary sodium multiplied by 100 and is plotted against the mean of the predicted and measured 24-h urinary sodium excretion. The solid black line represents the mean relative difference (bias). The dashed lines represent the 95% limits of agreement of the mean relative difference ± 1.96 × SD.
FIGURE 5.
Bland-Altman plots of the relative bias (difference in agreement) between measured 24-h urinary sodium excretion on one day and predicted 24-h urinary sodium excretion on the same day based on the Kawasaki equation (29) and spot urinary sodium collected in the morning. The relative bias for each individual is the predicted minus the measured 24-h urinary sodium excretion divided by the mean of the predicted and measured 24-h urinary sodium multiplied by 100 and is plotted against the mean of the predicted and measured 24-h urinary sodium excretion. The solid black line represents the mean relative difference (bias). The dashed lines represent the 95% limits of agreement of the mean relative difference ± 1.96 × SD.
FIGURE 6.
Bland-Altman plots of the relative bias (difference in agreement) between measured 24-h urinary sodium excretion on one day and predicted 24-h urinary sodium excretion on the same day based on the Mage equation (20, 21) and spot urinary sodium collected in the morning (A), in the afternoon (B), in the evening (C), and overnight (D). The relative bias for each individual is the predicted minus the measured 24-h urinary sodium excretion divided by the mean of the predicted and measured 24-h urinary sodium multiplied by 100 and is plotted against the mean of the predicted and measured 24-h urinary sodium excretion. The solid black line represents the mean relative difference (bias). The dashed lines represent the 95% limits of agreement of the mean relative difference ± 1.96 × SD.
Individual correlations with measured 24-h urinary sodium excretion
Total sodium excreted in measured spot urine collections at all 4 times was fair-to-moderately correlated with measured 24-h sodium excretions in all participants (0.45–0.60) (Table 3). Within race and sex subgroups, variability in correlations was somewhat greater. The lowest correlation was 0.24 when the afternoon specimens from other race men were used and the highest was 0.68 when the afternoon specimens from black men were used. Among all participants and race-sex subgroups, the range of correlations of overnight measured spot specimens with measured 24-h sodium excretion was 0.58–0.61.
TABLE 3.
Individual correlation coefficients (r) with measured 24-h urinary sodium excretion, by population subgroup and the timing of spot urine specimen collections in adults aged 18–39 y1
| Predicted 24-h urinary sodium excretion |
||||||
| No. of subjects | Measured sodium (mg) excreted in timed-spot urine specimens | INTERSALT2 | Tanaka3 | Kawasaki4 | Mage5 | |
| All | ||||||
| Morning | 339 | 0.45 | 0.47 | 0.50 | 0.52 | 0.51 |
| Afternoon | 389 | 0.50 | 0.49 | 0.51 | NA6 | 0.55 |
| Evening | 402 | 0.50 | 0.54 | 0.59 | NA6 | 0.61 |
| Overnight | 406 | 0.60 | 0.44 | 0.47 | NA6 | 0.51 |
| Black men | ||||||
| Morning | 76 | 0.53 | 0.63 | 0.65 | 0.65 | 0.65 |
| Afternoon | 85 | 0.68 | 0.71 | 0.72 | NA6 | 0.72 |
| Evening | 88 | 0.57 | 0.68 | 0.71 | NA6 | 0.72 |
| Overnight | 89 | 0.61 | 0.46 | 0.43 | NA6 | 0.44 |
| Black women | ||||||
| Morning | 90 | 0.46 | 0.29 | 0.34 | 0.36 | 0.33 |
| Afternoon | 102 | 0.44 | 0.32 | 0.46 | NA6 | 0.47 |
| Evening | 107 | 0.42 | 0.46 | 0.58 | NA6 | 0.60 |
| Overnight | 107 | 0.58 | 0.28 | 0.38 | NA6 | 0.40 |
| Other men | ||||||
| Morning | 77 | 0.32 | 0.50 | 0.59 | 0.55 | 0.58 |
| Afternoon | 90 | 0.24 | 0.32 | 0.43 | NA6 | 0.46 |
| Evening | 94 | 0.42 | 0.51 | 0.61 | NA6 | 0.62 |
| Overnight | 97 | 0.60 | 0.47 | 0.54 | NA6 | 0.54 |
| Other women | ||||||
| Morning | 96 | 0.42 | 0.41 | 0.46 | 0.46 | 0.48 |
| Afternoon | 112 | 0.51 | 0.53 | 0.52 | NA6 | 0.53 |
| Evening | 113 | 0.55 | 0.58 | 0.52 | NA6 | 0.54 |
| Overnight | 113 | 0.61 | 0.52 | 0.58 | NA6 | 0.60 |
All values are Spearman correlation coefficients between measured 24-h urinary sodium excretion and all sodium (mg) in a spot urine specimen or predicted 24-h urinary sodium excretion based on sodium concentration from a spot urine collection used with 1 of the 4 estimation equations: INTERSALT, Tanaka, Kawasaki, and Mage. The timing of urine specimens was as follows: morning (the second void on rising in the morning), 0830–1230; afternoon, 1231–1730; evening, 1731–2359; and overnight (the first void after the longest period of sleep), 0400–1200 the next morning. All correlation coefficients were statistically significant at P < 0.05. INTERSALT, International Cooperative Study on Salt and Blood Pressure.
Reference 20. For men: predicted 24-h urinary sodium excretion (mg/d) = 23 × {25.46 + [0.46 × timed-spot sodium concentration (mmol/L)] − [2.75 × timed-spot creatinine concentration (mmol/L)] − [0.13 × timed-spot potassium concentration (mmol/L)] + [4.10 × BMI (kg/m2)] + [0.26 × age (y)]}. For women: predicted 24-h urinary sodium excretion (mg/d) = 23 × {5.07 + [0.34 × timed-spot sodium concentration (mmol/L)] − [2.16 × timed-spot creatinine concentration (mmol/L)] − [0.09 × timed-spot potassium concentration (mmol/L)] + [2.39 × BMI (kg/m2)] + [2.35 × age (y)] – [0.03× age2 (y)]}.
Reference 23. Predicted 24-h urinary sodium excretion (mg/d) = 23 × (21.98 × XNa0.392), where XNa = [spot sodium concentration (mmol/L)/spot creatinine concentration (mg/dL) × 10] × [predicted 24-h creatinine (mg/d)]. Predicted 24-h creatinine (mg/d) = [−2.04 × age (y)] + [14.89 × weight (kg)] + [16.14 × height (cm)] − 2244.45.
Reference 22. Predicted 24-h urinary sodium excretion (mg/d) = 23 × (16.3 × XNa0.5). For men: predicted 24-h creatinine (mg/d) = [−12.63 × age (y)] + [15.12 × weight (kg)] + [7.39 × height (cm)] − 79.9. For women: predicted 24-h creatinine (mg/d) = [−4.72 × age (y)] + [8.58 × weight (kg)] + [5.09 × height (cm)] − 74.5.
References 32 and 33. Predicted 24-h sodium excretion (mg/d) = {[23 × spot sodium concentration (mmol/L)]/[spot creatinine concentration (mg/dL) × 10]} × [predicted 24-h creatinine (mg/d)]. For men: predicted 24-h creatinine (mg/d) = 0.00179 × [140 − age (y)] × [weight1.5 (kg) × height0.5 (cm)] × [1 + 0.18 × (black = 1, non-black = 0)] × [1.366–0.0159 × BMI (kg/m2)]. For women: predicted 24-h creatinine (mg/d) = 0.00163 × [140 − age (y)] × [weight1.5 (kg) × height0.5 (cm)] × [1 + 0.18 × (black = 1, nonblack = 0)] × [1.429–0.0198 × BMI (kg/m2)].
Not applicable because the Kawasaki equation was developed to estimate 24-h urinary sodium excretion based on the second morning void only.
In all participants, individual correlations between predicted and measured 24-h sodium excretions were 0.44–0.61 (Table 3). Within race-sex subgroups, the lowest correlation with measured 24-h urine excretion was 0.28 when the INTERSALT equation was used with overnight specimens from black women and the highest correlations were 0.71–0.72 when the Tanaka and Mage equations were used with afternoon and evening specimens from black men.
Additional analyses
Of the 407 participants, 7 (1.7%) participants in day 1 and 3 (2.3%) in day 2 reported missing one void during their collections. After exclusion of these individuals, we found no meaningful difference in the mean relative bias or individual correlations in relation to a single 24-h urine collection. After exclusion of 34 individuals with a measured-to-expected 24-h urine creatinine concentration <0.6, correlations did not differ nor did most estimates of bias (data not shown). Notably, the mean bias in predicted 24-h sodium excretion from the INTERSALT equations did not differ with and without exclusion of these participants (data not shown). Less than 1% of participants reported taking blood pressure–lowering medications, and 3% reported having hypertension; their exclusion did not change our results (data not shown).
DISCUSSION
Of the prediction equations evaluated, the INTERSALT equations may provide the least biased information about group mean 24-h sodium excretion in young US adults. When used with spot urine specimens collected in the morning, afternoon, or evening, INTERSALT equations appear to estimate group mean 24-h urinary sodium excretion, the current standard for assessment, by ±200 mg for all participants and within most race-sex subgroups. Timing of spot urine specimen collection, sex, and race may affect estimation of 24-h urinary sodium excretion. For individuals, significant over- and underprediction was not consistent across low to high levels of 24-h sodium excretion. The INTERSALT prediction equations, although close to observed levels at the mean, appear to have a positive bias at low levels and a negative bias at high levels of individual 24-h sodium excretion.
In general, mean predicted 24-h sodium excretion based on specimens collected in the afternoon and evening, compared with morning or overnight, was a better approximation of mean 24-h sodium excretion. Metabolic studies indicate that, among healthy persons, most of the sodium consumed is excreted in the afternoon and evening with sodium excretion dipping to low levels from midnight to early morning (13, 18). Thus, one might expect predicted 24-h sodium excretion based on sodium concentrations in afternoon or evening spot specimens to better represent measured 24-h urinary sodium excretion. Mean 24-h urinary sodium excretion predicted with overnight spot urinary sodium concentration was generally lower than that predicted with specimens collected at other times, particularly when the Mage equations were used.
Whereas the concentration of sodium may be lower, the overnight collection has a higher volume (38) and when expressed as total sodium excretion, the overnight collection may be a better predictor of 24-h excretion than collections at other times of the day. Compared with total sodium excretion from morning, afternoon, and evening specimens, total sodium excretion from the overnight spot urine collection was the most strongly correlated with measured 24-h sodium excretion on the same day. Currently, predictive equations use sodium concentrations from spot urine specimens. Measurement of total sodium excretion in a spot urine specimen requires collection of the entire void.
The individual correlations (r = 0.2–0.7) of predicted and measured 24-h urinary sodium excretion in our study were similar or lower than those published in previous studies (20, 22, 23, 25–28, 30). Correlations measure the strength of an association between 2 measurements, but not their agreement (41, 42). In the Kawasaki study (22), mean predicted and measured 24-h urinary sodium excretion did not differ, nor did they appear to differ in other studies of Japanese adults (26–28). Whereas the correlations using the Kawasaki approach also were evaluated in a Western population of 105 Canadian adults (r = 0.4–0.5) (25), no data were presented on the agreement in means or across the distribution of sodium excretion. It is possible that equations developed based on higher sodium intakes in Asian populations do not apply to the lower sodium intake measured in the US or Western populations (43). The Tanaka estimates also were developed for use in Japanese adults and were not as biased as the Kawasaki equations when applied in the current study; however, the mean 24-h sodium excretion of the population on which these equations was based (4545 mg for men and 4066 mg for women) was lower than that for the population used to develop the Kawasaki equations (5,350 mg for men and 4287 mg for women).
Our study had potential limitations. First, we used questionnaire data to assess whether 24-h urine collections were complete. Of the 407 participants, none missed more than one void, and, after exclusion of 1.7% of individuals who missed one void or individuals with potential incomplete urine collections based on measured-to-expected creatinine ratios, our results did not change. Second, the spot urine samples used with predictive equations to estimate 24-h sodium excretion were part of the whole 24-h urine collection, ie, were not independent; thus, it is likely that the correlations observed are higher than those expected if the spot specimens had been collected on a different day. In a post hoc analysis of the subset of 133 participants providing two 24-h urine collections, we found the correlations between spot and 24-h urinary sodium excretion collected on different days to be 0.18–0.27. Finally, our sample is not representative of the US population. We purposefully selected participants who were adults aged 18–39 y to minimize other possible factors that might affect urinary sodium excretion. For this reason, potential participants were ineligible if they were pregnant or reported taking loop diuretics, had chronic kidney disease, or had new or modified hypertension treatment in the past 2 wk. We did not exclude people with hypertension (n = 7), even though previous studies suggest that hypertension may affect urinary sodium excretion. In a subanalysis, exclusion of these individuals did not change the results. Importantly, it is not known whether our results apply to younger or older persons and populations with a higher prevalence of hypertension or other chronic diseases, including those taking diuretics.
Further analyses of these data include evaluating the use of more than one spot urine specimen to capture a greater amount of total sodium intake and/or adjust for diurnal variability as well as >1 d to allow estimation of population distributions. A urine calibration study in older adults with more participants with hypertension, mild-moderate chronic kidney disease, or use of diuretics is ongoing to better understand how these factors influence prediction. Designing a study to calibrate mean estimated sodium intake from spot urine samples among small (homogenous) groups of the population compared with mean measured 24-h urine excretion may better inform monitoring at the population level and support efforts to reduce sodium intake.
This was the first study to our knowledge to evaluate several urinary sodium predictive equations using the same sample of young adults with little or no hypertension. Our results indicated that the bias in mean predicted 24-h urinary sodium excretion was generally small when the INTERSALT predictive equations were used with morning, afternoon, or evening spot urine collections in our population. This was true among all participants and within race-sex subgroups across most timed-spot urine specimens. Thus, based on these data from young adults with little or no hypertension, mean US 24-h sodium intake may be slightly underestimated if INTERSALT equations are applied to single spot urine specimens in NHANES. Together with the calibration study showing accurate assessment of population means across low to high sodium levels (20), these data suggest that these equations could be used with a single spot urine specimen to monitor temporal trends in population mean sodium intake among young US adults. Our data also confirm that these prediction equations—based on a single spot urine specimen—should not be used to estimate individual 24-h sodium excretion because of the differential bias in individual estimated 24-h sodium excretion across low to high sodium levels. Although 24-h sodium excretion is the recommended method for evaluating population mean sodium intake, our findings inform the use of predictive equations to estimate population mean 24-h urinary sodium excretion as part of a national surveillance system critical to evaluating US efforts to reduce sodium intake.
Acknowledgments
We acknowledge the participants in this study, without whom the study would not have been possible. We also acknowledge Vicki L Burt, who was responsible along with C-YW for collecting the data.
The authors’ responsibilities were as follows—MEC, C-YW, T-CC, CMP, PE, CDG, ALC, CTS, KL, CGP, CAS, KLC, and CML: designed the analysis; MEC, C-YW, T-CC, and CDG: analyzed the data; MEC: wrote the initial draft, which was modified based on critical review from all coauthors, and had primary responsibility for all of the content. All authors read and approved the final manuscript. PE acknowledges support from the National Institute for Health Research Biomedical Research Centre, Imperial College Healthcare National Health Service Trust and Imperial College. PE is a Senior Investigator at the National Institute for Health Research. None of the authors had any conflicts of interest.
REFERENCES
- 1.Bibbins-Domingo K, Chertow CM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, Goldman L. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med 2010;362:590–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Institute of Medicine. Strategies to reduce sodium intake in the United States. Washington, DC: The National Academies Press, 2010. [Google Scholar]
- 3.US Department of Health and Human Services. Healthy People 2020. Nutrition and weight status objectives. Updated 18 May 2012. Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=29 (cited 5 June 2012).
- 4.US Department of Health and Human Services, US Department of Agriculture. Dietary Guidelines for Americans, 2010. 7th ed. Washington, DC: USDA, 2011.
- 5.US Department of Health and Human Services, US Department of Agriculture. Approaches to reducing sodium consumption; establishment of dockets; request for comments, data, and information. Federal Register 2011;76(179):57050-57054. Available from: http://www.regulations.gov/#!documentDetail;D=FDA-2011-N-0400-0001 (cited 5 June 2012).
- 6.World Health Organization/Pan American Health Organization Regional Expert Group for Cardiovascular Disease Prevention through Population-wide Dietary Salt Reduction. Protocol for population level sodium determination in 24-hour urine samples. May 2010. Available from: http://new.paho.org/hq/dmdocuments/2010/pahosaltprotocol.pdf (cited 18 June 2012).
- 7.Holbrook JT, Patterson KY, Bodner JE, Douglas LW, Veillon C, Kelsay JL, Mertz W, Smith JC. Sodium and potassium intake and balance in adults consuming self-selected diets. Am J Clin Nutr 1984;40:786–93. [DOI] [PubMed] [Google Scholar]
- 8.Schachter J, Harper PH, Radin ME, Caggiula AW, McDonald RH, Diven WF. Comparison of sodium and potassium intake with excretion. Hypertension 1980;2:695–9. [DOI] [PubMed] [Google Scholar]
- 9.Liu K, Stamler J. Assessment of sodium intake in epidemiological studies on blood pressure. Ann Clin Res 1984;16:49–54. [PubMed] [Google Scholar]
- 10.Strauss MB, Lamdin E, Smith WB, Bleifer SJ. Surfeit and deficit of sodium. AMA Arch Intern Med 1958;102:527–36. [DOI] [PubMed] [Google Scholar]
- 11.Black DA. Salt and hypertension. Br J Nutr 1952;6:428–32. [DOI] [PubMed] [Google Scholar]
- 12.Epstein M, Hollenberg NK. Age as a determinant of renal sodium conservation in normal man. J Lab Clin Med 1976;87:411–7. [PubMed] [Google Scholar]
- 13.Watson RL, Langford HG. Usefulness of overnight urines in population groups. Am J Clin Nutr 1970;23:290–304. [DOI] [PubMed] [Google Scholar]
- 14.Dyer AR, Stamler R, Grimm R, Stamler J, Berman R, Gosch FC, Emidy LA, Elmer P, Fishman J, Van Heel N, et al. Do hypertensive patients have a different diurnal pattern of electrolyte excretion? Hypertension 1987;10:417–24. [DOI] [PubMed] [Google Scholar]
- 15.Bankir L, Perucca J, Weinberger MH. Ethnic differences in urine concentration: possible relationship to blood pressure. Clin J Am Soc Nephrol 2007;2:304–12. [DOI] [PubMed] [Google Scholar]
- 16.Pietinen PI, Findley TW, Clausen JD, Finnerty FA, Jr, Altschul AM. Studies in community nutrition: estimation of sodium output. Prev Med 1976;5:400–7. [DOI] [PubMed] [Google Scholar]
- 17.Ji C, Sykes L, Paul C, Dary O, Legetic B, Campbell NRC, Cappuccio FP; Subgroup for Research and Surveillance of the PAHO-WHO Regional Expert Group for Cardiovascular Disease Prevention Through Population-Wide Dietary Salt Reduction. Systematic review of studies comparing 24-hour and spot urine collections for estimating population sodium intake. Rev Panam Salud Publica 2012;32:307–15. [DOI] [PubMed] [Google Scholar]
- 18.Dyer AR, Martin GJ, Burton WN, Levin M, Stamler J. Blood pressure and diurnal variation in sodium, potassium, and water excretion. J Hum Hypertens 1998;12:363–71. [DOI] [PubMed] [Google Scholar]
- 19.Liu K, Dyer AR, Cooper RS, Stamler R, Stamler J. Can overnight urine replace 24-hour urine collection to assess salt intake? Hypertension 1979;1:529–36. [DOI] [PubMed] [Google Scholar]
- 20.Brown IJ, Dyer AR, Chan Q, Cogswell ME, Ueshima H, Stamler J, Elliott P. on behalf of the INTERSALT Cooperative Study on Salt, Other Factors, and Blood Pressure. Estimating 24-hour urinary sodium excretion from casual urinary sodium concentration in Western populations: the INTERSALT Study. Am J Epidemiol 2013;177:1180–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joossens JV, Claessens J, Geboers J, Claes JH. Electrolyte and creatinine in multiple 24-hour urine collections (1970-1974). In: Kestoloot H, Joossens JV, eds. Epidemiology of arterial blood pressure. Boston, MA: Marinus Nijhoff Publishers, 1980:45–63. [Google Scholar]
- 22.Kawasaki T, Itoh K, Uezono K, Sasaki H. A simple method for estimation of 24 h urinary sodium and potassium excretion from second morning voiding urine specimens in adults. Clin Exp Pharmacol Physiol 1993;20:7–14. [DOI] [PubMed] [Google Scholar]
- 23.Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, Hasimoto T. A simple method to estimate populational 24-hour urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens 2002;16:97–103. [DOI] [PubMed] [Google Scholar]
- 24.Pan W-H, Chen J-Y, Chen Y-C, Tsai W-Y. Diurnal electrolyte excretion pattern affects estimates of electrolyte status based on 24-h, half-day, and overnight urine. Chin J Physiol 1994;37:49–53. [PubMed] [Google Scholar]
- 25.O'Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, McQueen M, Sleight P, Sharma AM, Dans A, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA 2011;306:2229–38. [DOI] [PubMed] [Google Scholar]
- 26.Kawamura M, Hashimoto T, Owada M, Sugawara T. The influence of posture on the estimation of daily salt intake by the second morning urine method. Hypertens Res 2010;33:505–10. [DOI] [PubMed] [Google Scholar]
- 27.Kawamura M, Ohmoto A, Hashimoto T, Yagami F, Owada M, Sugawara T. Second morning urine method is superior to the casual urine method for estimating daily salt intake in patients with hypertension. Hypertens Res 2012;35:611–6. [DOI] [PubMed] [Google Scholar]
- 28.Kawasaki T, Itoh K, Uezono K, Sasaki H. Estimation of 24-hour urinary sodium and potassium excretion from predicted value of 24-hour urinary creatinine excretion and fractional urine sodium/creatinine ratio and potassium/creatinine ratio. Seventh Symposium on Salt 1993;2:257–62. [Google Scholar]
- 29.Mann SJ, Gerber LM. Estimation of 24-hour sodium excretion from spot urine samples. J Clin Hypertens (Greenwich) 2010;12:174–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adachi T, Kawamura M, Owada M, Hiramori K. Effect of age on renal functional and orthostatic vascular response in healthy men. Clin Exp Pharmacol Physiol 2001;28:877–80. [DOI] [PubMed] [Google Scholar]
- 31.CDC. National Health and Nutrition Examination Survey. 2009-2010. Laboratory components. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/labcomp_f.pdf (cited 28 July 2012).
- 32.Mage DT, Allen RH, Kdali A. Creatinine corrections for estimating children's and adult's pesticide intake doses in equilibrium with urinary pesticide and creatinine concentrations. J Expo Sci Environ Epidemiol 2008;18:360–8. [DOI] [PubMed] [Google Scholar]
- 33.Huber DR, Blount BC, Mage DT, Letkiewicz FJ, Kumar A, Allen RH. Estimating perchlorate exposure from food and tap water based on US biomonitoring and occurrence data. J Expo Sci Environ Epidemiol 2011;21:395–407. [DOI] [PubMed] [Google Scholar]
- 34.CDC. National Health and Nutrition Examination Survey (NHANES). 2009-2010. Home Urine Collection. January 2009. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/HomeUrine.pdf (cited 28 July 2012).
- 35.Wang C-Y, Cogswell ME, Loria CM, Chen T-C, Pfeiffer CM, Swanson CA, Caldwell KL, Perrine CG, Carriquiry AL, Liu K, Sempos CT, Gillespie CD, Burt VL. Urinary excretion of sodium, potassium, and chloride, but not iodine, varies by timing of collection in a 24-hour calibration study. J Nutr 2013;. [DOI] [PMC free article] [PubMed]
- 36.Roche Diagnostics ion-selective electrodes (ISE)/Na+, K+, Cl- Package insert, 2009-03, V6.
- 37.Mazzachi BC, Peake MJ, Ehrhardt V. Reference range and method comparison studies for enzymatic and Jaffe creatinine assays in plasma and serum and early morning urine. Clin Lab 2000;46:53–5. (Roche/Hitachi Package Insert, 2010 04, V 17 English.) [PubMed]
- 38.Abou-Auda HS. Comparative pharmacokinetics and pharmacodynamics of furosemide in Middle Eastern and in Asian subjects. Int J Clin Pharmacol Ther 1998;36:275–81. [PubMed] [Google Scholar]
- 39.Kawasaki T, Ito K, Uezono K, Ueno M. Prediction of 24-h urinary creatinine excretion from age, body weight, and height of an individual and its application. Japanese J Pub Health 1991;38:567–74 (in Japanese with English abstract). [PubMed] [Google Scholar]
- 40.Cockcroft DW, Gault MH. Prediction of creatinine clearance is from serum creatinine. Nephron 1976;16:31–41. [DOI] [PubMed] [Google Scholar]
- 41.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–10 (PubMed). [PubMed] [Google Scholar]
- 42.Bland JM, Altman DG. Applying the right statistics: analyses of measurement studies. Ultrasound Obstet Gynecol 2003;22:85–93 (PubMed). [DOI] [PubMed] [Google Scholar]
- 43.Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intake around the world: implications for public health. Int J Epidemiol 2009;38:791–813 (PubMed). [DOI] [PubMed] [Google Scholar]
- 44.Bingham SA, Cummings JH. The use of creatinine output as a check on completeness of 24-hour urine collections. Hum Nutr Clin Nutr 1985;39:343–53 (PubMed). [PubMed] [Google Scholar]
- 45.Joossens JV, Geboers J. Monitoring salt intake of the population: methodological considerations. In: De Backer GG, Pedoe HT, Ducimetiere P, eds. Surveillance of the dietary habits of the population with regard to cardiovascular diseases, EURONUT Report 2. Wageningen, Netherlands: Department of Human Nutrition, Agricultural University, 1984:61–73. [Google Scholar]
- 46.Liu LS, Zheng DY, Jin L, Liao YL, Liu K, Stamler J. Variability of urinary sodium and potassium excretion in north Chinese men. J Hypertens 1987;5:331–5 (PubMed). [DOI] [PubMed] [Google Scholar]
- 47.Knuiman JT, Hautvast JG, van der Heijden L, Geboers J, Joossens JV, Tornqvist H, Isaksson B, Pietinen P, Tuomilehto J, Flynn A, et al. A multi-centre study on within-person variability in the urinary excretion of sodium, potassium, calcium, magnesium and creatinine in 8 European centres. Hum Nutr Clin Nutr 1986;40:343–8 (PubMed). [PubMed] [Google Scholar]