Abstract
Moxonidine is the newest, second-generation, centrally acting antihypertensive agent. It has selective agonist activity at imidazoline I1 receptors and less adverse effects than the other centrally acting drugs. This fact authorizes the frequent use of moxonidine in clinical practice, as monotherapy or in combination with other antihypertensive agents. Also, moxonidine has beneficial effects in obese and metabolic syndrome and in target-organs, such as heart and kidneys.
KEY WORDS: Moxonidine, organ protection, sympathetic nervous system
Moxonidine is a second-generation centrally acting antihypertensive drug [Figure 1].[1] It has selective agonist activity at imidazoline I1 receptors and only minor activity at imidazoline α-2 adrenoceptors.[2] Moxonidine reduce the activity of the sympathetic nervous system (SNS), because activates I1 imidazoline receptors in the rostal ventrolateral medulla (RVLM).[3] The result is the inhibition of peripheral alpha-adrenergic tone, and the decrease of blood pressure, due to a fall in systemic vascular resistant.[4] Moxinidine is used in patients with mild to moderate hypertension, as monotheraphy, or in combination with other antihypertensive agents.[2,5,6] A plenty of studies demonstrate that moxonidine acts on heart, a target-organ. This effect is achieved through the activation of cardiac I1 imidazoline receptors.[7] Through this mechanism, moxonidine produces clinically relevant sympatholysis, with beneficial effects on hemodynamics, coronary circulation, and neurohumoral parameters.[8] Also, studies indicated that moxonidine has antiarrhythmic reaction,[9] suppresses the activation of myocardial infarction, and reacts on postmyocardial infarction remodeling.[10]
Figure 1.
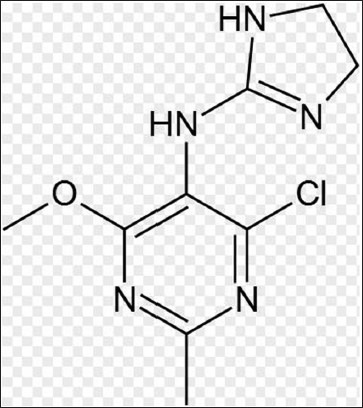
Chemical structure of moxonidine
Additional, moxonidine attenuates sympathetic tone[11] and improves the hemodynamic profile in patients with congestive heart failure.[12]
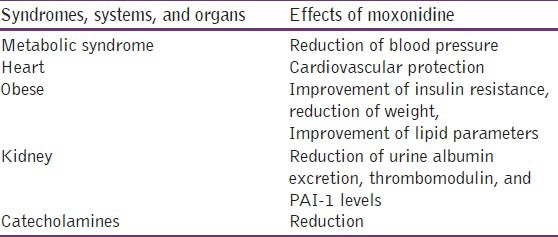
Also, moxonidine acts on other target-organs, like kidney and eye and on metabolism, with neutral or favorable effect on lipid parameters, improvement of insulin resistance in obese, and reduction of catecholamines. This may be due to the fact that moxonidine lowers leptin plasma levels and reduces weight in obese patients, through its action on SNS.[13]
Influence of moxonidine on target-organ protection and metabolism
During the last few years, a great number of studies involving moxonidine have been published. Most of them involve obesity, insulin resistance, and metabolic syndrome. Moxonidine reduces blood pressure in patients with metabolic syndrome while simultaneously reducing body weight in obese patients, as it has been showed in the postmarketing surveillance study CAMUS.[14] Also, Chazova et al.,[15] showed through a multicenter, prospective, randomized, open-label study that moxonidine improves insulin sensitivity in response to glucose challenge in patients with evidence of metabolic syndrome. This is the result of the reduction in plasma insulin levels. Moreover, several research groups independently found an improvement of insulin sensitivity in animals models too (mainly Zucker rats).[16]
Sanjuliani et al.,[17] showed that after 24 weeks of moxonidine treatment, plasma arterial adrenaline and noradrenaline were significantly reduced. This fact confirms the decrease of plasma catecholamines and, moreover, proves the action of the drug in conditions of sympathetic overactivity.
A double-blind, placebo-controlled crossover study demonstrate that moxonidine reduces exercise and mental stress-induced SNS activation and seems to be considered as an alternative to b-adrenoceptor blockers-in combination therapy-, when patients bothered by the exercise limitations of b-adrenoceptor blockers.[18] This antihypertensive agent lowers intraocular pressure, suggesting a possible benefit in glaucoma.[1]
The study of Krespi et al.,[19] suggests that in hypertensive patients with microalbuminuria, moxonidine reduces urine albumin excretion, thrombomodulin, and Plasminogen activator inhibitor-1 (PAI-1) levels. These results demonstrate an effect on renal function and endothelial homeostatic mechanisms. Also, a 3-year trial showed that treatment with standard antihypertensive therapy and adjunctive moxonidine in patients with advanced renal failure was predicted to reduce the number of new end-stage renal disease cases compared to adjunctive nitrendipine. The model showed that adjunctive moxonidine seems to increase life-years lived.[20]
Furthermore, moxonidine is used in the treatment of obese patients with metabolic syndrome, because this antihypertensive agent reduces leptin levels in plasma and reduces weight in obese patients, through the action of the SNS.[13]
Effects of imidazoline receptor activation by moxonidine in heart function
A lot epidemiological studies have shown that increased activity of SNS leads to an increase in cardiovascular morbidity and mortality. Considering that moxonidine decrease the SNS activity, it is safe to administrate that the drug has a place in cardiovascular protection and reversal of metabolic disorders due to SNS overactivity.[21]
Moxonidine is a selective imidazoline receptor (I1) agonist with central antihypertensive effects.[1] Imidazoline I1 receptors have been localized in the brainstem RVLM, and in peripherical nervous system, including heart-mainly in cardiac atria.[22] The atria are the primary site of atrial natriuretic peptide (ANP) production. The ANP is involved in blood pressure reduction and volume regulation.[23] The chronic hypotensive effect of ANP is mediated by attenuation of cardiovascular sympathetic tone.[24] Moxonidine can stimulate ANP release from heart.[25] The increase in ANP may be explained in part by moxonidine SNS inhibition in heart.[22]
A study, in spontaneously hypertensive rats, demonstrates that cardiac I1 receptors are upregulated and normalized by chronic antihypertensive treatment with moxonidine.[26]
Also, an other study contends the acute hemodynamic effects of moxonidine. These are the reduction in right atrial pressure, pulmonary artery pressure, and cardiac index.[27]
Additional, moxonidine seems to attenuate tachyarrhythmias[28] and increase left ventricular ejection fraction, in patients with chronic heart failure.[29] Also, moxonidine pretreatment provides a beneficial effect, during reperfusion-induced arrhythmias that appear after a brief period of myocardial ischemia.[30]
Regarding moxonidine and heart, there are studies that support the chronic therapy with this agent, in patients with chronic heart failure.[28] Chronic heart failure is associated with activation of SNS and the degree of this stimulation appears to be a marker for both the severity of the syndrome and the risk of death.[31,32,33]
On the contrary, the MOXCON study (MOXonidine CONgestive Heart Failure) demonstrates that the use of moxonidine in patients with advanced heart failure was associated with an early increase in morbidity and mortality in a large cohort of New York Heart Association classes II-IV patient.[34]
The use of moxonidine nowadays
Nowadays, according to the guidelines of ESH-ECS (European Society of Hypertension/European Society of Cardiology), moxonidine, as all centrally acting agents, is not a first-choice agent in antihypertensive treatment. It is mainly used in combination with the other categories of antihypertensive agents.[35]
Also, overweight patients with metabolic syndrome are more likely to be on combination therapy. Despite good blood pressure response to moxonidine and more frequent use of combination therapy, less than 5% of diabetic patients achieve blood pressure target (<130/80 mm Hg).[14]
Furthermore, moxonidine should not be used as treatment in patients when glomerular filtration rate < 30 ml/min.[36]
Conclusion
Moxonidine is the newest, second-generation, centrally acting antihypertensive agent. It is used in therapy of mild to moderate hypertension. Moxonidine has selective agonist activity at imidazoline I1 receptors and less adverse effects than the other centrally acting drugs. This fact authorizes the frequent use of moxonidine in clinical practice, as monotherapy or in combination with other antihypertensive agents. Also, the beneficial effects of moxonidine in target-organs, such as heart, are very important [Table 1]. Although, a lot of studies have conjecture the role that moxonidine displays in pathophysiological mechanisms, more studies are required, in order to clarify this role.
Table 1.
Effects of moxonidine on sympathetic nervous system, metabolism, and on target organs
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Ziegler D, Haxhiu MA, Kaan EC, Papp JG, Ernsberger P. Pharmacology of moxonidine, an I1-imidazoline receptor agonist. J Cardiovasc Pharmacol. 1996;27(Suppl 3):S26–37. doi: 10.1097/00005344-199627003-00005. [DOI] [PubMed] [Google Scholar]
- 2.Fenton C, Keating GM, Lyseng-Williamson KA. Moxonidine: A review of its use in essential hypertension. Drugs. 2006;66:477–96. doi: 10.2165/00003495-200666040-00006. [DOI] [PubMed] [Google Scholar]
- 3.Prichard BN, Graham BR, Owens CW. Moxonidine: A new antiadrenergic antihypertensive agent. J Hypertens Suppl. 1999;17:S41–54. [PubMed] [Google Scholar]
- 4.Prichard BN, Graham BR. The use of moxonidine in the treatment of hypertension. J Hypertens Suppl. 1997;15:S47–55. doi: 10.1097/00004872-199715011-00007. [DOI] [PubMed] [Google Scholar]
- 5.Prichard BN, Owens CV, Graham BR. Pharmacology and clinical use of moxonidine, anew centrally acting sympatholytic antihypertensive agent. J Hum Hypertens. 1997;11(Suppl 1):S29–45. [PubMed] [Google Scholar]
- 6.Sica DA. Centrally acting antihypertensive agents: An update. J Clin Hypertens. 2007;9:399–405. doi: 10.1111/j.1524-6175.2007.07161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cao Ch, Kang CW, Kim SZ, Kim SH. Augmentation of moxonidine-induced increase in ANP release by atrial hypertrophy. Am J Physiol Heart Circ Physiol. 2004;287:H150–6. doi: 10.1152/ajpheart.00977.2003. [DOI] [PubMed] [Google Scholar]
- 8.Mitrovic V, Hamel M, Miric M, Thormann J, Hamm C. Effect of the imidazoline receptor agonist moxonidine on hemodynamics, coronary circulation, metabolic ischemia markers and the neurohumoral system in patients with essential hypertention. Effects of moxonidine on coronary circulation. Z Kardiol. 2001;90:953–63. doi: 10.1007/s003920170066. [DOI] [PubMed] [Google Scholar]
- 9.Poisson D, Christen MO, Sannajust F. Protective effects of I (1)-antihypertensive agent moxonidine against neurogenic cardiac arrhythmias in halothane-anesthetized rabbits. J Pharmacol Exp Ther. 2000;293:929–38. [PubMed] [Google Scholar]
- 10.Van Kerckhoven R, van Veen TA, Boomsma F, Saxana PR, Schoemaker RG. Chronic administration of moxonidine suppresses sympathetic activation in a rat heart failure model. Eur J Pharmacol. 2000;397:113–20. doi: 10.1016/s0014-2999(00)00232-6. [DOI] [PubMed] [Google Scholar]
- 11.Swedberg K, Bergh CH, Dickstein K, McNay J, Steinberg M. The effects of moxonidine, a novel imidazoline, on plasma norepinephrine in patients with congestive heart failure. J Am Coll Cardiol. 2000;35:398–404. doi: 10.1016/s0735-1097(99)00565-3. [DOI] [PubMed] [Google Scholar]
- 12.Dickstein K, Manhenke C, Aarsland T, Køpp U, McNay J, Wiltse C. Acute Hemodynamic and neurohumoral effects of moxonidine in congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 1999;83:1638–44. doi: 10.1016/s0002-9149(99)00170-8. [DOI] [PubMed] [Google Scholar]
- 13.Karlafti E, Savopoulos CH, Baltatzi M, Hatzitolios Al. The position of central acting sympatholytic agents on Arterial hypertension therapy. Arterial Hypertens (Greek) 2010;19:32–43. [Google Scholar]
- 14.Sharma AM, Wagner T, Marsalek P. Moxonidine in the treatment of overweight and obese patients with metabolic syndrome: A postmarketing surveillance study. J Hum Hypertens. 2004;18:669–75. doi: 10.1038/sj.jhh.1001676. [DOI] [PubMed] [Google Scholar]
- 15.Chazova I, Almazov VA, Shlyakhto E. Moxonidine improves glycaemic control in mildly hypertensive, overweight patients: A comparison with metformin. Diabetes Obes Metab. 2006;8:456–65. doi: 10.1111/j.1463-1326.2006.00606.x. [DOI] [PubMed] [Google Scholar]
- 16.Keulen L, Henricksen EJ, Jacob S, Lang R. Antihypertensive treatment and cardiovascular risk management in patients with the Metabolic Syndrome-Focus on SNS and insulin resistance. J Clin Basic Cardiol. 2001;3:193–5. [Google Scholar]
- 17.Sanjuliani AF, Francischetti EA, Genelhu de Abreu V, Ueleres Braga J, et al. Effects of moxonidine on the Sympathetic Nervous System, Blood Pressure, Plasma Renin Activity, Plasma Aldosterone, Leptin, and Metabolic Profile in Obese Hypertensive Patients. J Clin Basic Cardiol. 2004;7:19. [Google Scholar]
- 18.Wenzel RR, Mitchell A, Siffert W, Bührmann S, Philipp T, Schäfers RF. The I 1-imidazoline agonist moxonidine decreases sympathetic tone under physical and mental stress. Br J Clin Pharmacol. 2004;57:545–51. doi: 10.1111/j.1365-2125.2003.02058.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krespi PG, Makris TK, Hatzizaxarias AN, Triposkiadis P, Tsoukala C, Kyriaki D, et al. Moxonidine effect on microalbuminuria, thrombomodulin, and plasminogen activator inhibitor-1 levels in patients with essential hypertension. Cardiovasc Drugs Ther. 1998;12:463–7. doi: 10.1023/a:1007702132210. [DOI] [PubMed] [Google Scholar]
- 20.Littlewood KJ, Greiner W, Baum D, Zoellner Y. Adjunctive treatment with moxonidine versus nitrendipine for hypertensive patients with advanced renal failure: A cost-effectiveness analysis. BMC Nephrol. 2007;8:9. doi: 10.1186/1471-2369-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borchard U. The role of sympathetic nervous system in cardiovascular disease. J Clin Basic Cardiol. 2001;4:175–7. [Google Scholar]
- 22.Mukaddam-Daher S, Gutkowska J. Imidazoline receptors in the heart: A novel target and a novel mechanism of action that involves atrial natriuretic peptides. Braz J Med Res. 2004;37:1239–45. doi: 10.1590/s0100-879x2004000800015. [DOI] [PubMed] [Google Scholar]
- 23.Steinheiper ME, Cohrane KL, Field LJ. Hypotension in transgenic mice expressing atrial natriuretic factor fusion genes. Hypertension. 1990;16:301–7. doi: 10.1161/01.hyp.16.3.301. [DOI] [PubMed] [Google Scholar]
- 24.Melo LG, Veress AT, Ackermann U, Steinhelper ME, Pang SC, Tse Y, et al. Chronic regulation of arterial blood pressure in ANP transgenic and knockout mice: Role of cardiovascular sympathetic tone. Cardiovasc Res. 1999;43:437–44. doi: 10.1016/s0008-6363(99)00104-2. [DOI] [PubMed] [Google Scholar]
- 25.Mukaddam-Daher S, Menaouar A, Gutkowska J. Receptors involved in moxonidine-stimulated atrial natriuretic peptide release from isolated normotensive rat hearts. Eur J Pharmacol. 2006;541:73–9. doi: 10.1016/j.ejphar.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 26.El-Ayoubi R, Menaouar A, Gutkowska J, Mukaddam-Daher S. Imidazoline receptors but not a2-adrenoceptors are regulated in spontaneously hypertensive rat heart by chronic moxonidine treatment. J Pharmacol Exp Ther. 2004;310:446–51. doi: 10.1124/jpet.104.067595. [DOI] [PubMed] [Google Scholar]
- 27.Mobini R, Fu M, Jansson PA, Bergh CH, Scharin Täng M, Waagstein F, et al. Influence of central inhibition of sympathetic nervous activity on myocardial metabolism in chronic heart failure: Acute effects of the imidazoline I1 receptor agonist moxonidine. Clin Sci. 2006;110:329–36. doi: 10.1042/CS20050037. [DOI] [PubMed] [Google Scholar]
- 28.Dickstein K, Manhenke C, Aarsland T, McNay J, Wiltse C, Wright T. The effect of chronic, sustained-release moxonidine therapy on clinical and neurohumoral status in patients with heart failure. Int J Cardiol. 2000;75:167–76. doi: 10.1016/s0167-5273(00)00319-3. [DOI] [PubMed] [Google Scholar]
- 29.Swedberg K, Bristow MR, Cohn JN, Dargie H, Straub M, Wiltse C, et al. Effects of Substained-Release Moxonidine, an imidazoline Agonist, on plasma Norepinephrine in Patients with Chronic Heart failure. Circulation. 2002;105:1797–803. doi: 10.1161/01.cir.0000014212.04920.62. [DOI] [PubMed] [Google Scholar]
- 30.Lepran I, Papp JG. Effect of moxonidine on arrhythmias induced by coronary artery occlusion and reperfusion. J Cardiovasc Pharmacol. 1994;24:S9–15. doi: 10.1097/00005344-199424001-00003. [DOI] [PubMed] [Google Scholar]
- 31.Benedict CR, Francis GS, Shelton B, Johnstone DE, Kubo SH, Kirlin P, et al. Effect of long-term enalapril therapy on neurohormones in patients with left ventricular dysfunction. SOLVD Investigators. Am J Cardiol. 1995;75:1151–7. doi: 10.1016/s0002-9149(99)80748-6. [DOI] [PubMed] [Google Scholar]
- 32.Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, Francis GS, et al. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med. 1984;311:819–23. doi: 10.1056/NEJM198409273111303. [DOI] [PubMed] [Google Scholar]
- 33.Swedberg K, Eneroth P, Kiekshus J, Wilhelmsen L. Hormones regulating cardiovascular function in patients with severe congestive heart failure and their relation to mortality. Circulation. 1990;82:1730–6. doi: 10.1161/01.cir.82.5.1730. [DOI] [PubMed] [Google Scholar]
- 34.Cohn JN, Pfeffer MA, Rouleau J, Sharpe N, Swedberg K, Straub M, et al. MOXCON Investigators. Adverse mortality effect of central sympathetic inhibition with sustained-release moxonidine in patients with heart failure (MOXCON) Eur J Heart Fail. 2003;5:659–67. doi: 10.1016/s1388-9842(03)00163-6. [DOI] [PubMed] [Google Scholar]
- 35.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. ESH-ESC Task Force on the Management of Arterial Hypertension. 2007 ESH-ESC practice guidelines for the management of arterial hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J Hypertens. 2007;25:1751–62. doi: 10.1097/HJH.0b013e3282f0580f. [DOI] [PubMed] [Google Scholar]
- 36.Kirch W, Hutt HJ, Planitz V. The influence of renal function on clinical pharmacokinetics of moxonidine. Clin Pharmacokinet. 1988;15:245–53. doi: 10.2165/00003088-198815040-00004. [DOI] [PubMed] [Google Scholar]


