Abstract
Macular edema is a significant cause of vision loss in patients with central retinal vein occlusions and branch retinal vein occlusions. Vascular endothelial growth factor (VEGF) appears to be a key factor in the pathogenesis of this disease. Anti-VEGF therapy, such as intravitreal ranibizumab provides an effective treatment against vision-threatening macular edema. We report three patients of retinal vein occlusion with macular edema who demonstrated overnight resolution of macular edema following treatment with intravitreal ranibizumab (0.5 mg). 3D optical coherence tomography (Optovue) was used as a tool for comparison of the macular thickness before and after treatment. The significant reductions in the central foveal thickness demonstrated in these patients one night after intravitreal injections could have significant influence on modifying current treatment protocols. Early treatment of macular edema related to retinal venous occlusive disease with anti-VEGF injections could result in faster visual rehabilitation in these patients.
Keywords: Macular edema, optical coherence tomography, ranibizumab, retinal vein occlusion, vascular endothelial growth factor
Macular edema is a significant cause of vision loss in patients with central retinal vein occlusions (CRVOs) and branch retinal vein occlusions (BRVOs).[1] Ischemic as well as non-ischemic conditions of the inner retina in patients with CRVO and BRVO have been associated with increased capillary permeability, macular edema, and neovascularization.[1] Vascular endothelial growth factor (VEGF) is a key factor in the pathogenesis of this disease and has been found in increased concentrations in eyes with retinal venous occlusive disease (RVO).[1,2,3,4] Anti-VEGF therapy, such as intravitreal ranibizumab and bevacizumab may provide an effective treatment against vision-threatening macular edema.
We report three patients with RVO who showed a dramatic overnight reduction in macular edema following treatment with intravitreal ranibizumab.
Case Reports
Case 1
A 60-year-old hypertensive man presented with decreased vision in the left eye since 6 months. Patient had been diagnosed with ischemic CRVO and secondary glaucoma in the left eye. He had undergone trabeculectomy in the left eye and was previously treated with intravitreal bevacizumab followed by intravitreal Ozurdex for persistent macular edema. Anterior segment evaluation of left eye showed well-formed bleb, no neovascularisation in iris or angle. Intra-ocular pressure was within normal limits. Fundus evaluation of the left eye was suggestive of old CRVO with diffuse macular edema [Fig. 1a]. Fundus fluorescein angiography (FFA) showed leakage within the foveal avascular zone (FAZ) in the late phase, there was no leakage related to neovascularization [Fig. 1b]. 3D spectral domain optical coherence tomography (OCT) (Optovue) showed gross cystoid macular edema [Fig. 1c].
Figure 1.
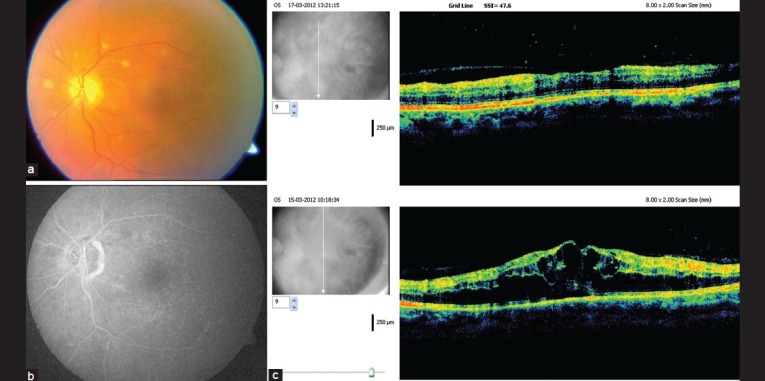
(a) Fundus photo of left eye of patient 1 demonstrating disc pallor with old central retinal vein occlusions, few hard exudates and mostly resolved retinal hemorrhages with persisting macular edema (b) Mid phase fundus fluorescein angiography picture of left eye of patient 1 showing minimal pooling of dye over foveal avascular zone (c) 3D optical coherence tomography pictures of the macula of left eye of patient 1 before and 1 day after intravitreal ranibizumab. The scan below shows diffuse macular edema while the upper scan shows resolved macular edema 1 day after treatment
Patient was treated with intravitreal ranibizumab (0.5 mg) in the left eye and 3D OCT was repeated the next day. A significant reduction in macular edema was demonstrated on OCT with reduction in central foveal thickness [Fig. 1c].
Case 2
A 70-year-old hypertensive “man presented with gross decrease in vision in the right eye since 1 month. Anterior segment examination and intra-ocular pressure were within normal limits, fundus evaluation of the right eye showed CRVO with retinal haemorrhages and cystoid macular edema. [Fig. 2a] FFA showed blocked fluorescence corresponding to retinal haemorrhages with leakage within the FAZ [Fig. 2b]. 3D OCT showed gross cystoid macular edema [Fig. 2c].
Figure 2.
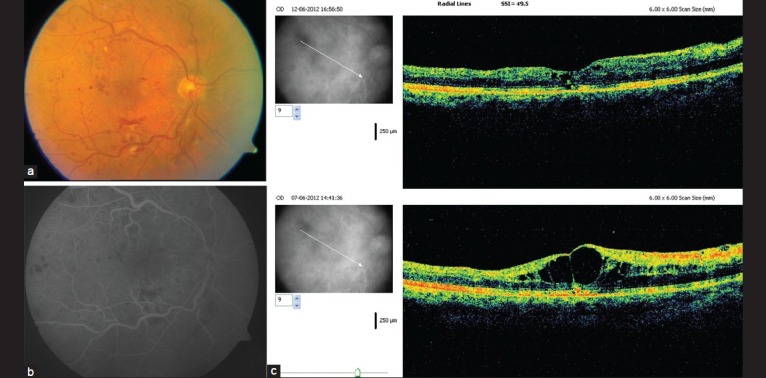
(a) Fundus photo of the right eye of patient 2 showing central retinal vein occlusions with tortuosity of veins around the disc with multiple retinal hemorrhages and diffuse macular edema (b) Early phase fundus fluorescein angiography of the right eye of patient 2 showing areas of blocked fluorescence corresponding to retinal hemorrhages and hyperfluorescence over the foveal avascular zone (c) 3D optical coherence tomography pictures of the macula of the right eye of patient 2 before and 1 day after intravitreal ranibizumab. The lower scan shows diffuse macular edema while the upper scan shows resolved macular edema 1 day after treatment
Patient was administered intravitreal ranibizumab (0.5 mg) in the right eye. 3D OCT demonstrated a dramatic overnight reduction in macular edema with reduction of central foveal thickness [Fig. 2c].
Case 3
A 50- year-old man presented with blurring of vision in the left eye since 6 months. Anterior segment evaluation and intra ocular pressure were within normal limits. Fundus evaluation of the left eye showed old inferotemporal BRVO with macular edema. Sectoral PRP marks were visible inferotemporally. Colour fundus photography [Fig. 3a] and 3D OCT was performed. OCT showed diffuse macular edema [Fig. 3b].
Figure 3.
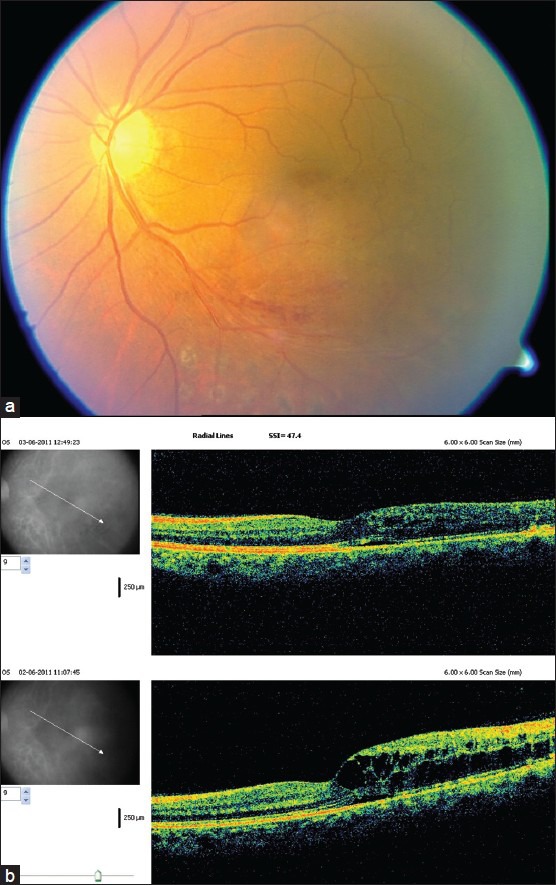
(a) Color fundus photo of the left eye of patient 3 showing inferotemporal branch retinal vein occlusions with retinal hemorrhages along inferotemporal arcade and diffuse macular edema. Old sectoral PRP marks are seen along and below the inferotemporal arcade (b) 3D optical coherence tomography pictures of the macula of left eye of patient 3 before and 1 day after intravitreal ranibizumab. The lower scan shows diffuse macular edema while the upper scan shows a significant reduction of macular edema 1 day after treatment
Patient was treated with intravitreal ranibizumab (0.5 mg) in the left eye. 3D OCT after 1 day showed a significant reduction in macular edema with a decrease in central foveal thickness [Fig. 3b].
Discussion
The standard of care for patients with CRVO-associated macular edema has been observation. Grid-laser photocoagulation represented the treatment for BRVO-induced macular edema according to the Branch Vein occlusion study, but the limited letter gain led to the pursuit of alternative treatment modalities.
In retinal vascular disorders with disruption of the inner blood-retinal barrier, visual acuity is altered in proportion to the central foveal thickness.
The CRUISE and BRAVO study evaluated the effect of ranibizumab on macular edema in patients with CRVO and BRVO diagnosed within a year from screening.[5,6] Eligible patients were randomized 1:1:1-6 monthly injections of 0.3 mg or 0.5 mg ranibizumab or sham injections. After 6 months, all patients with best-corrected visual acuity <20/40 or central subfield thickness >250 microns were to receive ranibizumab. BCVA score showed a 15-letter gain in BCVA from baseline to 6 months in 61% of patients with BRVO and 48% of patients with CRVO.
The GENEVA study evaluated the efficacy of dexamethasone intravitreal implant (0.7 mg and 0.35 mg) in comparision to sham treatment in the management of macular edema due to CRVO and BRVO.[7] A single treatment with dexamethasone implant 0.7 mg or 0.35 mg produced significantly greater improvements in visual acuity and decrease in central macular thickness on OCT than did a sham procedure. However, the BRAVO and CRUISE studies had shorter duration of macular edema as compared to the GENEVA study. Moreover the GENEVA study included both CRVO and BRVO patients.[5,6,7]
Early reduction of macular edema and photoreceptor recovery is vital for improvement of visual acuity. Maintenance of visual acuity gains with as-needed ranibizumab dosing after 6 months of monthly therapy in BRAVO and CRUISE study illustrates the same. However, in neither trial did patients in the sham/0.5 mg group achieve visual acuity gains from baseline as great as those of patients who received ranibizumab treatment beginning at day 0. This suggests that prolonged edema resulting from undertreatment, because of a PRN dosing schedule or delay in the initiation of treatment, may result in irreversible retinal damage.
There is lack of literature studying the immediate effect of anti VEGF drugs on macular edema and the associated changes in OCT. Most studies and published reports have followed up patients on a monthly basis. The BRAVO, CRUISE and GENEVA studies did not comment on the timing of improvement in terms of improvement of visual acuity and reduction in macular thickness, neither did these studies perform OCT on day 1 after treatment.
Early treatment of macular edema related to RVOs with anti-VEGF injections could result in faster visual rehabilitation in these patients. This is supported by the better results obtained in the BRAVO and CRUISE studies where 65% treated patients had macular edema of duration not more than 3 months. This is in contrast to the GENEVA study where only 14-17% of patients had macular edema of less than 3 months.[5,6,7] The significant reduction in central foveal thickness demonstrated in these patients after 1 day of intravitreal injections could have significant influence on modifying current treatment protocols.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994;331:1480–7. doi: 10.1056/NEJM199412013312203. [DOI] [PubMed] [Google Scholar]
- 2.Boyd SR, Zachary I, Chakravarthy U, Allen GJ, Wisdom GB, Cree IA, et al. Correlation of increased vascular endothelial growth factor with neovascularization and permeability in ischemic central vein occlusion. Arch Ophthalmol. 2002;120:1644–50. doi: 10.1001/archopht.120.12.1644. [DOI] [PubMed] [Google Scholar]
- 3.Noma H, Funatsu H, Yamasaki M, Tsukamoto H, Mimura T, Sone T, et al. Pathogenesis of macular edema with branch retinal vein occlusion and intraocular levels of vascular endothelial growth factor and interleukin-6. Am J Ophthalmol. 2005;140:256–61. doi: 10.1016/j.ajo.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Risard SM, Pieramici DJ, Rabena MD, Basefsky JC, Avery RL, Castellarin AA, et al. Intravitreal ranibizumab for macular edema secondary to central retinal vein occlusion. Retina. 2011;31:1060–7. doi: 10.1097/IAE.0b013e3181fbce76. [DOI] [PubMed] [Google Scholar]
- 5.Brown DM, Campochiaro PA, Bhisitkul RB, Ho AC, Gray S, Saroj N, et al. Sustained benefits from ranibizumab for macular edema following branch retinal vein occlusion: 12-month outcomes of a phase III study. Ophthalmology. 2011;118:1594–602. doi: 10.1016/j.ophtha.2011.02.022. [DOI] [PubMed] [Google Scholar]
- 6.Campochiaro PA, Brown DM, Awh CC, Lee SY, Gray S, Saroj N, et al. Sustained benefits from ranibizumab for macular edema following central retinal vein occlusion: Twelve-month outcomes of a phase III study. Ophthalmology. 2011;118:2041–9. doi: 10.1016/j.ophtha.2011.02.038. [DOI] [PubMed] [Google Scholar]
- 7.Haller JA, Bandello F, Belfort R, Jr, Blumenkranz MS, Gillies M, Heier J, et al. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010;117:1134–1146. doi: 10.1016/j.ophtha.2010.03.032. e3. [DOI] [PubMed] [Google Scholar]


