Introduction
Blindness continues to be one of the major public health problems in developing countries. Cataract and corneal diseases are major causes of blindness in countries with less-developed economies.(1) According to the World Health Organization, corneal diseases are among the major causes of vision loss and blindness in the world today, after cataract and glaucoma.(2) In India, it is estimated that there are approximately 6.8 million people who have vision less than 6/60 in at least one eye due to corneal diseases; of these, about a million have bilateral involvement.(3,4) It is expected that the number of individuals with unilateral corneal blindness in India will increase to 10.6 million by 2020.(4) According to the National Programme for Control of Blindness (NPCB) estimates, there are currently 120,000 corneal blind persons in the country. According to this estimate there is addition of 25,000-30,000 corneal blindness cases every year in the country.(5) The burden of corneal disease in our country is reflected by the fact that 90% of the global cases of ocular trauma and corneal ulceration leading to corneal blindness occur in developing countries.(6)
Materials and Methods
As corneal blindness is a major public health problem and the status is expected to change over time, there is a need to periodically review the published literature on the subject. An extensive Medline and Google search was performed, including websites of the National Programme for Control of Blindness, World Health Organization, Eye Bank Association of India, etc. The literature database was searched till October 2011. The terms, “corneal blindness and population-based surveys in India”; “visual impairment and corneal diseases”; “prevalence of corneal blindness”; “causes of unilateral and bilateral corneal blindness and morbidity in India” were used to locate papers on the subject in any language published 1991 onwards, covering about two decades up to the present. The abstract of each of these publications was reviewed; full papers that were actually related to corneal blindness and its causes in India were obtained from the journals.
Results
Magnitude of corneal blindness
Table 1 illustrates various community-based studies conducted in India and the burden of corneal blindness from 1987 through 2010.(4,7,8,9,10,11,12,13,14,15,16,17,18) A metaanalysis of seven relevant population-based studies published from 2001 to 2010 was performed [Table 2]. These studies were selected as comparable data on corneal blindness (similar methodology, age group, definition of blindness, type of population) could be retrieved from all seven studies. Full papers and reports of these population-based surveys were extensively studied to include a uniform definition of blindness (defined as “presenting visual acuity less than 6/60 in the better eye” in all seven studies included) and population aged 50 years and above only. This was done to obtain homogenous studies for analysis with similar inclusion criteria for metaanalysis. In the first stage of metaanalysis, the prevalence of corneal blindness with its 95% confidence intervals (CIs) was calculated for each individual study. In the second stage of metaanalysis, an overall prevalence of corneal blindness was calculated as a weighted average of individual summary statistics. The metaanalysis was conducted on Stata 12.0 (Stata Corporation, College Station, TX, USA). The forest plot [Figure 1] thus generated demonstrates that the true prevalence of corneal blindness in the Indian population is 0.45% (95% CI: 0.27-0.64%). The prevalence of unilateral corneal blindness and corneal opacities as estimated by population-based surveys is depicted in Tables 3 and 4, respectively.(19,20,21) The pattern of corneal blindness reported from hospital-based data is depicted in Table 5.(22,23)
Table 1.
Magnitude and causes of corneal blindness in India (community-based studies)
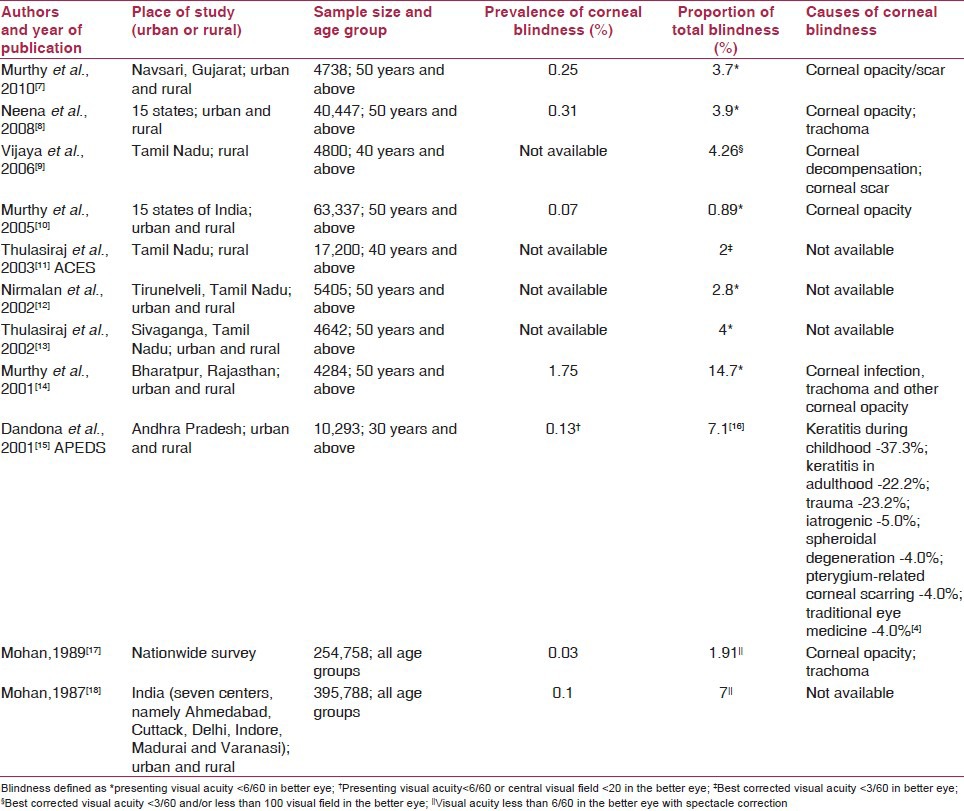
Table 2.
Community-based studies on corneal blindness included for metaanalysis*
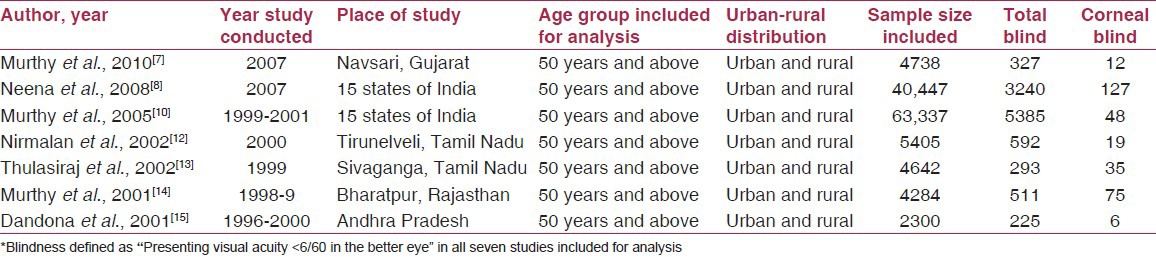
Figure 1.
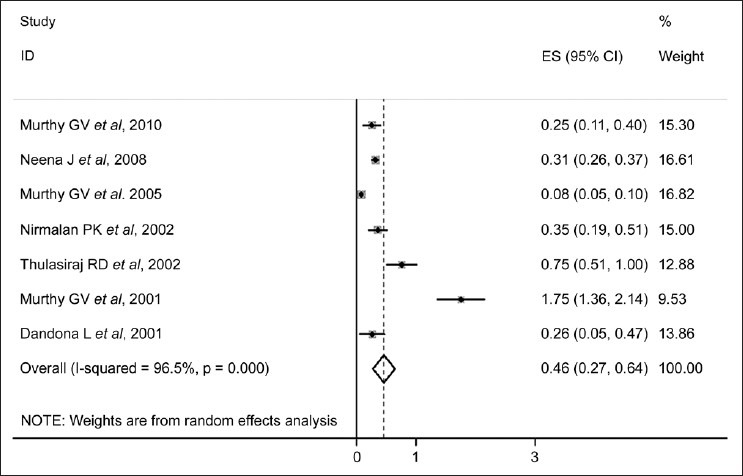
Forest plot demonstrating prevalence of corneal blindness in India
Table 3.
Magnitude of unilateral corneal blindness in India (community-based studies)
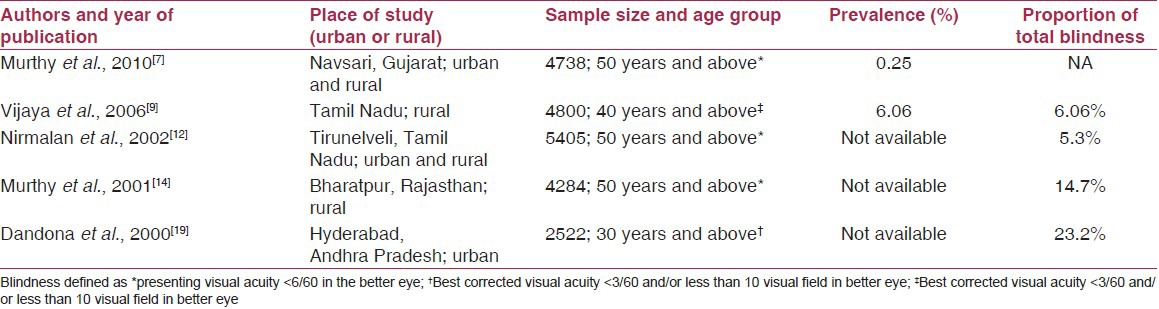
Table 4.
Magnitude of corneal opacities in India (community-based studies)
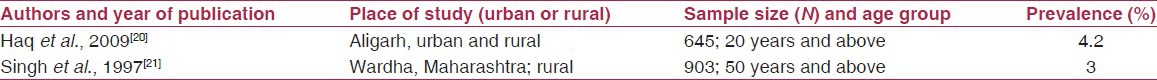
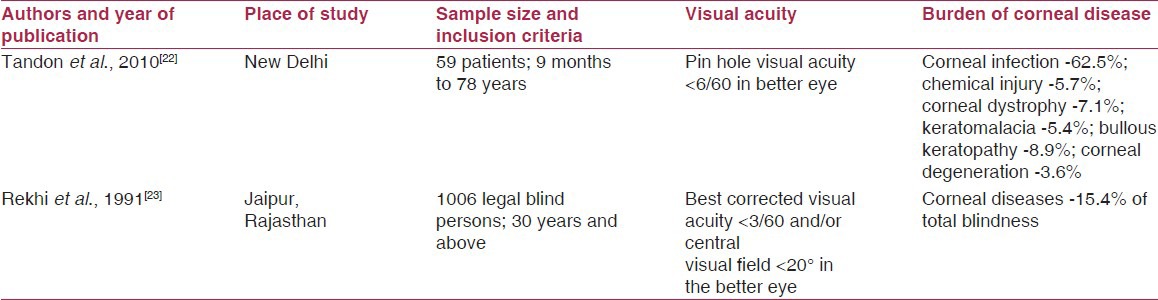
Table 5.
Magnitude and causes of corneal blindness in India (hospital-based studies)
Bilateral and unilateral corneal blindness
Corneal blindness and severe visual impairment due to corneal diseases (5.96 lakh unilateral blind and 1.91 lakh bilateral blind) as estimated by NPCB-WHO (National Programme for Control of Blindness-World Health Organization) (1986-9) are considered conservative figures based on several other indirect estimates.(24) It is estimated that approximately 20,000 patients with corneal blindness are being added to the backlog each year.(24) There is a tendency of sequential involvement of the other eye in majority of the cases with unilateral corneal blindness.(22)
Avoidable corneal blindness
The term avoidable encompasses preventable and treatable causes. The Andhra Pradesh Eye Disease Study reported that a significant burden of corneal blindness in the rural population of Andhra Pradesh was avoidable.(15) Of the 0.66% prevalence of corneal blindness in at least one eye in this population, nearly 95% was avoidable. The avoidable causes of corneal blindness reported in this study were keratitis in childhood, trauma, aphakic bullous keratopathy, severe astigmatism post cataract surgery, keratitis in adulthood and traditional eye medicines.
Corneal conditions amenable to primary prevention include measles infection, Vitamin A deficiency, ophthalmia neonatorum, trachoma, ocular trauma, the use of harmful traditional eye medication remedies and congenital rubella syndrome. Corneal blindness resulting due to these diseases can be completely prevented by institution of effective preventive or prophylactic measures at the community level.
Treatable or curable blindness can be tackled by an effective and accessible health care service delivery network. In cases such as corneal ulceration and selected cases of corneal scarring, sight can be restored with timely and prompt management. The prompt diagnosis and appropriate treatment of corneal ulceration and the easy availability of antibiotics and anti-fungals, even in rural areas, should be the aim of community health programs. Many of those currently blind from corneal diseases can be visually rehabilitated by corneal transplantation. Penetrating keratoplasty is the most effective and most often performed solid organ transplantation. It is estimated that 50% of corneal blindness is treatable.(25)
The economic burden due to corneal blindness has not been extensively studied. It has been estimated that if strategies are implemented successfully to prevent 90% of the preventable blindness due to corneal disease by 2020, blindness in an additional 3.6 million persons in 2020 and 29 million blind-years would be prevented.(26)
As most of the corneal blindness is preventable, and because surgical intervention for treating corneal blindness is a difficult option in a developing country setting, the need for effective health promotion strategies takes paramount importance. Prevention and early treatment will prove to be more viable and cost-effective in the long term in reducing the burden of corneal blindness in our country.
Causes of corneal blindness in India
Corneal blindness encompasses a range of eye conditions that alter the transparency of the cornea, leading to corneal scarring and, eventually, blindness. Causes of corneal blindness include a wide variety of infections and inflammatory eye diseases, ranging from keratitis, xerophthalmia, eye trauma, trachoma, congenital disease and traditional eye medicine or home remedies, which often harm the eye rather than relieve pain or improve eyesight.(27)
The causal factors responsible for corneal blindness vary with age. Significant causes of corneal blindness (based on indications of keratoplasty) in adults residing in countries with less-developed economies are corneal scars (28.1%) and active keratitis (12.2%).(1) In the pediatric age group, the most common indication for keratoplasty in the developing world has been reported to be acquired non-traumatic scars (71.32%).(28,29)
Childhood blindness and visual loss due to corneal diseases is important because of its significant impact on the child's development, education, future job opportunities and quality of life.(30) Xerophthalmia and ophthalmia neonatorum were important causes of corneal blindness in children.(31) It is estimated that approximately half of all childhood blindness in India is preventable or treatable, to which Vitamin A-associated corneal blindness is a significant contributor.(32) In a population-based assessment of childhood blindness involving 1,13,514 children less than 16 years of age in the West Godavari district of Andhra Pradesh, corneal opacity was responsible for 11.1% of the total burden of blindness in children.(33) A study involving 1318 blind children of various blind schools across nine states in the country reported that corneal diseases accounted for 26% of children with severe visual impairment or blindness (presenting visual acuity less than 6/60 in the better eye).(34) The causes of corneal scarring were Vitamin A deficiency (19%), measles in 3%, ophthalmia neonatorum in 1%, harmful traditional eye medicines in 1% and trauma and keratitis in the remaining 3%.(34) In a retrospective, hospital-based study conducted in Darjeeling, 23.8% (30 of 126) cases of visual loss in children were due to corneal diseases.(35) In another studyconducted in four states of the North Eastern region (N = 258), corneal blindness was the most common cause of severe visual impairment and blindness in children (36.7%) and the major preventable cause identified.(36) In a study conducted in 35 blind schools of Maharashtra between 2002 and 2005 (N = 1985), 22.2% children had visual loss due to corneal scarring; nearly one-third of all the children included in the study were blind from preventable or treatable causes.(37) Corneal diseases contributed to 14.9% (133/ 891) of childhood blindness in the blind schools of Karnataka, 21.7% (N = 703) of blindness/severe visual impairment in the blind schools of Delhi, 24.3% (N = 291) of blindness/severe visual impairment in six blind schools of Andhra Pradesh, 38.4% (N = 305) in a study from South India and 26.4% (N = 1318) in a multi-state blind school study in India.(38,39,40,41,42) Thus, the available data indicates that corneal scarring due to Vitamin A deficiency has been a major cause of childhood blindness in our country.
In India, ocular trauma, infectious keratitis, corneal ulceration and post-infectious keratitis corneo-iridic scars contribute significantly to pediatric ocular morbidity. Congenital corneal disorders are also an important cause of childhood blindness that usually result from hereditary dystrophies, congenital glaucoma, Peter's anomaly and other mesenchymal dysgenesis, birth trauma and metabolic disorders.
In adults, the major causes of corneal blindness include bacterial, fungal or viral keratitis, hereditary corneal dystrophy and eye injuries. The proportion of people aged over 60 years is growing faster than any other age group as a result of longer life expectancy and advancements in healthcare technology. The major causes of corneal morbidity in the elderly include trachomatous keratopathy, corneal degenerations and trauma-induced infectious keratitis. A study involving 102 consecutive cases of microbial keratitis in patients 65 years and older demonstrated that the principal predisposing factors for corneal ulceration in this age group were ocular disease (38.2%), previous ocular surgery in the same eye (29.4%), trauma (17.6%) and severe systemic disease (16.7%).(43) Thus, the risk factors responsible for corneal ulceration in the elderly may differ from those prevalent in the general population.
Etiological classification
- Infections
- Infectious keratitis
- Trachoma
- Nutritional disorders
- Vitamin A deficiency (xerophthalmia)
- Inherited
- Corneal dystrophies
- Trauma
- Corneal abrasion predisposing to microbial keratitis
- Penetrating trauma
- Chemical injury
- Iatrogenic
- Pseudophakic bullous keratopathy
Infectious keratitis
Corneal ulceration is a significant cause of corneal blindness.(6) With the worldwide decrease in trachoma and other traditional causes of blindness, such as onchocerciasis and leprosy, the World Health Organization has recognized that corneal blindness resulting from microbial keratitis is emerging as an important cause of visual disability.(44) Corneal ulceration has been recognized as a silent epidemic in developing countries, especially the South-east Asia Region.(45) By extrapolation of Indian estimates of the incidence of corneal ulcer, approximately 1.5-2 million people develop corneal ulcer annually in our country. Gonzales et al. estimated that the annual incidence of corneal ulceration in Madurai District of South India was 1130 per million population.(46)
The spectrum of microbial keratitis varies with geographical location, influenced by the local climate and occupational risk factors. Corneal blindness due to infectious keratitis has been more commonly reported in the rural population, particularly in those belonging to the lower socioeconomic strata and those who are illiterate with poor knowledge about proper eye care.(23) Mycotic keratitis is more common in the tropics and sub-tropical regions, and the major precipitating factor is trauma, followed by prior application of corticosteroids and traditional eye medicine.(47) In a hospital-based study on epidemiological profile of fungal keratitis, agriculture-related ocular trauma was the principal cause (70.3%) of mycotic keratitis.(48) Even though India has a heterogeneous population, the agents causing infective keratitis have been known to be the same since several decades. Fortunately, there has not been much shift in the spectrum of bacteria and fungi as etiological agents.(49)
Trauma is often the most significant precipitating factor for development of infectious keratitis. In a study from South India, corneal injury was identified as a cause of infective keratitis in 70.88% (2256 of 3183) patients.(50) As reported by Gopinathan et al., patients with agriculture-based activities were at 1.33-times (95% CI 1.16-1.51) greater risk of developing microbial keratitis and patients with ocular trauma were 5.33-times (95% CI 6.41-6.44) more likely to develop microbial keratitis.(51) Similarly, a hospital-based study from West Bengal reported that ocular trauma was the most common predisposing factor for development of microbial keratitis in 994 (82.9%) patients, followed by use of topical corticosteroids in 231 (19.28%) patients.(52)
The use of traditional eye medicines (e.g., dried plant materials crushed into powder and dissolved in an aqueous medium; animal/human products such as breast milk, saliva, urine, etc.) is an important risk factor for corneal ulceration in many developing countries. The use of traditional eye medicines is a public health problem in many developing countries, including India, and an important risk factor for corneal blindness. The traditional eye medicines are often contaminated and usually lead to delay in proper therapy. They also serve as a vehicle or culture media for spread and growth of pathogenic organisms. They may also cause corneal damage by their toxic effect. In a study from South India, patients with Acanthamoeba keratitis had used human milk, goat milk, castor oil and leaves extract as popular traditional eye medicines in eyes already compromised by injury or infection.(53) A study designed to document the prevalence of use of traditional eye medicines among patients with a predominantly rural background and presenting with corneal ulcer to a tertiary care center in India revealed that breast milk was the most common traditional medicine used.(54) In this study, traditional eye medicines were more commonly used by patients with a history of trauma; hence, health education and awareness about primary eye care following trauma needs to be created in our community. Traditional healers need to be educated and their cooperation must be sought in order to direct patients to appropriate health care facilities so that corneal blindness due to use of traditional eye medicines may be prevented.
The most common predisposing cause of corneal ulceration in the pediatric age group was trauma with organic matter (69%) as demonstrated by a retrospective analysis of hospital records in a tertiary eye care center of South India.(55) In another study, involving 113 eyes of 107 children with microbial keratitis in Hyderabad, India, the principal predisposing factors were trauma (21.2%), ocular disease (17.7%), systemic disease (15.9%) and prior penetrating keratoplasty in the same eye (8.8%). Vitamin A deficiency was an important factor within the category of severe systemic disease.(56) In cases of atraumatic microbial keratitis involving pre-school children, severe protein-energy malnutrition and incomplete immunization were reported to be significantly associated with the occurrence of bilateral keratitis.(57)
In the context of a developing country with a predominantly rural population, antibiotic and antifungal treatment available for microbial keratitis is relatively costly and the visual outcome post keratitis is almost invariably poor. Srinivasan et al. have now demonstrated that prevention of infective keratitis is feasible and cost-effective within the existing healthcare system.(58) According to them, village-level workers can effectively implement and sustain a corneal ulcer prevention programme at the village level by simple public health strategies. A guideline for managing infective keratitis at all levels was developed by an expert group for the South East Asian Region at the initiation of the World Health Organization meet at New Delhi in 2004.(59) Moreover, corneal transplantation in the scarred, vascularized tissue following a severe corneal infection is rarely successful. Hence, preventive control measures will prove to be more successful and cost-effective in decreasing the prevalence of blindness due to these diseases.
Trachoma
Trachoma is the leading cause of infectious blindness in the world.(44) It is currently estimated that, globally, there are about 1.3 million people blind from the disease and a further 8.2 million have trichiasis.(60) The most recent estimate by the World Health Organization estimated that the global burden of trachoma amounts to nearly 1.3 million disability-adjusted life years.(60) Estimated assessments of active trachoma and trachomatous trichiasis in India were updated in 2007, and the data revealed an average prevalence of active trachoma as 6% in children under 10 years of age, resulting in 4.5 million cases with trachoma, when applied to the five endemic states of Gujarat, Rajasthan, Uttar Pradesh (inclusive of Uttarakhand), Haryana and Punjab.(61) A study conducted in previously hyperendemic areas of Western Uttar Pradesh revealed declining trends in the magnitude of trachoma (33.7% in 1978 to 8.5% in 1998).(62) In rural Haryana, previously hyperendemic regions were surveyed and it was concluded that trachoma had ceased to be a public health problem in these areas of the country.(63) Because India is one of the most populous countries in the world, and trachoma prevalence in this region could make a profound difference to the global burden of trachoma, a coordinated effort to conduct population-based surveys with a national sampling frame is needed.
Trachoma-related blindness is preventable by implementing an integrated plan of action to eliminate trachomatous blindness through the SAFE strategy.(64) This approach includes Surgery for trichiasis, Antibiotic treatment of clinically active chlamydial infection, promotion of Facial cleanliness and improvement of Environmental conditions in the endemic region. Once trachomatous keratopathy has occurred, keratoplasty is the only choice of restoring vision in these patients. The outcome of penetrating keratoplasty in trachoma patients is often disappointing due to extensive corneal vascularization and consequent graft rejection, ocular surface problems and the invariable presence of entropion and trichiasis in these cases. It is essential, therefore, to prevent corneal blindness from occurring by instituting trachoma prevention programmes in trachoma-prone regions of the country.
Vitamin A deficiency (xerophthalmia)
Vitamin A deficiency is the single most frequent cause of blindness among pre-school children in developing countries.(65) In a recent study involving 3571 children under 5 years of age from rural and periurban areas of Aligarh, the overall prevalence of xerophthalmia was of serious public health importance at 9.1%, which was significantly associated with malnutrition and comorbidities in these children.(66) More emphasis needs to be laid on prevention and massive dose supplementation, fortification of common foodstuffs with Vitamin A, immunization, control of precipitating infections and dietary improvement to combat this public health problem effectively.(67)
Population-based assessment of childhood blindness in the state of Andhra Pradesh revealed corneal disease to be responsible for 17% of childhood blindness, half (8.3%) of which could be attributed to Vitamin A deficiency disorders.(32) A study involving 1318 blind children of various blind schools across nine states in the country reported varied causes of childhood blindness in different states on priority basis, e.g., Vitamin A deficiency contributed to 26.7% in Madhya Pradesh, whereas it was responsible for only 7.5% of childhood blindness in the state of Kerala.(34) The study demonstrated that, overall, Vitamin A deficiency was the single most important cause (19%) of childhood blindness and severe visual impairment in India. There were also marked regional variations in the magnitude of Vitamin A deficiency disorders between the states and within the state, with an urban-rural gradient varying from 8% to 30%.(34)
Corneal dystrophy
Corneal dystrophies are a heterogenous group of inherited corneal diseases that are more commonly reported as cause of corneal blindness in the developed world. A hospital-based study in South India reported that corneal dystrophy was responsible for 8.1% (144 patients) of all keratoplasty performed. The main types of corneal dystrophy encountered in this population were macular corneal dystrophy, congenital hereditary endothelial dystrophy, Fuchs dystrophy and lattice dystrophy.(68)
Trauma
Trauma is often the most significant cause of unilateral loss of vision in developing countries,(6) and up to 5% of all bilateral blindness has been attributed to direct ocular trauma.(69) Corneal and corneoscleral perforation and subsequent scarring due to ocular trauma may result in a variable amount of blindness.
Chemical injuries with acids and alkali contribute significantly to corneal blindness in the younger age group. In a study from North India, 43 of 102 patients suffered bilateral injuries and nearly 45% of the eyes had severe-grade burns. Occupational exposure contributed to a majority of the injuries in this study.(70)
Penetrating injuries remain an important cause of acquired corneal scarring in the pediatric age group. In a study involving 204 children below 14 years of age, the most common cause of injury was bow and arrow (15.2%), followed by household appliances (14.3%).(71) Most ocular injuries in children are preventable and occur from unsupervised activities, which can lead to significant visual loss.
Epidemiological community-based studies on ocular trauma have been conducted in various distinct populations of the country. In the urban slums of Delhi, the prevalence of ocular trauma in 6704 participants was 2.4%. Blunt trauma was the most common mode of injury (41.7%), and contributed to blindness in 11.4% of the eyes.(72) In the rural population of Andhra Pradesh, 824 of 7771 (10.6%) subjects reported having sustained ocular trauma. The most common mode of injury (45.3%) in this population was trauma with vegetative matter.(73) Likewise, nearly 5% people above 40 years of age were affected with ocular trauma in a rural population of Tamil Nadu. Blunt trauma in an agricultural setting was the most frequent cause of trauma in this population.(74) In the urban population of South India, the prevalence of ocular trauma was 3.97%, with majority of trauma resulting in blindness occurring during childhood and young adulthood.(75) Eye care programs and strategies targeting high-risk ocular trauma groups need to be developed in our country in order to reduce blindness due to trauma.
Pseudophakic/Aphakic bullous keratopathy
The etiology of pseudophakic bullous keratopathy is varied and depends largely on the surgical technique used for cataract extraction. The incidence of pseudophakic bullous keratopathy is on the increase as we strive to eliminate avoidable blindness due to cataract. With the increasing cataract surgical rate in India and because more intraocular lenses being implanted, a large number of eyes are at risk of going blind due to corneal decompensation. In a study involving 2022 penetrating keratoplasties performed in a tertiary eye care center in North India, bullous keratopathy accounted for 13.5% of all operated cases.(76) In cataract-related corneal edema, aphakic bullous keratopathy (7.27%) was almost as frequent as pseudophakic bullous keratopathy (6.18%). Visual rehabilitation after keratoplasty is compromised in these cases due to a high incidence of graft failure contributed by increased intraocular pressure.(77)
Conclusion
In aiming to eliminate corneal blindness, a multi-pronged strategy needs to be developed. In a country with limited resources and a vast population, optimization of available facilities and prioritization of healthcare commitments need to be proportioned rationally. Control of preventable causes requires extensive public support and community participation. It falls in the realm of public health. Curable or treatable blindness requires a spectrum of care, including medication, optical rehabilitation and corneal transplantation. Overall, continued assessment of the burden of corneal blindness with periodic review of trends is required to effectively plan preventive, promotive and rehabilitative blindness control strategies.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Garg P, Krishna PV, Stratis AK, Gopinathan U. The value of corneal transplantation in reducing blindness. Eye (Lond) 2005;19:1106–14. doi: 10.1038/sj.eye.6701968. [DOI] [PubMed] [Google Scholar]
- 2.Causes of blindness and visual impairment. [Last accessed on 2011 October 30]. Available from: http://www.who.int/blindness/causes/en .
- 3.National Programme for Control of Blindness. Report of National Programme for Control of Blindness, India and World Health Organization. 1986-89 [Google Scholar]
- 4.Dandona R, Dandona L. Corneal blindness in a southern Indian population: Need for health promotion strategies. Br J Ophthalmol. 2003;87:133–41. doi: 10.1136/bjo.87.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Programme for Control of Blindness. [Last accessed on 2011 October 30]. Available from: http://pbhealth.gov.in/pdf/Blindness.pdf .
- 6.Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: A global perspective. Bull World Health Organ. 2001;79:214–21. [PMC free article] [PubMed] [Google Scholar]
- 7.Murthy GV, Vashist P, John N, Pokharel G, Ellwein LB. Prevalence and causes of visual impairment and blindness in older adults in an area of India with a high cataract surgical rate. Ophthalmic Epidemiol. 2010;17:185–95. doi: 10.3109/09286586.2010.483751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neena J, Rachel J, Praveen V, Murthy GV Rapid assessment of avoidable blindness india study group. Rapid Assessment of Avoidable Blindness in India. PLoS One. 2008;3:e2867. doi: 10.1371/journal.pone.0002867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vijaya L, George R, Arvind H, Baskaran M, Raju P, Ramesh SV, et al. Prevalence and causes of blindness in the rural population of the Chennai glaucoma study. Br J Ophthalmol. 2006;90:407–10. doi: 10.1136/bjo.2005.081406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murthy GV, Gupta SK, Bachani D, Jose R, John N. Current estimates of blindness in India. Br J Ophthalmol. 2005;89:257–60. doi: 10.1136/bjo.2004.056937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thulasiraj RD, Nirmalan PK, Ramakrishnan R, Krishnadas R, Manimekalai TK, Baburajan NP, et al. Blindness and vision impairment in a rural south Indian population: The aravind comprehensive eye survey. Ophthalmology. 2003;110:1491–8. doi: 10.1016/S0161-6420(03)00565-7. [DOI] [PubMed] [Google Scholar]
- 12.Nirmalan PK, Thulasiraj RD, Maneksha V, Rahmathullah R, Ramakrishnan R, Padmavathi A, et al. A population based eye survey of older adults in Tirunelveli district of south India: Blindness, cataract surgery, and visual outcomes. Br J Ophthalmol. 2002;86:505–12. doi: 10.1136/bjo.86.5.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thulasiraj RD, Rahamathulla R, Saraswati A, Selvaraj S, Ellwein LB. The sivaganga eye survey: I. Blindness and cataract surgery. Ophthalmic Epidemiol. 2002;9:299–312. doi: 10.1076/opep.9.5.299.10334. [DOI] [PubMed] [Google Scholar]
- 14.Murthy GV, Gupta S, Ellwein LB, Munoz SR, Bachani D, Dada VK. A population-based eye survey of older adults in a rural district of Rajasthan: I. Central vision impairment, blindness, and cataract surgery. Ophthalmology. 2001;108:679–85. doi: 10.1016/s0161-6420(00)00579-0. [DOI] [PubMed] [Google Scholar]
- 15.Dandona L, Dandona R, Srinivas M, Giridhar P, Vilas K, Prasad MN, et al. Blindness in Indian state of Andhra Pradesh. Invest Ophthalmol Vis Sci. 2001;42:908–16. [PubMed] [Google Scholar]
- 16.Dandona R, Dandona L. Review of findings of the Andhra Pradesh eye disease study: Policy implications for eye-care services. Indian J Ophthalmol. 2001;49:215–34. [PubMed] [Google Scholar]
- 17.Mohan M. New Delhi: Ministry of health and family welfare, government of India; 1989. National survey of blindness-India. NPCB-WHO Report. [Google Scholar]
- 18.Mohan M. New Delhi, India: Indian Council of Medical Research; 1987. Collaborative study on blindness (1971-1974): A report; pp. 1–65. [Google Scholar]
- 19.Dandona L, Dandona R, Srinivas M, Mandal P, McCarty CA, Rao GN. Unilateral visual impairment in an urban population in southern India. Indian J Ophthalmol. 2000;48:59–64. [PubMed] [Google Scholar]
- 20.Haq I, Khan Z, Khalique N, Amir A, Jilani FA, Zaidi M. Prevalence of common ocular morbidities in adult population of Aligarh. Indian J Community Med. 2009;34:195–201. doi: 10.4103/0970-0218.55283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh MM, Murthy GV, Venkatraman R, Rao SP, Nayar S. A study of ocular morbidity among elderly population in a rural area of central India. Indian J Ophthalmol. 1997;45:61–5. [PubMed] [Google Scholar]
- 22.Tandon R, Sinha R, Moulick P, Agarwal P, Titiyal JS, Vajpayee RB. Pattern of bilateral blinding corneal disease in patients waiting for keratoplasty in a tertiary eye care centre in northern India. Cornea. 2010;29:269–71. doi: 10.1097/ICO.0b013e3181b6104e. [DOI] [PubMed] [Google Scholar]
- 23.Rekhi GS, Kulshreshtha OP. Common causes of blindness: A pilot survey in Jaipur, Rajasthan. Indian J Ophthalmol. 1991;39:108–11. [PubMed] [Google Scholar]
- 24.Saini JS, Reddy MK, Jain AK, Ravindra MS, Jhaveria S, Raghuram L. Perspectives in eye banking. Indian J Ophthalmol. 1996;44:47–55. [PubMed] [Google Scholar]
- 25.Eye Donation. NPCB India Newsletter. 2010. Jul-Sep. [Last accessed on 2011 October 30]. Available from: http://npcb.nic.in/writereaddata/mainlinkfile/File200.pdf .
- 26.Dandona L, Dandona R, John RK. Estimation of blindness in India from 2000 through 2020: Implications for the blindness control policy. Natl Med J India. 2001;14:327–34. [PubMed] [Google Scholar]
- 27.Burton MJ. Corneal blindness prevention, treatment and rehabilitation. [Last accessed on 2011 October 30];Community Eye Health Journal. 2009 71:33–5. Available from: http://www.cehjournal.org/indian/journal/21/jceh_21_68_s115.html . [PMC free article] [PubMed] [Google Scholar]
- 28.Dada T, Sharma N, Vajpayee RB. Indications for pediatric keratoplasty in India. Cornea. 1999;18:296–8. doi: 10.1097/00003226-199905000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Aasuri MK, Garg P, Gokhale N, Gupta S. Penetrating keratoplasty in children. Cornea. 2000;19:140–4. doi: 10.1097/00003226-200003000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Dandona L, Gilbert CE, Rahi JS, Rao GN. Planning to reduce childhood blindness in India. Indian J Ophthalmol. 1998;46:117–22. [PubMed] [Google Scholar]
- 31.Thylefors B, Négrel AD, Pararajasegaram R, Dadzie KY. Global data on blindness. Bull World Health Organ. 1995;73:115–21. [PMC free article] [PubMed] [Google Scholar]
- 32.Dandona R, Dandona L. Childhood blindness in India: A population based perspective. Br J Ophthalmol. 2003;87:263–5. doi: 10.1136/bjo.87.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dandona L, Williams JD, Williams BC, Rao GN. Population-based assessment of childhood blindness in southern India. Arch Ophthalmol. 1998;116:545–6. [PubMed] [Google Scholar]
- 34.Rahi JS, Sripathi S, Gilbert CE, Foster A. Childhood blindness due to vitamin A deficiency in India: Regional variations. Arch Dis Child. 1995;72:330–3. doi: 10.1136/adc.72.4.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bagchi K, Bhattacharya S. The profile of visual loss in children--a retrospective study in a referral hospital in India. J Indian Med Assoc. 2006;104:366. 368, 370. [PubMed] [Google Scholar]
- 36.Bhattacharjee H, Das K, Borah RR, Guha K, Gogate P, Purukayastha S, et al. Causes of childhood blindness in the northeastern states of India. Indian J Ophthalmol. 2008;56:495–9. [PMC free article] [PubMed] [Google Scholar]
- 37.Gogate P, Deshpande M, Sudrik S, Taras S, Kishore H, Gilbert C. Changing pattern of childhood blindness in Maharashtra, India. Br J Ophthalmol. 2007;91:8–12. doi: 10.1136/bjo.2006.094433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gogate P, Kishore H, Dole K, Shetty J, Gilbert C, Ranade S, et al. The pattern of childhood blindness in Karnataka, South India. Ophthalmic Epidemiol. 2009;16:212–7. doi: 10.3109/09286580902999405. [DOI] [PubMed] [Google Scholar]
- 39.Titiyal JS, Pal N, Murthy GV, Gupta SK, Tandon R, Vajpayee RB, et al. Causes and temporal trends of blindness and severe visual impairment in children in schools for the blind in North India. Br J Ophthalmol. 2003;87:941–5. doi: 10.1136/bjo.87.8.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hornby SJ, Adolph S, Gothwal VK, Gilbert CE, Dandona L, Foster A. Evaluation of children in six blind schools of Andhra Pradesh. Indian J Ophthalmol. 2000;48:195–200. [PubMed] [Google Scholar]
- 41.Gilbert CE, Canovas R, Hagan M, Rao S, Foster A. Causes of childhood blindness: Results from west Africa, south India and Chile. Eye (Lond) 1993;7:184–8. doi: 10.1038/eye.1993.39. [DOI] [PubMed] [Google Scholar]
- 42.Rahi JS, Sripathi S, Gilbert CE, Foster A. Childhood blindness in India: Causes in 1318 blind school students in nine states. Eye (Lond) 1995;9:545–50. doi: 10.1038/eye.1995.137. [DOI] [PubMed] [Google Scholar]
- 43.Kunimoto DY, Sharma S, Garg P, Gopinathan U, Miller D, Rao GN. Corneal ulceration in the elderly in Hyderabad, South India. Br J Ophthalmol. 2000;84:54–9. doi: 10.1136/bjo.84.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844–51. [PMC free article] [PubMed] [Google Scholar]
- 45.Whitcher JP, Srinivasan M. Corneal ulceration in the developing world-a silent epidemic. Br J Ophthalmol. 1997;81:622–3. doi: 10.1136/bjo.81.8.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gonzales CA, Srinivasan M, Whitcher JP, Smolin G. Incidence of corneal ulceration in Madurai District, South India. Ophthalmic Epidemiol. 1996;3:159–66. doi: 10.3109/09286589609080122. [DOI] [PubMed] [Google Scholar]
- 47.Tilak R, Singh A, Maurya OP, Chandra A, Tilak V, Gulati AK. Mycotic keratitis in India: A five-year retrospective study. J Infect Dev Ctries. 2010;4:171–4. doi: 10.3855/jidc.309. [DOI] [PubMed] [Google Scholar]
- 48.Saha S, Banerjee D, Khetan A, Sengupta J. Epidemiological profile of fungal keratitis in urban population of West Bengal, India. Oman J Ophthalmol. 2009;2:114–8. doi: 10.4103/0974-620X.57310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Srinivasan M. Infective keratitis: A challenge to Indian ophthalmologists. Indian J Ophthalmol. 2007;55:5–6. doi: 10.4103/0301-4738.29487. [DOI] [PubMed] [Google Scholar]
- 50.Bharathi MJ, Ramakrishnan R, Meenakshi R, Padmavathy S, Shivakumar C, Srinivasan M. Microbial keratitis in South India: Influence of risk factors, climate, and geographical variation. Ophthalmic Epidemiol. 2007;14:61–9. doi: 10.1080/09286580601001347. [DOI] [PubMed] [Google Scholar]
- 51.Gopinathan U, Sharma S, Garg P, Rao GN. Review of epidemiological features, microbiological diagnosis and treatment outcome of microbial keratitis: Experience of over a decade. Indian J Ophthalmol. 2009;57:273–9. doi: 10.4103/0301-4738.53051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Basak SK, Basak S, Mohanta A, Bhowmick A. Epidemiological and microbiological diagnosis of suppurative keratitis in gangetic West Bengal, eastern India. Indian J Ophthalmol. 2005;53:17–22. doi: 10.4103/0301-4738.15280. [DOI] [PubMed] [Google Scholar]
- 53.Bharathi JM, Srinivasan M, Ramakrishnan R, Meenakshi R, Padmavathy S, Lalitha PN. A study of the spectrum of acanthamoeba keratitis: A three-year study at a tertiary eye care referral center in South India. Indian J Ophthalmol. 2007;55:37–42. doi: 10.4103/0301-4738.29493. [DOI] [PubMed] [Google Scholar]
- 54.Prajna VN, Pillai MR, Manimegalai TK, Srinivasan M. Use of traditional eye medicines by corneal ulcer patients presenting to a hospital in South India. Indian J Ophthalmol. 1999;47:15–8. [PubMed] [Google Scholar]
- 55.Singh G, Palanisamy M, Madhavan B, Rajaraman R, Narendran K, Kour A, et al. Multivariate analysis of childhood microbial keratitis in South India. Ann Acad Med Singapore. 2006;35:185–9. [PubMed] [Google Scholar]
- 56.Kunimoto DY, Sharma S, Reddy MK, Gopinathan U, Jyothi J, Miller D, et al. Microbial keratitis in children. Ophthalmology. 1998;105:252–7. doi: 10.1016/s0161-6420(98)92899-8. [DOI] [PubMed] [Google Scholar]
- 57.Jhanji V, Naithani P, Lamoureux E, Agarwal T, Sharma N, Vajpayee RB. Immunization and nutritional profile of cases with atraumatic microbial keratitis in preschool age group. Am J Ophthalmol. 2011;151:1035–40.e2. doi: 10.1016/j.ajo.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 58.Srinivasan M, Upadhyay MP, Priyadarsini B, Mahalakshmi R, Whitcher JP. Corneal ulceration in South-East Asia III: Prevention of fungal keratitis at the village level in South India using topical antibiotics. Br J Ophthalmol. 2006;90:1472–5. doi: 10.1136/bjo.2006.103028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guidelines for the management of corneal ulcer at primary, secondary and tertiary health care facilities in SEAR 2004: SEA/Ophthal/126 [Google Scholar]
- 60.Burton MJ, Mabey DC. The global burden of trachoma: A review. PLoS Negl Trop Dis. 2009;3:e460. doi: 10.1371/journal.pntd.0000460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mariotti SP, Pascolini D, Rose-Nussbaumer J. Trachoma: Global magnitude of a preventable cause of blindness. Br J Ophthalmol. 2009;93:563–8. doi: 10.1136/bjo.2008.148494. [DOI] [PubMed] [Google Scholar]
- 62.Current trends in trachoma in a previously hyperendemic area. The Trachoma Study Group. Indian J Ophthalmol. 1998;46:217–20. [PubMed] [Google Scholar]
- 63.Khanduja S, Jhanji V, Sharma N, Vashist P, Murthy GV, Gupta S, et al. Rapid assessment of trachoma among children living in rural northern India. Ophthalmic Epidemiol. 2009;16:206–11. doi: 10.3109/09286580902999389. [DOI] [PubMed] [Google Scholar]
- 64.Bailey R, Lietman T. The SAFE strategy for the elimination of trachoma by 2020: Will it work? Bull World Health Organ. 2001;79:233–6. [PMC free article] [PubMed] [Google Scholar]
- 65.Global prevalence of Vitamin A Deficiency. Micronutrient Deficiency Information System Working Paper No. 2. World Health Organization, United Nations Children Fund. [Last accessed on 2011 October 30]. Available from: http://www.who. int/nutrition/publications/micronutrients/vitamin_a_deficiency/WHO_NUT_95.3/en/index.html .
- 66.Sachdeva S, Alam S, Beig FK, Khan Z, Khalique N. Determinants of vitamin a deficiency amongst children in Aligarh district, Uttar Pradesh. Indian Pediatr. 2011;48:861–6. doi: 10.1007/s13312-011-0140-8. [DOI] [PubMed] [Google Scholar]
- 67.McLaren DS. Vitamin A deficiency disorders. J Indian Med Assoc. 1999;97:320–3. [PubMed] [Google Scholar]
- 68.Pandrowala H, Bansal A, Vemuganti GK, Rao GN. Frequency, distribution, and outcome of keratoplasty for corneal dystrophies at a tertiary eye care center in South India. Cornea. 2004;23:541–6. doi: 10.1097/01.ico.0000126324.58884.b9. [DOI] [PubMed] [Google Scholar]
- 69.Thylefors B. Epidemiological patterns of ocular trauma. Aust N Z J Ophthalmol. 1992;20:95–8. doi: 10.1111/j.1442-9071.1992.tb00718.x. [DOI] [PubMed] [Google Scholar]
- 70.Saini JS, Sharma A. Ocular chemical burns-clinical and demographic profile. Burns. 1993;19:67–9. doi: 10.1016/0305-4179(93)90104-g. [DOI] [PubMed] [Google Scholar]
- 71.Saxena R, Sinha R, Purohit A, Dada T, Vajpayee RB, Azad RV. Pattern of pediatric ocular trauma in India. Indian J Pediatr. 2002;69:863–7. doi: 10.1007/BF02723708. [DOI] [PubMed] [Google Scholar]
- 72.Vats S, Murthy GV, Chandra M, Gupta SK, Vashist P, Gogoi M. Epidemiological study of ocular trauma in an urban slum population in Delhi, India. Indian J Ophthalmol. 2008;56:313–6. doi: 10.4103/0301-4738.41413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Krishnaiah S, Nirmalan PK, Shamanna BR, Srinivas M, Rao GN, Thomas R. Ocular trauma in a rural population of southern India: The Andhra Pradesh eye disease study. Ophthalmology. 2006;113:1159–64. doi: 10.1016/j.ophtha.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 74.Nirmalan PK, Katz J, Tielsch JM, Robin AL, Thulasiraj RD, Krishnadas R, et al. Ocular trauma in a rural South Indian population: The Aravind comprehensive eye survey. Ophthalmology. 2004;111:1778–81. doi: 10.1016/j.ophtha.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 75.Dandona L, Dandona R, Srinivas M, John RK, McCarty CA, Rao GN. Ocular trauma in an urban population in Southern India: The Andhra Pradesh eye disease study. Clin Experiment Ophthalmol. 2000;28:350–6. doi: 10.1046/j.1442-9071.2000.00334.x. [DOI] [PubMed] [Google Scholar]
- 76.Sony P, Sharma N, Sen S, Vajpayee RB. Indications of penetrating keratoplasty in Northern India. Cornea. 2005;24:989–91. doi: 10.1097/01.ico.0000157406.34662.0f. [DOI] [PubMed] [Google Scholar]
- 77.Dandona L, Naduvilath TJ, Janarthanan M, Rao GN. Causes of corneal graft failure in India. Indian J Ophthalmol. 1998;46:149–52. [PubMed] [Google Scholar]


