Abstract
Optical coherence tomography has already been proven to be useful for pre- and post-surgical anterior eye segment assessment, especially in lamellar keratoplasty procedures. There is no evidence for intraoperative usefulness of optical coherence tomography (OCT). We present a case report of the intraoperative donor disc attachment assessment with spectral-domain optical coherence tomography in case of Descemet stripping automated endothelial keratoplasty (DSAEK) surgery combined with corneal incisions. The effectiveness of the performed corneal stab incisions was visualized directly by OCT scan analysis. OCT assisted DSAEK allows the assessment of the accuracy of the Descemet stripping and donor disc attachment.
Keywords: Descemet membrane, keratoplasty, optical coherence tomography
Descemet stripping and endothelial keratoplasty is a frequent surgical procedure in the Corneal Ophthalmology department. The main complication of the surgery is the intraoperative disc dislocation estimated for 14% of cases.[1] The main reason for the disc dislocation is the presence of the interface fluid between the donor disc and host corneal stroma. There are several intraoperative techniques including: Injecting the air into the anterior chamber, performing corneal stab incisions, corneal surface sweeping or peripheral recipient bed scraping designed to remove fluid from the donor/recipient graft interface.[2,3,4] The effectiveness of those techniques could be evaluated after the surgical procedure. In this paper, we present a case report of the intraoperative use of anterior segment-optical coherence tomography during Descemet stripping automated endothelial keratoplasty (DSAEK).
Case Report
A 72-year-old female patient with corneal edema due to Fuchs corneal dystrophy, after 2 years, uneventful phacoemulsification surgery with intraocular lens implantation was scheduled for DSAEK. The visual acuity was 20/200. The following eye had visual acuity of 20/25 (correction + 1,0 Dsph) and underwent Descemet's stripping endothelial keratoplasty (DSEK) combined with phacoemulsification surgery 3 years earlier. Spectral-domain optical coherence tomography (SD OCT) examination revealed corneal edema with Descemet membrane folds on posterior corneal surface and fluid spaces under the corneal epithelium. Central corneal thickness was 843 μm.
The DSAEK procedure was performed under local, peribulbar anesthesia with additional intravenous sedation. The donor cornea was dissected with a Moria microkeratome (350 μm keratome plate). After fashioning the clear corneal incision, the Descemet membrane was stripped with reverse Sinskey hook. The surgery was discontinued and the optical coherence tomography (OCT) exam with commercially available SD OCT device (IVue; Optovue, Fremont; USA) was performed. The OCT device was held by the surgeon. Acquiring of the image was gained by pressing the foot pedal after focusing the anterior eye segment structures within the OCT scan [Fig. 1]. After making sure that all of Descemet membrane was removed, the donor disc was inserted into the anterior chamber with Busin glide spatula. The corneal incisions were sutured with 10-0 nylon. The air was injected into the anterior chamber with following eye surface sweeping in order to remove fluid from the graft interface. The graft seemed to be attached when analyzing in the surgical microscope. After performing SD OCT, multiple fluid micro-spaces were revealed in the area of the graft interface [Fig. 2]. Due to that, we performed corneal stab incisions in the four main clock hours. After incisions, SD OCT revealed a proper graft adhesion to the posterior corneal surface [Fig. 3]. At the end of the surgery, the anterior chamber was left filled with quarter of the volume of injected air. The whole procedure lasted for 35 min, which increased the time of the surgery by approximately 15 min.
Figure 1.
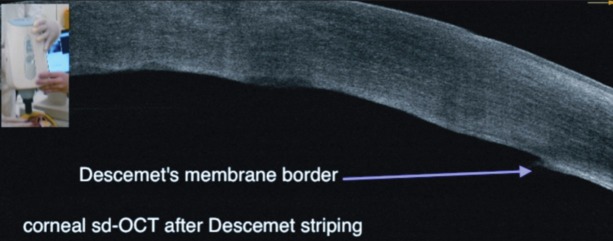
Spectral-domain optical coherence tomography scan after Descemet stripping. There is a border on posterior corneal surface with and without Descemet membrane
Figure 2.
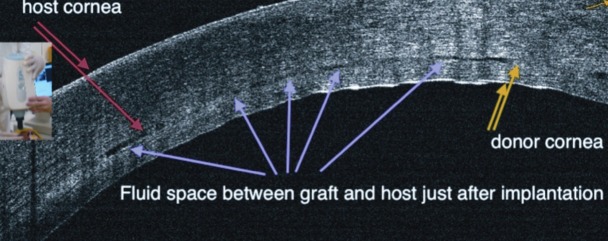
Spectral-domain optical coherence tomography scan performed after donor disc implantation. There is an inaccurate adhesion of a graft with accompanying fluid spaces noticeable
Figure 3.
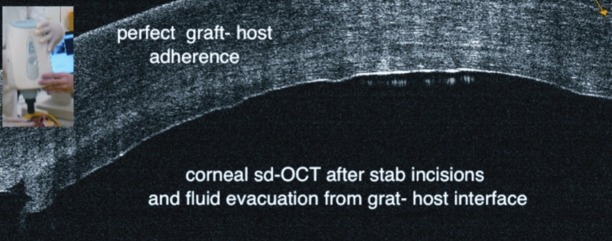
Spectral-domain optical coherence tomography scan performed after corneal stab incisions with a surface sweeping. A proper graft adhesion
Discussion
Assessment of the intraoperative donor disc attachment could be performed routinely with the use of a slit-lamp attached to the surgical microscope or alternatively by observing the donor lenticule border using very high microscope magnification. However, none of those methods gives such a certainty of proper graft attachment as performing intraoperative OCT. Moreover, OCT could be also useful in assessing the adequate Descemet membrane stripping. Intraoperative OCT analysis by revealing the residual interface space has a potential to reduce the post-operative disc dislocation rate.
Optical coherence tomography is a high speed, high resolution, non-contact optical imaging technique developed for noninvasive cross-sectional imaging in biologic systems. Recently, the system application was limited to the time before and after surgery.[5] After DSEK surgery, OCT was used to monitor cornea and graft morphometric dynamics and its influence on refractive changes after the surgery.[6] The prototype 3D anterior segment SD OCT device used intraoperatively was developed in 2010.[7] The first paper describing the use of handhold OCT (Bioptigen SD OCT) during the DSAEK to assess the donor-host interface was published in 2010.[8] This is the first report presenting the intraoperative commercially available OCT device.
In our opinion, there are two main problems regarding the intraoperative use of OCT: The surgery during the SD OCT exam is interrupted and there is a necessity of the use additional surgical drapes to prevent the possible touching of the operating field. This inconvenience could be removed by using C-arm allowing the OCT exam in the controlled manner. The ideal way would be to use integrated OCT and surgical microscope, similar to those used in the vitreoretinal surgery. To conclude: OCT assisted DSEK allows the assessment of the accuracy of the Descemet stripping and donor disc attachment.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Lee WB, Jacobs DS, Musch DC, Kaufman SC, Reinhart WJ, Shtein RM. Descemet's stripping endothelial keratoplasty: Safety and outcomes: A report by the American Academy of Ophthalmology. Ophthalmology. 2009;116:1818–30. doi: 10.1016/j.ophtha.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 2.Price FW, Jr, Price MO. Descemet's stripping with endothelial keratoplasty in 200 eyes: Early challenges and techniques to enhance donor adherence. J Cataract Refract Surg. 2006;32:411–8. doi: 10.1016/j.jcrs.2005.12.078. [DOI] [PubMed] [Google Scholar]
- 3.Terry MA, Shamie N, Chen ES, Hoar KL, Friend DJ. Endothelial keratoplasty a simplified technique to minimize graft dislocation, iatrogenic graft failure, and pupillary block. Ophthalmology. 2008;115:1179–86. doi: 10.1016/j.ophtha.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 4.Meisler DM, Dupps WJ, Jr, Covert DJ, Koenig SB. Use of an air-fluid exchange system to promote graft adhesion during Descemet's stripping automated endothelial keratoplasty. J Cataract Refract Surg. 2007;33:770–2. doi: 10.1016/j.jcrs.2006.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wylegała E, Teper S, Nowińska AK, Milka M, Dobrowolski D. Anterior segment imaging: Fourier-domain optical coherence tomography versus time-domain optical coherence tomography. J Cataract Refract Surg. 2009;35:1410–4. doi: 10.1016/j.jcrs.2009.03.034. [DOI] [PubMed] [Google Scholar]
- 6.Tarnawska D, Wylegala E. Monitoring cornea and graft morphometric dynamics after Descemet stripping and endothelial keratoplasty with anterior segment optical coherence tomography. Cornea. 2010;29:272–7. doi: 10.1097/ICO.0b013e3181b61496. [DOI] [PubMed] [Google Scholar]
- 7.Ide T, Wang J, Tao A, Leng T, Kymionis GD, O’Brien TP, et al. Intraoperative use of three-dimensional spectral-domain optical coherence tomography. Ophthalmic Surg Lasers Imaging. 2010;41:250–4. doi: 10.3928/15428877-20100303-15. [DOI] [PubMed] [Google Scholar]
- 8.Knecht PB, Kaufmann C, Menke MN, Watson SL, Bosch MM. Use of intraoperative fourier-domain anterior segment optical coherence tomography during Descemet stripping endothelial keratoplasty. Am J Ophthalmol. 2010;150:360–365. doi: 10.1016/j.ajo.2010.04.017. e2. [DOI] [PubMed] [Google Scholar]


