Abstract
The current study explores the personality traits of compulsivity (e.g., sense of orderliness and duty to perform tasks completely) and restricted expression (e.g., emotion expression difficulties) as potential moderators of the relation between affect lability and frequency of hard exercise episodes in a sample of individuals with bulimic pathology. Participants were 204 adult females recruited in five Midwestern cities who met criteria for threshold or subthreshold bulimia nervosa (BN). Compulsivity was found to significantly moderate the relation between affect lability and number of hard exercise episodes over the past 28 days, such that among those with high compulsivity, level of affect lability was associated with the number of hard exercise episodes; whereas, among those with low compulsivity, affect lability was not associated with the number of hard exercise episodes. The same pattern of findings emerged for restricted expression; however, this finding approached, but did not reach statistical significance. As such, it appears that affect lability is differentially related to hard exercise among individuals with BN depending upon the level of compulsivity and, to a more limited extent, restricted expression. These results suggest that, for individuals with BN with either compulsivity or restricted expression, focusing treatment on increasing flexibility and/or verbal expression of emotions may help them in the context of intense, fluctuating affect.
Keywords: exercise, emotion regulation, bulimia nervosa, affect lability, compulsivity, emotion expression
Binge eating and the compensatory behavior of purging (e.g., vomiting) have both been understood as modes of affect regulation in the context of bulimia nervosa (BN). That is, there is evidence to suggest that these bulimic behaviors may serve to help an individual manage his/her negative affect or escape from aversive self-awareness (Heatherton & Baumeister, 1991). This conceptualization has been put forth both in theoretical and narrative accounts of BN and has been tested empirically using various research methods, including experiments, ecological momentary assessment/experience sampling techniques, and retrospective reports (e.g., Engelberg, Steiger, Gauvin, & Wonderlich, 2007; Fox & Froom, 2009; Moon & Berenbaum, 2009; Telch, 1997). While some work has considered the potential affect regulation function of another compensatory behavior, hard exercise, this area of research is much less developed. In the current paper, we define hard exercise as intense exercise engaged in as a means of controlling one’s weight or shape. To date, there has been no consideration of factors that, in combination with affect regulation difficulties, may be associated with hard exercise. The current study tests whether the personality variables of compulsivity and restricted expression may moderate the relation between affect lability and hard exercise in a sample of women with threshold or subthreshold BN.
Hard exercise is a common symptom of eating disorders with prevalence rates within various eating disorder samples ranging from 20% to 58% (Dalle Grave, Calugi, & Marchesini, 2008; De Young & Anderson, 2010; Shroff et al., 2006), and a prevalence estimate of about 40% among individuals with BN (39.3% - Dalle Grave et al., 2008; 43.5%; Shroff et al., 2006). Given that a large proportion of individuals with BN engage in hard exercise and that this behavioral pattern can lead to excessive weight loss and possible medical and psychological complications such as potential changes in cardiac function, arrhythmias, and body image problems (La Gerche, Connelly, Mooney, Maclsaac, & Prior, 2008; La Gerche & Prior, 2007; Seigel & Hetta, 2001), it is important to more thoroughly explore factors associated with hard exercise among this population. Additionally, hard exercise has been found both among individuals with BN and unselected college samples to be associated with suicidal behavior and capability, as well as pain insensitivity (Smith et al., 2012), which suggests that hard exercise can be a clinically concerning behavior that requires increased understanding. It should be noted that not all forms of exercise, even among those with disordered eating, are necessarily deleterious in terms of medical complications or psychological difficulties. However, use of hard exercise to control weight or shape (as defined here) is arguably less healthy than exercise motivated by health.
1.1. Hard Exercise and Affect Regulation
There is a modest but building evidence base to suggest that hard exercise may serve as a form of affect regulation for individuals with eating disorders. For example, Powell and Thelen (1996) asked women with BN to report on their mood every two hours for six days, finding that momentary negative affect significantly decreased following exercise behaviors. These results provide in-the-moment evidence that exercise may serve as a means of down-regulating negative affect among individuals with BN. Additionally, using ecological momentary assessment methodology, Goldschmidt et al. (in press) found that individuals with BN and a history of anorexia nervosa (AN), but not those without a history of AN, reported a decrease in negative affect following exercise (although this difference was not statistically significant). This finding tentatively suggests that a history of AN may influence the extent to which exercise is motivated by affect regulation. Other work indicating associations between negative affect and exercise among those with eating disorders at least suggests a possible role for exercise in managing mood difficulties. Peñas-Lledo, Vaz Leal, and Waller (2002) found that individuals with anorexia nervosa who engaged in excessive exercise also tended to struggle with depression and anxiety, and Waller et al. (2003) found that excessive exercise in an eating disordered sample was associated with state anger. All of these findings taken together provide some evidence to suggest that exercise may, at least in part, be motivated by a desire to decrease aversive affect among individuals with eating disorders.
In nonclinical samples, numerous studies using experimental paradigms have found that exercise leads to improvement in mood; in particular, this phenomenon occurs by means of either increasing positive affect or decreasing negative affect (Anderson & Brice, 2011; Dunn & McAuley, 2000; Lutz, Lochbaum, & Turnbow, 2003; Steptoe & Cox, 1988). Work using experience sampling methodology has yielded similar findings. For example, using a nonclinical college sample, LePage and Crowther (2010) found that women reported lower negative affect, as well as higher positive affect following exercise episodes. Also using experience sampling methodology and a nonclinical college sample, De Young and Anderson (2010) found that 58% of their sample reported engaging in exercise in response to negative affect and that these individuals reported elevated eating pathology, as well as lower body image and self-esteem, compared to individuals who did not report using exercise as an affect regulation mechanism. In line with this finding, Adkins and Keel (2005) found that the extent to which college men and women reported exercising to manage mood or stress was positively correlated with number of exercise episodes engaged in (r = .34) and obligatory exercise scores (r = .41). These findings suggest that when exercise is motivated by negative affect, it may more likely be accompanied by eating disorder-related symptoms. Work examining personality, exercise, and affect found that neuroticism significantly predicted mood improvement as a motivation for exercise in a nonclinical sample (Davis, Fox, Brewer, & Ratusny, 1995), suggesting that perhaps the personality variable of neuroticism may impact the extent to which exercise is motivated by affect.
Thus, there is some evidence to suggest that exercise among individuals with BN and nonclinical populations may be reinforced by means of its modulating effects on aversive (as well as positive) affect. It appears that for at least some individuals, hard exercise is engaged in as a response to negative affect, possibly serving to decrease or modulate unpleasant affective experience. But for whom among those with BN does negative affect especially drive the behavioral pattern of hard exercise? In this study, using a sample of women with bulimic pathology, we consider personality factors that may help determine for whom emotion dysregulation might be associated with hard exercise.
1.2. Affect Lability
The current study examines a particular component of emotion dysregulation: affect lability. Affect lability refers to the extent to which affective experience changes over time in terms of intensity, valence, or discrete emotion category, and is generally considered aversive (Oliver & Simons, 2004). We see a clear theoretical connection between affect lability and emotion dysregulation, because if one’s affective state is shifting rapidly in an uncontrolled way, he/she likely has difficulty regulating his/her affect. This idea is supported by the fact that affect lability, based upon factor analytic analyses, is understood as a component of the emotion dysregulation factor of the Dimensional Assessment of Personality Pathology (Livesley & Larstone, 2008).
Research has indicated that individuals with BN experience significantly more fluctuations in mood compared to control individuals (Johnson & Larson, 1982), and that, in general, affect lability is an important correlate of binge eating and BN (Cassin & von Ranson, 2005; Greenberg & Harvey, 1987). Given the aversive quality of affect lability, individuals with BN are theoretically motivated to escape unpleasant affective states or to make efforts to modulate the fluctuations in affect over time. We consider two dimensions of personality that may direct efforts at affect regulation toward hard exercise: compulsivity and restricted expression.
1.3. Compulsivity
Compulsivity is a personality trait involving orderliness and conscientiousness characterized by a “strong sense of duty and obligation to complete all tasks thoroughly and meticulously” (Krueger et al., 2007, p. 68). Research has found that compulsivity (particularly when combined with impulsivity) is related to bulimic symptomatology, as well as personality problems, depressive symptoms, and substance use among women with BN (Engel et al., 2005). Further, research has indicated that the personality trait of compulsivity is elevated among individuals with BN (Raymond, Neumeyer, Thuras, Weller, Eckert, Crow, & Mitchell, 1999) and that individuals who report engaging in binge-purge behavior (i.e., individuals with BN or anorexia nervosa, binge/purge subtype) endorse similarly high levels of compulsivity as individuals with restricting anorexia nervosa (Claes, Vandereycken, & Vertommen, 2002). Thus, overall, compulsivity appears to have ties with bulimic pathology.
Little work has explored the relation between compulsivity and exercise among individuals with eating disorders in general or BN in particular. In one study that examined this relation, Shroff et al. (2006) found that individuals with eating disorders who reported excessive exercise (defined based upon quantity and the extent to which the exercise interfered with daily life) tended to display compulsive personality characteristics. Similarly, Davis, Kaptein, Kaplan, Olmsted, and Woodside (1998) found that individuals with AN who reported a high level of exercise scored significantly higher than their moderate/non-exercising counterparts on a measure of obsessive-compulsive personality. No research, to the authors’ knowledge, has specifically explored compulsivity and exercise in individuals with BN in particular. Connecting compulsivity with emotion in an eating disorder sample, Lawson, Waller, and Lockwood (2007) found that high levels of avoided emotional arousal were associated with compulsivity, indicating that individuals intent on escaping aversive affective states may engage in compulsive behaviors that aid in avoidance of emotion; exercise may serve this function. Exercise may be particularly effective for those in need of orderliness and predictability given that exercise can be done in a routine and automatized fashion with the help of work out equipment, timers, speedometers, and calorie counters. For this reason, those with combined compulsivity and affect lability may engage in exercise to stabilize emotional state or decrease intense negative affect in a way that aligns with needs related to compulsivity.
1.4. Restricted Expression
Restricted expression can be understood as a personality trait that encompasses emotion expression and interpersonal difficulties (Krueger, Skodol, Livesley, Shrout, & Huang, 2007). Emotion expression difficulties have been observed in individuals with eating disorders and in association with eating pathology. For example, Ioannou and Fox (2009) found that emotion expression skills were negatively correlated with Eating Disorder Inventory (EDI; Garner, Olmsted, & Polivy, 1983) subscale scores that reflect core disordered eating pathology: drive for thinness, bulimia, and body dissatisfaction. Additionally, Forbush and Watson (2006) explored emotional inhibition among individuals with varying eating disorder diagnoses and found that individuals with BN had higher emotional inhibition as compared to individuals with anorexia nervosa and healthy controls. Thus, evidence suggests that restricted expression, at least those difficulties related to emotional expression, may be related to eating disorder severity and BN in particular.
To the authors’ knowledge, no research has explored possible relationships between restricted expression and hard exercise in individuals with BN. Given that restricted expression encompasses expressive and interpersonal difficulties, for highly emotionally restricted individuals with BN, bulimic behaviors (like hard exercise) may become a primary means of emotional expression or outlet. Further, it is possible that this behavioral expression may become a means of regulating aversive emotional states. It is possible that affect lability and restricted expression combine in women with BN such that those who are both high in affect lability and restricted expression may engage in more hard exercise. In this scenario, exercise may serve as a grounding activity in the midst of affect fluctuation, particularly among those with few expressive outlets for managing this fluctuating affect (i.e., those high in restricted expression).
1.5. The Current Study
While there is growing evidence to suggest that hard exercise as a compensatory behavior of BN is related to affect regulation, to date, no work has examined potential moderators of the relation between affect lability (a component of emotion dysregulation) and frequency of hard exercise. The current study explored compulsivity and restricted expression as potential moderators of this relationship. In particular, we examined whether the relation between affect lability and number of hard exercise episodes over the past month is influenced by the personality traits of compulsivity and restricted expression. We hypothesized that these personality variables would interact with affect lability to identify levels of hard exercise. More specifically, we hypothesized that individuals with high affect lability and either high compulsivity or high restricted expression would indicate the highest frequencies of hard exercise episodes over the past 28 days.
2. Method
2.1. Participants
Participants were 204 adult women recruited through community advertising and eating disorder clinics in five Midwestern cities (Madison, WI; Minneapolis, MN; Fargo, ND; Chicago, IL; and Columbia, MO). Based upon a telephone interview, 144 (71%) met full diagnostic criteria for BN according to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV; APA, 1994), and 60 (29%) met criteria for subthreshold BN, defined as (a) binge eating and compensatory behavior occurring at least once per week over the past three months, or (b) compensatory behavior occurring at least once per week along with subjective bulimic episodes (i.e., episodes of binge eating that are not objectively large, but do involve loss of control). In order to further characterize this sample in terms of bulimic behaviors, we note that, over the past 28 days, self-report data yielded a mean number of 15.75 objective binges (SD = 23.56), 12.91 subjective binges (SD = 14.46), 22.5 vomiting episodes (SD = 36.4), 2.75 laxative use episodes (SD = 6.3), and 1.1 diuretic use episodes (SD = 5.1).
Mean age of participants was 25.7 years (SD = 8.8 years). The majority of participants was single and had never been married (75%), self-identified as Caucasian (n = 185, 90.7%; Asian: n = 7, 3.4%; Black: n = 5, 2.5%; Hispanic: n = 3, 1.5%; other races/ethnicities: n = 4, 2.0%), and had at least some college education (92%). Based upon self-reported weight and height, mean body mass index (BMI) was 22.9 kg/m2 (SD = 5.2).
2.2. Procedure
Trained interviewers administered a telephone interview that included the eating disorder module from the Structured Clinical Interview for DSM-IV, Patient Edition (SCID-P; First Spitzer, Gibbon, & Williams, 1995). Interviewers used criteria for binge eating established in the Eating Disorder Examination (EDE; Fairburn & Cooper, 1993) to determine if reported food portions during binge eating episodes were objectively large in amount. Participants who met current DSM-IV diagnostic criteria for threshold or subthreshold BN were scheduled for an in-person visit where they provided informed consent, completed a set of questionnaires, and received $50 compensation for their participation. The Institutional Review Boards at each study site approved this study.
2.3. Measures
2.3.1. The Structured Clinical Interview for DSM-IV, Patient Edition (SCID-P) Eating Disorder Module (First et al., 1995)
The SCID-P is a widely used semi-structured interview that assesses the presence of Axis I disorders. In this study, the eating disorder module of the SCID-P was used during the phone screen in order to determine diagnostic eligibility. Prior research suggests that phone versus in-person SCID interviews are not significantly different from each other (Keel et al., 1999).
2.3.2. Eating Disorder Examination-Questionnaire (EDE-Q; Fairburn & Beglin, 1994)
The EDE-Q is a 36-item self-report survey adapted from the EDE interview (Fairburn & Cooper, 1993). Relevant to the current study, number of hard exercise episodes was assessed by asking the number of times participants “exercised hard as a means of controlling your shape or weight” over the past 28 days. Although only one item was used to assess exercise, we note that other studies have used one- or two-item measures of exercise and found it to be a reliable approach (e.g., Joiner & Tickle, 1998; Mechanic & Hansell, 1987; Tanasescu, Letizmann, Rimm, Willett, Stampfer, & Hu, 2002). Given that individuals themselves are asked to judge for themselves whether or not exercise is “hard,” it should be acknowledged that we examined perceived hard exercise rather than hard exercise according to objective criteria.
2.3.3. Dimensional Assessment of Personality Pathology—Basic Questionnaire (DAPP-BQ; Liveseley, Jackson, & Schroeder, 1992)
The DAPP-BQ is a 290-item self-report measure of personality that encompasses 18 subscales, including the subscales of interest in the current study, including affect lability, compulsivity, and restricted expression. The affect lability factor reflects emotionality and fluctuating affect, the compulsivity factor reflects a need for order and exactness, and the restricted expression reflects difficulties expressing emotion and personal information to relevant others. The DAPP-BQ has acceptable psychometric properties with internal consistency coefficients for subscales ranging from 0.83 to 0.94, and test-retest reliability over a 3-week period from 0.81 to 0.93 (Livesley et al., 2008). Good validity has been demonstrated by high convergence between the DAPP-BQ and the Schedule for Nonadaptive and Adaptive Personality (SNAP; Clark, 1993). In the current study, the three subscales of restricted expression, compulsivity, and affect lability had coefficient alphas ranging from 0.90 to 0.92.
2.4. Analytic Strategy
To test the hypothesized moderator models involving the dependent variable of frequency of hard exercise episodes we used hierarchical multiple regression. In Step 1, affect lability and the moderator of interest (e.g., restricted expression) were entered as independent variables. In Step 2, the two-way interaction of affect lability and the moderator (e.g., affect lability x restricted expression) was entered. Interaction terms were created by multiplying together the centered independent variables as recommended by Frazier, Tix, and Barron (2004) for continuous variables. The nature of the significant interactions was assessed via simple slope analyses (Aiken & West, 1991).
3. Results
3.1. Descriptive Statistics
The average number of hard exercise episodes engaged in over the past 28 days was 6.89 (SD = 10.75) with a wide range from zero to 84 episodes, a median of 1.00 episodes, and the upper quartile was reporting at least 11 episodes over the past 28 days. Affect lability was significantly positively correlated with both compulsivity (r = .22, p = .002) and restricted expression (r = .14, p = .046), while compulsivity and restricted expression were also significantly positively correlated (r = .30, p < .001). These small to moderate correlations indicate that the independent variables of interest are related, but distinct constructs. Compulsivity was significantly correlated with the number of hard exercise episodes (r = .15, p = .039), with greater compulsivity associated with more episodes of hard exercise. In contrast, neither affect lability (r = .12, p = .094) nor restricted expression (r = .05, p = .493) were significantly related to frequency of hard exercise.
3.2. Interactive Findings
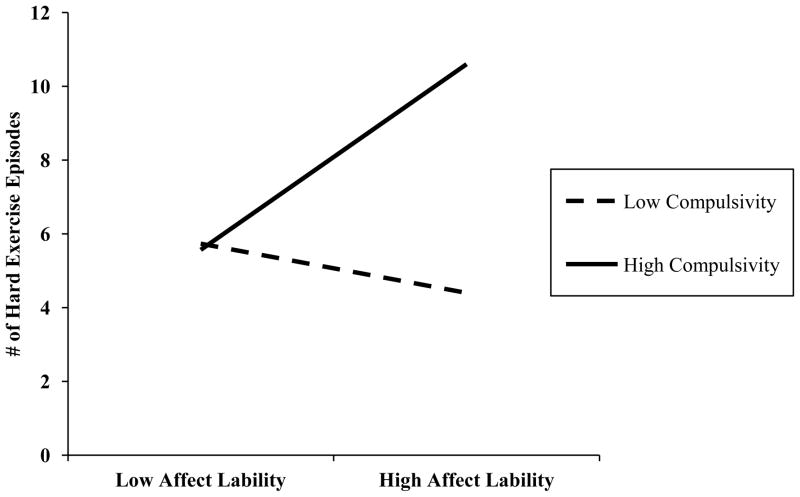
The interaction of affect lability and compulsivity was significant in identifying frequency of hard exercise episodes, t(199) = 2.20, p = .029 (see Table 2). As displayed in Figure 1, which depicts slopes based upon regression model coefficients, those with high levels of affect lability who also had high levels of compulsivity engaged in a higher number of hard exercise episodes over the past 28 days than those with high affect lability and low compulsivity. In contrast, among those with low levels of affect lability, level of compulsivity was not significantly related to the number of hard exercise episodes engaged in. (For all figures, high and low levels of the independent variables were determined by one standard deviation above and below the mean, respectively). Simple slope analyses indicated that affect lability was significantly associated with number of hard exercise episodes at high levels of compulsivity (1 SD above the mean), β = .24, t(199) = 2.43, p = .016, but not at low levels of compulsivity (1 SD below the mean), β = −.06, t(199) = −.64, p = .524. Due to the skewed nature of the hard exercise variable (many zeros with several extreme-range data points), we reran this regression using a log transformed dependent variable and the same pattern of findings emerged.
Table 2.
Hierarchical Multiple Regression Analyses of the Interaction of Affect Lability and Personality Variables with Number of Hard Exercise Episodes over the Past 28 Days as the Dependent Variable
| Step and predictors | B | SE B | β | t (dfs) | p | ΔR2 |
|---|---|---|---|---|---|---|
| Step 1 | .02 | |||||
| Affect Lability | .07 | .06 | .09 | 1.27 (2,200) | .206 | |
| Compulsivity | .11 | .07 | .13 | 1.75 (2,200) | .082 | |
| Step 2 | .05* | |||||
| Affect Lability x Compulsivity | .01 | .01 | .15* | 2.20 (1,199) | .029 | |
|
| ||||||
| Step 1 | .02 | |||||
| Affect Lability | .09 | .06 | .11 | 1.60 (2,200) | .111 | |
| Restricted Expression | .03 | .06 | .03 | .46 (2,200) | .648 | |
| Step 2 | .03^ | |||||
| Affect Lability x Restricted Expression | .01 | .01 | .13^ | 1.88 (1,199) | .062 | |
Note.
p < .10.
p < .05.
Figure 1.
The interaction of affect lability and compulsivity with number of hard exercise episodes over the past 28 days as the dependent variable.
The affect lability x restricted expression interaction approached significance in identifying frequency of hard exercise episodes, t(199) = 1.88, p = .062 (see Table 2). Those with high levels of affect lability who also had high levels of restricted expression reported a marginally higher frequency of hard exercise episodes over the past 28 days than those with high affect lability and low restricted expression (see Figure 2). In contrast, among those with low levels of affect lability, level of restricted expression did not differentiate as clearly the number of hard exercise episodes engaged in. Simple slope analyses indicated that affect lability was significantly associated with the number of hard exercise episodes at high levels of restricted expression (1 SD above the mean), β = .26, t(199) = 2.47, p = .014, but not at low levels of restricted expression (1 SD below the mean), β = −.02, t(199) = −.17, p = .866. Due to the skewed nature of the hard exercise variable (many zeros with several extreme-range data points), we reran this regression using a log transformed dependent variable and the same general pattern of findings emerged, within the context of trend-level findings (p = .117).
Figure 2.
The interaction of affect lability and restricted expression with number of hard exercise episodes over the past 28 days as the dependent variable.
Of note, we also ran the hierarchical multiple regressions excluding those who reported no episodes of hard exercise in the past 28 days (n = 98), resulting in 106 with at least one episode of hard exercise. The affect lability x compulsivity interaction remained significant, t(102) = 2.11, p = .037 with the same pattern of findings (i.e., the combination of high affect lability and high compulsivity associated with highest frequency of hard exercise). The affect lability x restricted expression interaction was also significant when limiting analyses to those with at least one episode of hard exercise, t(102) = 2.32, p = .022, and the pattern of results was also similar to that observed in the full sample with the combination of high affect lability and high restricted expression associated with the highest number of hard exercise episodes over the past 28 days.
Additionally, we ran each of our hierarchical multiple regressions again after controlling for age, BMI, site difference, and number of bulimic behaviors engaged in over the past 28 days (including OBEs, SBEs, vomiting, laxative use, and diuretic use episodes) and found no meaningful differences in our interactive findings.
4. Discussion
This study examined potential moderators in the relation between affect lability and hard exercise episode frequency among individuals with BN, finding that compulsivity moderated this relation. Further, there was a trend toward restricted expression also moderating the relation between affect lability and hard exercise; when analyses were limited to those who engaged in at least some hard exercise over the past 28 days, restricted expression was a significant moderator in this model. In particular, it was found that needing activities and the environment to be “just right” and orderly and/or being characterized as intensely conscientious (i.e., high compulsivity) in combination with high affect lability was associated with a high frequency of hard exercise episodes. Similarly, it was found that difficulty expressing oneself verbally (i.e., high restricted expression) in combination with fluctuating, often aversive affect (i.e., high affect lability) was associated with a high frequency of hard exercise. On the other hand, results suggested that when one is low in compulsivity (or restricted expression), affect lability does not appear to be related to frequency of hard exercise. These results suggest that within a sample of women with BN, the personality traits of compulsivity and restricted expression may be associated with the extent to which hard exercise is related to affect volatility. Thus, hard exercise may not serve as an emotion regulation technique for all individuals with BN who report engaging in hard exercise.
These findings are consistent with the hypothesis that hard exercise may be a particularly effective emotion regulation technique for those who tend to need extensive order and predictability in their lives and/or who have difficulty expressing emotions to others interpersonally. Exercise is a behavior that can be done in a highly ritualized and repetitive way, particularly when using machines or equipment that calculate exact calorie expenditure, distance, and heart rate. As such, for those high on compulsivity, hard exercise may serve as an effective safety behavior to manage affective discomfort in a way that is maximally tolerable, because it aligns with personality needs of order and predictability.
When considering the interaction of restricted expression and affect lability in the whole sample, trend-level findings emerged before and after performing a log transformation of the hard exercise variable; however, when this interaction was considered in the subset of individuals who reported at least some hard exercise over the past month, the interaction was significant regardless of whether or not a log transformation was applied to the hard exercise dependent variable. These discrepant findings taken together suggest that there may be unique characteristics of those who engage in at least one episode of hard exercise that lend themselves to different relations between interpersonal expressivity, affect, and hard exercise. Given the trend-level interaction in the full sample, future research is needed to replicate and expand upon this finding.
But, why would hard exercise be particularly effective for affect regulation among individuals with restricted expression? Hard exercise may serve as a replacement for verbal emotional expression and thus function as an emotional outlet for those with difficulties expressing emotions in conventional ways. Further, exercise may provide a form of social connectedness that may be otherwise hard to achieve due to restricted expression. Hard exercise, depending upon where it is performed, may serve as a means of engaging with the world without having to express oneself or take the initiative to connect with others. For example, a person may find that being in the presence of others at the gym while exercising or participating in an intense spinning class with others may give a sense of replaced connectedness in the context of actual isolation or interpersonal connection difficulties, with hard exercise thus providing an interpersonal element at the same time as it serves an affect regulation function. Of note, the current study did not assess whether hard exercise was completed in a social versus non-social context; therefore, this hypothesis is offered tentatively and requires future research. Additionally, this possible explanation would not elucidate the use of solitary hard exercise methods, such as running outdoors or on a treadmill in the solitude of one’s room.
It is interesting to note that there was a weak, but significant positive correlation between hard exercise and compulsivity, but not with affect lability or restricted expression. The correlation between number of hard exercise episodes and compulsivity is in line with previous studies that have found connections between hard (or excessive) exercise and compulsive personality characteristics among individuals with eating disorders (e.g., Davis et al., 1998; Shroff et al., 2006). No prior work, however, to the authors’ knowledge, has found a significant correlation between hard exercise and compulsivity in a sample of individuals with only bulimic-type psychopathology. The lack of significant correlations between affect lability and restricted expression with hard exercise, combined with the interactive findings involving these constructs, suggests that hard exercise is not on its own related to either of these variables, but rather it is the combined effects of affect lability and restricted expression that are related to hard exercise episode frequency.
4.1. Strengths
The current study contributes to the literature by expanding our understanding of the relation between affect lability and hard exercise using more complex models (i.e., moderator models), as well as well-established and validated measures. Additional strengths of the current study include the use of a clinical sample, the fact that data were collected from multiple sites, and the inclusion of subthreshold BN cases. In particular, the use of multiple data collection sites increased the generalizability of study results by introducing geographic diversity to the sample. The inclusion of both subthreshold and threshold cases of BN increased the clinical diversity of the current sample and further contributed to the generalizability of study findings.
4.2. Limitations and Future Directions
While results of the current study extend prior work, there are several limitations and related future directions that warrant attention. The cross-sectional nature of the study limited our ability to make conclusions regarding direction of influence. Future research should examine the prospective relations between study constructs, as it is possible that changes in emotion dysregulation (e.g., decrease in emotion dysregulation/affect lability) may contribute to decreased reliance on hard exercise as a means of mood regulation, even if personality (e.g., restricted expression, compulsivity) remains the same as is likely given its trait-like nature (e.g., McCrae & Costa, 1997). Additionally, using an ecological momentary assessment approach may shed light on the micro-relations and temporal ordering between the study constructs. For example, does affect lability over the course of a given day predict the presence of hard exercise episodes on that day (or the following day) and is this relation strengthened among those who are high in compulsivity and/or restricted expression? It may also be important for future research to examine the role of specific discrete emotions, such as anger (e.g., Engel et al., 2007), in the prediction of hard exercise. Another remaining question that extends from our findings is whether or not individuals with the combination of affect lability and one or both of these personality characteristics are more likely to engage in hard exercise than other compensatory behaviors, and, if so, why that might be. Is hard exercise particularly sought out above and beyond other behaviors among those with these combinations of characteristics?
There were several measurement limitations of importance in the current study. One measurement limitation is that affect lability and the personality constructs were assessed using the same questionnaire, resulting in shared method variance; future work should assess these constructs using separate assessment tools. Additionally, even though the current study measures hard exercise using a well-validated and widely used measure of eating disorder symptomatology (i.e., the EDE-Q), assessing hard exercise with one item from this measure is a limitation of the current study. In particular, a single item does not capture detailed information regarding length, intensity, and context of exercise (e.g., location of exercise; presence of others or not). Future research should examine other ways of assessing this construct. For example, what are the implications of leaving the definition of “hard exercise” fairly subjective (as was done in the current study) versus specifying an amount of time or a level of intensity that would be necessary for an exercise episode to be defined as “hard”? Further, how might the use of differing definitions of hard exercise impact the relations among the study constructs? Lastly, the fact that all constructs were assessed using self-report questionnaires is another limitation in the current study.
Additionally, the inclusion of both subthreshold and full threshold bulimic presentations may have introduced concerns regarding group differences within the sample. In particular, individuals with SBE-only presentations may have had different patterns of hard exercise behavior than individuals with OBE-only or combined-type (i.e., both OBEs and SBEs) presentations. Few differences have been found between SBE-only and OBE-only presentations in past work, but future work should consider these different diagnostic presentations in relation to hard exercise behaviors in particular (Brownstone et al., 2013; Goossens, Soenens, & Braet, 2009).
4.3. Clinical Implications
In sum, the current work contributes to a better understanding of whom among individuals with bulimic symptomatology may engage in hard exercise in the context of affect lability. Given the current findings, clinicians may find it useful to assess the extent to which their clients struggle with compulsivity and restricted expression in order to determine the variety of functions that hard exercise may serve. Interventions for hard exercise among those with threshold/subthreshold BN may then be improved by adapting them based upon personality characteristics of the client being treated. More specifically, interventions intended to decrease the use of hard exercise for individuals with BN may be improved by increasing clients’ comfort with unpredictability and lack of order and/or focusing on interpersonal, expressive skills.
For clients high in restricted expression, clinicians may find that Interpersonal Psychotherapy (which has shown promise in the treatment of BN; Fairburn, Kirk, O’Connor, & Cooper, 1986) and/or focusing on identifying and expressing emotions verbally in session may improve emotional expression and interpersonal relationships, in turn decreasing client reliance on hard exercise. For clients high in compulsivity, a focus on increasing tolerance of uncertainty and distress via exposure and teaching of distress tolerance skills may make it more possible for the client to seek out alternative, less predictable and structured modes of affect regulation like hard exercise. In particular, treatment may involve exposure to general lack of structure (and the anxiety that may result from that lack of structure). For example, clients may benefit from deliberately engaging in behaviors like arriving late for appointments, doing assignments for work or school slightly imperfectly, or not looking at indicators of distance or calorie burning during exercise, and then “sitting with” the anxiety without engaging in compulsive behaviors such as exercise.
Table 1.
Means, Standard Deviations, and Correlations for the Study Variables (N = 204)
| 1 | 2 | 3 | 4 | ||
|---|---|---|---|---|---|
| 1. Affect Lability | - | M = 51.29, SD = 13.42 | |||
| 2. Restricted Expression | .14* | - | M = 47.80, SD = 13.07 | ||
| 3. Compulsivity | .22** | .30*** | - | M = 54.06, SD = 11.88 | |
| 4. Number of Hard Exercise Episodes | .12 | .05 | .15* | - | M = 6.89, SD = 10.75 |
Note. Affect lability, restricted expression, and compulsivity are subscales of the Dimensional Assessment of Personality Pathology-Basic Questionnaire. Number of hard exercise episodes refers to exercise episodes over the past 28 days. Variables are continuous with higher values reflecting higher levels of the construct.
p < .05.
p < .01.
p < .001.
Highlights.
Compulsivity (C) moderated relation between affect lability (AL) & hard exercise.
Restricted expression (RE) moderated this relation as well among exercisers.
AL was related to hard exercise when C or RE were high (not when low).
Personality traits may influence motivation behind hard exercise in BN.
Flexibility & expressive skills in treatment may decrease hard exercise in BN.
Acknowledgments
Role of Funding Sources:
Research for this study was supported by the following grants: 1 R01-MH/DK58820, 1 R01-DK61973, 1 R01-MH59100, 1 R01-MH66287, P30-DK50456, K02-MH65919, and 1 R01-MH59234 from NIH and a University of Missouri Research Council Grant, the John Simon Guggenheim Foundation, and the Walden W. and Jean Young Shaw Foundation. These sources of funding had no role in study design, collection, analysis, or interpretation of data, writing of the manuscript, or deciding to submit the manuscript for publication.
Footnotes
Contributors:
Authors C, E, F, G, H, I, J, and K designed the study and wrote the protocol. Author A conducted literature searches and provided summaries of previous research studies. Author A conducted the statistical analysis. Author A wrote the first draft of the manuscript and Author K provided feedback across various drafts. All authors contributed to and have approved the final manuscript.
Conflict of Interest:
None of the authors have any conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Lisa M. Brownstone, Email: lisa.brownstone@unc.edu.
Ellen E. Fitzsimmons-Craft, Email: fitzsimmonscraft@unc.edu.
Stephen A. Wonderlich, Email: Swonderlich@nrifargo.com.
Thomas E. Joiner, Email: joiner@psy.fsu.edu.
Daniel Le Grange, Email: legrange@uchicago.edu.
James E. Mitchell, Email: Jmitchell@nrifargo.com.
Scott J. Crow, Email: crowx002@umn.edu.
Carol B. Peterson, Email: peter161@umn.edu.
Ross D. Crosby, Email: Rcrosby@nrifargo.com.
Marjorie H. Klein, Email: mhklein@facstaff.wisc.edu.
Anna M. Bardone-Cone, Email: bardonecone@unc.edu.
References
- Adkins EC, Keel PK. Does “excessive” or “compulsive” best describe exercise as a symptom of bulimia nervosa? International Journal of Eating Disorders. 2005;38:24–29. doi: 10.1002/eat.20140. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publications; 1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Anderson RJ, Brice S. The mood-enhancing benefits of exercise: Memory biases augment the effect. Psychology of Sport and Exercise. 2011;12:79–82. doi: 10.1016/j.psychsport.2010.08.003. [DOI] [Google Scholar]
- Brownstone LM, Bardone-Cone AM, Fitzsimmons-Craft EE, Printz K, Le Grange D, Joiner T. Subjective and objective binge eating in relation to eating disorder symptomatology, negative affect, and personality dimensions. International Journal of Eating Disorders. 2013;46:66–76. doi: 10.1002/eat.22066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassin SE, von Ranson KM. Personality eating disorders: A decade in review. Clinical Psychology Review. 2005;25:895–916. doi: 10.1016/j.cpr.2005.04.012. [DOI] [PubMed] [Google Scholar]
- Claes L, Vandereycken W, Vertommen H. Impulsive and compulsive traits in eating disordered patients compared to controls. Personality and Individual Differences. 2002;32:707–714. doi: 10.1016/S0191-8869(01)00071-X. [DOI] [Google Scholar]
- Clark LA. Personality disorder diagnosis: Limitations of the five factor model. Psychological Inquiry. 1993;4:100–104. doi: 10.1207/s15327965pli0402_5. [DOI] [Google Scholar]
- Dalle Grave R, Calugi S, Marchesini G. Compulsive exercise to control shape or weight in eating disorders: Prevalence, associated features, and treatment outcome. Comprehensive Psychiatry. 2008;49:346–352. doi: 10.1016/j.comppsych.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Davis C, Fox J, Brewer H, Ratusny D. Motivations to exercise as a function of personality characteristics, age, and gender. Personality and Individual Differences. 1995;19:165–174. doi: 10.1016/0191-8869(95)00030-A. [DOI] [Google Scholar]
- Davis C, Kaptein S, Kaplan AS, Olmsted MP, Woodside DB. Obsessionality in anorexia nervosa: The moderating influence of exercise. Psychosomatic Medicine. 1998;60:192–197. doi: 10.1097/00006842-199803000-00015. [DOI] [PubMed] [Google Scholar]
- De Young KP, Anderson DA. Prevalence and correlates of exercise motivated by negative affect. International Journal of Eating Disorders. 2010;43:50–58. doi: 10.1002/eat.20656. [DOI] [PubMed] [Google Scholar]
- Dunn EC, McAuley E. Affective responses to exercise bouts of varying intensities. Journal of Social Behavior and Personality. 2000;15:201–214. doi: 10.415/209-9838. [DOI] [Google Scholar]
- Engel SG, Boseck JJ, Crosby RD, Wonderlich SA, Mitchell JE, Smyth J, Steiger H. The relationship of momentary anger and impulsivity to bulimic behavior. Behaviour Research and Therapy. 2007;45:437–447. doi: 10.1016/j.brat.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Engel SG, Corneliussen SJ, Wonderlich SA, Crosby RD, le Grange D, Crow S, Steiger H. Impulsivity and compulsivity in bulimia nervosa. International Journal of Eating Disorders. 2005;38:244–251. doi: 10.1002/eat.20169. [DOI] [PubMed] [Google Scholar]
- Engelberg MJ, Steiger H, Gauvin L, Wonderlich SA. Binge antecedents in bulimic syndromes: An examination of dissociation and negative affect. International Journal of Eating Disorders. 2007;40:531–536. doi: 10.1002/eat.20399. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16:363–370. doi: 10.1002/1098-108X(199412)16:4<363::AID-EAT2260160405>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. 12. New York: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- Fairburn CG, Kirk J, O’Connor M, Cooper PJ. A comparison of two psychological treatments for bulimia nervosa. Behavior Research and Therapy. 1986;24:629–643. doi: 10.1016/0005-7967(86)90058-6. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for the DSM-IV Axis I Disorders-Patient Edition (SCID-I/P, version 2) New York State Psychiatric Institute, Biometrics Research Department; 1995. [Google Scholar]
- Forbush K, Watson D. Emotional inhibition and personality traits: A comparison of women with anorexia, bulimia, and normal controls. Annals of Clinical Psychiatry. 2006;18:115–121. doi: 10.1080/10401230600614637. [DOI] [PubMed] [Google Scholar]
- Fox JRE, Froom K. Eating disorders: A basic emotion perspective. Clinical Psychology. 2009;335:328–335. doi: 10.1002/cpp.622. [DOI] [PubMed] [Google Scholar]
- Frazier PA, Tix AP, Barron KE. Testing moderator and mediator effects in counseling psychology research. Journal of Counseling Psychology. 2004;51:115–134. doi: 10.1037/0022-0167.51.1.115. [DOI] [Google Scholar]
- Garner DM, Olmsted MP, Polivy J. Development and validation of multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders. 1983;2:15–34. doi: 10.1002/1098-108X(198321)2:2<15::AID-EAT2260020203>3.0.CO;2-6. [DOI] [Google Scholar]
- Goldschmidt AB, Peterson CB, Wonderlich SA, Crosby RD, Engel SG, Mitchell JE, Crow SJ, Cao L, Berg KC. Trait-level and momentary correlates of bulimia nervosa with a history of anorexia nervosa. International Journal of Eating Disorders. doi: 10.1002/eat.22054. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goossens L, Soenens B, Braet C. Prevalence and characteristics of binge eating in an adolescent community sample. Journal of Clinical Child and Adolescent Psychology. 2009;38:342–353. doi: 10.1080/15374410902851697. [DOI] [PubMed] [Google Scholar]
- Greenberg BR, Harvey PD. Affective lability versus depression as determinants of binge eating. Addictive Behaviors. 1987;12:357–361. doi: 10.1016/0306-4603(87)90049-9. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110:86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Ioannou K, Fox JRE. Perception of threat from emotions and its role in poor emotional expression within eating pathology. Clinical Psychology and Psychotherapy. 2009;16:336–347. doi: 10.1002/cpp.632. [DOI] [PubMed] [Google Scholar]
- Johnson C, Larson R. Bulimia: An analysis of moods and behavior. Psychosomatic Medicine. 1982;44:341–351. doi: 10.1097/00006842-198209000-00003. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Tickle JJ. Exercise and depressive and anxious symptoms: What is the nature of their interrelations? Journal of Occupational Rehabilitation. 1998;8:191–198. doi: 10.1023/A:1021326406744. [DOI] [Google Scholar]
- Keel PK, Mitchell JE, Miller KB, Davis TL, Crow SJ. Long-term outcome of bulimia nervosa. Archives of General Psychiatry. 1999;56:63–69. doi: 10.1001/archpsyc.56.1.63. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Skodol AE, Livesley WJ, Shrout RE, Huang Y. Synthesizing dimensional and categorical approaches to personality disorders: Refining the research agenda for DSM-V Axis II. International Journal of Methods in Psychiatric Research. 2007;16:S65–S73. doi: 10.1002/mpr.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Gerche A, Connelly KA, Mooney DJ, Maclsaac AL, Prior DL. Biochemical and functional abnormalities of left and right ventricular function after ultra-endurance exercise. Heart. 2008;94:860–866. doi: 10.1136/hrt.2006.101063. [DOI] [PubMed] [Google Scholar]
- La Gerche A, Prior DL. Exercise—Is it possible to have too much of a good thing? Heart, Lung, and Circulation. 2007;16:S102–S104. doi: 10.1016/j.hlc.2007.03.014. [DOI] [PubMed] [Google Scholar]
- Lawson R, Waller G, Lockwood R. Cognitive and process in eating-disordered patients with obsessive-compulsive features. Eating Behaviors. 2007;8:305–310. doi: 10.1016/j.eatbeh.2006.11.006. [DOI] [PubMed] [Google Scholar]
- LePage ML, Crowther JH. The effects of exercise on body satisfaction and affect. Body Image. 2010;7:124–130. doi: 10.1016/j.bodyim.2009.12.002. [DOI] [PubMed] [Google Scholar]
- Livesley WJ, Jackson DN, Schroeder ML. Factorial structure of traits delineating personality disorders in clinical and general populations. Journal of Abnormal Psychology. 1992;101:432–440. doi: 10.1037/0021-843X.101.3.432. [DOI] [PubMed] [Google Scholar]
- Livesley WJ, Larstone RM. The Dimensional Assessment of Personality Pathology (DAPP) In: Boyle GJ, Matthews G, Saklofske DH, editors. The SAGE handbook of personality theory and assessment. Thousand Oaks, California: SAGE Publications Ltd; 2008. [Google Scholar]
- Lutz R, Lochbaum M, Turnbow K. The role of relative autonomy in post-exercise affect responding. Journal of Sport Behavior. 2003;26:137–154. [Google Scholar]
- McCrae RR, Costa PT. Personality trait structure as a human universal. American Psychologist. 1997;52:509–516. doi: 10.1037//0003-066x.52.5.509. http://dx.doi.org/10.1037/0003-066X.52.5.509. [DOI] [PubMed] [Google Scholar]
- Mechanic D, Hansell S. Adolescent competence, psychological well-being, and self-assessed physical health. Journal of Health and Social Behavior. 1987;28:364–374. doi: 10.2307/2136790. [DOI] [PubMed] [Google Scholar]
- Moon A, Berenbaum H. Emotional awareness and emotional eating. Cognition & Emotion. 2009;23:417–429. doi: 10.1080/02699930801961798. [DOI] [Google Scholar]
- Oliver MNI, Simons JS. The affect lability scales: Development of a short-form measure. Personality and Individual Differences. 2004;37:1279–1288. doi: 10.1016/j.paid.2003.12.013. [DOI] [Google Scholar]
- Peñas-Lledo E, Vaz Leal FJ, Waller G. Excessive exercise in anorexia nervosa and bulimia nervosa: Relation to eating characteristics and general psychopathology. International Journal of Eating Disorders. 2002;31:370–375. doi: 10.1002/eat.10042. [DOI] [PubMed] [Google Scholar]
- Powell AL, Thelen MH. Emotions and cognitions associated with bingeing and weight control behavior in bulimia. Journal of Psychosomatic Research. 1996;40:317–328. doi: 10.1016/0022-3999(95)00641-9. [DOI] [PubMed] [Google Scholar]
- Raymond NC, Neumeyer B, Thuras P, Weller CL, Eckert ED, Crow SJ, Mitchell JE. Compulsive and impulsive traits in individuals with obese binge eating disorder and bulimia nervosa. Eating Disorders. 1999;7:299–317. doi: 10.1080/10640269908251201. [DOI] [Google Scholar]
- Seigel K, Hetta K. Exercise and eating disorder symptoms among females. Eating and Weight Disorders. 2001;6:32–39. doi: 10.1007/BF03339749. [DOI] [PubMed] [Google Scholar]
- Shieh G. Detecting interaction effects in moderated multiple regression with continuous variables: Power and sample size considerations. Organizational Research Methods. 2009;12:510–528. doi: 10.1177/1094428108320370. [DOI] [Google Scholar]
- Shroff H, Reba L, Thornton LM, Tozzi F, Klump KL, Berretini WH, Bulik CM. Features associated with excessive exercise in women with eating disorders. International Journal of Eating Disorders. 2006;39:454–461. doi: 10.1002/eat.20247. [DOI] [PubMed] [Google Scholar]
- Smith AR, Fink EL, Anestis MD, Ribeiro JD, Gordond KH, Davis H, Joiner TE. Exercise caution: Over-exercise is associated with suicidality among individuals with disordered eating. 2012. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Cox S. Acute effects of aerobic exercise on mood. Health Psychology. 1988;7:329–340. doi: 10.1037/0278-6133.7.4.329. [DOI] [PubMed] [Google Scholar]
- Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. Journal of the American Medical Association. 2002;288:1994–2000. doi: 10.1001/jama.288.16.1994. [DOI] [PubMed] [Google Scholar]
- Telch CF. Skills training treatment for adaptive affect regulation in a woman with binge-eating disorder. International Journal of Eating Disorders. 1997;22:77–81. doi: 10.1002/(SICI)1098-108X(199707)22:1<77::AID-EAT10>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- Waller G, Babbs M, Milligan R, Meyer C, Ohanian V, Leung N. Anger and core beliefs in eating disorders. International Journal of Eating Disorders. 2003;34:118–124. doi: 10.1002/eat.1016. [DOI] [PubMed] [Google Scholar]