Abstract
Community-based participatory research (CBPR) offers great potential for increasing the impact of research on reducing cancer health disparities. This article reports how the Community Outreach Core (COC) of the Meharry-Vanderbilt-Tennessee State University (TSU) Cancer Partnership has collaborated with community partners to develop and implement CBPR. The COC, Progreso Community Center, and Nashville Latino Health Coalition jointly developed and conducted the 2007 Hispanic Health in Nashville Survey as a participatory needs assessment to guide planning for subsequent CBPR projects and community health initiatives. Trained community and student interviewers surveyed 500 Hispanic adults in the Nashville area, using a convenience sampling method. In light of the survey results, NLHC decided to focus in the area of cancer on the primary prevention of cervical cancer. The survey led to a subsequent formative CBPR research project to develop an intervention, then to funding of a CBPR pilot intervention study to test the intervention.
Keywords: Community-based participatory research, Hispanic, survey, cancer
Community-based participatory research (CBPR) is an approach that combines scientific research with collective action to address issues that affect a community through the participation of community partners in all phases of the research process. It enables the inclusion of the concerns and cultural perspectives of affected populations in the design and implementation of health interventions. Community-based participatory research offers great potential for increasing the impact of research on reducing cancer health disparities. This article reports on the development, implementation, and results of a community health survey that has been used to advance subsequent phases of a CBPR process. The objective of the 2007 Hispanic Health in Nashville Survey was to identify the health priorities and health needs (including cancer-related needs) of the Nashville Hispanic community.
Participatory research and health disparities
Some authors argue that traditional research, such as disparities in cancer, has been ineffective in addressing health disparities because it has not included stakeholders (including both the grassroots community and community-based organizations) in all parts intervention design and implementation, which precludes the incorporation of the concerns and culture of the affected population.1-4 Community-based participatory research offers great potential for increasing the impact of research on reducing cancer health disparities.5 Community-based participatory research (CBPR) is not a research methodology, but instead CBPR is an approach for combining scientific research with collective action to address specific problems that affect a community.1 CBPR approaches involve forming collaborative community-academic partnerships, with the goal of working together as equal partners, in a way that balances power and shares resources, for the benefit of the community's health. Such collaborative partnerships offer the opportunity to combine in a complementary way the knowledge, skills, and resources of members of the community and affected populations, the people who work directly with the community, and academic researchers in order to identify and prioritize the needs of the community and to develop concrete projects to improve these problems and directly benefit members of the community.1,6
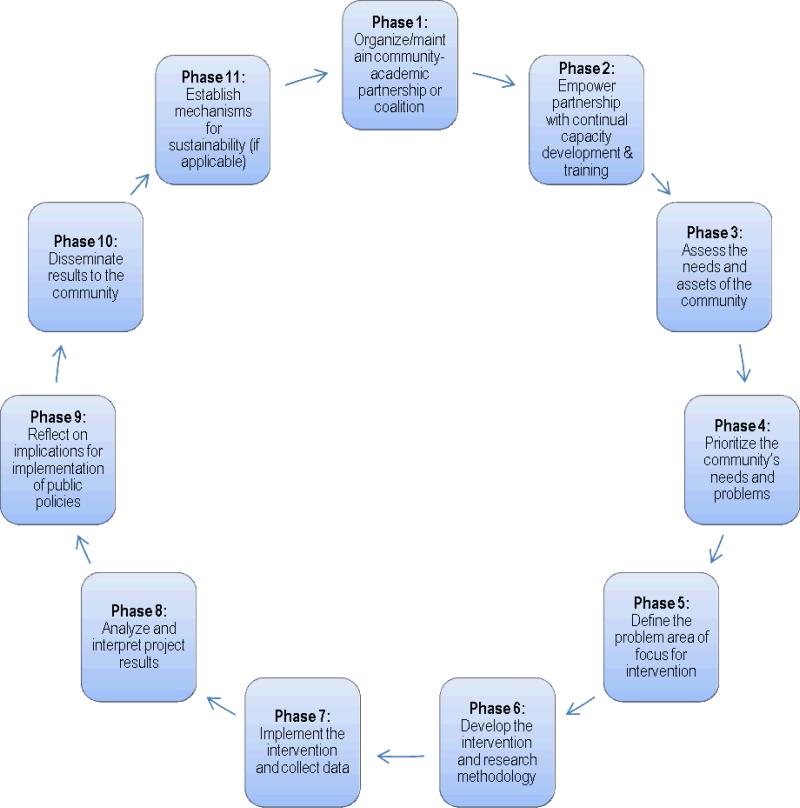
A CBPR process typically consists of the phases listed in Figure 1, in a process that is both cyclical and iterative, such that partnerships may move back and forth between phases and repeat the cycle as the partnership matures. Since every partnership and project is unique, they may not go through all of these phases or follow them in this exact order, but the phases listed in Figure 1 outline the general process.1,7-8 CBPR approaches differ from traditional scientific research approaches by focusing not only on individuals, but also on the social contexts and communities in which they live; by empowering affected communities to help identify problems as well as assets in the community, and to be part of the solutions; and by engaging community-based organizations and community members as equal and active partners throughout all phases of the research process.
Figure 1.
Phases of a Community-Based Participatory Research (CBPR) Process
Cancer Outreach Core of the Meharry-Vanderbilt-TSU Cancer Partnership
In 2000, Meharry Medical College (a Historically Black College/University [HBCU]) and Vanderbilt-Ingram Cancer Center (VICC) formed the Meharry-Vanderbilt Cancer Partnership to contribute to the elimination of racial/ethnic and socioeconomic disparities in cancer, with funding from the National Cancer Institute. The goal of the Meharry-Vanderbilt Cancer Partnership is to strengthen and expand collaborative cancer research at Meharry and VICC. In 2006, starting in the second funding cycle, Tennessee State University (TSU, another HBCU) was brought in as an additional academic partner in the Cancer Partnership to co-lead a new Cancer Outreach Core (COC).
The purpose of the COC is to provide a means for members of the local community and interested organizations to partner actively with Meharry, VICC, and TSU on cancer disparities research and outreach initiatives. The COC focuses on the African American and Hispanic communities in Nashville/Davidson County. The aims of the COC are: (1) to build capacity of academic and community partners to conduct community-based participatory research focused on reducing cancer disparities; (2) to collaborate with academic and community partners on planning and evaluation activities to guide the development of new research and outreach initiatives; and (3) to provide direct cancer outreach to consumers, support other local outreach efforts, and disseminate Partnership information.
With an explicit commitment to community engagement, the COC strives to build on existing community assets and to alter the unequal power dynamics of traditional research by facilitating CBPR. Community partner-identified needs, interests, and priority areas guide the COC's outreach activities, capacity-building activities, and new research projects. First, the COC established partnerships with three existing community coalitions (Phase 1 of the CBPR process). These coalitions comprise a range of local health care, public health, non-profit and academic organizations. The COC provides regular technical support, training, and resources to the coalitions based on each coalition's needs (Phase 2 of the CBPR process), to increase the coalition's capacity to collaborate with academic partners on CBPR that is relevant to the coalition's mission, strategic plan, and community-identified priorities.
Need for local data on Hispanics
One of the COC's objectives was to conduct a needs and assets assessment of cancer disparities in Nashville (Phase 3 of the CBPR process), to serve as a resource for guiding the planning of collaborative CBPR projects. In addition to cataloging local cancer-related resources (assets), secondary datasets were used to assess cancer-related needs in terms of cancer incidence (Tennessee Cancer Registry), cancer mortality (Tennessee Death Statistical Summary System), and modifiable risk factors (Tennessee Behavioral Risk Factor Surveillance System). However, reliable county-level data from these sources are only available for Whites and Blacks/African Americans, not for Hispanics. In fact, health-related data on Hispanics in Nashville are very scarce in general.
Tennessee and Nashville/Davidson County are new growth communities – communities that have historically had relatively few Hispanics but have experienced rapid growth in recent years.9 Tennessee ranked fourth among the 16 Southern states in the rate of growth of the Hispanic population from 1990-2000.10 According to U.S. Census Bureau, from 1990 to 2005-2007 the Hispanic population increased five times (504%) in the entire state and eight times (800%) in the county.11 In Nashville/Davidson County in 2005-2007, nearly 43,000 individuals (7.3%) identified themselves as being of Hispanic origin (compared with 3.3% in the entire state of Tennessee). However, the population is likely larger due to possible undercounts in official numbers. Hispanic immigrants in new growth communities face greater barriers in access to health care and related services, since these communities tend to have a less developed service infrastructure for serving this population compared to communities with established Hispanic populations.9,12 In previous CBPR research by TSU and Progreso Community Center (PCC), Hispanic community members in Nashville have expressed interest in being able to prevent health problems, in particular due to lack of health insurance and concerns about health care costs, but were unaware of many existing local resources for the uninsured.13
In 2007 the COC partnered with Progreso Community Center (PCC) and the Nashville Latino Health Coalition (NLHC) to address this lack of local health data on Hispanics. PCC is the first Hispanic community center and first Hispanic grassroots membership organization in Nashville, Tennessee. The partners did not establish a formal memorandum of understanding specific to the survey, but the academic partners and PCC had an established collaborative relationship as members of NLHC, which is led by PCC and is one of the COC's partner coalitions. PCC and NLHC were interested in collaborating on a community health survey to help guide NLHC planning efforts (Phase 3 of CBPR process). The COC and PCC jointly developed and implemented the survey as a CBPR project, collaborating on all phases of research. Nashville Latino Health Coalition also supported the project by facilitating permission to collect surveys at several community organizations. The survey results have been used to guide subsequent phases of the CBPR process in collaboration with NLHC.
Methods
The Meharry-Vanderbilt Cancer Partnership COC, Progreso Community Center (PCC) and the Nashville Latino Health Coalition (NLHC) collaborated to conduct the 2007 Hispanic Health in Nashville Survey as a participatory needs assessment study. Using a CBPR approach, academic and community partners worked together to develop and implement every phase of the project. The objective of the survey was to identify the Nashville Hispanic community's health priorities and health needs (including cancer-related needs). The findings of the study have been used to advance subsequent phases of the CBPR process. The study protocol was approved by the Institutional Review Boards (IRBs) at Meharry Medical College, Vanderbilt University, and Tennessee State University.
Participatory Process of Survey Development
Hispanic PCC members participated in developing the content of the questionnaire, including which topics to cover. Since we sought to assess the primary health concerns and interests of the Hispanic community, we created a list of 25 health topics based on major causes of death and disability, known areas of health disparities for Hispanics, barriers to healthcare access, and other topics suggested by PCC members to be important to their community. There was also a choice for “other” where respondents could write in other topics.
In addition, we created several new items to gauge opinions about cancer clinical trials, the new HPV vaccine (the new human papillomavirus vaccine for prevention of cervical cancer), and desired information about cancer. We also created an item to assess ethnic media usage in order to assist with identification of possible communication channels for future efforts. Based on suggestions from PCC members, the team decided not to ask household income since some potential respondents could perceive this question as too personal and lead them to refuse to participate in the survey. PCC members played a key role in refining the Spanish version of the questionnaire for appropriateness of questions, readability, ease of comprehension, and common vocabulary that could be understood by people from multiple Latin American countries.
Measures
The brief, structured questionnaire was two pages long and included many standard questions drawn from Behavioral Risk Factor Survey, National Health Interview Survey and the U.S. Census, as well as some new items that were created for the assessment. Demographic characteristics included age, sex, marital status, education, country of origin, occupation, length of residence in Nashville, and ZIP code of residence. Modifiable risk factors included insurance coverage, English ability, smoking, height and weight (to calculate body mass index [BMI]), fruit and vegetable consumption, and leisure-time physical activity. A series of items asked respondents to report how recently they had a list of preventive health screenings such as Pap smear (cervical cancer), mammography (breast cancer), PSA (prostate specific antigen) blood test (prostate cancer), or colonoscopy (colorectal cancer), with the following options: Yes, within the past 12 months; Yes, over a year ago; Never; Not sure; and Not familiar with this test.
Respondents were given the list of 25 health topics developed by the team (and an “other” option that could be filled in) and asked to choose the top five topics or health problems that concern or are important to them and their families. Top health concerns were identified by calculating the percentage of people that chose each topic as one of their choices, then ranking the most frequently chosen topics.
Two questions assessed attitudes about cancer clinical trials. The first asked, What is your opinion of clinical trials that study cancer treatments? and gave the following response options: I've never heard of those studies, I think they are good, I think they are not good, and I'm not sure. The second asked, If you had cancer, would you participate in a clinical trial to receive your treatment? and gave the following response options: Definitely yes, Probably yes, I'm not sure, Probably not, and Definitely not.
To assess attitudes about the HPV vaccine, parents with daughters ages 18 and younger were asked, There is a new vaccine against cervical cancer for girls and teenage girls at least 9 years old. If the vaccine were free, would you get it for your daughter (or daughters)? The response options were: Definitely yes, Probably yes, I'm not sure, Probably not, and Definitely not.
To assess desired information about cancer, a question asked, What information would you like to know about cancer?, and respondents could choose one or more of the following choices: how to prevent cancer, exams used to detect cancer, where to get exams for uninsured individuals, support for people with cancer, clinical trials that study treatments, and other (with write-in space).
Ethnic media usage was assessed with the following question, Which Spanish language media outlets do you use the most? Respondents were instructed to choose one newspaper (out of list of eight local newspapers), one radio station (out of a list of five local radio stations), and one television station (out of two local channels). We ranked the frequency of each media outlet being chosen, as well as the frequency of choosing any media outlet in each category or no Spanish-language media outlet.
Procedures
Two Hispanic TSU students and 13 Hispanic Progreso Community Center members were trained to be survey interviewers, including training in research ethics and human subjects protection. Interviewers gave potential respondents an information sheet/consent document and verbally explained the procedures for the anonymous survey. Participants gave verbal consent to participate in the survey. The questionnaire was self-administered by the respondents, unless they asked for assistance, in which case an interviewer asked the questions and marked the answers. Respondents were given a $5 grocery gift card as an incentive.
Limited funding necessitated use of a convenience sample instead of a probability sample, which limits the generalizability of our findings. However, a convenience sample was sufficient for the purposes of a needs assessment to guide planning, so we strove to generate a sample that represented the Nashville Hispanic population as closely as possible. Therefore, we aimed to collect a relatively large sample from a variety of community locations and parts of town where Hispanics live and work, at a range of different times and day of the week. The interviewers surveyed N=500 Hispanic adults both through social networks and in public places, at the following community locations: neighborhoods (35%), churches (14%), the local health department (13%), a community center (11%), restaurants (10%), job sites (4%), retail stores (4%), community health clinics (4%), and laundromats (3%). The number of refusals to participate was not tracked systematically, but based on informal reports from the interviewers, we estimate that less than 10% of the persons invited to participate in the survey refused. The distribution of the participants’ ZIP code of residence closely matched the distribution of the Hispanic population in Nashville/Davidson County in the 2000 U.S. Census.
Descriptive analyses (frequencies) were performed using the SPSS statistical program.14 Percentages were calculated based on valid responses, with missing values (blank items) excluded from analyses.
Results
Sample demographic characteristics
The demographic characteristics of the sample are summarized in Table 1. Even though this is a convenience sample, the sample characteristics are quite similar to 2005-2007 estimates of the Hispanic population in Davidson County from the U.S. Census Bureau. The exception is gender; there were slightly more females than males in the sample (54.6%), compared with the Census Bureau's estimate of women comprising 43% of the Hispanic population in Davidson County.11 However, this is not surprising because it is common for women to participate in research studies at higher rates than men. In terms of age, 44.7% of the sample was 18 to 29 years of age, compared with 34% reported by the Census Bureau. Educational attainment was lower in the sample (66.2% did not finish high school, compared with 50% reported by the Census Bureau).11
Table 1.
Sample Demographic Characteristics, Nashville, Tennessee (N=500)
| VARIABLE | N | % |
|---|---|---|
| Gender | ||
| Men | 227 | 45.4 |
| Women | 273 | 54.6 |
| No Response (missing) | 0 | -- |
| Age | ||
| 18-29 years | 221 | 44.7 |
| 30-39 years | 153 | 31.0 |
| 40-49 years | 69 | 14.0 |
| 50 years and older | 51 | 10.3 |
| No Response (missing) | 6 | -- |
| Education | ||
| Less than High School Degree | 325 | 66.2 |
| High School Degree | 81 | 16.5 |
| Post High School/College | 85 | 17.3 |
| No Response (missing) | 9 | -- |
| Country of Origin | ||
| Mexico | 261 | 54.5 |
| Central America | 134 | 28.0 |
| Puerto Rico | 27 | 5.6 |
| Other Latin American country | 50 | 10.4 |
| USA | 7 | 1.5 |
| No Response (missing) | 21 | -- |
| Marital Status | ||
| Never Married | 138 | 28.5 |
| Married | 263 | 54.2 |
| Living with Partner | 50 | 10.3 |
| Divorced or Widowed | 34 | 7.0 |
| No Response (missing) | 15 | -- |
| Occupation | ||
| Not Employed | 128 | 26.0 |
| Construction | 101 | 20.5 |
| Domestic Services | 52 | 10.5 |
| Food Service | 43 | 8.7 |
| Factory/Production | 41 | 8.3 |
| Clerical/Customer Service | 27 | 5.5 |
| Professional | 11 | 2.2 |
| Other | 90 | 18.3 |
| No Response (missing) | 7 | -- |
| Years in Nashville | ||
| Less than 2 years | 68 | 13.9 |
| 2-4 years | 153 | 31.4 |
| 5-9 years | 190 | 38.9 |
| 10 years or longer | 77 | 15.8 |
| No Response (missing) | -- |
In the sample, 54.5% were born in Mexico, which is slightly less than the 67% reported by the Census Bureau.11 Over a quarter (28.0%) were born in a Central American country (Guatemala, El Salvador, Honduras, Costa Rica or Nicaragua), 5.6% were born in Puerto Rico, 10.4% in another Latin American country, and 1.5% were born in the U.S. Therefore, nearly all members of the sample were first-generation immigrants. Just over half of the sample was married (54.2%), and over a quarter were never married (28.5%), reflecting the young age of the community. The most common occupations were construction, domestic services, and food service. As for duration of residency in Nashville, 45.3% of the sample had lived in Nashville for less than five years, and only 15.8% of the sample had lived in Nashville for 10 or more years, which reflects the recent growth of this population.
Modifiable risk factors
Lack of health insurance is potentially modifiable through policy changes. In this Nashville sample, four out of five Hispanic adults (79.5%) had no health insurance (see Table 2). Only 4.9% were enrolled in TennCare (Tennessee's Medicaid program), 1.3% in Medicare, and 14.3% in private or other insurance. English ability is also modifiable. Over half (56.0%) of the respondents reported that they spoke little or no English. About one in five (21.9%) respondents reported that they are current smokers, and another one in five (20.2%) were former smokers. Based on self-reported height and weight, about one-third (35.0%) of respondents had a normal weight (body mass index (BMI) under 25), over one-third (38.8%) of the respondents were overweight (BMI=25-29), and about one-quarter (26.1%) were obese (BMI=30 or higher). A high percentage of respondents (91.7%) reported that they consume less than the recommended five or more servings a day of fruits and vegetables. About one-third (32.3%) of respondents reported that they engage in the recommended level of leisure-time physical activity (at least 30 minutes a day for five days a week or more), while just over a quarter (27.0%) had a sedentary lifestyle (no days with at least 10 minutes of moderate to intense physical activity outside of work). In other words, about two-thirds (67.7%) did not meet the recommended level of physical activity.
Table 2.
Prevalence of Modifiable Risk Factors and Cancer Screening
| VARIABLE | N | % |
|---|---|---|
| Medical Insurance Coverage | ||
| None | 377 | 79.5 |
| Medicaid/TennCare | 23 | 4.9 |
| Medicare | 6 | 1.3 |
| Private/Other Insurance | 68 | 14.3 |
| No Response (missing) | 26 | -- |
| English Ability | ||
| Very well | 60 | 12.0 |
| Well | 48 | 9.6 |
| Somewhat | 111 | 22.2 |
| A little | 209 | 41.8 |
| Not at all | 71 | 14.2 |
| No Response (missing) | 1 | -- |
| Smoking | ||
| Current smoker | 108 | 21.9 |
| Former smoker | 100 | 20.2 |
| Never smoked | 286 | 57.9 |
| No Response (missing) | 6 | -- |
| Body Mass Index (BMI) | ||
| Normal weight (BMI under 25) | 146 | 35.0 |
| Overweight (BMI 25-29) | 162 | 38.8 |
| Obese (BMI 30 or higher) | 109 | 26.1 |
| No Response (missing) | 83 | -- |
| Fruit/Vegetable Consumption | ||
| Less than 5 servings per day | 453 | 91.7 |
| 5 or more servings per day | 41 | 8.3 |
| No Response (missing) | 6 | -- |
| Physical Activity | ||
| No leisure-time physical activity | 131 | 27.0 |
| Less than 30 min for 5 days | 198 | 40.7 |
| At least 30 min for 5 days | 157 | 32.3 |
| No Response (missing) | 14 | -- |
| Cervical Cancer Screening* | ||
| Pap Test in past 12 months | 164 | 65.9 |
| Not sure/unfamiliar with test | 3 | 1.2 |
| No Response (missing) | 18 | -- |
| Breast Cancer Screening† | ||
| Mammography in past 12 months | 31 | 54.4 |
| Not sure/unfamiliar with test | 0 | 0.0 |
| No Response (missing) | 6 | -- |
| Colorectal Cancer Screening‡ | ||
| Colonoscopy in past 12 months | 7 | 17.9 |
| Not sure/unfamiliar with test | 11 | 28.2 |
| No Response (missing) | 12 | -- |
Among women ages 18 and older (N=249)
Among women ages 40 and older (N=57)
Among men and women ages 50 and older (N=39)
Cancer screening
Two-thirds (65.9%) of female respondents reported that they had a Pap smear for cervical cancer screening during the past 12 months (Table 2). Just over half of Hispanic women ages 40 and older (54.4%) reported having a mammogram for breast cancer screening in the past 12 months. Among Hispanic men and women ages 50 and older in the survey, 17.9% reported having a colonoscopy in the past year for colorectal cancer screening. Interestingly, 28.2% of these respondents indicated that they were not sure or were unfamiliar with the colonoscopy. There were not enough men in the recommended ages for prostate cancer screening (50 to 70 years) to estimate the frequency of this type of screening.
Top health concerns
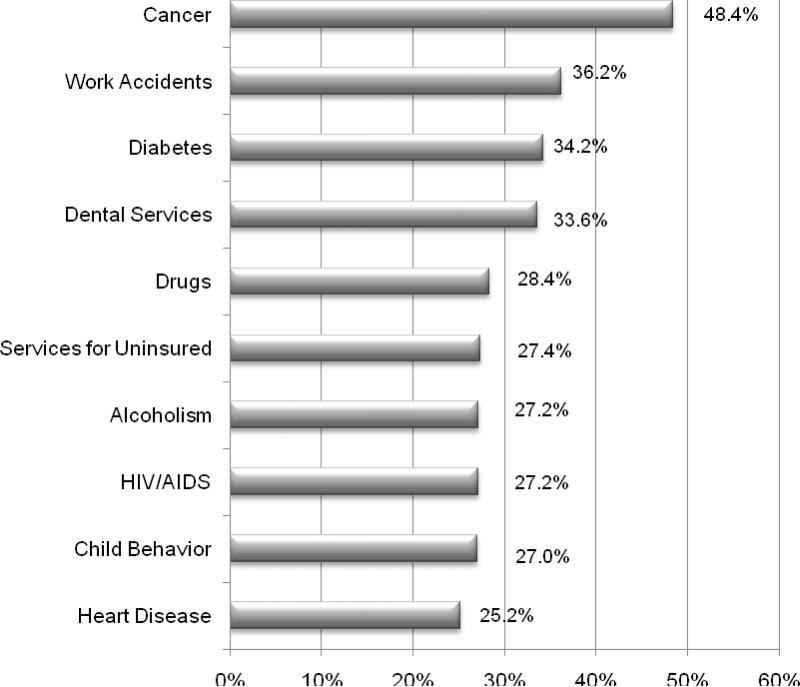
Cancer ranked as the #1 health concern in the Hispanic community, cited by nearly half of respondents, or 48.4% (see Figure 2). After cancer, other high-ranking concerns included work accidents (36.2%), diabetes (34.2%), and dental services (33.6%). The other topics among the top-ten health concerns included drugs (28.4%), services for the uninsured (27.4%), alcoholism (27.2%), HIV/AIDS (27.2%), child behavior (27.0%), and heart disease (25.2%).
Figure 2.
Top Health Concerns among Hispanic Adults in Nashville
Attitudes about cancer clinical trials
When asked their opinion of studies that investigate treatments for cancer (i.e., clinical trials), 70.6% said that they thought that the studies are good, 5.3% said that they are not good, 6.0% said they were not sure, and 18.1% said they had never heard of these studies (see Table 3). The vast majority of participants said they would participate in a clinical trial to receive treatment if they had cancer; specifically, 83.6% said definitely yes, and 12.3% said probably yes. Only 1.0% said they probably or definitely would not participate in a cancer clinical trial.
Table 3.
Attitudes about Cancer Clinical Trials and HPV Vaccine
| Question and Response Choices | N | % |
|---|---|---|
| What is your opinion of clinical trials that study cancer treatments? | ||
| I've never heard of those studies | 88 | 18.1 |
| I think they are good | 343 | 70.6 |
| I think they are not good | 26 | 5.3 |
| I am not sure | 29 | 6.0 |
| No Response (missing) | 6 | -- |
| If you had cancer, would you participate in a clinical trial to receive your treatment? | ||
| Definitely yes | 414 | 83.6 |
| Probably yes | 61 | 12.3 |
| I'm not sure | 16 | 3.2 |
| Probably not/Definitely Not | 4 | 1.0 |
| No Response (missing) | 5 | -- |
| There is a new vaccine aqainst cervical cancer for girls and teenage girls at least 9 years old. If the vaccine were free, would you get it for your daughter (or daughters)? | ||
| Definitely yes | 210 | 79.5 |
| Probably yes | 32 | 12.1 |
| I'm not sure | 19 | 7.2 |
| Probably not/Definitely Not | 3 | 1.2 |
| No Response (No daughters 18 and under/missing) | 236 | -- |
Attitudes about HPV vaccine
Nearly all (92.6%) of Hispanic parents with daughters age 18 and under reported that they would either definitely (79.5%) or probably (12.1%) get the new cervical cancer vaccine (HPV vaccine) for their daughters if it were free (see Table 3). Some parents were not sure (7.2%), and only 1.2% said probably or definitely not.
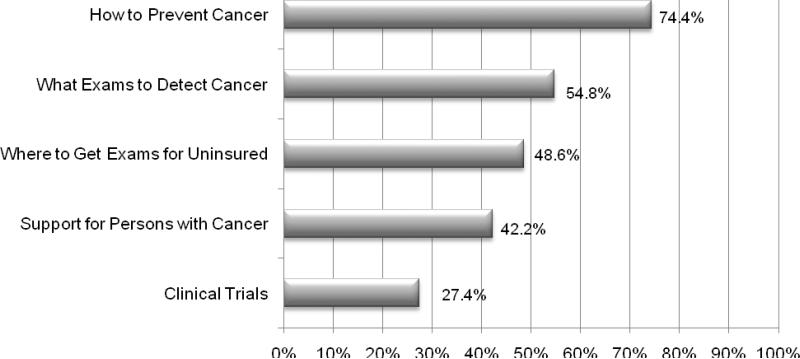
Desired information about cancer
Three-fourths of participants (74.4%) indicated that they would like more information on how to prevent cancer, and just over half (54.8%) wanted information on where to get cancer screening (see Figure 3). Nearly half (48.6%) wanted information on the availability of screening services for uninsured individuals, and slightly less wanted information on support for persons with cancer (42.2%). Just over one-fourth of participants (27.4%) indicated that they would like more information about cancer clinical trials.
Figure 3.
Desired Information about Cancer
Ethnic media
Nearly all (95.8%) respondents reported that they use at least one form of Spanish language media (see Table 4). Specifically, 70.6% watch a local Spanish television station, 74.0% read a local Spanish newspaper, and 77.5% listen to a Spanish radio station. In addition, almost half (47.6%) use all three forms of Spanish language media.
Table 4.
Ethnic Media Use
| Form of Local Spanish-Language Media | N | % |
|---|---|---|
| Television | 351 | 70.6 |
| Newspaper | 368 | 74.0 |
| Radio | 385 | 77.5 |
| At least one media | 479 | 95.8 |
| All three media | 238 | 47.6 |
Community dissemination of results
Preliminary survey results were presented to NHLC for input on interpretation of findings and to begin using the data to guide planning efforts. For example, the ranking of health concerns informed NLHC's development of a bilingual health resource guide designed for uninsured Hispanics in the Nashville area. The survey results were disseminated to NHLC and the local community through a bilingual presentation and a printed report in November 2007. At this presentation, the PCC interviewers and TSU student interviewers were recognized for their hard work and contributions. The COC and NLHC have used the results to advance through subsequent stages of the CBPR process.
Discussion
Discussion of survey findings
Lack of health insurance among Nashville Hispanics (79.5%) was higher than national rates for Hispanics and other groups, which in 2007 was 32.1% for Hispanics, 10.4% for non-Hispanic Whites, and 19.2% non-Hispanic Blacks.15 In addition to relatively low levels of education, over half of respondents reported that they spoke little or no English. This is substantially higher than the 28.3% of Spanish-speaking adults in the 2000 U.S. Census who reported that they spoke English “not well” or “not at all”.16 All of these characteristics likely reflect the fact that Nashville's Hispanic population is predominantly comprised of first-generation immigrants who are more likely to have no health insurance, lower education and lower English ability, compared to the Hispanic population at a national level that is comprised of a higher percentage of U.S.-born Hispanics.
The prevalence of current smoking among Nashville Hispanics (21.9%) was in between the national prevalence (19.8%) and Tennessee prevalence (24.3%) of current smoking in 2007.17 The prevalence of overweight and obesity very closely matched national prevalence data for Hispanics in 2007 (38.7% overweight and 26.7% obese), and were slightly higher than national prevalence for non-Hispanic Whites in the same year (36.7% overweight and 25.7% obese).18 Low consumption of fruits and vegetables was more common among Nashville Hispanics (91.7%) compared to the national prevalence of 75.6% of adults who consumed less than the recommended five servings a day in 2007.17 Low levels of leisure-time physical activity were more common in this sample (67.7%) compared to the national prevalence of 50.5% of adults who did not meet recommended physical activity levels.17
Cervical cancer screening in the past year was slightly higher among Hispanic women in the survey (65.9%) than the national rate of 60% in 2007.18 Mammography screening for breast cancer in the past year was lower in the survey sample (54.4%) than the 2006 national estimate of 61.2%.19 Colorectal cancer screening with colonoscopy was much lower in the survey sample (17.9%) than the national rate of 59% in 2006.18
Cancer ranked as the top health concern among Hispanic adults in Nashville, followed by work accidents, diabetes, and dental services. Indeed, three out of four respondents reported that they wanted more information on how to prevent cancer, and about half wanted more information about where to get cancer screening, in particular for the uninsured. In addition, Hispanic parents with daughters age 18 and under overwhelmingly indicated a positive attitude about the new HPV vaccine to prevent cervical cancer and willingness to get their daughters vaccinated. Furthermore, most Hispanic adults in Nashville indicated positive attitudes about cancer clinical trials, while some reported a lack of awareness about cancer clinical trials. Very little previous research has explored attitudes about the new HPV vaccine or attitudes about cancer clinical trials among Hispanics. Finally, the survey results suggested that the use of ethnic media is very important in the Nashville Hispanic community, with nearly all of respondents using Spanish-language newspapers, radio or television. This suggests an opportunity for Spanish-language media to be used as a communication channel for potential public health interventions.
Using the results to further the CBPR process
The COC, PCC and NLHC conducted the 2007 Hispanic Health in Nashville Survey as Phase 3 of the CBPR process described above, to assess the health needs and interests of the local Hispanic community. These partners have used the survey results to inform Phases 4 - 6 of the CBPR process and to continue on to subsequent phases. Phase 4 is to prioritize the community's needs and problems. PCC has led NLHC through a participatory strategic planning guided by the interests and concerns of Hispanic community members, with technical support from the academic partners. NLHC used the survey's ranking of top health concerns to prioritize the coalition's areas of focus. In the survey, the top health concerns were ranked as cancer, work accidents, diabetes, dental services, drugs, and services for the uninsured. With additional input from PCC members and consideration of resources available through NLHC organizations, NLHC has chosen to focus primarily on cancer, diabetes, and services for the uninsured, and secondarily on dental services/oral health, holding onto work accidents and drugs as potential focus areas in the future.
Phase 5 is to define the specific problem area of focus for intervention within these priority areas, and Phase 6 is to develop the intervention and research methodology. In the area of cancer, NLHC decided to focus first on cervical cancer for several reasons (Phase 5). First, the survey showed that the Hispanic population in the Nashville area is young, with about 75% of the adult population under age 40. Cervical cancer tends to affect women at younger ages than breast cancer or prostate cancer in men. Cervical cancer screening using Pap smears is recommended for women starting at age 18 or initiation of sexual activity, compared with mammography starting at age 40 or colorectal and prostate cancer screening starting at age 50.18 Thus, coalition members felt that NLHC could make a larger impact in the local community by focusing on cervical cancer. Second, PCC members participating in NLHC have indicated strong support for an emphasis on prevention, both primary prevention (preventing a disease) and secondary prevention (early detection), because previous research by our team members has shown that Hispanic community members without insurance are largely concerned about avoiding major chronic diseases that would entail high health care costs or even potentially interfere with one's ability to work.13 NLHC members felt that the survey results resonated with this perception by showing a low rate of insurance coverage.
Third, three-fourths of the surveyed adults wanted more information on how to prevent cancer, and about half wanted information on detection of cancer. NLHC members felt that it made sense to focus on cervical cancer because the new HPV vaccine exists as a method of primary prevention, and the Pap smear is effective for both primary and secondary prevention. Finally, cervical cancer is one of the areas of health disparities for Hispanics. Incidence of new cervical cancer cases is double for Hispanic women and the mortality rate is 50% higher in Hispanic women compared with non-Hispanic White women.20,21 Therefore, the coalition's work could contribute new knowledge to the evidence base on effective ways to reduce ethnic disparities in cervical cancer.
NLHC used the survey results of the survey and input from PCC members to develop an intervention strategy and methodology (Phase 6). The survey showed great interest in the HPV vaccine among parents and high use of Spanish-language media. Furthermore, anecdotal evidence from PCC members suggested that there was negligible awareness in the Nashville Hispanic community about the existence of the new HPV vaccine and the fact that it is available for free for girls who are on Medicaid, uninsured, or underinsured. The survey findings and input from PCC members led NLHC to plan a culturally-appropriate social marketing campaign for the Hispanic community focused on cervical cancer prevention through the HPV vaccine using Spanish-language media. NLHC members TSU and PCC obtained funding from TSU in 2008 for a small formative research project to begin the process of intervention development.22 Results from the 2007 Hispanic Health in Nashville Survey were combined with data collected through focus groups to develop the intervention.
Based on the formative research results, NLHC collaborated with academic partners from TSU, Meharry, and Vanderbilt and with PCC to submit a pilot project proposal to the Meharry-Vanderbilt-TSU Cancer Partnership. This proposal was selected for funding a two-year pilot study (2009-2011) of the social marketing intervention to increase HPV vaccine utilization among Hispanic girls. This pilot project is currently being implemented (Phase 7). The pilot study involves a collaboration among TSU, Meharry, Vanderbilt, PCC, Hispanic community members through PCC, the local public health department, several community health centers, and local Spanish-language media. The Meharry-Vanderbilt-TSU Cancer Partnership's Community Outreach Core continues to support the implementation of this project with NLHC through technical assistance and resources.
Implications for cancer disparities in Hispanics
Cancer is the second leading cause of death for the overall population and for Hispanics in the US, accounting for about 20% of all deaths. However, disparities in incidence and mortality from various types of cancer exist across racial/ethnic groups. While Hispanics have lower incidence rates for all cancers combined compared to whites, they have higher rates of cancers associated with infections, including cancers of the cervix, uterus, liver, gallbladder, and stomach.23 In addition, breast cancer is more frequently diagnosed at a later stage among Hispanic women than in non-Hispanics. Hispanics are also more likely than non-Hispanic Whites to die from cervical, stomach, and liver cancers.21,23
A combination of economic, social, and cultural factors contributes to racial/ethnic disparities in health status.24-26 Cancer mortality rates are higher for people with low incomes and low education compared with those having greater incomes and education.23 Both across and within racial/ethnic groups, low income and education influence the prevalence of underlying risk factors for cancer (e.g., tobacco use and obesity), access to general medical care, and access to high quality cancer prevention, early detection, and treatment services. Since Hispanics and African Americans are more likely than non-Hispanic Whites to live below the poverty line and to lack health insurance, they are at greater risk of late-stage cancer diagnosis and generally have lower survival rates.23,27-28 Social inequities, such as discrimination, can also affect risk for cancer (e.g., stress levels) as well as access to and quality of care.24,29
Recent immigrants face additional risk factors for cancer incidence and survival, such as greater exposure to infections linked to certain cancers, language barriers and cultural differences in health behaviors and beliefs. There are a number of unique social, cultural, and economic challenges facing Hispanics that can contribute to cancer disparities, including immigration status, cultural beliefs about cancer, comfort level in discussing it, and a sense of fatalism (“it's in God's hands”), limited Spanish media outlets, lack of insurance coverage, low health care access to preventive care, low levels of literacy (in English and Spanish) and lack of information and awareness. CBPR provides an approach that can help overcome a number of these barriers by engaging persons at risk for or affected by cancer to inform the ways interventions are shaped, participants recruited, and information disseminated. The participatory needs assessment reported here demonstrated that engaging community members in the research process increases the likelihood that interventions and strategies can be developed that address these concerns.
Study limitations
The main limitation of the survey was that the sample was a convenience sample and not a probability sample. This limits our ability to perform statistical tests and to generalize results to the larger population. Other limitations were not gathering information on household income or the exact number of refusals to participate in the survey. However, the convenience sample is useful for the purposes of describing the needs and concerns of the Hispanic community to guide intervention planning. Further, the similarities between the sample characteristics and Census bureau estimates of the Hispanic population in Davidson County suggest that the sample does not appear to be biased and mirrors the Hispanic population reasonably well.
Conclusion
Collaboration among the Partnership's Community Outreach Core, PCC, and NLHC led to the implementation of the 2007 Hispanic Health in Nashville Survey as a CBPR project. This participatory needs assessment survey facilitated the academic and community partners in NLHC to advance through subsequent phases of the CBPR process, leading to funding of a formative research project to develop an intervention, and then to funding a pilot intervention study aimed at reducing cervical cancer disparities among Hispanic women. The academic and community partners in NLHC will jointly analyze and interpret the results of the ongoing pilot study of the HPV vaccine intervention (Phase 8), reflect on the policy implications of the results (Phase 9), and disseminate the results to the local community, the scientific community, and the public health community (Phase 10). Finally, assuming that the HPV intervention is successful, NLHC will explore mechanisms for sustainability of the intervention program through additional funding and/or institutionalization, and for expansion of the study to other geographical regions (Phase 11).
This study contributes to the scant literature regarding the participation of Hispanics in research. In this project, members of the Hispanic community were partners in the research team, their needs and concerns were built into the methodology, and their feedback indicated that participating in the research was a positive experience. The CBPR process used successfully by these partners and the results of this survey demonstrates the benefits of engaging community members in the research process.
Acknowledgments
This research was supported by Grant No. 2 U54 CA091408 from National Cancer Institute, National Institutes for Health, and by a Faculty Research Award from Tennessee State University (TSU). In addition to the research team members who are listed as co-authors, we would like to thank the TSU student assistants (Veronica Melendez and Rosalina Moore) and the volunteer community interviewers who were trained and collected surveys (Irma Criollo, Enrique Segura, Dora Guerrero, Fernando I., Andrea Bachus, Isaura Gonzalez, and others). We would also like to thank Yvonne Joosten and Richard Ramker of the Nashville Latino Health Coalition for their support and contributions.
Contributor Information
Pamela C. Hull, Director of the Ctr. for Health Research at Tennessee State University (TSU) in Nashville, Tenn.
Juan R. Canedo, Director of Progreso Community Center, a non-profit organization, in Nashville.
Michelle C. Reece, Center for Health Research at TSU..
Irma Lira, member of Progreso Community Center..
Francisco Reyes, member of Progreso Community Center..
Erandi Garcia, member of Progreso Community Center..
Paul Juarez, Family and Community Medicine and Vice Chair Academic Affairs at Meharry Medical College (MMC)..
Elizabeth Williams, Director of Minority Affairs at the Vanderbilt-Ingram Cancer Center.
Baqar A. Husaini, Sociology and Director of the Center for Health Research at TSU..
REFERENCES
- 1.Israel BA, Schulz AJ, Parker EA, et al. Review of community-based research: assessing partnership approaches to improve public health. Ann Rev Public Health. May. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 2.Mittelmark MB, Hunt MK, Heath GW, et al. Realistic outcomes: lessons from community-based research and demonstration programs for the prevention of cardiovascular diseases. J Public Health Policy. Winter. 1993;14(4):437–62. [PubMed] [Google Scholar]
- 3.Steuart GW. Social and cultural perspectives: community intervention and mental health. Health Educ Q. 1993;20(suppl. 1):S99–S111. doi: 10.1177/10901981930200s109. [DOI] [PubMed] [Google Scholar]
- 4.Susser M. The tribulations of trials-intervention in communities. Am J Public Health. Feb. 1995;85(2):156–8. doi: 10.2105/ajph.85.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Cancer Institute . NCI strategic plan for leading the nation to eliminate the suffering and death due to cancer. National Cancer Institute, National Institutes of Health, & Department of Health and Human Services; Bethesda, MD: 2006. [Google Scholar]
- 6.Viswanathan M, Ammerman A, Eng E, et al. Community-based participatory research: assessing the evidence. AHRQ; Rockville, MD: 2004. (Pub. No. 04-E022-2.) [PMC free article] [PubMed] [Google Scholar]
- 7.Minkler M, Wallerstein N. Community-based participatory research for health. 1st ed. Jossey-Bass; San Francisco: 2003. [Google Scholar]
- 8.O'Fallon L, Tyson F, Dearry A. Successful models of community-based participatory research. National Institute of Environmental Health Sciences; Research Triangle Park, NC: 2000. [Google Scholar]
- 9.Cunningham P, Banker M, Artiga S, et al. Health coverage and access to care for Hispanics in “new growth communities” and “major Hispanic centers”. Henry J. Kaiser Family Foundation; Washington, DC: 2006. [Google Scholar]
- 10.Kochhar R, Suro R, Tafoya S. The new Latino south: the context and consequences of rapid population growth. Pew Hispanic Center; Washington, D.C.: 2005. [Google Scholar]
- 11.Census Bureau US. American FactFinder: 2005-2007 American Community Survey 3-year estimates, Custom Table: 2009. U.S. Census Bureau; Washington, D.C.: Available at: http://factfinder.census.gov. [Google Scholar]
- 12.Capps R, Fix ME, Passel J. The Dispersal of Immigrants in the 1990s. Urban Institute, Immigration Studies Program; Washington, DC: 2002. [Google Scholar]
- 13.Hull PC, Canedo JR, Aguilera J, et al. Assessing community readiness for change in the Nashville Hispanic community through participatory research. Progress in Community Partnerships for Health. Fall. 2009;2(3):185–194. doi: 10.1353/cpr.0.0032. [DOI] [PubMed] [Google Scholar]
- 14.SPSS for Mac. SPSS Inc.; Chicago: Rel. 11.0.1. 2001. [Google Scholar]
- 15.DeNavas-Walt C, Proctor BD, Smith JC. U.S. Census Bureau, Current Population Reports, P60-235. U.S. Government Printing Office; Washington, D.C.: 2008. Income, poverty, and health insurance coverage in the United States: 2007. [Google Scholar]
- 16.U.S. Census Bureau . Language use and English-speaking ability: 2003. U.S. Census Bureau; Washington, DC: (Census 2000 Brief C2KBR-29) Available at: http://www.census.gov/prod/2003pubs/C2KBR-29.pdf. [Google Scholar]
- 17.Tennessee Department of Health and Tennessee State University Center for Health Research . The burden of heart disease and stroke in Tennessee. Tennessee Department of Health; Nashville, TN: 2010. (In Press) [Google Scholar]
- 18.Centers for Disease Control and Prevention . Behavioral risk factor surveillance system: prevalence and trends data. Centers for Disease Control; Atlanta, GA: 2009. Available at: http://apps.nccd.cdc.gov/brfss. [Google Scholar]
- 19.American Cancer Society . Cancer prevention and early detection facts and figures 2009. American Cancer Society; Atlanta, GA: 2009. [Google Scholar]
- 20.American Cancer Society . Cancer facts and figures for Hispanics/Latinos. American Cancer Society; Atlanta, GA: 2006. [Google Scholar]
- 21.Ries AG, Harkins D, Krapcho M, et al. SEER cancer statistics review, 1975-2003. National Cancer Institute; Bethesda, MD: 2006. [Google Scholar]
- 22.Hull PC, Canedo JR. Formative research for social marketing campaign to increase HPV vaccine use among Hispanic girls.. Presented at: Social Marketing in Public Health Conference; Clearwater Beach (FL). 2009. [Google Scholar]
- 23.American Cancer Society . Cancer facts and figures 2009. American Cancer Society; Atlanta, GA: 2009. [Google Scholar]
- 24.Institute of Medicine (IOM) Unequal treatment: Confronting racial and ethnic disparities in health care. National Academy Press; Washington, DC: 2002. [Google Scholar]
- 25.Kawachi I, Kennedy BP, Lochner K, et al. Social capital, income inequality, and mortality. Am J Public Health. Sep. 1997;87(9):1491–8. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Ann Rev Sociol. 1995 Aug;21:349–386. [Google Scholar]
- 27.Brawley OW. Disaggregating the effects of race and poverty on breast cancer outcomes. J Natl Cancer Inst. April 3. 2002;94(7):471–473. doi: 10.1093/jnci/94.7.471. [DOI] [PubMed] [Google Scholar]
- 28.National Center for Health Statistics . Health, United States, 2006 with chartbook on trends in the health of Americans. U.S. Public Health Service; Hyattsville, MD: 2006. [PubMed] [Google Scholar]
- 29.Collins C, Williams DR. Segregation and mortality: the deadly effects of racism? Sociological Forum. Sept. 1999;14(3):495–523. [Google Scholar]