Abstract
Objectives
Compare primary care providers’ (PCPs) perceptions about dementia and its care within their healthcare organization with perceptions of other common chronic conditions, and explore factors associated with differences.
Design
Cross-sectional survey
Setting
3 California healthcare organizations
Participants
164 PCPs
Measurements
PCPs’ views about primary care for dementia, compared to heart disease, diabetes, and selected other conditions were analyzed. Differences in views across conditions by PCP type (internists, family physicians) were assessed. Multivariate analysis examined relationships between provider/practice characteristics and views about dementia care.
Results
More PCPs strongly agreed that: older patients with dementia are difficult to manage (24%) than for heart disease (5%) or diabetes (6%); PCPs can improve quality of life for heart disease (59%) and diabetes (62%) than for dementia (31%); older patients should be routinely screened for heart disease (64%) and diabetes (68%) than dementia (56%); and their organizations have expertise/referral resources to manage diabetes (49%) and heart disease (52%) than dementia (21%). More PCPs reported “almost effortless” organizational care coordination for heart disease (13%) or diabetes (14%) than for dementia (6%), and “a great deal”/“a lot” of room for improvement in their ability to manage dementia (51%) than incontinence, depression, or hypertension (7-34%; all P’s<0.05). Internists’ views regarding dementia care were less optimistic than family physicians, but PCP type was unrelated to views on diabetes or heart disease.
Conclusion
Improving primary care management of dementia should directly address PCP concerns about expertise/referral resources, difficulty of care provision, and PCP views about prospects for patient improvement.
Keywords: dementia, disease management, health services research, primary care, healthcare delivery
Introduction
Sixty-five percent of older Americans suffer from multiple chronic conditions, including heart disease, diabetes, and hypertension1, and an estimated 5.2 million suffer from dementia.2 Despite increasing prevalence and frequency of older patient visits to primary care providers (PCPs), dementia detection in primary care is low 3-5, and quality of care for dementia is lower than that for other common conditions.6, 7
PCPs manage patients with a broad range of chronic conditions such as heart disease, hypertension, depression, diabetes, and dementia. Although many of these conditions overlap with the domains of other specialties, PCPs often assume principal responsibility for their management. More so than for some diseases that are often managed in primary care settings, optimizing dementia care requires frequent interaction with caregivers and other family members, addressing caregiving needs, behavioral disturbances, loss of function, and connection of patients and caregivers to key resources in the community such as respite care.8, 9 It also requires vigilance for potential complications that typically arise in the course of this degenerative disease, so that they can be identified and managed before escalating to crises. The complexity of tasks and intensity of demands for evaluation and management of dementia may affect PCPs’ attitudes towards caring for these patients. Insufficient access to resources and care coordination may also affect providers’ perceptions of their ability to care for these patients.
We surveyed PCPs’ perceptions of dementia care as measured against their perceptions of other common chronic conditions affecting older primary care patients, including heart disease and diabetes. We assessed differences in providers’ perceptions of their capability within their health care organization to effectively manage dementia compared with other chronic conditions in elders. We also assessed whether type of PCP, provider demographics, practice characteristics, number of older patients seen, and knowledge were associated with attitudes and perceptions towards dementia care.
Methods
Sample and Data Collection
We surveyed by mail all PCPs at 18 outpatient clinics in 3 San Diego-area healthcare organizations that participated in a cluster randomized (clinic level), controlled trial of a dementia quality of care improvement intervention.10, 11 Surveys were conducted 9 months after initiation of patient enrollment into the trial. At 2 of the 3 organizations, providers were compensated $20 for survey participation; one organization did not allow compensation to its providers for research participation. Follow-up surveys were mailed to nonrespondents at 4 and 8 weeks after the initial mailing. Of the 230 PCPs including internists, family physicians, nurse practitioners and physician’s assistants, 164 (71.3%) completed the survey. Respondents and nonrespondents did not differ in terms of gender, PCP type, or years since graduation (all P’s>0.05). Provider knowledge about dementia across intervention and usual care arms was previously reported (for the purpose of this study’s aims, we excluded from our eligible sample two providers with added qualifications in geriatrics).10 The institutional review boards of University of California, Los Angeles and all participating health care organizations approved the study procedures.
Provider Survey Measures
Provider attitudes towards condition-specific primary care for older patients with dementia, heart disease, and diabetes (3 items per condition)
Three items assessed provider attitudes about managing older patients for each of 3 conditions: dementia, heart disease, and diabetes. One item addressed providers’ perception about difficulty managing each condition in primary care; a second addressed providers’ perception of their ability to significantly improve quality of life for older patients with each condition; and a third addressed providers’ belief about routine screening for each condition. Items were presented as statements and providers were asked their degree of agreement with each statement, using Likert scales (range: 1-6) from “strongly agree” to “strongly disagree”. For every item, the conditions were listed in this order: heart disease, dementia, and diabetes.
Provider perceptions about condition-specific care in their healthcare organization (2 items per condition)
One item assessed level of agreement with a statement that expertise and referral resources for managing each condition were available within their healthcare organization, using the same 6-category response choice defined above. Providers were also asked to rate their perceptions of care coordination within their organization for older patients with each condition, with 6 response choices ranging from “almost effortless” to “difficult struggle”.
Provider self-ratings of room for improvement in their care for older patients with specific conditions (1 item per condition)
Providers were asked to assess how much they could improve in their ability to evaluate and manage older patients having each of six conditions: hypertension, depression, dementia, gait disorders/falls, delirium, and incontinence. Response choices for these statements were “a great deal”, “a lot”, “some”, “a little”; and “not at all”.
Of these six attitude and perception items, only one differed across intervention and usual care group providers, with intervention providers more likely than usual care providers to agree that older patients with dementia are difficult to manage in primary care (P=0.03).10 With this one exception, no other differences were found between intervention and usual care group providers in any of the six attitude and perception items for any conditions or symptoms.
Potential Explanatory Variables
Knowledge About Management of Dementia
Providers were asked five multiple-choice questions regarding their knowledge about capacity determination, delirium evaluation, patient safety, and depression therapy in dementia.10 These items were based on guidelines recommended for primary care management of dementia.8, 9 Each item was scored as either correct or incorrect, and each respondent was given a summary knowledge score of 0-5, indicating the number of questions answered correctly. We previously reported that the only one of the four knowledge areas in which the dementia care management intervention had an impact was provider knowledge about capacity determination; a higher percentage of intervention than usual-care clinic providers answered both capacity determination knowledge questions correctly (adjusted difference=12%; adjusted odds ratio (AOR)=2.4; 95% confidence interval=1.2-4.8; P=0.02); there were no differences between groups in the other 3 knowledge areas.10
Provider and Practice Characteristics
Other survey items included provider gender, year of medical, osteopathic or nurse practitioner school graduation, and practice duration (years or months) in their current clinical setting. Providers were asked to estimate the number of unique dementia patients they had seen in their practice in the last 12 months and the percentage of patients over age 65. PCP type (internists, family physicians, and nurse practitioners/physician’s assistants) was determined from clinic records and web listings.
Analysis
For each item on attitude (3 items), perceptions about care (2 items), and amount PCP could improve his/her ability to provide care for the condition (1 item), differences in the distribution of the 5 or 6 response choices on each item for dementia versus each of the other conditions were compared using the Wilcoxon signed-rank test (Stata, version 9.2, College Station, Texas).
We conducted bivariate analyses of potential explanatory factors (provider and practice characteristics) and the 6 attitude, perception, and self-ratings of room for improvement items for each chronic condition and found that PCP type was the only factor having multiple statistically significant associations. We also found a trend toward a higher proportion of family physicians than other PCP types in the intervention arm (P=0.07). Because of this trend, we regressed each item for each condition onto PCP type, with intervention/usual care status as a covariate, to assess whether observed associations of provider type with attitudes/perceptions/self-ratings of ability to improve by chronic condition were independent of intervention/usual care status.
We explored whether provider’s belief about difficulty managing a condition (heart disease, dementia, diabetes) in primary care was associated with perceptions about availability of expertise and referral resources to manage the disorder in the healthcare organization, as well as how effortless or how much of a struggle care coordination and information sharing with other providers in the healthcare organization was in managing that condition, using Wilcoxon signed rank test.
To assess whether any of the potential explanatory variables accounted for variation in responses for dementia, we conducted bivariate analyses of each of the six items on attitude, perception, and self-reported ability with respect to dementia, with provider demographic and practice characteristics (including PCP type), individual dementia knowledge questions, and summary dementia knowledge score. To identify whether any provider or practice characteristics uniquely explained variation in provider attitudes, perceptions, and room for improvement in care for dementia, we then conducted multivariable analyses using ordered logistic regression.12 These models included as independent variables all variables from the bivariate analyses with a P-value ≤ 0.15. For models in which bivariate analyses showed that PCP type was associated with one of the six dependent variables (attitudes, perceptions, or room for dementia care improvement) at P ≤ 0.15, models were run once with two indicator variables for PCP type (family medicine, nurse practitioner/physician assistant, reference group: internal medicine), and then run a second time with a different reference group for PCP type (family medicine, internal medicine, reference group: nurse practitioner/physician assistant), to tease apart differences across all three PCP types. All models included site (healthcare organization) as a covariate, accounted for assignment of providers to intervention or usual care clinic groups, and accounted for clustering of clinics using the sandwich variance estimator (robust variance estimator and Huber correction) as implemented in Stata version 9.2.
Results
Forty-three percent of respondents were female. About equal proportions were internists (44%) and family physicians (45%), while 11% were nurse practitioners or physician assistants. Median number of dementia patients seen by providers in the prior year was 20 (interquartile range: 10-35). Of five multiple-choice dementia knowledge questions, respondents answered an average of 3.1 questions correctly.
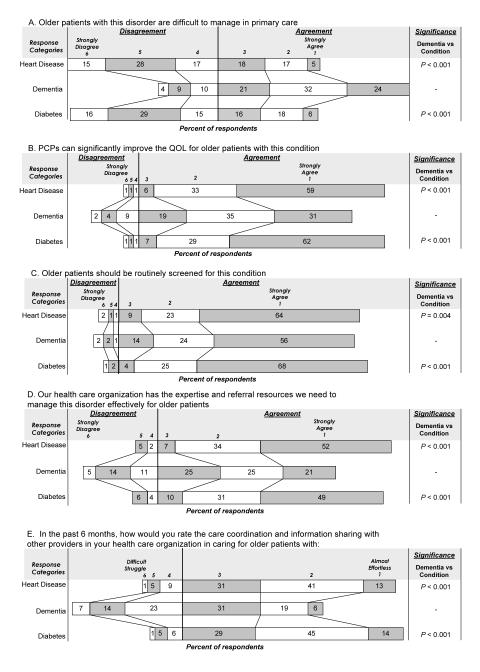
Provider Attitudes
Higher proportions of PCPs agreed that older patients with dementia are difficult to manage in primary care than those with diabetes (P<0.001), or heart disease (P<0.001; Figure 1A). Internists did not differ from family physicians on their views about difficulty managing older patients with dementia, heart disease, or diabetes in primary care (all P-values>0.05; Table 1).
Figure 1.
Provider Responses to Survey Items on Attitudes and Perceptions (N=164)
Bars represent provider responses for each item on provider attitudes (A-C) and perceptions (D, E) towards heart disease, dementia, or diabetes. Percent of respondents is indicated for each response category. Differences in the distribution of responses for dementia vs. another condition were compared using the Wilcoxon signed-rank test. Additionally, Pearson’s Chi square tests were used to compare differences in provider responses on each item using a cutpoint of 1= “Strongly agree” vs. all other responses for dementia and each of the other conditions. More PCPs strongly agreed that older patients with dementia are difficult to manage (24%) than did so for heart disease (5%) or diabetes (6%), that PCPs can improve quality of life for heart disease (59%) and diabetes (62%) than for dementia (31%); that older patients should be routinely screened for heart disease (64%) and diabetes (68%) than for dementia (56%); That their organizations have more organizational expertise and referral resources to manage diabetes (49%) and heart disease (52%) than for dementia (21%). More PCPs also reported “almost effortless” organizational care coordination for heart disease (13%) or diabetes (14%) than for dementia (6%; all P’s <0.05)
PCP=Primary Care Provider
QOL=Quality Of Life
Table 1.
Comparison of internists’ and family physicians’ responses to survey statements for dementia*
| Percent of Respondents | |||
|---|---|---|---|
|
| |||
| Internal Medicine (N=72) |
Family Physician (N=74) |
P- value† |
|
| A. Difficult to manage | |||
| Agree‡ | 75 | 76 | 0.76 |
| Disagree§ | 25 | 24 | |
| B. Significantly improve quality of life | |||
| Strongly Agree¶ | 24 | 40 | 0.03 |
| All others# | 76 | 60 | |
| C. Routinely screened | |||
| Strongly Agree¶ | 43 | 66 | 0.008 |
| All others# | 57 | 34 | |
| D. Healthcare organization has expertise & referral resources |
|||
| Agree‡ | 56 | 81 | 0.002 |
| Disagree§ | 44 | 19 | |
| E. Rate care coordination & information sharing in your healthcare organization |
|||
| Effortless** | 44 | 65 | 0.02 |
| Difficult†† | 56 | 35 | |
Note: Significance tests remained unchanged when covaried by intervention/usual care status.
There were no differences across internists and family physicians in their response to these items for heart disease and for diabetes (all P-values >0.05); data not shown
Significance determined by Chi-square analysis (STATA v.9.2, Stata Data Corp, College Station, TX)
Agree indicates a response selection of 1, 2, or 3 on a Likert scale of 1-6 (“strongly agree” to “strongly disagree”)
Disagree indicates a response selection of 4, 5, or 6 on a Likert scale of 1-6 (“strongly agree” to “strongly disagree”)
Strongly Agree indicates a response choice of 1 on a Likert scale of 1-6 (“strongly agree” to “strongly disagree”)
All others indicates a response selection of 2, 3, 4, 5, or 6 on a Likert scale of 1-6 (“strongly agree” to “strongly disagree”)
Effortless indicates a response selection of 1, 2, or 3 on a Likert scale of 1-6 (“almost effortless” to “difficult struggle”)
Difficult indicates a response selection of 4, 5, or 6 on a Likert scale of 1-6 (“almost effortless” to “difficult struggle”)
There was greater and stronger agreement that PCPs can improve quality of life for older patients with diabetes (P<0.001) or heart disease (P<0.001) than for those with dementia (Figure 1B). Smaller proportions of internists than family physicians strongly agreed that they could improve quality of life for older patients with dementia (24% vs. 40%, P=0.03, Table 1), but there was no difference in proportions of internists and family physicians indicating PCPs could significantly improve quality of life for heart disease or diabetes (all P’s >0.05).
Providers more strongly agreed that older patients should be routinely screened for diabetes (P<0.001) and heart disease (P=0.004), than for dementia (Figure 1C). Smaller proportions of internists than family physicians strongly agreed that older patients should be routinely screened for dementia (43% vs. 66%, P=0.008), but there was no difference between the proportion of internists and family physicians that strongly agreed about routine screening for heart disease or diabetes (P’s >0.05).
Perceptions about Condition-Specific Care in their Healthcare Organization
Fewer providers felt that their healthcare organization has expertise and referral resources to manage dementia compared to those with this view about heart disease (P<0.001) or diabetes (P<0.001; Figure 1D). This perception differed between internists and family physicians, with 81% of family physicians reporting agreement (responses ‘1’, ‘2’, or ‘3’) that their healthcare organization has resources to manage dementia, compared with 56% of internists (P=0.002), but no differences in the proportion of internists and family physicians in agreement with this statement regarding heart disease or diabetes (all P’s >0.05).
When asked about effort involved in care coordination and information sharing with providers in their healthcare organization, more providers rated it as greater difficulty for dementia than for heart disease or diabetes (P<0.001; Figure 1E). Internists were more likely than family physicians to report that care coordination and information sharing for dementia is difficult (56% internists, 35% family physicians, P=0.02), with no differences across specialty regarding heart disease or diabetes (P’s >0.05).
Exploratory Associations Between Difficulty with Management in Primary Care and Healthcare Organization Resources and Care Coordination
Extent of agreement with the statement that older patients with dementia are difficult to manage was inversely associated with the perception that their healthcare organization has expertise and referral resources to manage these patients (P<0.001) and with the perception that care coordination and information sharing with other providers in their healthcare organization was effortless for dementia (P<0.001). In contrast, there were no associations between providers’ perceptions of difficulty in managing patients with diabetes or heart disease in primary care and their beliefs about expertise and referral resources or care coordination at their healthcare organization (all P’s>0.05).
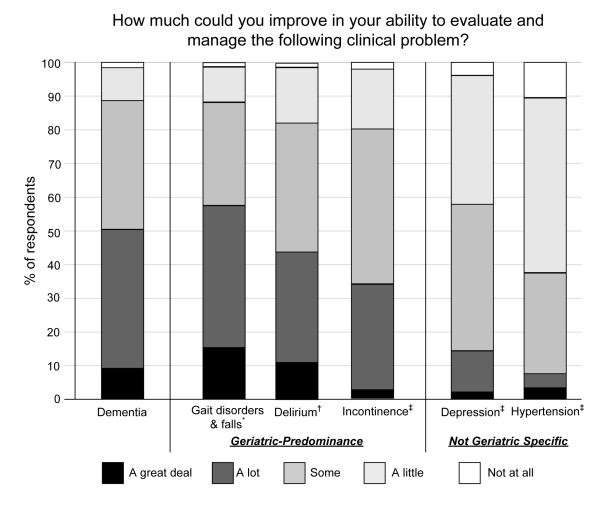
Provider Ratings of How Much their Ability to Care for Older Patients with Specific Conditions Could be Improved
About half of providers reported they could improve “a great deal” or “a lot” in evaluation and management of dementia (Figure 2). This proportion was no different to that for delirium and slightly lower than that for gait disorders/falls, but significantly higher than the proportions of providers with respect to incontinence, depression or hypertension evaluation and management (P’s<0.001; Figure 2). A smaller proportion of family physicians than internists (41% vs. 56%) reported more room for improvement in their ability to manage dementia, although the difference was not statistically significant. Only for incontinence did the two PCP types differ, with 42% of internists versus 23% of family physicians reporting “a great deal” or “a lot” of room for improvement (P=0.03).
Figure 2.
Provider Responses to Perceived Room for Improvement in PCPs Evaluation and Management for Different Conditions
Provider responses to one item for conditions predominant in geriatric patients (dementia, gait disorders and falls, delirium, incontinence), and for non-geriatric-specific conditions (depression, hypertension). For each condition, percent of respondents is indicated by response category, “a great deal”, “a lot”, “some”, “a little”, or “not at all”. Differences in the distribution of responses for dementia vs. another condition were compared using the Wilcoxon signed-rank test. Pearson’s Chi square tests were used to compare differences in provider responses on this item for dementia vs. each condition using a cutpoint of “a great deal” to “a lot” vs. all other responses. More PCPs responded thtat there is “a great deal” or “ a lot” of room for improvement in their ability to manage dementia (51%) than for incontinence (34%), depression (14%), or hypertension (7%; all P’s <0.01).
*P=0.04 for Wilcoxon signed rank test for condition compared to dementia
†P=0.06 for Wilcoxon signed rank test for condition compared to dementia
‡P<0.001 for Wilcoxon signed rank test for condition compared to dementia
Factors Explaining Variations in Provider Attitudes, Perceptions, and Self Assessment Skills for Dementia (Table 2)
Table 2.
Factors related to attitudes, perceptions, and self-rated room for improvement in dementia management
| Odds ratio | 95% Confidence Interval |
P-value | |
|---|---|---|---|
| A. Difficult to manage dementia in primary care* | |||
| - | - | - | |
| B. PCPs can improve the quality of life for older patients with dementia† |
|||
| Family physicians vs. internists | 2.82 | 1.51-5.27 | 0.003 |
| C. Older patients should be routinely screened for dementia‡ |
|||
| Family physicians vs. internists | 3.59 | 1.53-8.45 | 0.006 |
| D. Healthcare organization has expertise and referral resources to manage dementia effectively§ |
|||
| Family physicians vs. internists | 2.57 | 1.02-6.43 | 0.05 |
| E. Greater ease in dementia care coordination and information sharing with other providers in your healthcare organization¶ |
|||
| Family physicians vs. internists | 4.20 | 1.53-11.47 | 0.008 |
| NP/PAs vs. internists | 3.11 | 1.32-7.37 | 0.01 |
| Greater percentage of patients over age 65 | 0.97 | 0.96-0.99 | 0.01 |
| F. Greater room for improving ability to evaluate and manage dementia# |
|||
| Family physicians vs. internists | 0.46 | 0.21-1.00 | 0.05 |
| NP/PAs vs. family physicians | 9.46 | 2.94-30.42 | <0.001 |
| NP/PAs vs. internists | 4.35 | 1.30-14.65 | 0.02 |
| Lower volume of dementia patients | 1.01 | 1.00-1.02 | 0.02 |
This model had no bivariates with a P-value ≤ 0.15.
Model included all variables from bivariate analysis with a P-value ≤ 0.15: provider specialty, gender, score for one dementia knowledge question on patient safety, site, and intervention status. Only provider specialty had a significant P-value in multivariate analysis, as shown here.
Model included all variables from bivariate analysis with a P-value ≤ 0.15: provider specialty, summary dementia knowledge score, site, and intervention status. Only provider specialty had a significant P-value in multivariate analysis, as shown here.
Model included all variables from bivariate analysis with a P-value ≤ 0.15: provider specialty, number of years since professional school graduation, amount of time spent at current practice, summary dementia knowledge score, site, and intervention status. Only provider specialty had a significant P-value in multivariate analysis, as shown here.
Model included all variables from bivariate analysis with a P-value ≤ 0.15: provider specialty, number of patients over age 65, number of years since graduation, amount of time spent at current practice, summary dementia knowledge score, number of patients assigned to the dementia care management intervention, site, and intervention status. Only provider specialty and number of patients over age 65 had significant P-values in multivariate analysis, as shown here.
Model included all variables from bivariate analysis with a P-value ≤ 0.15: provider specialty, volume of dementia patients, number of patients over age 65, number of patients assigned to the dementia care management intervention, site, and intervention status. Only provider specialty and volume of dementia patients had significant P-values in multivariate analysis, as shown here.
PCP= Primary care physician
NP/PA= Nurse practitioner/Physician’s assistant
Ordered logistic regression analysis showed that compared to family practitioners, internists have lesser agreement with the statement that they can improve quality of life for older patients with dementia (P=0.003), that older patients should be routinely screened for dementia (P=0.006), and that their healthcare organization has the expertise and referral resources to manage dementia effectively (P=0.05). Internists were more likely than both family physicians (P=0.008) and nurse practitioner/physician assistants (P=0.01) to rate care coordination as difficult; internists tended to perceive more room for improvement in their ability to evaluate and manage dementia patients than family practitioners (P=0.05; Table 2). No other factor we analyzed was consistently associated with variations in attitudes and perceptions about dementia.
Discussion
We contrasted PCPs’ views about dementia with those of other chronic conditions common among older patients and found substantial differences on all attitudes and perceptions that were assessed. For example, more than three-fourths of providers felt that older patients with dementia were difficult to manage, while fewer than half shared that view with respect to heart disease. Nearly twice the proportion of providers strongly believed that PCPs could make a significant improvement in quality of life for older patients with diabetes and for older patients with heart disease, compared to the proportion holding that view about older patients with dementia. The differences we found reflect potentially more pessimism among providers in areas of routine screening, improving quality of life, and difficulty in managing dementia patients, relative to those with heart disease and diabetes.
Several factors may account for these findings. The particular difference in providers’ view of screening for dementia may stem from the lack of uniform agreement among providers that screening for dementia should occur in primary care, even though most would agree that older patients should be screened for functional status decline, which is related to dementia. Providers may feel more confident treating diabetes or heart disease because the nature of the intervention for these conditions differs markedly from dementia treatment. Accustomed to following standard diagnostic and laboratory measures such as HbA1c, lipid and blood pressure levels, providers may feel frustrated that such definitive measures are lacking for dementia management. Dementia management requires behavioral and psychosocial assessment, both of which require interpretation, making it difficult to define real differences when tracking the response to interventions over time. In other studies, PCPs express more comfort in their ability to manage what they see as “treatable” conditions than in their ability to manage dementia.13-15 Providers may also recognize that they can alter the natural history of the disease when treating heart disease or diabetes, whereas they may perceive that their ability to improve or slow the decline of cognitive function is very limited.
We found that providers who perceived less difficulty with dementia management also perceived adequate resources and support for management of older dementia patients. Unlike many other common conditions treated in primary care, optimal dementia management is highly dependent on accessing social services for behavior management, respite care, and other community resources that are prominent components of recommendations found in multiple practice guidelines.8, 9, 16 Indeed, there is strong evidence that receipt of services typically provided outside of traditional health care delivery systems, such as caregiver support and respite care, can delay institutionalization and reduce caregiver burden.17, 18 PCPs may have particular challenges in providing patients and caregivers with access to services provided by community agencies and with coordinating care across their healthcare organization and these community agencies.19
Large majorities of providers had positive assessments of their ability to evaluate and manage conditions not specific to geriatric patients, such as depression and hypertension. However, for conditions highly prevalent in geriatric patients such as dementia, gait disorders/falls, delirium, and incontinence,20 a third or more of providers identified substantial room for improvement in the care that they provide. These syndromes are generally more complex to manage compared to hypertension and depression, for which medications are often a mainstay of management.
Differences in attitudes about dementia between internists and family physicians may reflect differences in training between the two specialties. More positive attitudes about the utility of screening for dementia, care coordination, availability of resources, and improving quality of life reported by family physicians may reflect more emphasis in their training on providing comprehensive biopsychosocial care, with a greater focus on behavioral science.21 Compared to internists, family physicians have been found in other studies to have a greater likelihood of recognizing cognitive impairment 4, report higher confidence than internists in performing geriatric procedures 22, and have more training in psychosocial issues 23, 24.
This study has several limitations. The results may not be generalizable to other settings, as participants were from three healthcare organizations in one region of the United States that agreed to participate in an intervention study relating to dementia care. Although we found differences in PCPs’ perceptions of dementia relative to other conditions in primary care, we cannot be certain that changing these attitudes and perceptions will change their practice styles in managing dementia.
We found substantial differences and generally less optimistic views among PCPs’ perceptions about dementia relative to their views about heart disease and depression. Quality improvement programs for heart disease and diabetes are relatively common and increasingly being disseminated in many healthcare systems.25-30 Two recently published trials have found that chronic care models also substantially improve quality of care for dementia.11, 31 Yet dissemination and implementation of such models may be more challenging for dementia without making it explicit that these models can improve the organizational capacity to coordinate and provide referral resources for key components of dementia care. Quality of care improvement programs for dementia should optimize availability of community resources, but also should address directly the concerns of PCPs about being able to manage this socially complex disorder, obtaining appropriate consultation, and improving quality of life for their patients, as well as dementia caregivers. Including the caregiver as part of the dementia management program can result in substantial improvements in care quality for dementia patients 11, and can provide meaningful milestones to track progress in dementia care. Programs to improve care should also address differences across primary care specialties in concerns about dementia management. Care management approaches may empower PCPs by providing a structure through which they can be proactive within their healthcare organization in improving the evaluation and management of older patients with dementia, in a way that makes such care less burdensome. The challenge lies in instituting cultural changes in primary care practice and training – such as making the caregiver a focal point of care interventions – to elevate this type of care to the same status as practices for treating heart disease, diabetes, and other common chronic conditions that rely more centrally on prescribing medications.
Acknowledgements
The authors thank Elise Berry, BS, Karen Connor RN, MBA, PhD, Robert DeMonte, MD, Theodore Ganiats, MD, and Lisa Heikoff, MD for assisting in subject recruitment and survey data collection. Martin Lee, PhD provided suggestions about the statistical approach.
Funding: This study was supported by the California Department of Public Health (contract 06-55314) for the Alzheimer’s Disease Research Center of California and the American Heart Association (AHA) through funding for the AHA/Pharmaceutical Roundtable Outcomes Research Center at UCLA. Dr. Shapiro was supported in part by UCLA/DREW Project EXPORT, National Institutes of Health, National Center on Minority Health and Health Disparities (P20MD000182).
Sponsor’s Role: None
Footnotes
The results of this study were presented at the 32nd Annual Meeting of the Society of General Internal Medicine in 2009.
Conflict of Interest: Drs. Harris, Shapiro, and Ms. Vassar have no conflicts of interest to report. Drs. Chodosh and Vickrey received honoraria from SCAN Healthplan. Dr. Vickrey received a grant from Genentech, Inc., and served as a consultant for Secured Independence, Inc. and EMD Serono Canada, Inc.
The definitive version is available at www.blackwell-synergy.com. The definitive publisher’s version is available at www3.interscience.wiley.com.
Full text: http://onlinelibrary.wiley.com/doi/10.1111/j.1532-5415.2009.02572.x/full.
References
- 1.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162:2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 2.Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. 2007;29(1-2):125–132. doi: 10.1159/000109998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Callahan CM, Hendrie HC, Tierney WM. Documentation and evaluation of cognitive impairment in elderly primary care patients. Ann Intern Med. 1995;122:422–429. doi: 10.7326/0003-4819-122-6-199503150-00004. [DOI] [PubMed] [Google Scholar]
- 4.Chodosh J, Petitti DB, Elliott M, et al. Physician recognition of cognitive impairment: evaluating the need for improvement. J Am Geriatr Soc. 2004;52:1051–1059. doi: 10.1111/j.1532-5415.2004.52301.x. [DOI] [PubMed] [Google Scholar]
- 5.Valcour VG, Masaki KH, Curb JD, et al. The detection of dementia in the primary care setting. Arch Intern Med. 2000;160:2964–2968. doi: 10.1001/archinte.160.19.2964. [DOI] [PubMed] [Google Scholar]
- 6.Rosen CS, Chow HC, Greenbaum MA, et al. How well are clinicians following dementia practice guidelines? Alzheimer Dis Assoc Disord. 2002;16:15–23. doi: 10.1097/00002093-200201000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Wenger NS, Solomon DH, Roth CP, et al. The quality of medical care provided to vulnerable community-dwelling older patients. Ann Intern Med. 2003;139:740–747. doi: 10.7326/0003-4819-139-9-200311040-00008. [DOI] [PubMed] [Google Scholar]
- 8.Cummings JL, Frank JC, Cherry D, et al. Guidelines for managing Alzheimer’s disease: Part II. Treatment. Am Fam Physician. 2002;65:2525–2534. [PubMed] [Google Scholar]
- 9.Cummings JL, Frank JC, Cherry D, et al. Guidelines for managing Alzheimer’s disease: part I. Assessment. Am Fam Physician. 2002;65:2263–2272. [PubMed] [Google Scholar]
- 10.Chodosh J, Berry E, Lee M, et al. Effect of a dementia care management intervention on primary care provider knowledge, attitudes, and perceptions of quality of care. J Am Geriatr Soc. 2006;54:311–317. doi: 10.1111/j.1532-5415.2005.00564.x. [DOI] [PubMed] [Google Scholar]
- 11.Vickrey BG, Mittman BS, Connor KI, et al. The effect of a disease management intervention on quality and outcomes of dementia care: a randomized, controlled trial. Ann Intern Med. 2006;145:713–726. doi: 10.7326/0003-4819-145-10-200611210-00004. [DOI] [PubMed] [Google Scholar]
- 12.Bender R, Grouven U. Ordinal logistic regression in medical research. J R Coll Physicians Lond. 1997 Sep-Oct;31(5):546–551. [PMC free article] [PubMed] [Google Scholar]
- 13.Adams WL, McIlvain HE, Geske JA, et al. Physicians’ perspectives on caring for cognitively impaired elders. Gerontologist. 2005;45:231–239. doi: 10.1093/geront/45.2.231. [DOI] [PubMed] [Google Scholar]
- 14.Boise L, Camicioli R, Morgan DL, et al. Diagnosing dementia: perspectives of primary care physicians. Gerontologist. 1999;39:457–464. doi: 10.1093/geront/39.4.457. [DOI] [PubMed] [Google Scholar]
- 15.Connell CM, Boise L, Stuckey JC, et al. Attitudes toward the diagnosis and disclosure of dementia among family caregivers and primary care physicians. Gerontologist. 2004;44:500–507. doi: 10.1093/geront/44.4.500. [DOI] [PubMed] [Google Scholar]
- 16.Diagnosis, management, and treatment of dementia: A practical guide for primary care physicians. American Medical Association; Chicago: 1999. [Google Scholar]
- 17.Brodaty H, Green A, Koschera A. Meta-analysis of psychosocial interventions for caregivers of people with dementia. J Am Geriatr Soc. 2003;51:657–664. doi: 10.1034/j.1600-0579.2003.00210.x. [DOI] [PubMed] [Google Scholar]
- 18.Mittelman MS, Haley WE, Clay OJ, et al. Improving caregiver well-being delays nursing home placement of patients with Alzheimer disease. Neurology. 2006;67:1592–1599. doi: 10.1212/01.wnl.0000242727.81172.91. [DOI] [PubMed] [Google Scholar]
- 19.Fortinsky RH. How linked are physicians to community support services for their patients with dementia? Journal of Applied Gerontology. 1998;17:480–498. [Google Scholar]
- 20.Inouye SK, Studenski S, Tinetti ME, et al. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55:780–791. doi: 10.1111/j.1532-5415.2007.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Physicians AAoF [Accessed October 17, 2008];Family Medicine, Scope, and Philosophical Statement. http://www.aafp.org/online/en/home/policy/policies/f/scope/scopephil.html.
- 22.Robinson BE, Barry PP, Renick N, et al. Physician confidence and interest in learning more about common geriatric topics: a needs assessment. J Am Geriatr Soc. 2001;49:963–967. doi: 10.1046/j.1532-5415.2001.49188.x. [DOI] [PubMed] [Google Scholar]
- 23.Paasche-Orlow M, Roter D. The communication patterns of internal medicine and family practice physicians. J Am Board Fam Pract. 2003;16:485–493. doi: 10.3122/jabfm.16.6.485. [DOI] [PubMed] [Google Scholar]
- 24.Gaufberg EH, Joseph RC, Pels RJ, et al. Psychosocial training in U.S. internal medicine and family practice residency programs. Acad Med. 2001;76:738–742. doi: 10.1097/00001888-200107000-00020. [DOI] [PubMed] [Google Scholar]
- 25.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002;288:1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 26.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. Jama. 2002 Oct 9;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 27.Fonarow GC, Gawlinski A, Moughrabi S, et al. Improved treatment of coronary heart disease by implementation of a Cardiac Hospitalization Atherosclerosis Management Program (CHAMP) Am J Cardiol. 2001;87:819–822. doi: 10.1016/s0002-9149(00)01519-8. [DOI] [PubMed] [Google Scholar]
- 28.Piatt GA, Orchard TJ, Emerson S, et al. Translating the chronic care model into the community: results from a randomized controlled trial of a multifaceted diabetes care intervention. Diabetes Care. 2006;29:811–817. doi: 10.2337/diacare.29.04.06.dc05-1785. [DOI] [PubMed] [Google Scholar]
- 29.Rich MW. Heart failure disease management: a critical review. J Card Fail. 1999;5:64–75. doi: 10.1016/s1071-9164(99)90026-x. [DOI] [PubMed] [Google Scholar]
- 30.Wagner EH, Glasgow RE, Davis C, et al. Quality improvement in chronic illness care: a collaborative approach. Jt Comm J Qual Improv. 2001;27:63–80. doi: 10.1016/s1070-3241(01)27007-2. [DOI] [PubMed] [Google Scholar]
- 31.Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA. 2006;295:2148–2157. doi: 10.1001/jama.295.18.2148. [DOI] [PubMed] [Google Scholar]