ABSTRACT
BACKGROUND
In our ever-increasingly multicultural, multilingual society, medical interpreters serve an important role in the provision of care. Though it is known that using untrained interpreters leads to decreased quality of care for limited English proficiency patients, because of a short supply of professionals and a lack of formalized, feasible education programs for volunteers, community health centers and internal medicine practices continue to rely on untrained interpreters.
OBJECTIVE
To develop and formally evaluate a novel medical interpreter education program that encompasses major tenets of interpretation, tailored to the needs of volunteer medical interpreters.
DESIGN
One-armed, quasi-experimental retro-pre–post study using survey ratings and feedback correlated by assessment scores to determine educational intervention effects.
PARTICIPANTS
Thirty-eight students; 24 Spanish, nine Mandarin, and five Vietnamese. The majority had prior interpreting experience but no formal medical interpreter training.
OUTCOME MEASURES
Students completed retrospective pre-test and post-test surveys measuring confidence in and perceived knowledge of key skills of interpretation. Primary outcome measures were a 10-point Likert scale for survey questions of knowledge, skills, and confidence, written and oral assessments of interpreter skills, and qualitative evidence of newfound knowledge in written reflections.
RESULTS
Analyses showed a statistically significant (P <0.001) change of about two points in mean self-ratings on knowledge, skills, and confidence, with large effect sizes (d > 0.8). The second half of the program was also quantitatively and qualitatively shown to be a vital learning experience, resulting in 18 % more students passing the oral assessments; a 19 % increase in mean scores for written assessments; and a newfound understanding of interpreter roles and ways to navigate them.
CONCLUSIONS
This innovative program was successful in increasing volunteer interpreters’ skills and knowledge of interpretation, as well as confidence in own abilities. Additionally, the program effectively taught how to navigate the roles of the interpreter to maintain clear communication.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-013-2502-5) contains supplementary material, which is available to authorized users.
KEY WORDS: interpreter, community health, minority health, quality improvement, underserved populations
INTRODUCTION
With ever-increasing numbers of immigrants and individuals for whom English is not the primary language, physicians and health centers in cities across the country must adapt to appropriately serve an increased number of limited English proficiency (LEP) patients. However, studies have shown that LEP patients experience limited access to medical care and inferior quality of care overall.1 Although professional interpreter services can improve the quality of care provided to LEP patients2 and even increase delivery of care,3 the few current education programs are typically intended for those pursuing medical interpretation as a career, are not consistent or offered in every state, and often require 1 to 2 years of post-baccalaureate education. Education programs vary from as few as 2 hours to as many as 200+ hours,4 and there are currently many competing accreditation bodies for medical interpreter certification. As a result, no clear standard exists and the present pathways to the various certifications are too long to be feasible requirements for volunteer medical interpreters. Many healthcare centers consequently develop internal trainings to address the lack of preparation, with training varying widely.5
Community health centers (CHCs) generally provide no professional interpreter services, relying on untrained volunteer interpreters or family members due to limited resources.6,7 Additionally, CHCs often do not prescreen their bilingual volunteers or require formalized training as a prerequisite for interpreting. To our knowledge, only one formal course exists to train volunteer interpreters who do not intend to pursue medical interpretation as a profession.8 However, this course is not tailored to the typical interpreter base of most CHCs: less-fluent, home-background speakers of their Language of Service (LOS). Though some volunteers at CHCs are native speakers of the LOS, many are home-background speakers (individuals with exposure to a heritage language within home and/or community9) with varying levels of fluency. Similarly, even native speakers may not be sufficiently fluent in English to provide high-quality interpretation and are unprepared to navigate the various roles of an interpreter, such as serving as a conduit, message clarifier, cultural broker, and patient advocate.10,11 Qualified instruction is needed to understand such complex roles. The cultural broker role (defined as providing a cultural framework for understanding a message in situations where cultural differences can lead to misunderstanding11) has been shown to be especially difficult to navigate.12
To our knowledge, no existing medical interpreter education program addresses the needs of volunteer interpreters and provides the necessary comprehensive interpretation training. A recent study by Flores has shown that the number of hours of prior formal training, rather than years of previous experience, is significantly correlated with the proportion and rate of errors of potential clinical consequence and suggests that a minimum of 100 hours is optimal.2 However, the Flores study focuses on hours of training and not content. Previous literature suggests that basic training requirements should include instruction and practice in interpretation accuracy; identification of appropriate interpreter roles for specific situations; applicable training on when and how to intervene; cross-cultural communication strategies; mentoring; and an interpreter support network to maintain skills over time.5,13 Additionally, it has been suggested that reverse shadowing of interpreters by colleagues would provide valuable performance feedback and evaluation.14 Taking all of this into account, we developed and formally evaluated an innovative volunteer medical interpreter education program that combines these elements and establishes a benchmark for training volunteer medical interpreters.
METHODS
Study Site and Sample Selection
Arbor and Pacific Free Clinics, affiliates of Stanford School of Medicine and jointly known as the Cardinal Free Clinics (CFC), are representative CHCs and provide acute medical care for a combined 1,750 patients each year, more than 30 % of which are considered LEP and require interpreters. The clinics rely solely on volunteer interpreters and, prior to the intervention, none had previously undergone formalized medical interpretation education or been formally and systematically assessed for fluency in their LOS, which resulted in varying levels of language proficiency. All CFC interpreters were eligible to participate in the study and those who underwent the training were included in the sample. This study was exempt from human subjects review by the Stanford University School of Medicine Institutional Review Board.
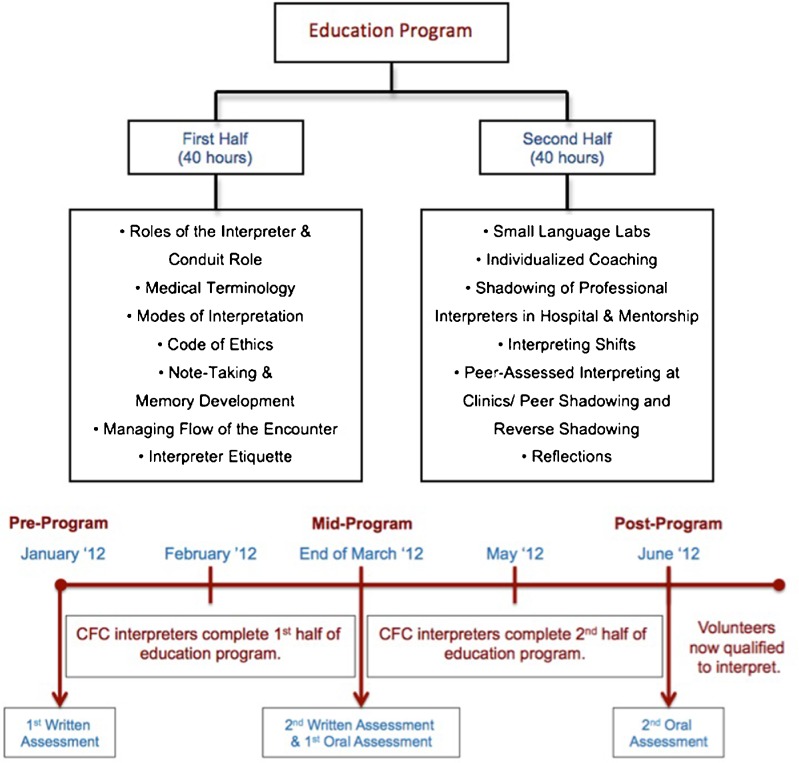
Intervention Design
As outlined in Figure 1, the intervention consisted of two parts. The foundation of the first half was the Cross Cultural Health Care Foundation’s 40-hour Bridging the Gap (BTG) interpreting curriculum.15 This training is usually taught entirely in English and allows students to learn through hands-on activities. However, to address varying levels of language proficiency typical of a volunteer interpreter base, the curriculum was supplemented with language-specific role-plays and medical terminology instruction, along with individual and group language coaching. Other teaching methods included didactic lectures, readings, online quizzes, group projects, and feedback from professional interpreters. This half provided a largely theoretical knowledge base of medical interpretation.
Figure 1.
Medical interpreter education program curriculum. The program was implemented between January 2012 and June 2012. Written assessments were administered at the pre-program and mid-program time points and oral assessments were administered at the mid-program and post-program time points.
The second half of the program complemented the first, with increased exploration of practical applications and individualized attention via one-on-one professional mentorship and coaching. This half consisted of a 10-week practicum that included biweekly language labs led by professional interpreters, clinic shifts, on-site peer assessments at CFC, shadowing of professional interpreters at Stanford Hospital, and a reflection on shadowing experiences. The language lab component consisted of small group sessions with a maximum of ten students. Professional interpreters served as instructors and evaluated individual performance on lightning-round word interpretation, interpretation of prompted, pre-recorded audio scenarios, and group role-plays. Students also received individual mentorship by professional interpreters whom they shadowed.
Survey Design and Administration
Anonymous surveys were administered post-program. Students were asked to respond to ten survey questions, six of them on a 10-point Likert scale. The survey also invited free-text responses for questions regarding obstacles in employing proper interpreter etiquette.
Since the purpose of this intervention was to change the interpreters’ understanding or awareness of variables being measured, we expected standards of evaluation to change throughout the timeline of the study.16 As such, a retro-pre test was administered at the post-program time point to ensure an accurate baseline with the same standards for assessment of confidence in skills and abilities. To control for cognitive distortions inherent in retro-pre evaluations,17 the retrospective segment was split from the rest of the survey by a series of free-response questions meant to focus respondents’ attention on another aspect of the program and a different method of evaluation. Retrospective and post-test questions were consistent in wording and set-up. The students were first asked to rate their current levels of confidence and later advised to think back to the time before the program and rate their state then, but the questions themselves made no reference to time (See Appendix online). We thus expect any response-shift bias to be most attributable to revised standards as a function of knowledge gained from the program. Consequently, all survey data comparisons utilize retrospective data for baseline comparison to the post.
Survey Questions
Four of the survey questions were designed to measure competency in upholding basic tenets of medical interpretation and facilitating effective and clear communication between patients and providers. The questions were newly developed based on the body of existing medical interpretation literature and the goals of the BTG curriculum. See Appendix online.
Oral and Written Assessment Design and Analysis
Improvement in performance was also tracked via written exams in English administered pre-program and mid-program, and oral interpreter skills assessments in English and the LOS at various time points (Fig. 1). Data from the written assessments was used as a direct evaluation of the first half of the education program, while data from the oral assessments was used as a direct evaluation of the second half of the education program. The pre-program exam was composed of 12 multiple-choice questions covering interpreter skills, roles, and etiquette, as well as general knowledge of the field. The second exam was composed of 50 questions, mostly multiple-choice, with some free-response, testing interpretation skills more in-depth. The instructors who developed and scored the exams based them on national BTG exams and deemed them both comparably rigorous. Oral interpreter assessments were administered by professional interpreters and were composed of two scenarios, one in English and another in the LOS. The examinee was asked to interpret these, applying the skills and roles that an interpreter would in a real encounter. A passing score was awarded to students who maintained the intended message.
Cursory Theme and Content Analysis
Two authors (OH, KP) independently read and content-analyzed free-text responses and discussed common themes that emerged in the professional interpreter shadowing reflections regarding the educational impact of the experience.
Statistical Analysis
The unit of analysis for the evaluation of this curriculum was individual subjects in the intervention. Unpaired student t-tests were used for survey analysis to examine associations between retro-pre and post ratings, using Satterthwaite test for unequal variance. A paired t-test was used to analyze the change in written exam score percentage of correct answers from pre-program to mid-program. In education and behavioral science research, statistical significance and effect size have been shown to complement each other and are both recommended for good research practice.18,19 An effect size estimate is more useful for making judgments than a binary choice between significance and nonsignificance.20 Cohen’s well-cited conventions for psychological investigations continue to guide most researchers, with a d of 0.20 being small, 0.50 being moderate, and 0.80 being large.21 All data was analyzed with SAS Enterprise Guide 5.1.
RESULTS
Respondent Characteristics
Thirty-eight students completed the program in June 2012, from a starting N of 51 (attrition rate of 26 %), with students withdrawing due to logistical issues, such as scheduling conflicts, and resignation following a self-identified need to improve fluency in their LOS. Of the 38 students who completed the program, 24 interpreted for Spanish, nine for Mandarin, and five for Vietnamese. While the majority of students were home-background speakers of their LOS, some learned the language in an academic setting and a few were native speakers. Survey response rate was 92 %. The characteristics of the respondents were compared with non-respondents and determined to have no significant demographic differences.
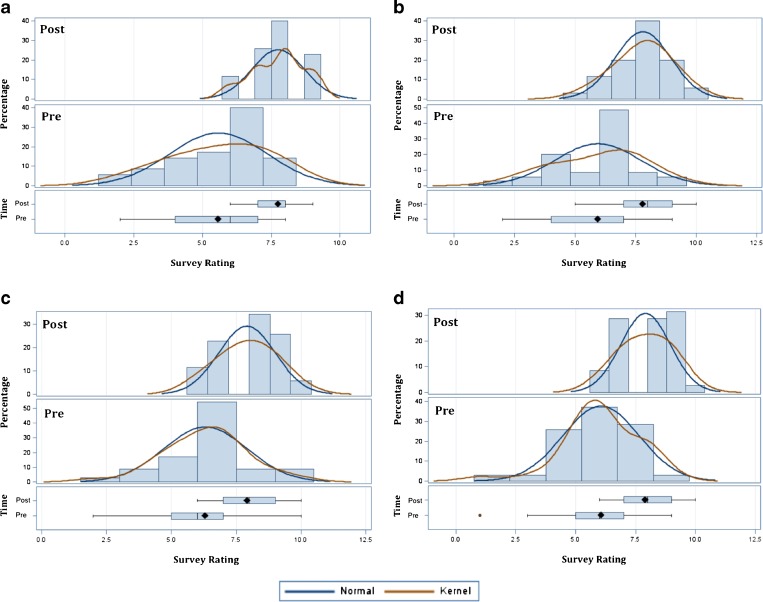
Change in Self-Assessed Knowledge, Skills, and Confidence
As shown in Figure 2, self-rated confidence levels for the four variables tested showed a statistically significant mean change of two points for all variables. Additionally, effect size for all variables was shown to be large. Cohen’s d was 1.60 for Variable A, 1.27 for Variable B, 1.19 for Variable C, and 1.41 for Variable D.
Figure 2.
Change in distributions of ratings and mean rating of self-assessed interpretation knowledge, skills, and competency. N = 35. Statistically significant (P < 0.001) change of about two points in mean rating was observed for ability to: a Provide the highest quality of interpretation (retro-pre = 5.6, post = 7.7, change = 2.2) b Maintain the message completely and accurately (retro-pre = 5.9, post = 7.8, change = 1.9) c Accurately interpret words with no direct translation (retro-pre = 6.3, post = 7.9, change = 1.6) d Serve as a cultural broker (retro-pre = 6.1, post = 7.9, change = 1.9). A distribution shift to no rating below five was observed post-program.
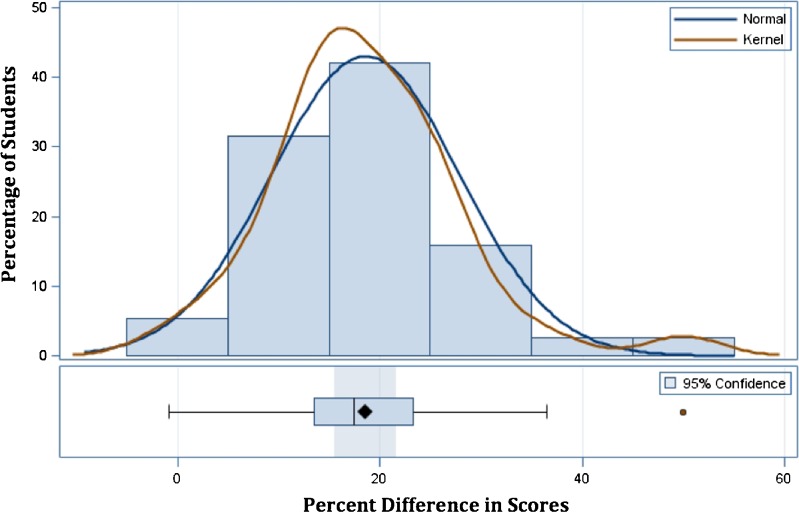
Objective Assessments: Written and Oral
A total of 38 students took both pre-program and mid-program written assessments testing knowledge of the roles of an interpreter and skills needed for proper medical interpretation. Comparison of mean test results and distribution of scores for each of the assessments can be seen in Figure 3. The mean change between percentage score from first to second assessment was 18.6 % (pre-mean = 68.7 %, post-mean = 87.3 %, P <0.001). Cohen’s d was 2.38. An examination of the student whose percentage change was negative (− 0.83 %) showed he had done well on the pretest and had little room for improvement. One student who took the initial assessment did not have a second score.
Figure 3.
Distribution of percentage change in written assessment score from pre-program to mid-program. N = 38. The mean percentage change observed for written interpreter assessments from pre-program to mid-program was 18.6 % (pre-mean = 68.7 %, post-mean = 87.3 %, P < 0.001).
A total of 39 oral interpreter assessments were administered (one student was assessed for two languages). At the mid-program time point, 33 passed and six failed the English-to-LOS Assessment, while 37 passed and two failed the LOS-to-English Assessment. However, post-program, there was only one student who failed the English-to-LOS Assessment and none who failed the LOS-to-English Assessment (Table 1). In evaluating the student who did not pass, it was determined it was likely because of a lack of fluency in the LOS and not a lack of ability in interpreter skills. This is corroborated by the fact that the student passed the LOS-to-English assessment but not the English-to-LOS assessment, which requires a high-level of fluency in the LOS.
Table 1.
Results of Mid-Program and Post-Program Oral Interpreter Assessments
| English to language of service* | Language of service* to English | |||
|---|---|---|---|---|
| Mid-program (n = 39) | Post-program (n = 39) | Mid-program (n = 39) | Post-program (n = 39) | |
| Pass, No. (%) | 33 (85) | 38 (97) | 37 (95) | 39 (100) |
| Fail, No. (%) | 6 (15) | 1 (2.6) | 2 (5.1) | 0 (0) |
*Language of Service = Vietnamese, Mandarin, or Spanish
Cursory Thematic Analysis of Mentorship and Shadowing Reflections
Reflections on the professional interpreter shadowing experience corroborated the need for further exploration of interpretation theory through exposure to its practical applications in real encounters. A number of educational themes emerged during content analysis, ranging from clarification on the use of social cues, intonations, and physical gestures, to practical limitations of theory and various interpreting techniques, to how to properly apply the various roles of an interpreter. A sampling of these themes is shown in Text Box 1.
Text Box 1.
Major Themes in Reflections on Shadowing Experience and Its Impact
| Serving the Role of Patient Advocate |
| • “[The interpreter] actually did step into the role of the advocate when she felt that the nurse didn’t understand that the patient’s co-pay might be too large at a certain pharmacy. That was really helpful to see, and I think it’s important for the interpreter to know when such an intervention is appropriate. I also really liked how the interpreter explained carefully to the patient when the nurse was [talking] to another nurse. It clearly comforted the patient.” |
| Serving the Role of Cultural Broker |
| • “A few months beforehand, [the patient] had gone back to her homeland to visit family. While there…[she was] diagnosed her with some form of calcification in her tissue. She came back to America and wanted to see what was wrong but did not have the words to describe it … what the patient had been trying to explain to the secretary for 20 minutes took seconds to get across through a trained medical interpreter. It was a great educational experience to see the balance and catching of social cues required to be an effective interpreter.” |
| • “The patient [was] an old Vietnamese lady, her knowledge about medical terminology [was] limited … The interpreter also noticed [a] cultural gap … When the doctor said that he hasn’t yet been able to explain her condition, the patient seemed to be very disappointed and questioned his reliability, perhaps because the Vietnamese culture is very sensitive and very dependent on doctors. Thus, the interpreter was able to explain to the patient that it was not because the doctor didn’t look at her case closely, but it was because her condition was rare and needed further consultant from specialists and radiologists from the field.” |
| Managing the Encounter: Family Members in Room |
| • “This interpreting session was difficult to navigate due to the daughter’s presence in the room. [The daughter] wanted the doctor to withhold information from the patient… [she] usually served as his interpreter; it was obvious. At times, she would interject and interpret for the patient, but the interpreter always handled those situations with ease.” |
| Managing the Encounter: Intervening & Working with Providers |
| • “The physical therapist told the interpreter that she spoke relatively fluent Spanish and would likely not need his help. As we quickly learned, however, the therapist did not speak very good Spanish at all. Although some of what she said could be understood, it was clearly creating a barrier of understanding. The interpreter was able to step in to facilitate communication between the wife and the physical therapist.” |
| Navigating Limitations of Interpretation Theory: Simultaneous Interpretation |
| • “The interpreter used simultaneous interpretation to interpret the directions of provider… Even though the interpreter did her simultaneous interpretation very well, [it] delayed several seconds so that the patient delayed to respond to the provider’s directions. Then the interpreter told the patient the meaning of each English direction, then asked the patient to follow the provider’s English directions to breathe without simultaneous interpretation. Finally, the patient successfully produced an eligible breath.” |
| Navigating Limitations of Interpretation Theory: Use of First Person |
| • “Even in the strange set up with all the family members, the interpreter did an excellent job of ensuring that everyone was included in the discussions … While talking to the patient, he couldn’t always use the first person because she became confused. This is something we had talked about during the course, and seeing it in action, it made sense when it was appropriate to use and not to use first-person.” |
DISCUSSION
Utilizing untrained interpreters or no interpreter is indisputably suboptimal for encounters with LEP patients and should be avoided, given the high risk for errors and potential for adverse patient outcomes.3,22–24 This novel 6-month training program was shown to be an effective, accelerated, and comprehensive solution for the optimization of interpreter services at CHCs, and sets a new benchmark for volunteer medical interpreter education. Comparison of retro-pre–survey and post-survey data showed a statistically significant improvement in self-assessed competency in interpretation knowledge, skills, and confidence that was corroborated by significant improvements in written and oral assessments of interpretation skills. Additionally, for all variables, effect size was greater than 0.8, which is large by most standards.21
Previous literature has suggested that mentoring and an interpreter support network are necessary to maintain skills over time.5,13 Other studies have corroborated the impact of mentoring in increasing students’ confidence in their skills and understanding of their field of study.25 Qualitative data did reveal that the language-specific mentorship provided by professional interpreters throughout the program was an invaluable counterpart to the didactic instruction. Importantly, shadowing real patient encounters also allowed students to see the limitations of medical interpretation theory first-hand and gain insight into practical applications of the various roles of an interpreter. From simpler clarifications of terminology to in-depth discussions on best approaches to working with a provider, the mentorship and shadowing clarified a wide range of issues regarding theory and the complexities of medical interpretation. For such complex roles as that of being a cultural broker, observing real instances where cultural misunderstandings could potentially hinder quality of care proved invaluable in learning the practical application of this skill. This echoes literature showing the importance and complexity of serving as a cultural broker12 and explains the need for additional exploration through hands-on practice, observation of its application in real-life encounters, and discussion.
Interestingly, the duration of our program totaled around 80 hours, which was close to the 100 hours recently described by Flores as the “useful minimum” number of hours of interpreter training.2 In fact, while their study makes a strong argument that 100 hours is necessary to significantly reduce the mean number of errors, choosing that as the cut-off for significance groups 80 hours with much less significant training and makes it appear less effective. Their preliminary analysis of varying cut-points of training and the effect on the number of total errors did show that the 80-hour cut-point also yielded a significant reduction in mean error rate to a point comparable to the 150-hour group.
Our model can be feasibly adapted by other CHCs and internal medicine practices that need interpreter services given its flexibility for implementation, short time span, and lower costs than post-baccalaureate and other more extensive programs. It is also important to note that the cost for this program is not recurring for most practices and CHCs, as interpreters typically remain on staff for long periods of time. However, an initial grant may be required to cover the cost of the professional instruction required for this program.
Our study has several limitations. First, our sample size was small and thus generalizability of results may be limited. Second, we did not use preexisting survey instruments, as none were appropriate for our purposes. Third, reoccurrence of questions in the surveys risked responses being influenced by earlier exposure. However, we controlled for such cognitive distortions with the surveys’ design, as discussed in the Methods.
Overall, this program was shown to effectively increase volunteer interpreters’ knowledge, skills, and confidence, thereby increasing the quality of the volunteers’ interpretation. Though not directly measured, we expect this intervention to have improved quality of care for LEP patients through the improved interpreter services. Although we have demonstrated one successful model for training interpreters, as education programs vary widely, future research should explore different approaches to medical interpreter education and the optimal period and duration of training. An analysis of categorical interpreter error rates before and after the intervention would also quantify the program’s ability to improve patient safety.
Electronic supplementary material
(DOCX 131 kb)
Acknowledgements
Contributors
We gratefully acknowledge Johanna Parker, MA, Margarita Bekker, AHI (CCHI), BA, and Natalia Becerra, MA, the instructors of the program, for sharing their passion for the medical interpreter profession and vast experience with our students through their enthusiastic instruction and mentoring. We are also deeply grateful to Stanford Interpreter Services for their mentorship and tireless support of the program. We also thank Jie Li, PhD, of the Center of Excellence for Diversity in Medical Education of Stanford School of Medicine, for her valuable input in survey review and editing, as well as advice on program evaluation strategies. We further extend our gratitude to Sylvia Bereknyei, DrPH, MS for her generous advice and assistance in editing and review of the manuscript. Finally, we thank Raymond Balise, PhD, of the Center for Health Research and Policy of Stanford School of Medicine, for his help with statistical analysis and advice on data presentation.
Funders
The costs of instruction of the Bridging the Gap curriculum and program costs of instructor and coach time were generously donated to the Cardinal Free Clinics by Stanford Hospital Guest Services and Stanford Interpreter Services (SIS). The study itself did not receive financial support from any individual or organization.
Prior Presentations
2012 WGEA/WGSA/WOSR/WAAHP AAMC Western Regional Conference, April 1, 2012. The 11th Annual Community Health Symposium, Stanford School of Medicine, Office of Community Health, November 8, 2012. The Society of Student-Run Free Clinics (SSRFC) 2013 Conference, January 26, 2013.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
REFERENCES
- 1.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- 2.Flores G, Abreu M, Barone CP, Bachur R, Lin H. Errors of medical interpretation and their potential clinical consequences: a comparison of professional versus ad hoc versus no interpreters. Ann Emerg Med. 2012;20(10):1–8. doi: 10.1016/j.annemergmed.2012.01.025. [DOI] [PubMed] [Google Scholar]
- 3.Jacobs EA, Lauderdale DS, Meltzer D, Shorey JM, Levinson W, Thisted RA. Impact of interpreter services on delivery of health care to limited–english-proficient patients. J Gen Intern Med. 2001;16(7):468–474. doi: 10.1046/j.1525-1497.2001.016007468.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Council on Interpreting in Health Care. National standards for healthcare interpreter training programs. 2011. Available at: http://www.ncihc.org/assets/documents/National_Standards_5-09-11.pdf. Accessibility verified May 1,2013.
- 5.Hwa-Froelich DA, Westby CE. Considerations when working with interpreters. Commun Disord Q. 2003;24(2):78–85. doi: 10.1177/15257401030240020401. [DOI] [Google Scholar]
- 6.Casey M. Providing health care to latino immigrants: community-based efforts in the rural midwest. Am J Public Health. 2004;94(10):1709–1711. doi: 10.2105/AJPH.94.10.1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vandervort E. Linguistic services in ambulatory clinics. J Transcult Nurs. 2003;14(4):358–366. doi: 10.1177/1043659603257338. [DOI] [PubMed] [Google Scholar]
- 8. “Volunteer Health Interpreters Organization.” Volunteer Health Interpreters Organization. Volunteer Health Interpreters Organization at UC Berkeley, n.d. Web. Available at: http://calhbc.wordpress.com/decal-class/. Accessibility verified May 1, 2013.
- 9.Lacorte M, Canabal E. Interaction with heritage language learners in foreign language classrooms. In: Blyth C, editor. The Sociolinguistics of Foreign-Language Classrooms: Contributions of the Native, the near Native, and the Non-Native Speaker. Boston: Heinle and Heinle; 2002. pp. 107–129. [Google Scholar]
- 10.Larrison CR, Velez-Ortiz D, Hernandez PM, Piedra LM, Goldberg A. Brokering language and culture: can ad hoc interpreters fill the language service gap at community health centers? Soc Work Public Health. 2010;25(3):387–407. doi: 10.1080/19371910903241009. [DOI] [PubMed] [Google Scholar]
- 11.Long R, Roy NG, editors. Bridging the Gap: An Interactive Textbook for Medical Interpreters. 1. Seattle: Cross Cultural Health Care Program; 2002. [Google Scholar]
- 12.Butow PN, Lobb E, Jefford M, Goldstein D, Eisenbruch M. A bridge between cultures: interpreters' perspectives of consultations with migrant oncology patients. Support Care Canc. 2012;20(2):235–244. doi: 10.1007/s00520-010-1046-z. [DOI] [PubMed] [Google Scholar]
- 13.Langdon HW, Cheng L-RL. Collaborating with interpreters and translators: A guide for communication disorders professionals. Thinking Publications, 2002.
- 14.Smirnov S. An overview of liaison interpreting. Perspect Stud Transl. 1997;5(2):211–226. doi: 10.1080/0907676X.1997.9961311. [DOI] [Google Scholar]
- 15.Cross Cultural Healthcare Program. Bridging the Gap Training Programs. The Cross Cultural Healthcare Program. July 25, 2012. Available at http://xculture.org/medical-interpreter-training/bridging-the-gap-training-program. Accessibility verified May 1, 2013.
- 16.Howard G. Internal invalidity in pretest–posttest self-report evaluations and a re-evaluation of retrospective pretests. Appl Psychol Meas. 1979;3(1):1–23. [Google Scholar]
- 17.Hill L. Revisiting the retrospective pretest. Am J Eval. 2005;26(4):501–517. doi: 10.1177/1098214005281356. [DOI] [Google Scholar]
- 18.Fan X. Statistical significance and effect size in education research: two sides of a coin. J Educ Res. 2001;94(5):275–282. doi: 10.1080/00220670109598763. [DOI] [Google Scholar]
- 19.Cohen J. Statistical power analysis for the behavioral sciences. Lawrence Erlbaum, 1988.
- 20.McCartney K, Rosenthal R. Effect size, practical importance, and social policy for children. Child Dev. 2003;71(1):173–180. doi: 10.1111/1467-8624.00131. [DOI] [PubMed] [Google Scholar]
- 21.Cohen J. Things I have learned (so far) Am Psychol. 1990;45(12):1304. doi: 10.1037/0003-066X.45.12.1304. [DOI] [Google Scholar]
- 22.Flores G, Laws MB, Mayo SJ. Errors in pediatric medical interpretation and their potential clinical consequences in encounters. Pediatrics. 2003;111(1):6–14. doi: 10.1542/peds.111.1.6. [DOI] [PubMed] [Google Scholar]
- 23.Jacobs E. The impact of an enhanced interpreter service intervention on hospital costs and patient satisfaction. J Gen Intern Med. 2001;22(2):306–311. doi: 10.1007/s11606-007-0357-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baker D, Parker R, Williams M, Coates WPK. Use and effectiveness of interpreters in an emergency department. JAMA. 1996;275(10):783–788. doi: 10.1001/jama.1996.03530340047028. [DOI] [PubMed] [Google Scholar]
- 25.Falk GA, Robb WB, Khan WH, Hill AD. Student-selected components in surgery: providing practical experience and increasing student confidence. Ir J Med Sci. 2009;178:267–272. doi: 10.1007/s11845-009-0306-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 131 kb)