Abstract
Aplastic anemia is a bone marrow failure syndrome characterized by peripheral cytopenias and hypocellular bone marrow. Although aplastic anemia is idiopathic in most cases, rheumatic diseases such as systemic lupus erythematosus are recognized as causes of aplastic anemia, with their possible etiological mechanisms being T and B lymphocyte dysfunction and pro-inflammatory cytokines and autoantibody production directed against bone marrow components. In the course of the human immunodeficiency virus infection/acquired immunodeficiency syndrome, the identification of autoantibodies and the occurrence of rheumatic events, in addition to the natural course of systemic lupus erythematosus which is modified by immune changes that are characteristic of human immunodeficiency virus infection/acquired immunodeficiency syndrome, make the diagnosis of systemic lupus erythematosus challenging. This study reports the case of a woman with acquired immunodeficiency syndrome treated with a highly active antiretroviral therapy, who had prolonged cytopenias and hypocellular bone marrow consistent with aplastic anemia. The clinical picture, high autoantibodies titers, and sustained remission of the patient's hematological status through immunosuppression supported the diagnosis of systemic lupus erythematosus-associated aplastic anemia. This is the first report of aplastic anemia concurrent with systemic lupus erythematosus and acquired immunodeficiency syndrome, providing additional evidence that immune dysfunction is a key part of the pathophysiological mechanism of aplastic anemia.
Keywords: Anemia, aplastic; Lupus erythematosus, systemic; HIV infections; Pancytopenia; Autoantibodies; Acquired immunodeficiency syndrome; Humans; Female; Case reports
Introduction
Aplastic anemia (AA) is a potentially fatal bone marrow failure syndrome in which hematopoietic precursor cells are replaced by fat, resulting in pancytopenia. The estimated incidence of AA in Latin America is considered low (1.6 cases per 1,000,000 individuals per year)(1). Multiple conditions are indicated as causes; however, most cases have unexplained etiologies and are considered idiopathic.
Cases of secondary AA are commonly related to exposure to toxic substances and drugs, viral infections, radiation, pregnancy and rheumatic diseases. Systemic lupus erythematosus (SLE)-associated AA is rare, and immune dysfunction is incriminated as a potential pathophysiological mechanism. In the course of human immunodeficiency virus (HIV) infection, the identification of autoantibodies and outbreak of rheumatological manifestations following the restoration of immunocompetence by a highly active antiretroviral therapy (HAART) provide additional data that may clarify the mechanisms directly involved in the pathophysiological mechanism of SLE and AA(2,3).
This paper reports the case of a young woman with prolonged pancytopenia and acquired immunodeficiency syndrome (AIDS) without evidence of myelotoxicity related to antiretroviral therapy and the criteria for SLE evolving with excellent response to immunosuppressive therapy. After an extensive evaluation of the literature in English, we found 24 reports of an association between SLE and AA; however, the present report is the first to describe a case of SLE-associated AA in a patient with AIDS(4).
Case report
This report describes the clinical course of a 39-year-old woman who was referred to our institute for evaluation due to persistent pancytopenia with intermittent transfusion treatment (packed red blood cells and platelets). Her medical history indicated HIV infection for 15 years, regular HAART (tenofovir, lamivudine, ritonavir, and atazanavir) with good and prolonged virological control (viral load < 50 copies/mL and CD4 T-lymphocyte count of 628 cells/ µL), intermittent polyarthritis of the hands, transvaginal bleeding and bacterial pneumococcal meningitis four months earlier. There was no report of fever, rash, photosensitivity, oral or nasal ulcers, or neurological or renal disorders. Her physical examination was normal, except for pallor and petechiae in the lower limbs without adenopathy or hepatosplenomegaly.
Repeated tests performed within the previous 16 weeks showed anemia (hemoglobin level: 6.8-9.7 g/dL; mean cell volume, 90.5-110.0 fL), absolute reticulocyte count (8.7-29.1 × 109/L), leukopenia (1.71-3.49 × 109/L) with neutropenia (0.58-1.53 × 109/L), variable lymphocyte count (0.44-2.79 × 109/L) and severe thrombocytopenia (2-10 × 109/L). An extensive laboratory evaluation was conducted for vitamin B12, folate, bilirubin, lactate dehydrogenase, haptoglobin, rheumatoid factor, complement components (C3 and C4), prothrombin time, activated partial thromboplastin time, thyroid function, and renal and hepatic tests without alterations. Serologic markers for hepatitis B and C, cytomegalovirus (immunoglobulin M), and parvovirus (immunoglobulin M) were nonreactive. A direct antiglobulin test was negative. Urinary protein was 610 mg/24h. Effusions were not detected in imaging studies. A myelogram showed severe hypoplasia of the erythrocytic, granulocytic, and megakaryocytic series with the presence of 40% of typical lymphocytes and no evidence of infiltration by parasites or tumor cells. A bone marrow biopsy confirmed hypocellularity with reduced hematopoiesis (5% cellularity) and absence of reticular fibrosis or necrosis (Figures 1 and 2). Analysis of antinuclear antibodies (> 1:640, coarse speckled nuclear pattern), anti-ribonucleoprotein (1:1600) and anti-Sm (1:800) antibodies were reactive at high titers (antiScl70 and anti-native DNA did not react). In accordance with the criteria of the American College of Rheumatology for SLE and the International Agranulocytosis and Aplastic Anemia Study Group, the diagnosis of SLE-associated AA was proposed.
Figure 1.
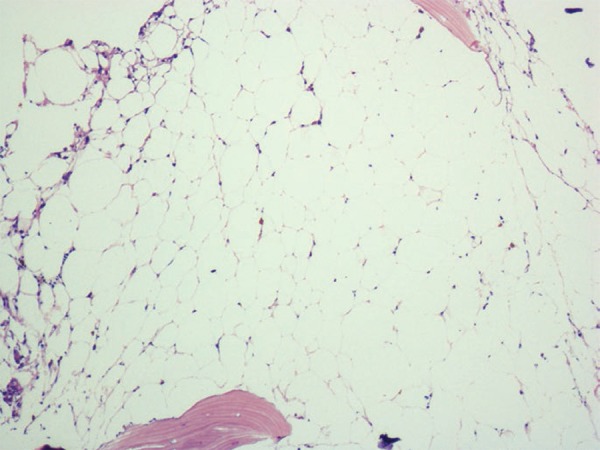
Hypocellular bone marrow marked by intense replacement of normal cellularity by adipose tissue. Maximow staining, 200 x original magnification
Figure 2.
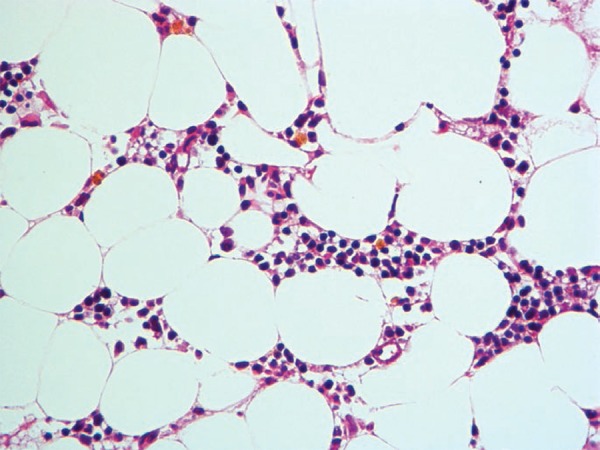
Hypocellular bone marrow with 10% hematopoietic cells, predominance of erythroid lineage cells, and abundant hemosiderin deposits (3+/4+). Hematoxylin and eosin staining, 400 x original magnification
The potential toxic effects of antiretroviral drugs as a cause of AA were tested before the start of immunosuppressive therapy through a temporary eight-week treatment interruption, but no change in the hematological picture or transfusion dependence was observed. Thus, according to the hypothesis of SLE-associated AA, immunosuppression with prednisone (1 mg/kg/day) and hydroxychloroquine (400 mg/day) was initiated with progressive and sustained improvement of the cytopenias during the following six weeks and total transfusion independence. The patient remained in follow-up with regular use of hydroxychloroquine and HAART; the CD4 count > 500 cells/µL and no cytopenias were reported after 20 months.
Discussion
SLE is a heterogeneous autoimmune disease that features variable impairment of different tissues due to the action of autoantibodies and immunocomplex deposition. Anemia, leukopenia, lymphopenia, and thrombocytopenia are the most common hematological findings and, in most cases, are derived from autoantibody-mediated peripheral destruction, inflammatory state (anemia), or drug toxicity in treatment(5,6). The association between AA and SLE is extremely rare, with 24 cases found after a thorough review of the scientific literature in English(4,6,7). This report is particularly interesting as it is the first to describe the association between AA, SLE and AIDS.
The pathophysiological mechanisms determining the suppression of normal hematopoiesis in SLE patients have not been defined, but the identified possible causes include T- and B-lymphocyte dysfunction, autoantibody production (dependent or independent of the complement system), and the action of pro-inflammatory cytokines. Their potential targets include progenitor cells and bone marrow stromal(4-9). Evidence that the bone marrow is the target organ in patients with SLE and cytopenia lies with the histological demonstration of hypocellularity, dysplastic changes, necrosis, reticular fibrosis, and vasculitis(8-10). On the other hand, the relationship between SLE and AIDS, diseases characterized by multisystem involvement and immune dysfunction related to T lymphocytes, polyclonal activation of B lymphocytes, and cytokine production alterations(11), is both unusual and intriguing. HIV infected patients have frequent rheumatological manifestations that in conjunction with a high incidence of broad-spectrum autoantibodies, make the diagnosis of SLE with concomitant HIV/AIDS a challenge(2,3,11,12). Zandman-Goddard & Shoenfeld proposed stages in the course of HIV infection for the occurrence of autoimmune manifestations in which the restoration of immunological competency (CD4 count > 500 cells/µL and low viral load) using HAART, as in our patient, allows the emergence of autoimmune diseases(2). In this report, autoantibodies at high titers and the resolution of the hematological picture upon the initiation of therapy specific for SLE (immunosuppression) supports the diagnosis of SLE.
HIV infection (direct viral action on the hematopoietic tissue) is recognized as a rare cause of AA. Drugs routinely used in the AIDS treatment are cited as a cause of cytopenias and the potential effects of these drugs as a cause of hematopoiesis suppression are difficult to document by laboratory tests; thus, no in vitro test was performed in this case(5). In the currect work, the temporary suspension of HAART for eight weeks did not alter the patient's clinical (dependence on transfusion) or laboratory course (maintenance of cytopenias), leading to exclusion of this etiology and justifying the reintroduction of treatment.
The best treatment for SLE-associated AA has yet to be defined. Immunosuppression therapy (steroids, hydroxychloroquine, cyclosporine, and cyclophosphamide), androgens, plasmapheresis, human immunoglobulin, antithymocyte globulin, and rituximab are used(4). The use of immunosuppressive drugs (hydroxychloroquine and prednisone) with improvement in hematologic parameters as reported herein constitutes strong additional evidence of immune dysfunction(5-7). In such a situation, unlike with idiopathic AA, response to the treatment modalities described previously is satisfactory and sustained(6,7).
Special attention should be given to patients with SLE and persistent cytopenias justifying a bone marrow evaluation. At the same time, the need to exclude rheumatic diseases, especially SLE, in patients with AA should be emphasized in order to recognize the reversal of the potential hematological status with the introduction of treatment. The rare association of AA, SLE, and AIDS provides additional evidence that autoantibodies and T lymphocytes play a key role in the pathophysiological mechanism of AA.
Footnotes
Conflict-of-interest disclosure: The authors declare no competing financial interest
References
- 1.Maluf E, Hamerschlak N, Cavalcanti AB, Júnior AA, Eluf-Neto J, Falcão RP, et al. Incidence and risk factors of aplastic anemia in Latin American countries: the LATIN case-control study. Haematologica. 2009;94(9):1220–1226. doi: 10.3324/haematol.2008.002642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zandman-Goddard G, Shoenfeld Y. HIV and autoimmunity. Autoimmun Rev. 2002;1(6):329–337. doi: 10.1016/s1568-9972(02)00086-1. [DOI] [PubMed] [Google Scholar]
- 3.Daikh BE, Holyst MM. Lupus-specific autoantibodies in concomitant human immunodeficiency virus and systemic lupus erythematosus: case report and literature review. Semin Arthritis Rheum. 2001;30(6):418–425. doi: 10.1053/sarh.2001.23149. [DOI] [PubMed] [Google Scholar]
- 4.Alishiri GH, Saburi A, Bayat N, Saadat AR, Saburi E. The initial presentation of systemic lupus erythematosis with aplastic anemia successfully treated with rituximab. Clin Rheumatol. 2012;31(2):381–384. doi: 10.1007/s10067-011-1878-z. [DOI] [PubMed] [Google Scholar]
- 5.Tabushi Y, Fukazawa T, Abe K, Kaneda K, Hirashima M, Young-Joon K, et al. A case of aplastic anemia in a patient with systemic lupus erythematosus. Mod Rheumatol. 2003;13(2):177–180. doi: 10.3109/s10165-002-0219-0. [DOI] [PubMed] [Google Scholar]
- 6.Tagoe C, Shah A, Yee H, Belmont HM. Aplastic anemia in systemic lupus erythematosus: a distinct presentation of acquired aplastic anemia? J Clin Rheumatol. 2001;7(6):377–383. doi: 10.1097/00124743-200112000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Jose W, Unnikrishnan A, Muthu P, Kumar K, Pavithran K. Aplastic anaemia complicating systemic lupus erythematosus (SLE) at presentation: a clinical vignette and review of the literature. J Clin Diag Res. 2011;5(3):637–639. [Google Scholar]
- 8.Voulgarelis M, Giannouli S, Tasidou A, Anagnostou D, Ziakas PD, Tzioufas AG. Bone marrow histological findings in systemic lupus erytematosus with hematologic abnormalities: a clinicopathological study. Am J Hematol. 2006;81(8):590–597. doi: 10.1002/ajh.20593. [DOI] [PubMed] [Google Scholar]
- 9.Giannouli S, Voulgarelis M, Ziakas PD, Tzioufas AG. Anaemia in systemic lupus erythematosus: from pathophysiology to clinical assessment. Ann Rheum Dis. 2006;65(2):144–148. doi: 10.1136/ard.2005.041673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pereira RM, Velloso ER, Menezes Y, Gualandro S, Vassalo J, Yoshinari NH. Bone marrow findings in systemic lupus erythematosus patients with peripheral cytopenias. Clin Rheumatol. 1998;17(3):219–222. doi: 10.1007/BF01451051. [DOI] [PubMed] [Google Scholar]
- 11.Sekigawa I, Okada M, Ogasawara H, Naito T, Kaneko H, Hishikawa T, et al. Lessons from similarities between SLE and HIV infection. J Infect. 2002;44(2):67–72. doi: 10.1053/jinf.2001.0959. [DOI] [PubMed] [Google Scholar]
- 12.Gould T, Tikly M. Systemic lupus erythematosus in a patient with human immunodeficiency virus infection - challenges in diagnosis and management. Clin Rheumatol. 2004;23(2):166–169. doi: 10.1007/s10067-003-0833-z. [DOI] [PubMed] [Google Scholar]


