Abstract
Transition from pediatric to adult care represents a high risk period for adolescents and emerging adults with diabetes. Fundamental differences between pediatric and adult care delivery models may contribute to increased risk for poor health outcomes. This review provides a brief overview of models of care in pediatric and adult settings and focuses on patient-provider communication content and quality as potential points of intervention to improve transition-related outcomes. This review also highlights disparities in transition and communication for adolescents and emerging adults from racial/ethnic minority groups and discusses recent changes in health care legislation that have significant implications for the transition process. Intervention opportunities include programs to enhance developmentally-appropriate patient-provider interactions and increased attention to promoting transition readiness skills. Improving patient-provider communication may hasten the development of vital self-advocacy skills needed in adult health care systems and, thus, help establish a lasting pattern of positive diabetes self-care.
Keywords: Diabetes, Transition, Adolescents, Young Adults, Glycemic Control, Health Care Delivery, Patient-Provider Communication, Racial/Ethnic Minority Groups, Health Insurance
Introduction
Late adolescence and emerging adulthood is a challenging time for diabetes management [1, 2]. The unique developmental stage between late adolescence and adulthood, also known as emerging adulthood, covers the period between ages 18–30 when youth begin to take primary responsibility for key tasks associated with adulthood [3]. In parallel with transition from pediatric to adult health care, emerging adults with diabetes also must assume increasingly independent responsibility for disease management. Transition is a life course issue and successful “transition” cannot be achieved entirely in the pediatric setting. The skills that emerging adults develop related to successful navigation of and engagement with the adult care setting are critical to the maintenance of lifelong patterns of disease management [4, 5].
Research is beginning to identify salient factors that contribute to seamless transition from pediatric to adult medical care and successful assumption of independent responsibility for disease care [1, 6]. Both processes require changes in the relationship between the patient and the health care provider. Moreover, pediatric and adult medical care systems place different demands and expectations on patients. This review will first provide an overview of issues associated with the transition to adult care and how systems level differences between pediatric and adult care influence the transition process and related outcomes in patients with type 1 diabetes. It will also highlight racial/ethnic disparities observed during the transition process. The review will then focus on the relationship between emerging adult patients and providers and the role of patient-provider communication as a potential, yet relatively unexplored, mechanism for promoting optimal diabetes care processes and reducing health disparities. Implications for intervention will be discussed.
Transition to Adult Medical Care
Garvey and colleagues recently detailed relevant research on the transition to adult diabetes care [1]. As reviewed by Garvey [1], studies have demonstrated that emerging adults with type 1 diabetes are at risk for gaps in medical care, premature mortality and morbidity, and poor health outcomes during and after the transition from pediatric to adult health care [7, 8]. Few emerging adults meet the American Diabetes Association recommendation for glycemic control for adults (A1c<7.0%) [9]. Further, data indicate that those from racial/ethnic minority groups tend to have longer gaps in treatment when transferring from pediatric and adult diabetes care and demonstrate poorer diabetes management and glycemic control both prior to and after entrance into adult care, suggesting increased risk for this group during a vulnerable developmental period [10, 11].
Differences in the Pediatric and Adult Care Systems
A myriad of factors likely contribute to poor health outcomes and gaps in care related to the transition to adult medical care. Patients perceive fundamental differences between pediatric and adult care health systems and emerging adults may not be fully prepared to meet the demands of adult care [12, 13]. The pediatric care system is highly standardized, with access to a multidisciplinary team and a family-based approach to care [7]. In pediatric care, youth typically have a long-standing, comfortable relationship with one diabetes care provider who is knowledgeable about their unique disease and personal/social history [2]. However, qualitative studies suggest that pediatric providers may not shift their consultation style to match the developmental needs of adolescent and emerging adult patients, often leading older youth to feel uncomfortable in the pediatric setting [12]. In contrast, the adult care setting often has discontinuity among health care providers, and patients may see a different provider at each visit [12]. Clinic visits are shorter and tend to focus on strict glycemic control and risk for long-term complications rather than addressing psychosocial concerns or issues related to diet and physical activity [2, 14, 15]. Emerging adults are also less likely to receive all recommended medical tests at clinic visits as compared to adolescent patients. Only 55% of emerging adults with type 1 diabetes report having A1c levels measured at each clinic visit as compared to 73% of adolescents ages 12–17 [16]. Patients may not feel fully informed about this systematic shift in treatment practices when moving from pediatric to adult medical care [17].
Timing of Transition to Adult Care
Anecdotal evidence suggests pediatric patients who are doing poorly may be transferred to adult care earlier than their adherent peers [10]. Physicians also may transfer pediatric patients who are experiencing “adult” problems – such as pregnancy or substance use – to an adult care setting in an attempt to best meet the patient’s needs. Pediatric physicians may perceive that they lack the expertise to address “adult” issues in a pediatric setting [18].
Recent studies suggest that transitioning to adult care too early may be detrimental. The SEARCH for Diabetes in Youth study group examined transition from pediatric to adult care for 185 emerging adults diagnosed with type 1 diabetes during adolescence. Results showed that the odds of having poor glycemic control were 2.46 times higher for those who had transitioned adult care as compared to those who remained in pediatric care [19]. Helgeson and colleagues found that early age at transition, particularly transition prior to high school graduation, was associated with poor post-transition health outcomes such as higher A1c levels and poorer self-care skills [10]. Similarly, Nakhla and colleagues reviewed medical records of 1507 emerging adults with diabetes in Ontario and found that transfer to a new physician in adult medical care was associated with a 77% increase in risk for hospitalization after transition as compared to those who remained with the same physician [20]. Further, clinic attendance significantly decreases during the move from pediatric to adult care, and studies suggest that more than 25% of emerging adults with diabetes report a 6 month gap or greater in medical care after transfer to an adult care provider [7, 8, 21].
Emerging adults from racial/ethnic minority groups are at risk for earlier transition to the adult care setting and poorer health outcomes in adult care. In the SEARCH study, African American and Hispanic emerging adults with type 1 diabetes transitioned to adult care at an earlier age than non-Hispanic whites [19]. Further, Helgeson and colleagues found that early transition had a more detrimental effect on emerging adults from racial/ethnic minority groups, with nonwhite participants experiencing 3.44 times higher odds of having poor glycemic control at follow-up in adult care compared to non-Hispanic white participants, even after controlling for socioeconomic status and baseline A1c [10]. Differences in treatment in the pediatric setting may also contribute to poor transition outcomes. For example, use of intensive insulin regimens has been associated with better glycemic control [22]. Yet, youth from racial/ethnic minority groups are less likely to be prescribed more intensive insulin regimens than non-Hispanic white youth [23, 24]. In summary, both the act and the timing of transfer to adult care contribute to poor health outcomes in emerging adults with diabetes, and effects are more pronounced among those from racial/ethnic minority groups.
Health Insurance Status and Transition to Adult Care
Financial barriers, including lack of health insurance and cost of medical care, contribute to difficulties with transition to adult medical care [25]. Changing health insurance, particularly for individuals from racial/ethnic minority groups or those on public insurance, may hasten transfer and contribute to gaps in medical care [26]. Emerging adults, including those with chronic illnesses like diabetes, are less likely to have health insurance than any other age group [27, 28]. In 2011, 25.9% of all 18–24 year olds were uninsured [29].
Insufficient health insurance coverage impacts health care utilization in emerging adults. In 2009, individuals ages 18–26 had the lowest health care utilization rates of any age group, and a significant percentage delayed accessing health care due to cost [30]. Moreover, substantial racial/ethnic disparities exist in access to care. Hispanic emerging adults are significantly less likely to report a doctor’s visit within the past 12 months as compared to non-Hispanic white and African American emerging adults [31]. African American emerging adults are also significantly more likely to report an emergency department visit within the past 12 months [31].
Recent health care reform has opened doors to affordable insurance coverage for emerging adults. Starting in 2010, the Patient Protection and Affordable Care Act (PPACA) extended the age that youth can remain on a parent’s insurance plan and mandated that all insurance plans maintain dependent insurance coverage until age 26 [32]. This provision led to increased insurance coverage for approximately 3 million emerging adults from 2010 to 2011 [33]. In 2014, the PPACA will expand Medicaid coverage for all adults with incomes ≤133% of the federal poverty level, including those with special health care needs or who are unable to remain on a parent’s insurance plan. Additionally, individuals with annual incomes ≤400% of the federal poverty level will be eligible to purchase private health insurance plans through state insurance exchanges. Income-based subsidies will offset costs of health insurance purchased through state insurance exchanges [34].
The impact of health reform on the transition to adult care is yet unknown. However, current and future PPACA provisions provide vastly increased options for emerging adults with diabetes to obtain private or public insurance coverage. The systemic challenges in preparing emerging adults for adult care and ensuring seamless transfer between pediatric and adult medical care may be more apparent as the barrier of insurance coverage is removed and greater potential for engagement with the health care system exists. Thus, it is exceedingly important to examine key points of intervention in pediatric and adult medical care that may improve the transition process for all patients with diabetes, including those from racial/ethnic minority groups. Patient-provider communication related to transition from pediatric to adult care settings may be an effective point of intervention in the health care system.
Patient-Provider Communication
Patient-provider communication represents a complex dyadic interaction (Table 1). This component of high-quality health care appears to play a salient role in readying adolescents and emerging adults for adult care. Few studies have evaluated the relationship with the physician as a critical element of transition readiness, particularly the quality and content of information communicated during the transition process. However, research with individuals with chronic illness has demonstrated that patient-provider communication interactions contribute to health care satisfaction, adherence, and experience of acute and chronic health complications [35, 36].
Table 1.
Health care provider and patient behaviors to facilitate communication
| Domain | Health Care Provider Behaviors | Adolescent and Emerging Adult Patient Behaviors |
|---|---|---|
| Questions and information-sharing |
|
|
| Tone and affect |
|
|
| Autonomy-promotion |
|
|
| Problem-solving |
|
|
| Preparation prior to visit |
|
|
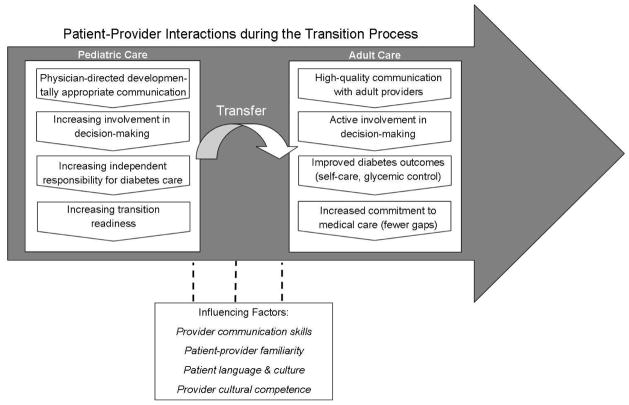
Health care providers are integral in helping youth develop skills necessary for communication with other – including future – providers about their medical condition and needs [37]. Poor health outcomes may be due to difficulty adhering to provider recommendations or poor understanding of the health treatment plan. Lack of patient-reported trust in providers is also a salient barrier to effective communication in pediatric and adult care, particularly for patients from ethnic/racial minority groups [38–40]. Pediatric providers are in a unique position to shape their adolescent and emerging adult patients’ health communication skills by directing questions to the young person, involving them in medical decision making, encouraging increasing responsibility for diabetes care, and preparing patients and their families for the transfer to adult medical care. Such high quality communication may lead to greater involvement in, motivation for, and satisfaction with pediatric and adult health care, which directly influences self-care and more distal health outcomes across the transition to adult medical care (Figure 1) [36]. Evaluation of communication surrounding the transition from pediatric to adult medical care is particularly important to help emerging adults prepare for changing demands and expectations across health care systems.
Figure 1.
Patient-provider interactions during the transition process. High-quality, developmentally appropriate communication with a health care provider plays a key role in preparation for transition to adult medical care. Support for decision making, independent responsibility, and transition readiness in pediatric care may contribute to improved health outcomes and increased engagement in adult medical care.
Adolescent and Emerging Adult Communication with Health Care Providers
Adolescents and emerging adults have the potential to be more engaged in medical care when physicians direct medical information toward them and include them in developmentally-appropriate decision making related to transition to adult care [21, 41, 42]. Little research has examined patient-provider communication interactions during adolescence, and even fewer studies have addressed this issue among emerging adults. Qualitative studies with adolescents suggest that prevailing health care communication patterns may not promote readiness for independent disease management [39]. In a study by Sonneveld and colleagues, adolescents with juvenile rheumatoid arthritis, neuromuscular disorder with chronic ventilation, or type 1 diabetes reported that pediatric providers offered few opportunities to make their own decisions or be seen without parents present. Additionally, adolescents’ ratings of providers’ communication skills were lower than their parents’ ratings of the providers in a number of areas, including listening skills, honesty, and demonstrating understanding [43]. Parents and adolescents both agreed that communication related to the transition process could be improved [43]. Unfamiliarity with a health care provider also has been noted as a significant barrier to communication [44]. On the adult side of care, emerging adults frequently raise concerns about lack of coordination of care and feeling “lost” after transfer, suggesting difficulty establishing relationships with adult care providers [45, 46].
Adolescents and emerging adults desire the opportunity to be the main partner in health-related communication [47], yet there are a number of barriers to optimal patient-provider communication. Adolescents’ verbal contributions to clinic visits may be limited by parent and physician turn-taking and lack of questions directed to adolescents [48–50]. The presence of more adult participants in a medical encounter (e.g. medical residents) further limits an adolescent’s communication with a health care provider [49]. Many adolescents report that they lack the skills necessary to communicate with health care providers, including how to raise sensitive issues [51]. For example, some adolescents report difficulty disclosing information related to risky behaviors or poor medical regimen adherence, suggesting a level of discomfort that may interfere with communication about important health topics [51, 52]. Many of these studies have utilized retrospective self-report measures to evaluate communication styles. There is a significant need for observational and mixed-methods research to evaluate the content and quality of adolescent and emerging adult communication with health care providers and satisfaction with health communication prior to and after the transition to adult medical care [47].
Patient-Provider Communication and Adherence
Research has consistently demonstrated that, across all ages and disease groups, poor patient-provider communication is associated with a higher risk of nonadherence [53]. As hypothesized in our model of patient-provider communication (Fig. 1), high-quality communication in pediatric and adult care settings has the potential to positively influence diabetes self-care and medical regimen adherence. Table 1 summarizes key behaviors by both health care providers and adolescent and emerging adult patients that contribute to high quality dyadic communication.
A recent meta-analysis reviewed 106 correlational studies and 21 interventions and found a 19% higher risk of non-adherence related to poor physician communication. The relationship between communication and adherence was even stronger when the physician was a pediatrician, suggesting that high-quality, developmentally appropriate health communication during adolescence and emerging adulthood is critical to promote optimal adherence [53]. In adults with diabetes, high-quality general and diabetes-specific communication is associated with 10–30% better adherence to medication, dietary, and exercise regimens [54]. Patients who rate their provider high in communication domains also report better diabetes self-management. Patient-provider communication quality accounts for 21% of the variance in diabetes self-care, including adherence to medication taking, blood glucose monitoring, and diet recommendations [55]. Thus, improving the quality of patient-provider communication surrounding the transition to adult care during adolescence may ultimately lead to better adherence and improved health outcomes in emerging adults with diabetes.
Communication is not one-sided and relatively few studies have examined patient contribution to health care interactions [56, 57]. Among adults with diabetes, increased patient participation, disclosure, and positive affect leads to improved self-care and better health outcomes [35, 55]. One study found that adult patients initiate 84% of active participation behaviors in medical visits and, in turn, greater patient participation elicits higher quality communication from the provider [57]. Interventions designed to enhance patient communication have positively impacted communication competence, increasing patient involvement in medical visits, question asking, and disclosure of detailed information [58–60]. To date, little is known about patient driven communication behaviors in emerging adulthood and these interventions have not been evaluated in emerging adults with diabetes.
Patient-Provider Communication as a Transition Skill
Effective communication with health care providers is a critical component of independent self-care skills in emerging adults [61]. However, research often demonstrates that emerging adults and health care providers face barriers and struggle to communicate effectively with one another regarding transition. Garvey and colleagues evaluated transition preparation in a sample of 258 emerging adults with type 1 diabetes and found that less than 15% reported having a transition preparation visit or receiving transition-specific resources from their health care provider. Greater perception of transition readiness was associated with less likelihood for gaps in treatment when transitioning to adult care, highlighting the importance of physician communication about transition tasks [21].
Evidence from other chronic illness populations further supports that neither adolescents nor emerging adults receive adequate information and support from health care providers regarding transition issues [62, 63]. In 2005, the multisite National Survey of Children with Special Health Care Needs evaluated transition care in 18,198 adolescents (ages 12–17). Results indicated that only 42% of adolescents with special health care needs received transition counseling and 34% discussed health insurance changes associated with adult status [63]. African American and Hispanic adolescents with special health care needs were less likely to receive transition counseling than non-Hispanic white adolescents, possibly contributing to racial/ethnic disparities in post-transition outcomes [11]. Sawicki and colleagues analyzed data from the 2007 Survey of Adult Transition and Health (n = 1865; ages 19–23) and found that only 55% of emerging adults reported discussing developmental changes in health care needs and transition to adult care with a health care provider. Higher self-reported quality of patient-provider communication was associated with more frequent guidance on issues related to transition [41]. Further, van Staa and colleagues surveyed 954 adolescents (ages 12–19) with chronic illness and found that frequency of transition discussions during consultations was a more powerful predictor of readiness for adult medical care than age. Greater self-reported independence during medical visits was also strongly associated with transition readiness [42].
Communication and Racial/Ethnic Minority Groups
Research in chronic illness populations suggests that racial/ethnic group status may influence communication, and youth from minority groups are at risk for poor communication with health care providers [64–66]. Stivers and Majid found that providers were less likely to direct questions to African American and Hispanic youth as compared to non-Hispanic white youth [66]. A large study on African American adults with hypertension found that 51% of participants rated their provider’s communication as non-collaborative, which was particularly concerning because perception of more collaborative communication with the provider was associated with better medication adherence [67]. African American adults with diabetes prefer to play an active role in decision making related to medical care, yet are not consistently included as partners in medical decisions [68]. Although this has not been evaluated in emerging adults with diabetes, there is evidence to suggest that cultural differences in patient preferences may influence patient-provider communication and have implications for long-term health outcomes.
Language is also a salient factor in patient-provider communication. Differences in cultural communication styles, including tone, eye contact, questioning of doctors in positions of authority, and multi-generational roles, present additional challenges when communicating with racial/ethnic minority patients [69]. Language translators may be required for medical visits when the health care provider does not speak the same language as the patient and/or family. Translator services may be formal (e.g. a translator employed by a medical setting) or informal (e.g. a family member translating for another family member). Use of translators may affect rapport, as patients may feel more comfortable communicating with the translators than speaking directly to the health care provider. Translators may also paraphrase or omit content, and some phrases used by health care providers may not have direct translations in the patient’s language of origin [70]. Research with adults with diabetes has found that language barriers contribute to health disparities among Hispanic patients. Hispanic patients with language-discordant physicians have significantly poorer glycemic control as compared to language-concordant physician relationships [71]. It is recommended that physicians communicate with hospital-based translators prior to a medical visit to review key terminology and concepts that will be discussed, including topics related to transition to adult medical care.
Implications for Intervention
The aforementioned challenges related to transition to adult care and patient-provider communication have significant implications for intervention. There is much work to be done in pediatric practices prior to transferring a patient to adult medical care, and providers should be aware of potential disparities in care for adolescents and emerging adults from racial/ethnic minority groups. Synthesis of the literature suggests that changes to the care delivery model may move towards offering targeted emerging adult clinics or increased opportunity to meet with adult care providers prior to the transfer [5, 72]. However, little focus has been given to how the transfer is managed by adult providers including whether they make accommodations for new transfers such as a longer first visit or provision of new patient orientation materials. The patient-provider relationship may also be a powerful mechanism to promote successful health outcomes after transition. Teaching patients and providers skills to enhance communication in pediatric and adult care settings offers another potential avenue for intervention. Both adolescent and emerging adult patients may benefit from explicit instruction in how to effectively ask questions, disclose concerns, and effectively participate in collaborative problem solving. In addition, improving providers’ communication skills related to discussing what to expect during transition can enhance transition readiness and lead to fewer gaps in medical care.
Developmentally appropriate care for adolescents and emerging adults should include opportunities to meet alone with pediatric providers [2, 51]. The confidence and comfort to raise questions about difficult issues, including risk behaviors and behaviors related to non-adherence, develop over time and the opportunity to be seen without a parent for part of the visit should start in early adolescence. Increased patient participation and disclosure leads to improved self-care and better health outcomes in adults with chronic illness [35, 73, 74], suggesting that the benefits of engaging adolescent and emerging adult patients may extend well into adulthood. Further, little is known about relationships with health care providers in the adult care setting. Adult endocrinologists may benefit from increased training in addressing emerging adult issues and fostering effective, high-quality communication skills in emerging adult patients with diabetes.
Most research on diabetes care in adolescents and emerging adults has focused on the non-Hispanic white racial/ethnic group. As highlighted in this review, patients with diabetes from other racial/ethnic groups have unique challenges related to glycemic control during the transition to adult medical care, communication with health care providers, and access to medical care. Future research should target key, modifiable factors that influence health care quality and health outcomes in adolescents and emerging adults with diabetes from racial/ethnic minority groups. The patient-provider relationship represents one potentially modifiable factor to improve outcomes [71]. Language barriers are especially important to address, as language barriers have been associated with decreased satisfaction with care and decreased use of health care services, even among insured patients [71]. Through culturally-sensitive, developmentally-appropriate care, we may best prepare emerging adults from racial/ethnic minority groups for entrance into the adult health care system. Providers may benefit from training related to cultural competence and communication skills related to adolescent and emerging adult patients. We are entering an exciting new frontier of health care utilization and improved access as health care legislation expands access to health insurance for all emerging adults. Developing, validating, and translating evidence-based interventions to increase preparation for adult medical care is needed. Such interventions should be evaluated in adolescents and emerging adults from racial/ethnic minority groups to determine any adjustments necessary for timing, treatment targets, and preferred language.
Conclusion
The process of transition from pediatric to adult medical care is a vulnerable period for emerging adults with diabetes. Effective communication with health care providers is a key component of independent self-care skills, and the quality of communication between young patients and their health care providers may contribute to successful transition to adult diabetes care [44]. As highlighted in this review, research suggests that both transfer itself as well as timing of transfer to adult care influences diabetes-related health outcomes. Difficulties maintaining health insurance coverage during emerging adulthood also may contribute to decreased access to medical care. More frequent communication about transition-related issues promotes emerging adults’ perceived readiness for adult care and reduces treatment gaps. Thus, enhancing the quality of patient-provider communication in adolescent and emerging adult medical encounters is a potential intervention target to smooth transition to adult care and improve health outcomes in youth with diabetes. Additionally, the potential for racial/ethnic disparities exists at the provider, health system, and health policy levels. Efforts should be made to improve patient-provider communication as well as to eliminate health disparities that make the transition process more difficult for patients from racial/ethnic minority groups. Increased attention to the transition from pediatric to adult care in both research and clinical practice can ultimately improve health outcomes for individuals with diabetes.
Acknowledgments
Maureen Monaghan has received grant support from a KL2 Career Development Award from the Clinical and Translational Science Institute - Children’s National (KL2TR000076).
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest
Maureen Monaghan, Marisa Hilliard, Rachel Sweenie, Kristin Riekert declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Maureen Monaghan, Email: mmonagha@childrensnational.org, Center for Translational Science, Children’s National Medical Center, 111 Michigan Ave NW, Washington, DC 20010, (202) 476-4726 (phone); (202) 476-3966 (fax).
Marisa Hilliard, Email: marisa.hilliard@jhmi.edu, Johns Hopkins Adherence Research Center, Johns Hopkins Medical Center, 5501 Hopkins Bayview Circle, Baltimore, MD 21224, (401) 550-6083 (phone); (410) 550-2612 (fax).
Rachel Sweenie, Email: rsweenie@childrensnational.org, Center for Translational Science, Children’s National Medical Center, 111 Michigan Ave NW, Washington, DC 20010, (202) 476-3328 (phone); (202) 476-3966 (fax).
Kristin Riekert, Email: kriekert@jhmi.edu, Johns Hopkins Adherence Research Center, Johns Hopkins Medical Center, 5501 Hopkins Bayview Circle, Baltimore, MD 21224, (410) 550-7755 (phone); (410) 550-2612 (fax).
References
Papers of particular interest, published recently, have been highlighted as:
*Of importance
**Of major importance
- 1**.Garvey KC, Markowitz JT, Laffell LMB. Transition to adult care for youth with type 1 diabetes. Curr Diab Rep. 2012;12:533–541. doi: 10.1007/s11892-012-0311-6. This review paper discusses the rationale for transition research by identifying unique challenges of emerging adulthood, providing recommendations for transition services, and specifying how transition is particularly challenging for emerging adults with type 1 diabetes. It reviews both observational and interventional studies evaluating transition to adult diabetes care and stresses the need for further research through randomized controlled trials. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peters A, Laffel L American Diabetes Association Transitions Working Group. Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems. Diabetes Care. 2011;34:2477–2485. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arnett J. Emerging adulthood: a theory of development from late teens through the twenties. Am Psychol. 2000;55:469–480. [PubMed] [Google Scholar]
- 4.Luyckx K, Seiffge-Krenke I. Continuity and change in glycemic control trajectories from adolescence to emerging adulthood: relationships with family climate and self-concept in type 1 diabetes. Diabetes Care. 2009;32:797–801. doi: 10.2337/dc08-1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weissberg-Benchell J, Wolpert H, Anderson B. Transitioning from pediatric to adult care: a new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care. 2007;30:2441–2446. doi: 10.2337/dc07-1249. [DOI] [PubMed] [Google Scholar]
- 6.Viner RM. Transition of care from paediatric to adult services: One part of improved health services for adolescents. Arch Dis Child. 2008;93:160–163. doi: 10.1136/adc.2006.103721. [DOI] [PubMed] [Google Scholar]
- 7.Pacaud D, Yale J, Stephure D, et al. Problems in transition from pediatric care to adult diabetes care for individuals with diabetes. Can J Diabetes. 2005;29:13–18. [Google Scholar]
- 8.Van Walleghem N, MacDonald CA, Dean HJ. Evaluation of a Systems Navigator Model for Transition From Pediatric to Adult Care for Young Adults With Type 1 Diabetes. Diabetes Care. 2008;31:1529–1530. doi: 10.2337/dc07-2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Petitti DB, Klingensmith GJ, Bell RA, et al. Glycemic control in youth with diabetes: The SEARCH for diabetes in Youth Study. J Pediatr. 2009;155:668–672. doi: 10.1016/j.jpeds.2009.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10**.Helgeson VS, Reynolds KA, Snyder PR, et al. Characterizing the transition from paediatric to adult care among emerging adults with type 1 diabetes. Diabet Med. 2013;30:610–615. doi: 10.1111/dme.12067. This is an innovative prospective study of youth with type 1 diabetes in various stages of the transition from pediatric to adult care. Findings highlight that youth who remained in pediatric diabetes care demonstrated better self-care and did not experience a deterioration in glycemic control as compared to youth who transitioned to adult diabetes care. Moreover, early transition was associated with worse self-care and glycemic control, and minority patients were more likely to transition early. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lotstein D, Kuo A, Strickland B, Tait F. The transition to adult health care for youth with speical health care needs: do racial and ethnic disparities exist? Pediatr. 2010;126:S129–S136. doi: 10.1542/peds.2010-1466F. [DOI] [PubMed] [Google Scholar]
- 12.Dovey-Pearce G, Hurrell R, May C, et al. Young adults’ (16–25 years) suggestions for providing developmentally appropriate diabetes services: a qualitative study. Health Soc Care Community. 2005;13:409–419. doi: 10.1111/j.1365-2524.2005.00577.x. [DOI] [PubMed] [Google Scholar]
- 13.Eiser C, Flynn M, Green E, et al. Coming of age with diabetes: patients’ views of a clinic for under-25 year olds. Diabet Med. 1993;10:285–289. doi: 10.1111/j.1464-5491.1993.tb00061.x. [DOI] [PubMed] [Google Scholar]
- 14.Geddes J, McGeough E, Frier B. Young adults with type 1 diabetes in tertiary education: do students receive adequate specialist care? Diabet Med. 2005;23:1155–1157. doi: 10.1111/j.1464-5491.2006.01933.x. [DOI] [PubMed] [Google Scholar]
- 15.Visentin K, Koch T, Kralik D. Adolescents with type 1 diabetes: transition between diabetes services. J Clin Nurs. 2006;15:761–769. doi: 10.1111/j.1365-2702.2006.01347.x. [DOI] [PubMed] [Google Scholar]
- 16.Waitzfelder B, Pihoker C, Klingensmith G, et al. Adherence to guidelines for youth with diabetes mellitus. Pediatr. 2011;128:531–538. doi: 10.1542/peds.2010-3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Busse F, Hiermann P, Galler A, et al. Evaluation of patients’ opinion and metabolic control after tranfer of young adults with type 1 diabetes from a pediatric diabetes clinic to adult care. Horm Res. 2007;67:132–138. doi: 10.1159/000096583. [DOI] [PubMed] [Google Scholar]
- 18.Reiss J, Gibson R. Health care transition: destinations unknown. Pediatr. 2002;110:1307–1314. [PubMed] [Google Scholar]
- 19.Lotstein D, Seid M, Klingensmith G, et al. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatr. 2013;131:e1062–e1070. doi: 10.1542/peds.2012-1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakhla M, Daneman D, To T, et al. Transition to adult care for youths with diabetes mellitus: findings from a universal health care system. Pediatr. 2009;124:e1134–e1141. doi: 10.1542/peds.2009-0041. [DOI] [PubMed] [Google Scholar]
- 21.Garvey KC, Wolpert HA, Rhodes ET, et al. Health care transition in patients with type 1 diabetes: young adult experiences and relationship to glycemic control. Diabetes Care. 2012;35:1716–1722. doi: 10.2337/dc11-2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Eng J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 23.Pihoker C, Badaru A, Anderson A, et al. Insulin regimens and clinical outcomes in a type 1 diabetes cohort. Diabetes Care. 2013;36:27–33. doi: 10.2337/dc12-0720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paris C, Imperatore G, Klingensmith G, et al. Predictors of insulin regimens and impact on outcomes in youth with type 1 diabetes: the SEARCH for Diabetes in Youth Study. J Pediatr. 2009;155:183–189. doi: 10.1016/j.jpeds.2009.01.063. [DOI] [PubMed] [Google Scholar]
- 25.Pai ALH, Ostendorf HM. Treatment adherence in adolescents and young adults affected by chronic illness during the health care transition from pediatric to adult health care: a literature review. Child Health Care. 2011;40(1):16–33. [Google Scholar]
- 26.Willoughby L, Fukami S, Bunnapradist S, et al. Health insurance consideratins for adolescent transplant recipients as they transition to adulthood. Pediatr Transplantat. 2007;11:127–131. doi: 10.1111/j.1399-3046.2006.00639.x. [DOI] [PubMed] [Google Scholar]
- 27.Callahan S, Cooper W. Continuity of health insurance coverage among young adults with disabilities. Pediatrics. 2007;119(6):1175–1180. doi: 10.1542/peds.2006-1881. [DOI] [PubMed] [Google Scholar]
- 28.Okumura M, Hersh A, Hilton J, Lotstein D. Change in health status and access to care in young adults with special health care needs: results from the 2007 National Survey of Adult Transition and Health. J Adolesc Health. 2013;52:413–418. doi: 10.1016/j.jadohealth.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 29.Cohen R, Martinez M. Health insurance coverage: early release of estimates from the National Health Interview Survey, 2011. Atlanta, GA: Centers for Disease Control and Prevention; 2012. pp. 1–37. [Google Scholar]
- 30.Lau J, Adams S, Irwin C. Young adult health care utilization and expenditures before the implementation of the Affordable Care Act. J Adolesc Health; Society for Adolescent Health and Medicine 2013 Annual Meeting; Atlanta, GA. 2013. p. S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kirzinger W, Cohen R, Gindi R. Health care access and utilization among young adults aged 19–25: early release of estimates from the national health interview survey, January – September 2011. Atlanta, GA: Centers for Disease Control and Prevention; 2012. pp. 1–10. [Google Scholar]
- 32*.Collins S, Robertson R, Garber T, Doty M. Tracking Trends in Health System Performance. New York: The Commonwealth Fund; 2012. Young, uninsured, and in debt: why young adults lack health insurance and how the Affordable Care Act is helping; pp. 1–23. This brief is the results of a survey of emerging adults (ages 19–25) between November 2010 and November 2011. The survey found that almost 40% of emerging adults did not have health insurance for all or part of 2011, and many emerging adults did not seek healthcare when needed due to cost as well as reported difficulty paying medical bills or medical debt. The Affordable Care Act helped many emerging adults by allowing them to stay on parents’ health plans, and these survey findings indicated the need for policymakers to enact the additional coverage expansions outlines in the Affordable Care Act. [PubMed] [Google Scholar]
- 33.Sommers B, Buchmueller T, Decker S, Carey C, Kronick R. The Affordable Care Act has led to significant gains in health insurance and access to care for young adults. Health Aff. 2013;32:165–174. doi: 10.1377/hlthaff.2012.0552. [DOI] [PubMed] [Google Scholar]
- 34.Collins S, Garber T, Robertson R. Realizing health reform’s potential: how the affordable care act is helping young adults stay covered. New York: The Commonwealth Fund; 2011. pp. 1–26. [PubMed] [Google Scholar]
- 35.van Dam HA, van der Horst F, van den Borne B, et al. Provider-patient interaction in diabetes care: effects on patient self-care and outcomes. A systematic review. Patient Educ Couns. 2003;51:17–28. doi: 10.1016/s0738-3991(02)00122-2. [DOI] [PubMed] [Google Scholar]
- 36.Street RLJ, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74:295–301. doi: 10.1016/j.pec.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 37.Geenen SJ, Powers LE, Sells W. Understanding the role of health care providers during the transition of adolescents with disabilities and special health care needs. J Adolesc Health. 2003;32:225–233. doi: 10.1016/s1054-139x(02)00396-8. [DOI] [PubMed] [Google Scholar]
- 38.DiMatteo MR. The role of effective communication with children and their families in fostering adherence to pediatric regimens. Patient Educ Couns. 2004;55:339–344. doi: 10.1016/j.pec.2003.04.003. [DOI] [PubMed] [Google Scholar]
- 39.van Staa A, Jedeloo S, van der Stege H On Your Own Feet Research Group. “What we want”: Chronically ill adolescents’ preferences and priorities for improving health care. Patient Prefer Adherence. 2011;5:291–305. doi: 10.2147/PPA.S17184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Armstrong K, Ravenell K, McMurphy S, Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Public Health. 2007;97:1283–1289. doi: 10.2105/AJPH.2005.080762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sawicki GS, Whitworth R, Gunn L, et al. Receipt of health care transition counseling in the national survey of adult transition and health. Pediatr. 2011;128:e521–529. doi: 10.1542/peds.2010-3017. [DOI] [PubMed] [Google Scholar]
- 42.van Staa A, van der Stege H, Jedeloo S, et al. Readiness to transfer to adult care of adolescents with chronic conditions: exploration of associated factors. J Adolesc Health. 2011;48:295–302. doi: 10.1016/j.jadohealth.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 43.Sonneveld HM, Strating MM, van Staa A, Nieboer AP. Gaps in transitional care: what are the perceptions of adolescents, parents and providers? Child Care Health Dev. 2013;39:69–80. doi: 10.1111/j.1365-2214.2011.01354.x. [DOI] [PubMed] [Google Scholar]
- 44.Nobile C, Drotar D. Research on the quality of parent-provider communication in pediatric care: implications and recommendations. J Dev Behav Pediatr. 2003;24:279–290. doi: 10.1097/00004703-200308000-00010. [DOI] [PubMed] [Google Scholar]
- 45.Perry L, Lowe J, Steinbeck K, Dunbabin J. Services doing the best they can: service experiences of young adults with type 1 diabetes mellitus in rural Australia. J Clin Nurs. 2012;21:1955–1963. doi: 10.1111/j.1365-2702.2011.04012.x. [DOI] [PubMed] [Google Scholar]
- 46.van Staa A, Jedeloo S, van Meeteren J, Latour J. Crossing the transition chasm: experiences and recommendations for improving transitional care of young adults, parents, and providers. Child Care Health Dev. 2011;37:821–832. doi: 10.1111/j.1365-2214.2011.01261.x. [DOI] [PubMed] [Google Scholar]
- 47**.van Staa A On Your Own Feet Research Group. Unraveling triadic communication in hospital consultations with adolescents with chronic conditions: the added value of mixed methods research. Patient Educ Couns. 2011;82:455–464. doi: 10.1016/j.pec.2010.12.001. This study was conducted with adolescents with various chronic illnesses (ages 12–19), parents, and providers using mixed-methodology. It highlights discrepancies in communication and communication styles between adolescents, parents, and providers. Specifically, although adolescents had varying preferences regarding health communication, in general all wanted to be involved as partners in their own care. However, they often behaved more as spectators and were non-compliant and/or uninvolved. Parents took dominant roles in medical encounters and providers were often frustrated by perceived adolescent ambivalence. Authors suggest that providers should encourage adolescents to take a more active role in their own care. [DOI] [PubMed] [Google Scholar]
- 48.Martenson EK, Fagerskiold AM. Information exchange in paediatric settings: An observational study. Paediatr Nurs. 2007;19:40–43. doi: 10.7748/paed2007.09.19.7.40.c4458. [DOI] [PubMed] [Google Scholar]
- 49.Pyorala E. The participation roles of children and adolescents in the dietary counseling of diabetics. Patient Educ Couns. 2004;55:385–395. doi: 10.1016/j.pec.2003.04.008. [DOI] [PubMed] [Google Scholar]
- 50.Tates K, Meeuwesen L. Doctor-parent-child communication. A (re)view of the literature. Soc Sci Med. 2001;52:839–851. doi: 10.1016/s0277-9536(00)00193-3. [DOI] [PubMed] [Google Scholar]
- 51.Beresford BA, Sloper P. Chronically ill adolescents’ experiences of communicating with doctors: a qualitative study. J Adolesc Health. 2003;33:172–179. doi: 10.1016/s1054-139x(03)00047-8. [DOI] [PubMed] [Google Scholar]
- 52.Klein JD, Wilson KM. Delivering quality care: adolescents’ discussion of health risks with their providers. J Adolesc Health. 2002;30:190–195. doi: 10.1016/s1054-139x(01)00342-1. [DOI] [PubMed] [Google Scholar]
- 53**.Zolnierek KB, DiMatteo MR. Physician communication and patient adherence: a meta-analysis. Med Care. 2009;47:826–834. doi: 10.1097/MLR.0b013e31819a5acc. This is a meta-analysis of 106 correlational and 21 experimental intervention studies linking patient adherence to patient-provider communication. Results demonstrate that physician communication is significantly positively correlated with adherence, and that training physicians in communication results in improved adherence. Additionally, results showed that physician type (pediatric or adult) moderates the correlation between communication and adherence, such that the correlation is higher when the physician is a pediatrician. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Piette J, Schillinger D, Potter M, Heisler M. Dimensions of patient-provider communication and diabetes self-care in an ethnically divese population. J Gen Intern Med. 2003;18:624–633. doi: 10.1046/j.1525-1497.2003.31968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Heisler M, Bouknight RR, Hayward RA, et al. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17:243–252. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Verlinde E, De Laender N, De Maesschalck S, Deveugele M, Willems S. The social gradient in doctor-patient communication. Int J Equlity Health. 2012;11:12. doi: 10.1186/1475-9276-11-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Street RJ, Jr, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient participation in medical consultations: Why some patients are more involved than others. Med Care. 2005;43:960–969. doi: 10.1097/01.mlr.0000178172.40344.70. [DOI] [PubMed] [Google Scholar]
- 58.Kinnersley P, Edwards A, Hood K, et al. Interventions before consultations for helping patients address their information needs by encouraging question asking: systematic review. BMJ. 2008;337:a485. doi: 10.1136/bmj.a485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Harrington J, Noble LM, Newman SP. Improving patients’ communication with doctors: a systematic review of intervention studies. Patient Educ Couns. 2004;52:7–16. doi: 10.1016/s0738-3991(03)00017-x. [DOI] [PubMed] [Google Scholar]
- 60.Zoffmann V, Kirkevold M. Realizing empowerment in difficult diabetes care: A guided self-determination intervention. Qual Health Res. 2012;22:103–118. doi: 10.1177/1049732311420735. [DOI] [PubMed] [Google Scholar]
- 61.American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians Transitions Clinical Report Authoring Group. Clinical report - supporting the health care transition from adolescence to adulthood in the medical home. Pediatr. 2011;128:182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- 62.Telfair J, Alexander L, Loosier P, et al. Providers’ perspectives and beliefs regarding transition to adult care for adolescents with sickle cell disease. J Health Care Poor Underserved. 2004;15:443–461. doi: 10.1353/hpu.2004.0049. [DOI] [PubMed] [Google Scholar]
- 63.Lotstein D, Ghandour R, Cash A, et al. Planning for health care transitions: results from the 2005–2006 National Survey of Children with Special Health Care Needs. Pediatr. 2009;123:e145–e152. doi: 10.1542/peds.2008-1298. [DOI] [PubMed] [Google Scholar]
- 64.Stivers T. Physician-child interaction: when children answer physicians’ questions in routine medical encounters. Patient Educ Couns. 2012;87:3–9. doi: 10.1016/j.pec.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 65.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94:2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Stivers T, Majid A. Questioning children: interactional evidence of implicit bias in medical interviews. Soc Psychol Q. 2007;70:424–441. [Google Scholar]
- 67.Schoenthaler A, Chaplin W, Allegrante J, et al. Provider communication effects medication adhenrece in hypertensive Afircan Americans. Patient Educ Couns. 2009;75:185–191. doi: 10.1016/j.pec.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Peek ME, Quinn MT, Gorawara-Bhat R, et al. How is shared decision-making defined among African Americans with diabetes? Patient Educ Couns. 2008;72:450–458. doi: 10.1016/j.pec.2008.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Teal C, Street R. Critical elements of culturally competent communication in the medical encounter: a review and model. Soc Sci Med. 2009;68:533–543. doi: 10.1016/j.socscimed.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 70.Miller K, Martell Z, Pazdirek L, et al. The role of interpreters in psychotherapy with refugees: an exploratory study. Am J Orthopsychiatry. 2005;75:27–39. doi: 10.1037/0002-9432.75.1.27. [DOI] [PubMed] [Google Scholar]
- 71.Fernandez A, Schillinger D, Warton E, et al. Language barriers, physician-patient langauge concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE) J Gen Intern Med. 2011;26:170–176. doi: 10.1007/s11606-010-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.de Beaufort C, Jarosz-Chobot P, Frank M, et al. Transition from pediatric to adult diabetes care: smooth or slippery? Pediatr Diabetes. 2009;11:24–27. doi: 10.1111/j.1399-5448.2009.00524.x. [DOI] [PubMed] [Google Scholar]
- 73.Swedlund MP, Schumacher JB, Young HN, Cox ED. Effect of communication style and physician-family relationships on satisfaction with pediatric chronic disease care. Health Commun. 2012;27:498–505. doi: 10.1080/10410236.2011.616632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Croom A, Wiebe DJ, Berg CA, et al. Adolescent and parent perceptions of patient-centered communication while managing type 1 diabetes. J Pediatr Psychol. 2011;36:206–215. doi: 10.1093/jpepsy/jsq072. [DOI] [PMC free article] [PubMed] [Google Scholar]