Abstract
Objective:
To evaluate the factors influencing final vision outcome after surgical repair of open globe injuries and to correlate the Ocular trauma score.
Materials and Methods:
Retrospective case analysis of patients with open globe injuries at a tertiary referral eye care centre in Singapore was performed. Pre-operative factors affecting final vision outcome in patients with open globe injury and correlation of ocular trauma score in our study with international ocular trauma scoring system was performed.
Results:
Case records of 172 eyes with open globe injury were analyzed. Mean age was 36. 67 years. Mean follow up was 12.26 m. Males were pre-dominantly affected. Initial visual acuity was ≥20/40, 20/50 < 20/200, 20/200- CF, HM– PL and NLP in 24 (14%), 39 (22.7%), 16 (9.3%), 66 (38.4%) and 27 (15.7%) eyes respectively. Final visual acuity was ≤20/40, 20/50 < 20/200, 20/200- 1/200, HM– PL and NLP in 76 (44.2%), 28 (16.3%), 11 (6.4%), 30 (17.4%) and 27 (15.7%) eyes respectively. Ocular trauma score in our study correlates with international ocular trauma scoring system.
Conclusion:
The present study showed pre-operative variables such as mode of injury, pre-operative visual acuity, traumatic cataract, hyphaema, relative afferent papillary defect, vitreous lossand vitreous hemorrhage to be adversely affecting the final vision outcome. Our study showed a good synchrony with international ocular trauma score (OTS) and based on this study we were able to validate application of OTS in Singapore population. Recognizing these factors can help the surgeon in evidence based counseling.
Keywords: Ocular trauma, open globe injury, preoperative (initial) visual acuity, prognostic factors, relative afferent pupillary defect
Ocular trauma is one of the leading causes of ocular morbidity in children and young adults.[1] Successful surgical repair of open globe injury and subsequent visual rehabilitation is a topic of great significance and challenge to the practicing ophthalmologists.[2] One of the important components in management of open globe injury is counseling of the trauma victim and his family.[2] Even though, with advent of new modalities and improved technology the management of penetrating ocular injuries has changed,[2] we need to counsel and prognosticate any patient with ocular trauma before and even after the repair of open globe injury. To predict the vision outcome in ocular trauma patients, there have been numerous literature till date.[3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22] International classification of ocular trauma is based on some of the variables affecting the final visual outcome.[18] Ocular trauma score (OTS) system suggested by Kuhn et al., is the current system to predict the vision outcome in patients with open globe injury.[19] Kuhn et al., analyzed more than 2500 injuries from the United States and Hungarian eye injury registries to identify the predictors of final vision outcome after open globe injury.[19] The OTS is calculated by assigning certain numerical raw points to six variables: initial visual acuity, globe rupture, endophthalmitis, perforating injury, retinal detachment, and relative afferent papillary defect (RAPD). The scores are stratified into five categories that give the probabilities of attaining a range of visual acuities post-injury.[19] There are very limited studies on validation of scoring system used by OTS.[14,20,21]
Based on literature review, the factors likely to predict outcome after open globe injury are mechanism or type of injury, preoperative visual acuity (VA), time lag between injury and surgery, relative afferent pupillary defect (RAPD), size and location of the wound. Besides the above listed variables, other parameters that can predict vision outcome are retinal detachment, uveal or retinal tissue prolapse, vitreous hemorrhage, lens damage, hyphema and number of operative procedures.[3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]
However, there is limited literature for epidemiology and outcome of open globe injuries from Singapore.[23,24] The present study was aimed at evaluating the factors affecting the final vision outcome and to validate the ocular trauma score in patients with open globe injuries at a tertiary referral eye care center in Singapore.
Materials and Methods
We retrospectively reviewed the case records of the patients who underwent surgical repair of open globe injury at a tertiary referral eye care center in Singapore from January 2000 to December 2009. The center receives high volume of emergency patients out of which a proportion of patients presents with history of ocular trauma and open globe injury. Cases were identified from computerized admissions database. Approval from local ethics committee was obtained to conduct this retrospective review.
Case records of 172 eyes of 172 patients with open globe injuries operated over 10 years from January 2000 till December 2009 were retrospectively analyzed. Most of the open globe injuries were secondary to work-related ocular injuries. Cases with surgical repair done before presentation to our center, with poor visual acuity of the injured eye prior to injury and with follow up of less than four months post surgery were excluded from the study. The factors studied were age and sex of the patient, initial VA after injury, presence or absence of RAPD, details of the object causing the injury, duration between injury and the surgery, total extent of the wound and zone of the injury, wound involving limbus or not, wound involving visual axis, extent of wound beyond recti insertion which was noted intraoperatively, presence or absence of hyphema, uveal tissue prolapse, lens status, vitreous loss, vitreous hemorrhage, presence or absence of retinal detachment and evidence of infection on or around the wound.
Details of all the surgical steps were recorded. Total duration of follow up, visual acuity at four months follow up and anatomical status of the eye at final follow up were recorded. Final anatomical status of the eye indicating corneal scar, phthisis bulbi, pseudophakia or traumatic cataract, retinal detachment, glaucoma was recorded in the study eyes.
For statistical analysis, the initial visual acuity (VA) after injury and the VA at final follow up were grouped in five categories: Group 1 - VA ≤ 20/40, Group 2 - VA: 20/50 < 20/200, Group 3 - VA: 20/200 - CF, Group 4 - VA: HM– PL and Group 5-VA: NLP. The relationship between different preoperative variables and the final VA was analyzed using correlation analysis (Spearman's rho) for univariate analysis. Furthermore, binary logistic regression was performed for the purpose of multivariate analysis, in which final VA were grouped into only two categories: ≤20/200 and >20/200. Whenever necessary, the association between factors and final VA was considered statistically significant if P ≤ 0.05.
Results
Of the 172 patients, 166 (96.5%) were males and 6 (3.5%) were females. The average age was 36.67 years, with a median age of 34 years (range: 15-91 years). Right eye was involved in 89 (51.7%) patients and left eye in 83 (48.3%) patients. None of the patient in the series had bilateral eye involvement secondary to injury. One hundred and seventeen (68%) patients had injury following blunt trauma and remaining 55 (32.0%) had laceration.
There were 24 (14.0%) patients having a preoperative VA better than 20/40, 39 (22.7%) patients had VA between 20/50 < 20/200, 16 (9.3%) patients had VA between 20/200 – CF, 66 (38.4%) patients had VA of HM-PL and the remaining 27 (15.7%) had a preoperative VA of NLP. After surgery, at four months follow up 76 (44.2%) patients had VA better than 20/40, 28 (16.35) had VA between 20/50 < 20/200, 11 (6.4%) had VA between 20/200 to CF, 30 (17.4%) had final VA of CF-HM and rest 27 (15.7%) had NLP. The bar graph comparing preoperative with final VA is as presented in Fig. 1. One hundred and eight (63%) patients had only one surgery, while 46 (27%) had two and the remaining 18 (10%) patients had three or more surgeries [Fig. 2]. Average follow-up was 7 m, with a median of 6 m (range: 4-24 m).
Figure 1.
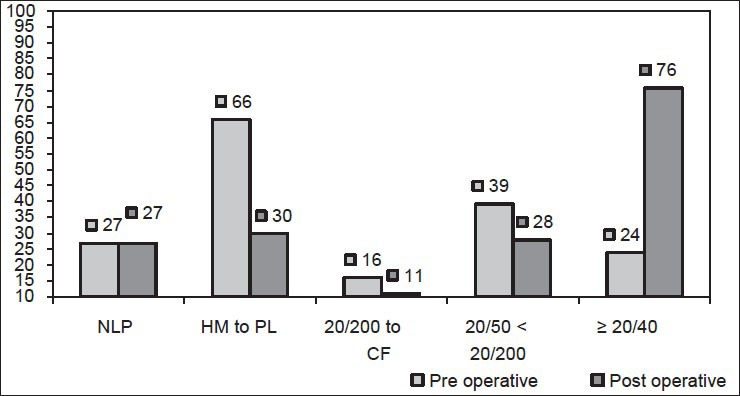
Pre-operative v/s post-operative VA
Figure 2.
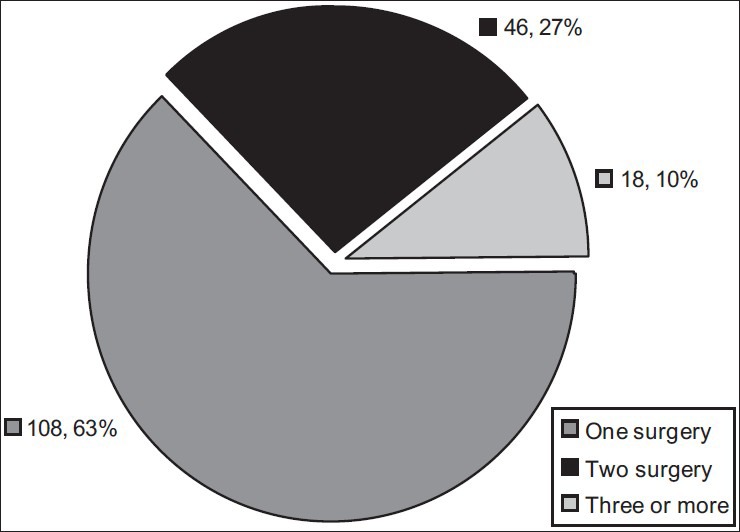
Number of operations
Of 172 eyes, 88 (51.2%) had injury limited to cornea i.e. in Zone I of international ocular trauma classification for open globe injury,[19] 58 (33.7%) eyes had injury involving zone II i.e., within 5 mm of sclera from limbus and remaining 26 (15.1%) eyes had injury extending into zone III i.e., beyond 5mm of corneoscleral junction.
Lid laceration was associated in 22 (12.8%) eyes and orbital involvement was associated in 7 (4.1%) patients. RAPD was noted in 72 eyes (41.9%). Hyphema was seen in 73 (42.4%) eyes. Lens was found to be cataractous with or without rupture of anterior capsule in 103 eyes (59.9%). Vitreous loss was noted in 44 (25.6%) eyes. Wound was seen extending to insertion of rectus muscle (intra-operative finding) in 22 eyes (30.55%). Retinal detachment was present in 36 eyes (20.9%). Intra-ocular foreign body was seen in 27 (15.7%) eyes.
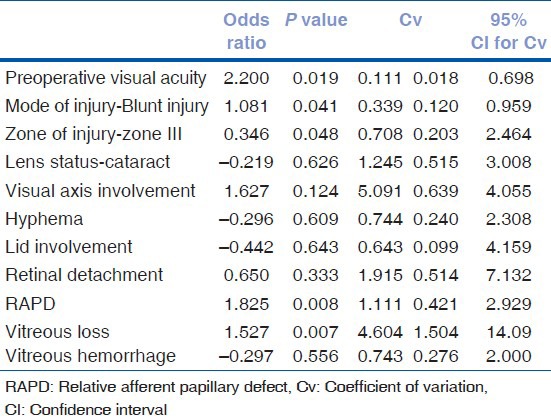
Based on the univariate logistic regression analysis [Table 1] and cross tab correlation analysis [Table 2], almost all the preoperative variables were found to be statistically significant for predicting final vision outcome: Preoperative visual acuity, mode of injury with blunt trauma, visual axis involvement, lid and orbital involvement, traumatic cataract, RAPD, hyphaema, vitreous loss, vitreous hemorrhage and retinal detachment. Furthermore, all the factors found significant in univariate analysis were included in the multivariate analysis using binary logistic regression to further evaluate their associations with final VA. As shown in Table 3, pre-operative visual acuity (P = 0.019, OR = 2.20), blunt ocular trauma, RAPD and presence of vitreous loss were found to be statistically significant for poor vision outcome on multivariate logistic regression analysis.
Table 1.
Univariate logistic regression: Preoperative variables adversely affecting final VA with statistical calculations
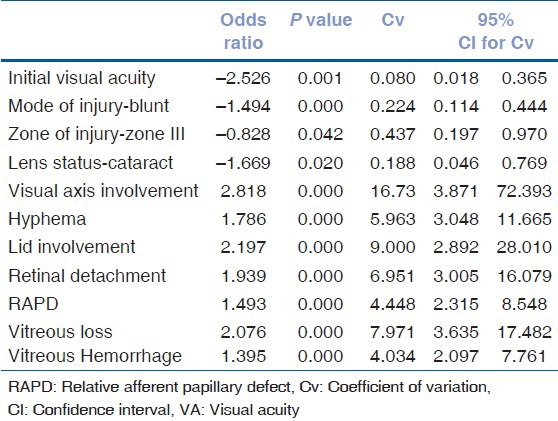
Table 2.
Cross tab correlation analysis: Preoperative variables adversely affecting final VA
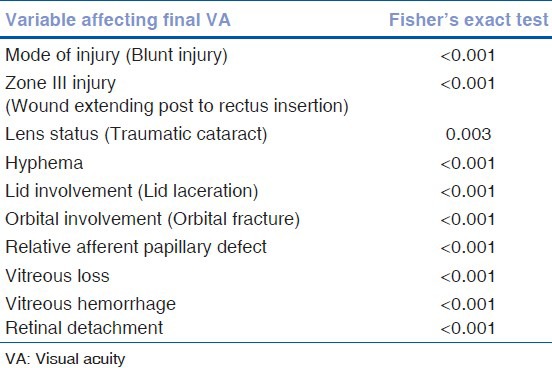
Table 3.
Multivariate logistic regression: Preoperative variables adversely affecting final VA
Good initial VA was associated with good final vision outcome. Similarly, poor pre-operative VA is associated with worse outcome and is shown to be statistically significant on multivariate logistic regression analysis (P < 0.001 by Fisher's test of independence). Significant (>50%) proportion of patients with presence of RAPD on initial pre-operative examination had poor final vision outcome (P < 0.001 by Fisher's test of independence). Similarly presence of vitreous loss was significantly associated with poor final vision outcome group and 60% of patients with pre-operative vitreous loss are having final VA of Hand Movements (HM) or worse (P < 0.001 by Fisher's test of independence). IOFB had no impact on final vision outcome irrespective of zone of injury: this can be partly accounted by small number of cases of IOFB with open globe injury in the current series.
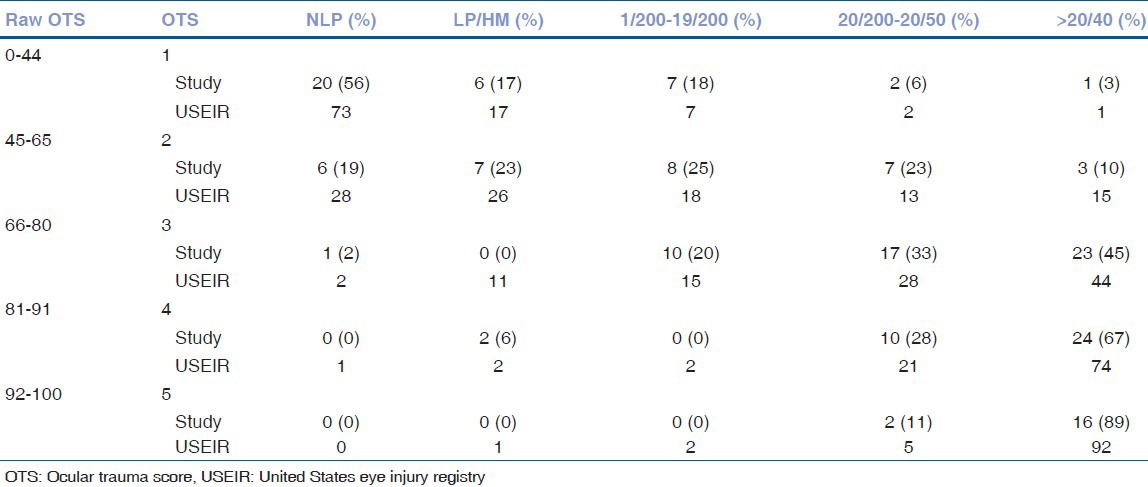
Ocular trauma score was also computed for all the patients in our series and the final outcome was correlated with prediction based on international ocular trauma scoring system.[19] Comparative head to head scores for both our study and international ocular trauma scoring system is as shown in Table 4. Even though the current study has a smaller sample size as against United States Eye Injury Ocular Trauma Scoring (USEIR-OTS) system, we can see close resemblance between the scores in our study and that in USEIR study for all 5 grades of Ocular trauma score (OTS).[19]
Table 4.
Ocular trauma score: Head to head analysis of USEIR OTS v/s OTS of our study
Discussion
Open globe injuries are a common and often preventable cause of permanent visual impairment and visual loss. Conventional practice worldwide by ophthalmologists across the world is primary surgical closure of the open globe injury regardless of initial VA in order to restore the structural integrity of the globe at the earliest possible. Counseling of the trauma victim and family members is one of the important components in management of ocular trauma. In order to possibly predict the outcome of surgical repair of open globe injury, numerous studies have been done in the past to co-relate the final visual outcome with the several preoperative factors related to ocular injury. United States Eye Injury Registry have also formulated scoring system based on significant pre-operative variables affecting the final vision outcome.[19] Numerous factors that have been found to correlate significantly with visual outcome include age,[11,22] type or mechanism of injury,[3,6,8,19,20,21,22] initial VA,[3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,19,20,21,22] presence of RAPD,[11,15,19,20,21,22] extent of wound and size of open-globe injury,[3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,20,21,22] location of open globe wound,[3,8,9,19,20,21,22] lens damage,[3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,19,20,21,22] hyphema,[4,20,22] vitreous hemorrhage,[3,4,8,9,20,21,22] retinal detachment,[3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,20,21,22] and presence and type of intraocular foreign body.[17]
We analyzed the data regarding the pre-operative factors affecting final vision outcome following surgical repair of open globe injury. We attempted to create homogenous group of patients with open globe injuries by excluding cases with surgical repair done elsewhere and endophthalmitis at presentation as both of them can affect the visual outcome.[2] Endophthalmitis by itself is very strong predictor of visual outcome;[2] hence, it was excluded as the current series was undertaken to find out factors besides endophthalmitis which can affect the final vision outcome.
In most population based studies, there is a strong preponderance for open globe injuries to affect males,[15,23,24] likewise in our series there was a very strong male preponderance. This may reflect the more aggressive characteristics of male behavior and to a lesser extent the involvement of men in higher risk working activities. Also, in the current series the majority of patients were in younger age group with 126 out of 172 patients (73.2%) less than 40 years of age which is also similar to other studies till date.[11,22,23,24] Out of 172 injuries, 96 (55.81%) injuries were work related trauma and hence significantly high percentage of the open globe injuries were industrial accidents or work-related eye injuries. Being work-related eye injuries, it suggests the central authorities to take preventive measures and to enforce eye protection at work place to prevent serious eye injuries.
Pre-operative VA was shown to be most important prognostic factor by almost all the studies.[3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21] Agrawal et al.,[22] have however documented initial visual acuity as not the statistically significant preoperative variable in predicting final vision outcome. However, in their study they have excluded patients with endophthalmitis and intraocular foreign body. In the current study, poor preoperative visual acuity is significantly associated with poor post-operative visual acuity on both univariate and multivariate logistic regression analysis. In classification and regression tree model by Schmidt et al., they have shown initial vision as a key predictor in the open globe outcome prognostic tree and was found to correlate significantly with final outcome.[14] Pieramici et al.,[9] described a significantly reduced rate of enucleation if the presenting visual acuity was 20/200 or better, whereas, 34% of those with a presenting visual acuity of worse than 20/200 underwent eventual enucleation.
In the current study, based on mode of injury, blunt injury was shown to be 1.494 times more likely to have poor final VA compared to penetrating trauma on univariate logistic regression analysis. On multivariate logistic regression analysis blunt trauma has 1.081 times higher risk of poorer outcome as against penetrating injury. This is in concordance with other studies where the authors have shown injury by sharp objects are correlated with a more favorable visual outcome when compared to blunt impact mechanisms.[8,15] Rahman et al., showed a statistically significant improved visual outcome in patients suffering sharp injuries compared to blunt injuries (P = 0.004).[15] Blunt injury can affect the internal structures of the eye by coup-countercoup mechanism resulting in more significant damage and similarly significant injury to optic nerve. With blunt injury, wound can get extended posterior to recti insertion resulting in poorer final vision outcome. In the current study, wound extending posterior to rectus insertion had poorer outcome as against wound limited anterior to rectus insertion (P = 0.048 on multivariate logistic regression analysis).
Of all the clinical signs at presentation after injury, presence of an RAPD and vitreous loss were statistically significant in predicting outcome. If RAPD was present, the final vision outcome was significantly worse as seen in other studies.[3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22] In series by Rahman et al., 48% of patients with RAPD proceeded to eventual enucleation.[15] Similarly, in series by Pieramici et al., 55% of eyes were enucleated if an RAPD was documented at presentation, compared to 7% in the absence of an RAPD. The presence of RAPD resulted in tenfold chance of attaining a final VA of counting fingers (CF) or worse in a series by Rofail et al.[13] RAPD has hence been identified as an important predictor of visual outcome both in the present study and existing literature. In the current study, more than 50% of patients had final VA of less than hand movements (HM) if RAPD was present at time of initial assessment. With odds ratio of 1.825 it showed to be statistically significant predictor of final vision outcome on multivariate logistic regression analysis in our study. It was a concern that there was a tendency not to examine the pupil responses during the initial assessment of open globe injury patients as resident may get overwhelmed by presence of significant corneoscleral laceration with obscured details of anterior and posterior segment of the traumatized eyes. In such cases, always presence of consensual reflex in the fellow eye or presence or absence of reverse RAPD should be documented at time of initial assessment.
In the current study, vitreous loss was found to be associated with poorer outcome. In a series published by Leonardo et al.,[10] in 2003, authors reported presence of vitreous loss as a poor prognostic indicator on multivariate logistic regression analysis. In more than 65% of patients with vitreous loss, the final vision outcome was poorer than hand movements in the current study. Presence of vitreous loss does indicate associated vitreoretinal disturbances and possibly retinal trauma. During the primary corneoscleral wound repair, surgeon needs to pay attention to vitreous in the wound and try and clear it off the wound with help of sponge vitrectomy otherwise vitreous incarceration in the wound can result in vitreoretinal traction with possible poorer outcome.
In 2002, Kuhn et al., developed a prognostic model, the ocular trauma score (OTS), to predict the visual outcome of patients after ocular trauma.[19] Authors analysed over 2500 eye injuries from the United States and Hungarian Eye Injury registries and evaluated more than 100 variables to identify theses predictors. Essentially it's like APGAR score used in Obstetrics and is calculated by assigning certain numerical raw points to six variables: initial visual acuity, globe rupture, endophthalmitis, perforating injury, retinal detachment and an RAPD. The scores are subsequently stratified into five categories from one to five with one being the lowest score and five being the highest score. The patient with OTS score of one will have a higher risk of poorer final visual outcome as against the patient with OTS score of five who will have higher probability of better final vision outcome.[19] We attempted to compare and stratify our study subjects into the same scoring system and study score in our series was very much comparable to international OTS system as seen in Table 4. In most of the table, there was complete agreement between OTS in our study with USEIR OTS except for study subset with score of 1 where vision recovery of 20/200 or better was predicted in 23% of patients in USEIR data as against 6% in our study. Similarly, in patients with OTS of three, vision outcome was LP/HM in 11% of patients in USEIR whereas it was 0% in our study. But, with scores of two, four and five there was significant concordance between our study and USEIR OTS, signifying the clinical importance and practical application of OTS. In another series from Asia, Han and Yu[21] had documented final VA assessment using OTS categories to be comparable to USEIR OTS. It suggests that OTS possibly has predictive value in open globe injuries in Asians.
In this retrospective review, we have shown several factors that may aid the clinician in deciding on the prognostic value after primary repair of open globe injury. In conclusion, in the current study initial visual acuity after trauma, mode of the injury, presence of RAPD, posterior extent of the wound, presence of vitreous loss adversely affect the final visual outcome. Ocular trauma score (OTS) is a very comprehensive score to predict the final vision outcome in patients with open globe injury and hence should be more widely used by ophthalmologists across the world for counseling of trauma victim and family. OTS calculated at initial evaluation may have predictive value in patients with open globe injury.
Footnotes
Source of Support: Nil.
Conflict of Interest: No.
References
- 1.Parver LM. Eye trauma: The neglected disorder. Arch Ophthalmol. 1986;104:1452. doi: 10.1001/archopht.1986.01050220046022. [DOI] [PubMed] [Google Scholar]
- 2.Shah A, Blackhall K, Ker K, Patel D. Educational interventions for the prevention of eye injuries. Cochrane Database Syst Rev. 2009;4 doi: 10.1002/14651858.CD006527.pub3. CD006527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Juan EJ, Sternberg PJ, Michels RG. Penetrating ocular injuries: Types of injuries and visual results. Ophthalmology. 1983;90:1318–22. doi: 10.1016/s0161-6420(83)34387-6. [DOI] [PubMed] [Google Scholar]
- 4.Barr CC. Prognostic factors in corneoscleral laceration. Arch Ophthalmol. 1983;101:919–24. doi: 10.1001/archopht.1983.01040010919013. [DOI] [PubMed] [Google Scholar]
- 5.Issac DL, Ghanem VC, Nascimento MA. Prognostic factors in open globe injuries. Ophthalmologica. 2003;217:431–5. doi: 10.1159/000073075. [DOI] [PubMed] [Google Scholar]
- 6.Esmaeli B, Elner SG, Schork A, Elner VM. Visual outcome and ocular survival after penetrating trauma: A clinicopathologic study. Ophthalmology. 1995;102:393–400. doi: 10.1016/s0161-6420(95)31009-3. [DOI] [PubMed] [Google Scholar]
- 7.Gilber CM, Soong HK, Hirst LW. A two-year prospective study of penetrating ocular trauma at the Wilmer Ophthalmological Institute. Ann Ophthalmol. 1987;19:104–6. [PubMed] [Google Scholar]
- 8.Pieramici DJ, Mathew W, Mac C, Humayun MU. Open globe injury: Update on types of injuries and visual results. Ophthalmology. 1996;103:1798–803. doi: 10.1016/s0161-6420(96)30424-7. [DOI] [PubMed] [Google Scholar]
- 9.Pieramici DJ, Au Eong K, Sternberg PJ, Marsh MJ. Prognostic significance of a system for classifying mechanical injuries of the eye (globe) in open globe injuries. J Trauma. 2003;54:790–4. doi: 10.1097/01.TA.0000047053.53821.C8. [DOI] [PubMed] [Google Scholar]
- 10.Leonardo D, Ghanem VC. Prognostic factors in open globe injuries. Ophthalmologica. 2003;217:431–5. doi: 10.1159/000073075. [DOI] [PubMed] [Google Scholar]
- 11.Sternberg P, Jr, de Juan E, Jr, Michels RG, Auer C. Multivariate analysis of prognostic factors in penetrating ocular injuries. Am J Ophthalm. 1984;98:467–72. doi: 10.1016/0002-9394(84)90133-8. [DOI] [PubMed] [Google Scholar]
- 12.Hutton WL, Fuller DG. Factors influencing final visual results in severely injured eyes. Am J Ophthalm. 1984;97:715–22. doi: 10.1016/0002-9394(84)90503-8. [DOI] [PubMed] [Google Scholar]
- 13.Rofail M, Lee GA, Rourke P. Prognostic factors for open globe injury. Clin Exp Ophthalmol. 2006;34:783–6. doi: 10.1111/j.1442-9071.2006.01309.x. [DOI] [PubMed] [Google Scholar]
- 14.Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 2008;115:202–9. doi: 10.1016/j.ophtha.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Rahman I, Maino A, Devadason D, Leatherbarrow B. Open globe injuries: factors predictive of poor outcome. Eye. 2006;20:1336–41. doi: 10.1038/sj.eye.6702099. [DOI] [PubMed] [Google Scholar]
- 16.Thakker MM, Ray S. Vision limiting complications in open globe injuries. Can J Ophthalmol. 2006;41:86–92. doi: 10.1016/S0008-4182(06)80074-8. [DOI] [PubMed] [Google Scholar]
- 17.Brinton GS, Aaberg TM, Reeser FH, Topping TM, Abrams GW. Surgical results in ocular trauma involving the posterior segment. Am J Ophthalmol. 1982;93:271–8. doi: 10.1016/0002-9394(82)90524-4. [DOI] [PubMed] [Google Scholar]
- 18.Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Ophthalmology. 1996;103:240–3. doi: 10.1016/s0161-6420(96)30710-0. [DOI] [PubMed] [Google Scholar]
- 19.Kuhn F, Maisiak R, Mann L, mester V, Morris R, Witherspoon CD. The ocular trauma score (OTS) Ophthalmol Clin North Am. 2002;15:163–5. doi: 10.1016/s0896-1549(02)00007-x. [DOI] [PubMed] [Google Scholar]
- 20.Yu Wai Man, Steel D. Visual outcome after open globe injury: A comparison of two prognostic models - the Ocular trauma score and the classification and regression tree. Eye. 2010;24:84–9. doi: 10.1038/eye.2009.16. [DOI] [PubMed] [Google Scholar]
- 21.Han SB, Yu HG. Visual outcome after open globe injury and its predictive factors in Korea. J Trauma. 2010;69:E66–72. doi: 10.1097/TA.0b013e3181cc8461. [DOI] [PubMed] [Google Scholar]
- 22.Agrawal R, Rao G, Naigaonkar R, Xiaoling Ou. Prognostic factors for vision outcome after surgical repair of open globe injuries. Indian J Ophthalmol. 2011;59:465–70. doi: 10.4103/0301-4738.86314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wong TY, Tielsch JM. A population-based study on the incidence of severe ocular trauma in Singapore. Am J Ophthalmol. 1999;128:345–51. doi: 10.1016/s0002-9394(99)00167-1. [DOI] [PubMed] [Google Scholar]
- 24.Loon SC, Tay WT, Saw SM, Wang JJ, Wong TY. Prevalence and risk factors of ocular trauma in an urban south-east Asian population: The Singapore Malay Eye Study. Clin Exp Ophthalmol. 2009;37:362–7. doi: 10.1111/j.1442-9071.2009.02035.x. [DOI] [PubMed] [Google Scholar]


