Abstract
Research Question:
Use of community based volunteers, frequently reaching and counseling a selected group of prioritized families, can make a substantial difference in improving maternal and child care practices and in reducing child undernutrition.
Setting:
Program Rural Uttar Pradesh, India.
Study Design:
A comparison of baseline and endline surveys following 4 years of community based project intervention
Participants:
“At risk” undernutrition families comprising mothers of under twos, newlyweds, and severely undernourished children below 6 years.
Intervention:
Mapping and counseling of “at risk” families. Measuring impact on maternal-child care practices, underweight status.
Results:
Trained community mobilizers identified and counseled selected “at risk” families. Following 4 years of implementation in 907 villages of 8 blocks of four districts, significant improvement was noted in practices of early initiation of breastfeeding, feeding colostrum, timely introduction of complementary feeding, and washing the hands after defecation. Percentage of mothers exclusively breastfeeding at 6 months was only 2.1% with 78% receiving prelacteal feeds. A small increase in normal and mild malnutrition and a significant reduction of 43% in severe malnutrition was noted.
Conclusion:
Frequently counseling by accredited social health activists by focusing on selected defined “at risk” families of under twos and those with severe malnourished children could result in increasing acceptability of correct child health, feeding, and care practices and in contributing to improving nutritional status scenario.
Keywords: Accredited social health activists, at risk families, child feeding practices, community volunteers, inter-personal counseling, severe malnutrition, undernutrition
Introduction
Every 6th undernourished child in India lives in the state of Uttar Pradesh.(1) Almost every second child in the state is undernourished.(1,2,3) A state based study in 1999 revealed that preventive measures for influencing the serious and stagnant problem undernutrition need to concentrate in the first year of life itself since highest prevalence of underweight occurs in late infancy between 8 months and 11 months.(1,4) Moreover, a community based strategy based on the success reported by Thailand in South Asia,(5) was considered vital. A community based demonstration project was designed and implemented for 4 years in four districts located in three distinct regions of the state. Baseline and end line surveys were undertaken to assess the impact of the interventions.
Intervention Strategy
Following a baseline study in 2000, a demonstration Community Based Maternal and Child Health Nutrition (Community Based MCHN), referred commonly as “MCHN Project”, was launched in January 2001 in 907 villages located in 8 blocks of 4 districts of the state of Uttar Pradesh (Agra, Allahabad, Jhansi, and Varanasi) with a population of 1.33 m [Figure 1]. The objective of the project was to reduce underweight prevalence rate by 20% and severe malnutrition by 50% in children below 2 years. Each district, project was managed by a team of persons from the Departments of Community Medicine, Based at the District Based Medical Colleges of the State Governments. A block trainer cum monitor (BTM) was appointed for each of the blocks.
Figure 1.
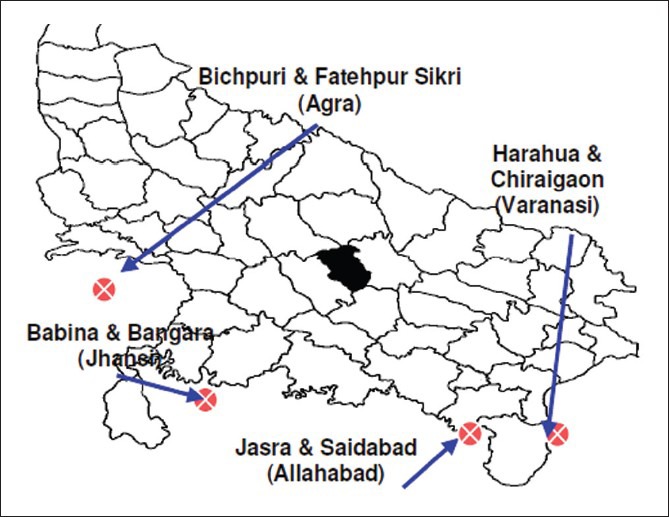
The MCHN project blocks (districts) of Uttar Pradesh state
The project strategy focused on selecting village-wise community cluster mobilizers for mapping and counseling selected families who were considered “at risk of malnutrition” — commonly referred as “at risk” families. The criteria for “at risk” families was defined as those households with any of the following conditions — family having at least one child below 24 months of age or a child below 6 years with severe malnutrition or a pregnant/lactating mother or a newlywed woman. The newly married women were defined as those married for not more than 1 year who were not pregnant nor had a child. All pregnant women were considered “at risk of malnutrition” since this period is critical for interventions for reducing the incidence of low birth weight and for preparing mothers for self-care and child care and feeding.
The community based mobilizers, commonly referred as in local language as Bal Parivar Mitras (BPMs) meaning “friend of families with a young children” were volunteers selected and assigned the tasks of reaching the “at risk” families at least once a fortnight. Volunteers, preferably women, with a positive attitude and who were vocal, dynamic and respected were selected – one BPM for 50-60 households. Clusters in communities were mapped on the basis of religion, caste, geographical location in a village and selection was based on consensus emerging from cluster community dialogues organized by BTMs in the presence of frontline workers of health and Integrated Childe Development Services (ICDS) i.e., Auxillary Nurse-midwifes (ANMs) and Aanganwadi Workers (AWWs).
Each BPM worked at a time with only the identified 15-20 “at risk families” within the group of 50-60 allocated households. The primary responsibility of these volunteers was to visit homes of identified families and counsel them on adoption of appropriate maternal and child care and feeding practices and create demands for child health and Antenatal Care (ANC) Services. Right advice at the right time to the right recipient or family was the principle applied in the interpersonal counseling sessions conducted by the BPMs. Simple pictorial counseling cum monitoring family cards were developed and used to help BPMs in counseling as well as in maintaining family-wise records of actions taken on counseling as well as adoption of practices.
For reduction of severely malnourished (SM) children, the BPMs were trained to screen SM children of under 6 years on the basis of selected clinical signs since availability of weighing scales was rather poor. Skill training was an imparted to BPMs to identify children who looked apathetic and disinterested and appeared extremely wasted or underweight — often with the very little subcutaneous fat or muscle or disproportionately larger head with discolored or very little hair or protruding abdomen. Identified SM cases were referred to ANMs or the Primary Health Center. Home level feeding of such children 6-7 times per day with the following local culturally accepted calorie dense foods was advised — mashed dalbhat (rice and pulse with added oil/ghee) or khichari (well-cooked and soft pulse-dal mixture cooked in fat/oil) or kheer (rice-milk-sugar mashed with additional oil or animal fat). The feeding was monitored by BPMs every 7-10 days.
BPMs also mobilized the “at risk families’ to avail of ANC and routine immunization (RI) services, use of Oral rehydration salt (ORS), vitamin A supplements and use of iodized salt. Washing hands with soap and water after defecation and daily use of iodized salt was also promoted.
A 3 day intensive pre-service training, with emphasis on selected messages and their rationale as well as counseling skills, was followed by half day training at the sub-center village level for a batch of 15-20 BPMs during the quarterly monitoring meetings. A specially, designed case study based training manual in the format of case studies was developed and used. A six panel pictorial card was used for monitoring and for conducting in service training. Understanding and completing the simple monitoring format was a central part of the training since this formed the primary tool for counseling as well as monitoring. No printed information, education and communication materials other than the pictorial counseling cum monitoring cards were used for the project.
The BPMs received no honorarium or salary but fees of INR 100 (about US $ 2.00) per day for initial 3 days training, annual 1 day district review meeting as well as 4 times a year following checking of completed family level monitoring pictorial cards at the quarterly monitoring meetings with the Block coordinator of the Medical Colleges. Additionally, social recognition and high level motivation was ensured by providing a badge with a project logo, a large name plate for the house, a cloth bag for carrying monitoring forms and the training manual as well as a certificate following completion of training. BPMs were provided with a stock of supply ORS packets and salt testing kits.
The profile of BPMs was studied through the project records. The impact of the 4 year intervention was assessed by comparing the baseline survey findings of July-December 2000 with an end-line survey conducted in April-May 2005, following 4 months of the closure of the project in December 2004. The total population of the 8 project blocks was 1,331,549 with total fertility rate of the state being 3.99 with underweight prevalence rate of under three children being 52%. For both these surveys, mothers of under 2 years were interviewed — 4952 mothers in the baseline and 1601 in the end-line. For household practices, 239 newly-weds were interviewed at the end line survey. Children under 2 years were weighed using the solar scale provided by State Government. Nutritional status was measured using the weight for age criteria and using the Indian Academy of Pediatrics (IAP) classification, which was in use at that period by the Government of India. Conversion of all the data to WHO 2006 classification was not possible in the absence of required raw baseline data. This therefore remained a limitation of the study. The data of baseline and end-line surveys were compared using the Epistat package and application of appropriate statistical tests.
Results
In a period of 4 years, 5816 BPMs were selected and trained in 8 blocks of 4 districts. Of these 97.6% were females and 67.6% were in the age group of 18-40 years. The dropout rate in the project period varied between 5.8% and 15.5% in the four districts.
The findings revealed that BPMs were the primary source of information for influencing promotion of child feeding or maternal care practices with health and ICDS workers AWWs playing a negligible role [Table 1]. A significant improvement in the three critical Infant and Young Child Feeding practices – initiation of breastfeeding within 1 h of birth (increased from 4.6% to 21.9%), feeding colostrum (baseline 27.9% to end-line 52.9%) and timely introduction of semi-solid foods between 6 months and 9 months (increased from 18.2% at baseline to 62.6% at the end-line) was observed [Table 2]. The end-line survey revealed that the practice of exclusively breastfeeding for the first 6 months remained extremely low despite frequent counseling by community volunteers [Figure 2]. The three primary patterns of breastfeeding were as follows – never breastfed (1.3%), initiated breastfeeding only after the introduction of pre-lacteals (78%) and initiated feeding with only breast milk (22%). In both groups of mothers, who fed pre-lacteals or not, there was a sharp drop in the practice of breastfeeding after the first month [Figure 3]. Fifty percent of 1601 women contacted during the survey were aware that exclusive breastfeeding is the correct practice for the first 6 months of infancy while only 2.1% practiced it. This trend was attributed to the strong cultural belief in the community that breast milk secretion of mothers has been often insufficient and should be supplemented with animal milk from 1 month onwards.
Table 1.
Source responsible for imparting information on various behavioral practices and services to “at risk” families
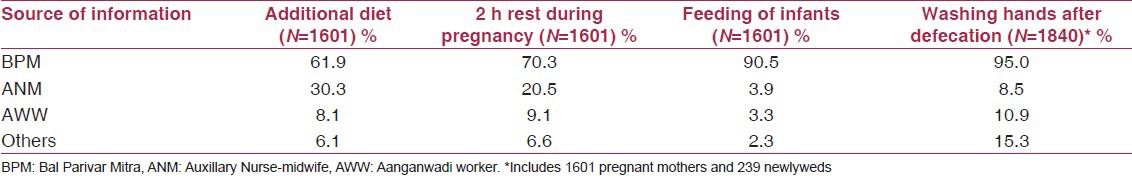
Table 2.
Impact on breastfeeding and complementary feeding practices
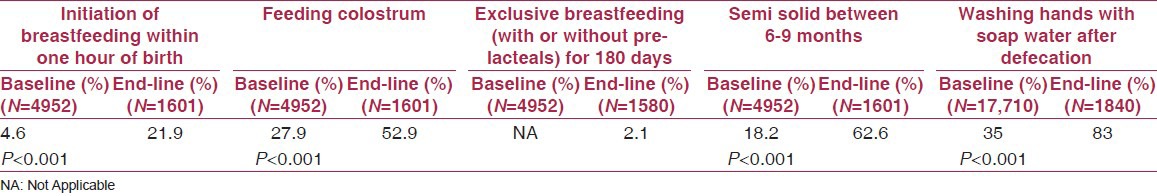
Figure 2.
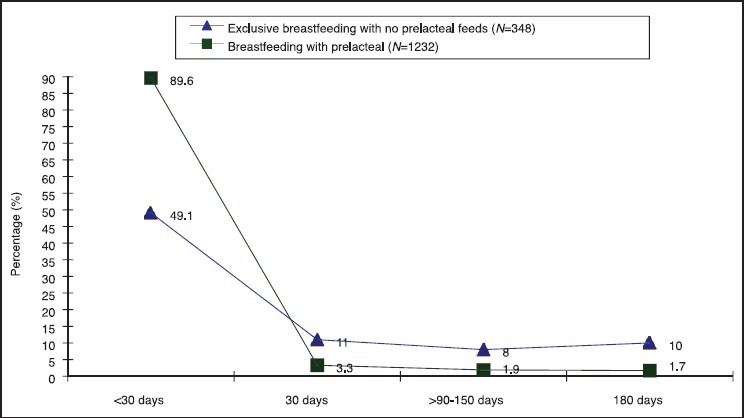
Trends in the pattern of exclusive breastfeeding practices in children fed pre-lacteals and not fed pre-lacteals
Figure 3.
Nutritional status (underweight) of children <2 years of age at baseline and endline surveys
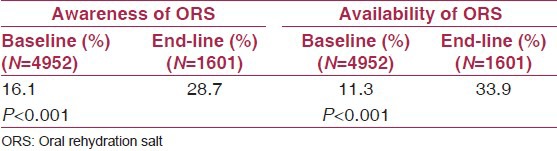
Following counseling, a very significant increase was noted in the practice of washing of hands with soap and water after defecation — 34.8% at baseline to 83.2% at the end-line [Table 3]. A significant three-fold increase in awareness regarding use of ORS as well as availability of ORS packets were noted [Table 3]. Counseling of “at risk” families and easy access to ORS packets contributed to a significant increase use of ORS packets. Despite emphasis that feeding should be continued during diarrhea, 58.7% mothers reported being following the incorrect practice of reducing the quantity of feed and breastfeeding during the diarrhea.
Table 3.
Awareness of benefits of use of ORS during diarrhoea and availability of ORS packets
The end-line survey also revealed that the project resulted in over 60% mothers being aware of significance of gaining 8-10 kg weight and the importance of consuming additional diet during the pregnancy [Table 4]. However, counseling by BPMs resulted in only a fifth (18%) of mothers following the practice of taking additional diet despite the fact that three fifths were aware of its importance. The primary reasons stated for not taking extra diet by 707 women interviewed were loss of appetite (48.4%), feeling of heaviness and indigestion (35.2%) and fear that additional diet will compress baby (16.1%) and family resistance for such a practice (2.7%). There was no baseline data for comparison.
Table 4.
Impact on behavioral practices and health services
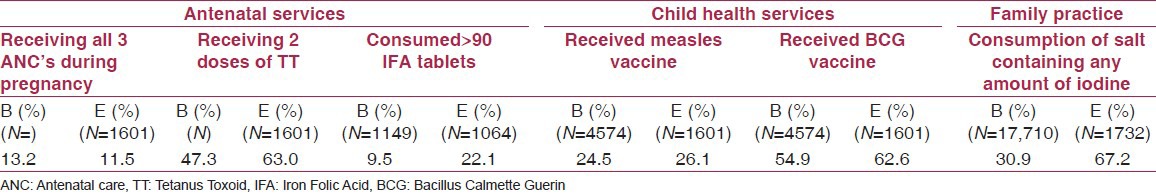
The coverage of the ANC services, RI, vitamin A, and iodized salt availability is presented in Table 4. The coverage remained low since the health and ICDS systems were engaged in Pulse Polio Drive and often could not respond to the demands generated.
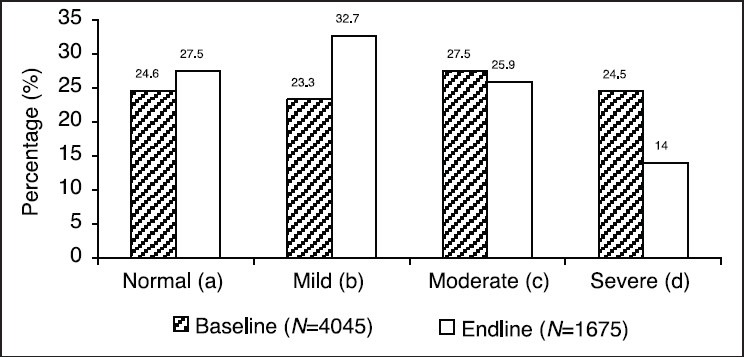
The impact on nutritional status of children less than 2 years was assessed using the IAP classification. Against the project objective of 50%, a statistically significant decrease of 43% in severe underweight children was recorded – from 24.5% at baseline to 14.0% at the end-line survey [Figure 2]. The increase in percentage of children with normal weight was only 11.8% but was significant [Figure 2]. The decrease in percentage of moderate underweight was only 3.9%, and the difference was statistically non-significant.
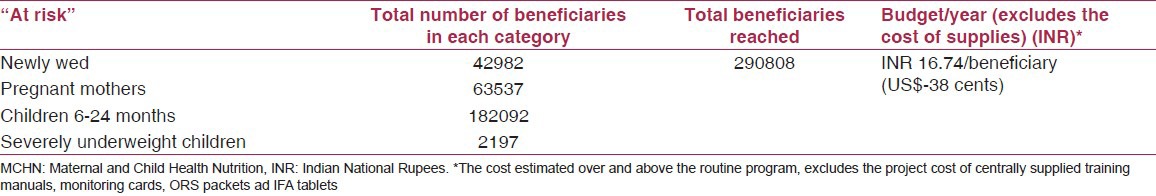
The additional cost incurred in the project in terms of training, monitoring, including monitoring fees to BPMs was studied for one of the 4 projects — Allahabad [Table 5]. The findings reveal that the additional cost incurred over and above the routine system was INR 16.74 (US $0.38)/beneficiary/year.
Table 5.
Allahabad district MCHN project–estimated annual cost/beneficiary
Discussion
Community based mobilizers were effective in reaching the “at risk” families and influencing behavioral practices. The current strategy of a volunteer focusing on only 20 families “at risk” of malnutrition increased the scope of volunteers reaching more frequently and concentrating only on those families where advice given was relevant to the family situation and had higher possibility of acceptability. Moreover, higher frequency also contributes in building a good rapport with families and in enhancing acceptance of specific behavioral changes by families with a less resistance. Similar ratio of community volunteers to households of 1:15 - 0.20 was reported to be effective in Thailand.(5)
In a period of 4 years, a remarkable decrease of 43% in severely underweight children below 2 years and 11.8% increase in normal weight children was observed. Moderate underweight remained rather stagnant since a substantial upward shift to moderate grade from severe grade of undernutrition (SU) was evident. Similar decrease of 44% was observed in Tamil Nadu Integrated Project I following a 5 years intervention targeting a specific age group of 6-36 months with a package of interventions comprising growth monitoring, food supplementation for 90 days and nutrition education.(6) Dular project of Jharkhand, with a rather high annual cost of $16 per child, reported a similar decrease of 45% in SU under 3 years children but with not much difference in the percentage of normal weight children.(7) The present finding concurs with an earlier report that intensive nutrition education in the absence of provision of supplementary feeding contributes to reduction of malnutrition.(8) The findings also highlight that practices of child feeding and hand washing can be influenced with frequent interactions with families of under twos. Improvement in hygiene practices observed appear to have contributed significantly in the prevention of malnutrition as has been reported earlier.(9)
The sharp decline noted in exclusive breastfeeding practice after 30 days of feeding reconfirms the need for nutrition education to address the common strong traditional belief that there is insufficient milk secreted by most of the mothers after 30-40 days since the mothers appear weak and thin. This is evident from the median duration of exclusive breastfeeding reported in the 2000 India survey to be between 1.7 months and 2.1 months.(3) In the absence of a simple indicator such as average frequency of urination or any other tool which can be used by mothers themselves to assess the sufficiency of milk secreted, the counseling per se on benefits of exclusive breastfeeding is ineffective in convincing mothers for continuing with exclusive breastfeeding for the first 6 months of life. Moreover, such interpersonal counseling efforts need to be complemented with multiple media channel actions for generating community support and influencing public opinion for overcoming the strong cultural practices of introduction of milk other than breast milk in the first 6 months of life.(10)
Identification and feeding advice to clinical “visible” cases of severe malnutrition appears to incite the interest of community in relating inappropriate child feeding to the problem of malnutrition as well as in building confidence in community volunteers. Such a strategy therefore, facilitates in generating family interest in child care practices and in higher acceptance of advice on appropriate child feeding practices by community volunteers. Involving community volunteers in the identification and care of cases of severe acute malnutrition (SAM); therefore, needs to be considered as a useful entry point for promotion of appropriate child feeding practices. Moreover, such a strategy is desirable since it is well-documented that 80% children with SAM, identified through active case finding or through sensitizing and mobilizing communities can be treated at home.(11)
Conclusion
The MCHN project was launched in 2001 while the Government of India launched the National Rural Health Mission in April 2005 with the introduction of a cadre of community volunteers referred as accredited social health activists (ASHAs).(12,13) The lessons learned from the MCHN project findings reveal that ensuring frequent home visits of ASHAs with a focus on selected “at risk” families of under twos could accelerate the process of reduction of undernutrition by improving coverage of 10 essential evidence based services which comprises interventions pertaining to improving child feeding practices, maternal-child health services such as RI, ANC, vitamin A supplementation and management of SAM.(14,15,16)
Acknowledgment
The program was supported by the State Government of Uttar Pradesh and UNICEF. The author, ex-UNICEF Nutrition Project Officer, would like to thank late Dr. Bachhi Lal, ex — Director of General Health and Family Welfare Services, Government of Uttar Pradesh (GoUP) for providing overall guidance in the finalization of the project design. The implementation of the Project by the Community Medicine Departments of the Medical College Teams of Agra, Allahabad, Jhansi, and Varanasi is acknowledged along with special appreciation of leadership and monitoring support provided by the following faculty of the departments — Prof. Deoki Nandan, SN Medical Collge, Agra. Prof. Sadhu C. Mohapatra MD, Institute of Medical Sciences, Banaras Hindu University, Prof. Shraddha Dwivedi, MLN Medical College, Allahabad, and Prof. Shyam B Gupta MD, Maharani Laxmi Bai Medical College, Jhansi. The support of Ms. Ritu Jain and Ms Richa Malik, Research Nutritionist, Public Health Nutrition and Development Center, New Delhi, is appreciated for their contribution in statistical analysis and presentation of this manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Lucknow, U.P: UNICEF; 2001. Nutrition Profile of Uttar Pradesh, Government of Uttar Pradesh and UNICEF. [Google Scholar]
- 2.International Institute for Population Science (IIPS) ORC Macro, National Family Health Survey (NFHS-2), 1998-99. India. 1999 [Google Scholar]
- 3.International Institute for Population Science (IIPS) ORC Macro, National Family Health Survey (NFHS-3), 2005-06. India. 2007 [Google Scholar]
- 4.Vir SC. NFI Bulletin; 2001. Jan, 2001 Nutritional status of children in Uttar Pradesh, Nutrition Foundation of India. [Google Scholar]
- 5.Tontisirin K, Winichagoon P. Community based programmes: Success factors for public nutrition derived from the experience of Thailand. Food Nutr Bull. 1999;20:315–22. [Google Scholar]
- 6.Heaver R. Washington DC: World Bank; 2002. India's Tamil Nadu nutrition program: Lessons and issues in management and capacity. Health, Nutrition and Population (HNP) Discussion Paper. [Google Scholar]
- 7.Dubowitz T, Levinson D, Peterman JN, Verma G, Jacob S, Schultink W. Intensifying efforts to reduce child malnutrition in India: An evaluation of the Dular program in Jharkhand, India. Food Nutr Bull. 2007;28:266–73. doi: 10.1177/156482650702800302. [DOI] [PubMed] [Google Scholar]
- 8.Roy SK, Fuchs GJ, Mahmud Z, Ara G, Islam S, Shafique S, et al. Intensive nutrition education with or without supplementary feeding improves the nutritional status of moderately-malnourished children in Bangladesh. J Health Popul Nutr. 2005;23:320–30. [PubMed] [Google Scholar]
- 9.Shahid NS, Greenough WB, 3rd, Samadi AR, Huq MI, Rahman N. Hand washing with soap reduces diarrhoea and spread of bacterial pathogens in a Bangladesh village. J Diarrhoeal Dis Res. 1996;14:85–9. [PubMed] [Google Scholar]
- 10.Bhandari N, Bahl R, Mazumdar S, Martines J, Black RE, Bhan MK, et al. Effect of community-based promotion of exclusive breastfeeding on diarrhoeal illness and growth: A cluster randomised controlled trial. Lancet. 2003;361:1418–23. doi: 10.1016/S0140-6736(03)13134-0. [DOI] [PubMed] [Google Scholar]
- 11.Collins S, Sadler K, Dent N, Khara T, Guerrero S, Myatt M, et al. Key issues in the success of community-based management of severe malnutrition. Food Nutr Bull. 2006;27:S49–82. doi: 10.1177/15648265060273S304. [DOI] [PubMed] [Google Scholar]
- 12.WHO/WFP/UNSCN/UNICEF. Community Based Management of Severe Acute Malnutrition [Google Scholar]
- 13.National Rural health Mission, Government of India. Ministry of Health and Family Welfare, Government of India. 2005 Apr [Google Scholar]
- 14.Swaminathan MS. Undernutrition in infants and young children in India: A leadership agenda for action. IDS Bull. 2009;40:103–10. [Google Scholar]
- 15.Ministry of Health and Family Welfare, Government of India; 2011. Ministry of Health and Family Welfare, Government of India. Operational Guidelines on Facility Based Management of Children with Severe Acute Malnutrition. [Google Scholar]
- 16.Menon P, Aguayo V. No. 3. Vol. 5. The World Bank; 2011. Jun, The 1000 day window of opportunity for improving child nutrition in India: Insights from national level data. India Health Beat, supporting evidence based policies and implementation. [Google Scholar]


