ABSTRACT
CONTEXT
Diagnosis and treatment of depression has increased over the past decade in the United States. Whether self-reported depressive symptoms among older adults have concomitantly declined is unknown.
OBJECTIVE
To examine trends in depressive symptoms among older adults in the US between 1998 and 2008.
DESIGN
Serial cross-sectional analysis of six biennial assessments.
SETTING
Health and Retirement Study (HRS), a nationally-representative survey.
PATIENTS OR OTHER PARTICIPANTS
Adults aged 55 and older (N = 16,184 in 1998).
MAIN OUTCOME MEASURE
The eight-item Center for Epidemiologic Studies Depression scale (CES-D8) assessed three levels of depressive symptoms (none = 0, elevated = 4+, severe = 6+), adjusting for demographic and clinical characteristics.
RESULTS
Having no depressive symptoms increased over the 10-year period from 40.9 % to 47.4 % (prevalence ratio [PR]: 1.16, 95 % CI: 1.13–1.19), with significant increases in those aged ≥ 60 relative to those aged 55–59. There was a 7 % prevalence reduction of elevated symptoms from 15.5 % to 14.2 % (PR: 0.93, 95 % CI: 0.88–0.98), which was most pronounced among those aged 80–84 in whom the prevalence of elevated symptoms declined from 14.3 % to 9.6 %. Prevalence of having severe depressive symptoms increased from 5.8 % to 6.8 % (PR: 1.17, 95 % CI: 1.06–1.28); however, this increase was limited to those aged 55–59, with the probability of severe symptoms increasing from 8.7 % to 11.8 %. No significant changes in severe symptoms were observed for those aged ≥ 60.
CONCLUSIONS
Overall late-life depressive symptom burden declined significantly from 1998 to 2008. This decrease appeared to be driven primarily by greater reductions in depressive symptoms in the oldest-old, and by an increase in those with no depressive symptoms. These changes in symptom burden were robust to physical, functional, demographic, and economic factors. Future research should examine whether this decrease in depressive symptoms is associated with improved treatment outcomes, and if there have been changes in the treatment received for the various age cohorts.
KEY WORDS: depression, United States, older adults, Health and Retirement Study, HRS
INTRODUCTION
Depression diagnosis and treatment has increased over time in general,1 and among those over 65 years of age.2 Among older adults, 15–27 % in the community and up to 37 % seen in primary care settings experience depressive symptoms.3,4 This represents a shift where acceptance of depression as a “normal” part of aging and stigma had historically hindered depression recognition and care.5 It is unknown whether the prevalence and severity of depressive symptoms among older adults have decreased with expanded diagnosis and treatment.
Population-based studies examining late-life depressive symptom trends are sparse or limited by study design. Reasons include use of: a single cross-sectional data assessment,6 longitudinal study designs (which represent intra-individual change, not population trends),7–10 lifetime prevalence measures,11 data solely from younger adults,12 samples from narrowly defined geographic areas,13 or clinic samples.14 Attempts to compare information from different sources may generate uncertainty. The only repeated cross-sectional assessment of current depressive symptoms was conducted in the Stirling County Study,15 which interviewed representative population samples of a Canadian region in 1952, 1970, and 1992, and cannot address more recent or representative population trends in depressive symptoms.
Given limited prior findings, we conducted a population-based evaluation of depressive symptom prevalence over time by characterizing symptom trends over a decade among older adults in the United States.
METHODS
We used the Health and Retirement Study (HRS), a nationally representative study of older adults, which assesses health, wealth, and functioning.16 Participants are re-interviewed biennially; new respondents are added to HRS every 6 years (including 1998 and 2004). High initial (86–91 %)17 and re-interview response rates (94–96 %), limited migration in and out of the sample, and use of non-response adjusted respondent-level sample weights for each biennial survey18 allows the HRS sample to maintain representativeness of the target population over time, while minimizing any risk of healthy survivor bias. HRS is continuously representative of the non-institutionalized US adult population age 55 and older for all study waves between 1998 and 2008,17, the time period we selected for a repeated cross-sectional analysis. Only self-respondents were included; depressive symptoms are not assessed for proxy respondents.
Dependent Variable: Depressive Symptom Burden
The eight-item Center for Epidemiologic Studies Depression scale (CES-D8)19 assessed depressive symptoms. The CES-D8 asks whether the respondent experienced the following sentiments all or most of the time during the past week: (1) depressed, (2) everything is an effort, (3) sleep is restless, (4) happy, (5) lonely, (6) enjoyed life, (7) sad, (8) could not get going. The “yes” responses to questions 1, 2, 3, 5, 7, and 8 and “no” responses to questions 4 and 6 were summed for a total symptom score ranging from 0–8; with 8 representing the greatest symptom burden. Scores ≥ 4 on the CES-D8 corresponds to ≥ 16 on the full CES-D, indicating elevated depressive symptoms.20–22 Psychometric properties of the CES-D8 are well-established overall and among older people.19 It has been used in several studies of late-life depressive symptoms, demonstrating associations between elevated symptoms and poor self-rated health,23 physical illness,21 and mortality.24 We examined three symptom burdens: no symptoms (CES-D8 = 0), elevated symptoms (CES-D8 = 4+), and severe symptoms (CES-D8 ≥ 6).
Independent Variables
Demographic characteristics assessed included age (5-year increments from 55 to 85, > 85) sex (male, female), race/ethnicity (white/other, black, Hispanic), educational attainment (11 years, 12 years, 13–15 years, and ≥ 16 years), net worth quartile, marital status (married/partnered, separated/divorced, widowed, never married), and work status (working full-time, working part-time, retired, other employment status including disabled, student, or homemaker). We controlled for mode of administration (face-to-face, telephone); however, telephone administration of clinical interviews is now widely used and accepted based on evidence of comparable validity to in-person interviews in clinical reappraisal studies, including those assessing depressive symptoms.25
Health-related factors included: weight (normal/underweight [BMI < 25], overweight [BMI 25–30], obese [BMI > 30], cigarette smoking status (current, former, never smoker), alcohol use (non-drinker, one to four drinks per week, or five or more drinks per week), activities of daily living (ADL: bathing, eating, dressing, walking across a room, and getting in or out of bed) and instrumental activities of daily living (IADL: using a telephone, taking medication, handling money, shopping, preparing meals; 0, 1, 2–5, with higher counts representing greater impairment), and a count of the seven chronic medical comorbidities assessed by HRS (hypertension, diabetes, any heart condition, stroke, arthritis, chronic lung disease, cancer, scored 0, 1–3, ≥ 4).
Statistical Analysis
We identified the proportion of individuals with each covariate in each study wave using descriptive statistics. Unadjusted logistic regressions examined prevalence of depressive symptoms by wave from 1998– to 2008, prevalence differences (PD: 2008 prevalence minus 1998 prevalence) and prevalence ratios (PR: 2008/1998 prevalence) of having no, elevated, and severe symptoms.
Analyses predicting each outcome used logistic regression for overall and age-specific adjusted prevalence, adjusted prevalence differences (PD), and adjusted prevalence ratios (PR) of the 10-year change using the method of “recycled predictions.”26 This method calculates mean predicted prevalence of the outcome (depressive symptom level) based on coefficients from the fitted regression model, fixing the independent variable of interest (year overall, and by age group) at a specific value while letting other covariates vary at their original values for every individual in the sample. The process is repeated, fixing the independent variable at alternate values. These models, successfully implemented elsewhere,27,28 standardize the PR to the distribution of variables in the sample and ease interpretation of interactions. Analyses used STATA 12.1 with a two-sided p value of < 0.05 indicating statistical significance. Analyses were adjusted for the multi-stage, area-clustered, stratified sample for use with repeated cross-sectional analyses, which accounts for cluster-level homogeneity (intra-class correlation), including the overlap in cases between waves.29
RESULTS
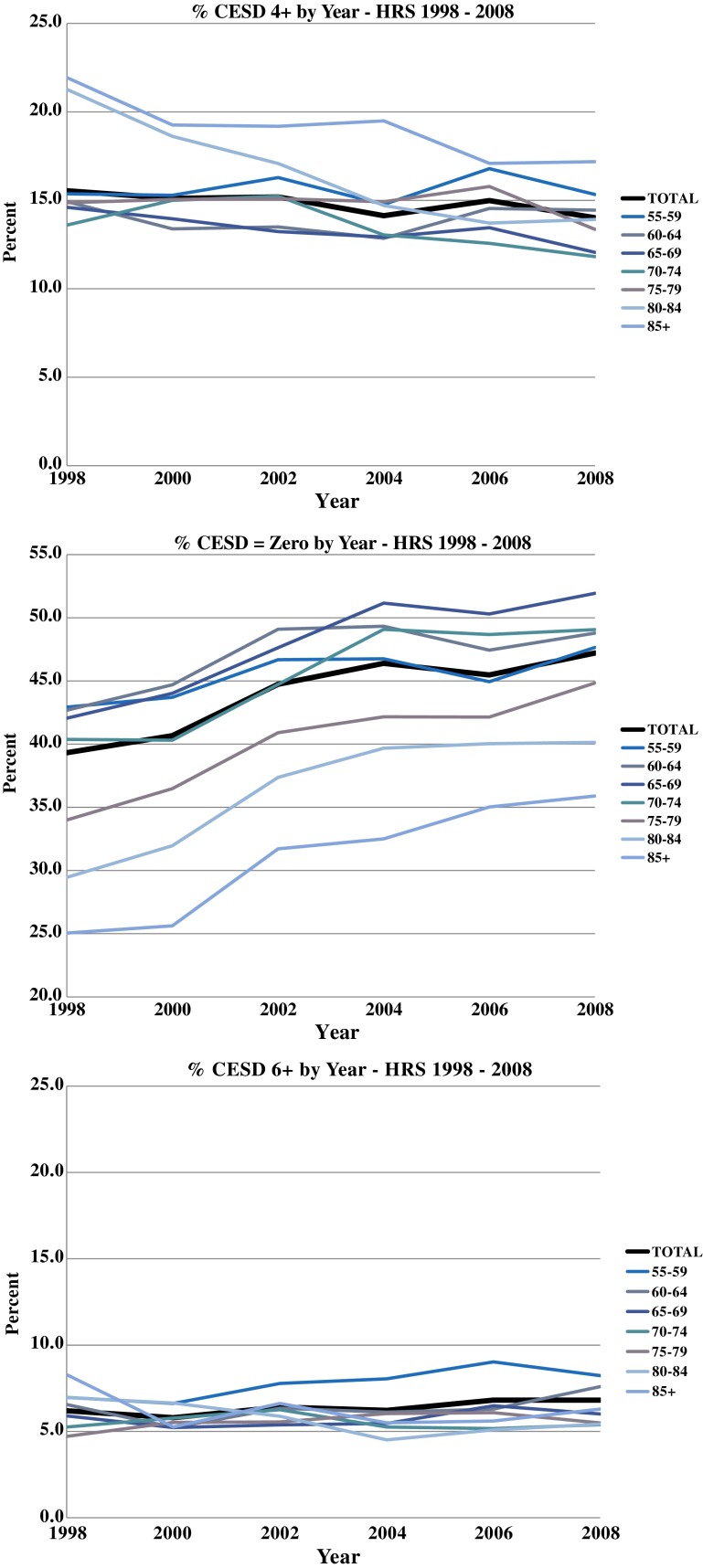
Table 1 presents sociodemographic and clinical characteristics of the study population by year, which varied from 16,338 in 1998 to 14,050 in 2008. Figure 1 illustrates proportions of individuals with no, elevated, and severe symptoms, overall, and by age group. Table 2 presents covariate PRs. Table 3 presents adjusted prevalence, PDs, and PRs for depressive symptom trends overall and by age group.
Table 1.
Characteristics by Year (HRS 1998–2008) (%, N)
| 1998 | 2000 | 2002 | 2004 | 2006 | 2008 | |
|---|---|---|---|---|---|---|
| n = 16184 | n = 15,293 | n = 14,750 | n = 14,616 | n = 14,699 | n = 14,482 | |
| CESD 0 (no symptoms) | 39 (6,198) | 41 (6,112) | 45 (6,461) | 46 (6,665) | 45 (6,601) | 47 (6,696) |
| CESD 1–8 | 61 (9,986) | 59 (9,181) | 55 (8,289) | 54 (7,951) | 55 (8,098) | 53 (7,786) |
| CESD 0–3 | 84 (13,539) | 85 (12,927) | 85 (12,459) | 86 (12,501) | 85 (12,497) | 86 (12,478) |
| CESD 4+ (elevated symptoms) | 16 (2,645) | 15 (2,366) | 15 (2,291) | 14 (2,115) | 15 (2,202) | 14 (2,004) |
| CESD 0–5 | 94 (15,120) | 94 (14,367) | 94 (13,798) | 94 (13,699) | 93 (13,719) | 93 (13,530) |
| CESD 6+ (severe symptoms) | 6 (1,064) | 6 (926) | 6 (952) | 6 (917) | 7 (980) | 7 (952) |
| Age 55–59 | 23 (3,495) | 24 (2,765) | 25 (2,173) | 26 (2,216) | 29 (2,380) | 28 (2,378) |
| Age 60–64 | 18 (3,374) | 18 (3,315) | 19 (3,318) | 20 (2,844) | 20 (2,227) | 21 (2,001) |
| Age 65–69 | 17 (2,778) | 17 (2,932) | 16 (2,967) | 15 (3,053) | 15 (3,191) | 16 (2,938) |
| Age 70–74 | 17 (2,471) | 15 (2,193) | 14 (2,273) | 14 (2,410) | 12 (2,632) | 12 (2,685) |
| Age 75–79 | 13 (2,011) | 12 (1,928) | 12 (1,762) | 12 (1,799) | 11 (1,833) | 10 (1,979) |
| Age 80–84 | 8 (1,202) | 8 (1,284) | 9 (1,375) | 8 (1,345) | 8 (1,346) | 7 (1,341) |
| Age 85+ | 5 (853) | 5 (876) | 5 (882) | 5 (949) | 6 (1,090) | 6 (1,160) |
| Age range min–max | 55–105 | 55–101 | 55–109 | 55–103 | 55–105 | 55–107 |
| Mean age (se) | 67.9 (0.14) | 67.9 (0.15) | 67.8 (0.15) | 67.5 (0.17) | 67.1 (0.16) | 67.0 (0.16) |
| Birth cohorts min–max | 1892–1944 | 1898–1945 | 1892–1947 | 1900–1950 | 1900–1952 | 1900–1953 |
| Male | 42 (6,750) | 42 (6,246) | 42 (5,941) | 43 (5,953) | 44 (6,048) | 45 (6,001) |
| Female | 58 (9,434) | 58 (9,047) | 58 (8,809) | 57 (8,663) | 56 (8,651) | 55 (8,481) |
| White/Other | 86 (12,838) | 85 (12,142) | 85 (11,676) | 85 (11,474) | 85 (11,485) | 84 (11,155) |
| Hispanic | 6 (1,156) | 6 (1,110) | 6 (1,088) | 6 (1,162) | 6 (1,226) | 7 (1,305) |
| Black | 9 (2,190) | 9 (2,041) | 9 (1,986) | 9 (1,980) | 9 (1,988) | 9 (2,022) |
| Education 0–11 years | 28 (4,865) | 25 (4,303) | 23 (3,812) | 21 (3,612) | 20 (3,535) | 18 (3,258) |
| Education 12 years | 35 (5,535) | 35 (5,312) | 35 (5,182) | 35 (5,106) | 34 (5,060) | 33 (4,908) |
| Education 13–15 years | 19 (2,973) | 20 (2,852) | 21 (2,874) | 21 (2,919) | 22 (2,987) | 23 (3,067) |
| Education 16 years | 19 (2,810) | 20 (2,826) | 22 (2,880) | 23 (2,972) | 25 (3,102) | 26 (3,228) |
| Net worth ≤ $65,293† | 26 (4,465) | 25 (4,055) | 24 (3,826) | 24 (3,759) | 25 (3,835) | 26 (3,891) |
| Net worth $65,293–$222,461 | 28 (4,663) | 26 (4,153) | 27 (3,999) | 25 (3,726) | 22 (3,309) | 23 (3,429) |
| Net worth $222,462–$572,099 | 25 (3,923) | 25 (3,768) | 26 (3,648) | 25 (3,563) | 25 (3,660) | 24 (3,471) |
| Net worth > $572,099 | 21 (3,133) | 23 (3,317) | 24 (3,276) | 26 (3,568) | 28 (3,895) | 27 (3,691) |
| Married/partnered | 62 (10,490) | 62 (9,773) | 62 (9,363) | 64 (9,419) | 64 (9,407) | 64 (9,176) |
| Separated/divorced | 11 (1,701) | 13 (1,646) | 13 (1,666) | 13 (1,600) | 14 (1,676) | 15 (1,780) |
| Widowed | 23 (3,496) | 22 (3,407) | 21 (3,289) | 20 (3,166) | 19 (3,194) | 18 (3,078) |
| Never married | 3 (476) | 4 (449) | 3 (416) | 4 (422) | 4 (421) | 4 (447) |
| Working full time | 22 (3,412) | 23 (3,019) | 23 (2,744) | 24 (2,673) | 27 (2,680) | 28 (2,822) |
| Working part time | 14 (2,212) | 14 (2,153) | 14 (2,057) | 15 (2,108) | 14 (2,062) | 14 (1,976) |
| Retired | 50 (8,126) | 48 (7,620) | 48 (7,644) | 49 (8,075) | 49 (8,365) | 48 (8,282) |
| Other employment status | 14 (2,434) | 15 (2,501) | 15 (2,304) | 12 (1,760) | 11 (1,592) | 10 (1,402) |
| Normal/under weight | 39 (6,102) | 36 (5,486) | 35 (5,144) | 35 (5,078) | 31 (4,630) | 29 (4,397) |
| Overweight | 39 (6,388) | 40 (6,090) | 39 (5,770) | 38 (5,558) | 39 (5,641) | 39 (5,529) |
| Obese | 22 (3,678) | 24 (3,705) | 26 (3,817) | 27 (3,964) | 31 (4,412) | 32 (4,540) |
| Never smoked | 41 (6,585) | 41 (6,268) | 41 (6,105) | 41 (6,108) | 42 (6,225) | 43 (6,238) |
| Past smoker | 44 (7,042) | 44 (6,769) | 45 (6,599) | 44 (6,535) | 44 (6,562) | 43 (6,408) |
| Current smoker | 15 (2,480) | 15 (2,179) | 14 (1,969) | 14 (1,902) | 14 (1,845) | 14 (1,770) |
| Non-drinker | 69 (11,431) | 71 (11,145) | 68 (10,279) | 65 (9,976) | 64 (9,943) | 63 (9,697) |
| Drinks 1–4 days/week | 20 (3,122) | 19 (2,696) | 22 (2,985) | 23 (3,085) | 24 (3,173) | 25 (3,237) |
| Drinks 5–7 days/week | 11 (1,631) | 10 (1,440) | 10 (1,461) | 11 (1,531) | 11 (1,561) | 12 (1,534) |
| 0 ADL | 85 (13,681) | 85 (12,963) | 86 (12,543) | 86 (12,431) | 85 (12,270) | 86 (12,196) |
| 1 ADL | 8 (1,311) | 8 (1,296) | 8 (1,217) | 8 (1,189) | 9 (1,332) | 8 (1,238) |
| 2–5 ADL | 7 (1,175) | 6 (1,025) | 6 (985) | 6 (992) | 7 (1,096) | 6 (1,043) |
| 0 IADL | 88 (14,187) | 89 (13,539) | 88 (12,972) | 88 (12,776) | 87 (12,708) | 88 (12,568) |
| 1 IADL | 7 (1,146) | 6 (1,010) | 7 (1,016) | 7 (1,107) | 7 (1,130) | 7 (1,077) |
| 2–5 IADL | 5 (829) | 5 (734) | 5 (757) | 5 (729) | 5 (860) | 5 (831) |
| 0 chronic conditions | 22 (3,322) | 20 (2,831) | 18 (2,375) | 17 (2,158) | 16 (1,893) | 16 (1,703) |
| 1–3 chronic conditions | 71 (11,701) | 72 (11,189) | 72 (10,889) | 72 (10,790) | 72 (10,858) | 72 (10,660) |
| 4+ chronic conditions | 7 (1,161) | 8 (1,273) | 9 (1,485) | 10 (1,668) | 11 (1,947) | 12 (2,118) |
| telephone interview | 66 (11,091) | 84 (12,708) | 81 (11,815) | 30 (3,513) | 42 (5,943) | 46 (6,214) |
| Face to face interview | 34 (5,023) | 16 (2,556) | 19 (2,935) | 70 (11,103) | 58 (8,755) | 54 (8,268) |
†The consumer price index was used to convert net worth to 2009 dollars, and then quartiles of net worth were created
CESD Center for Epidemiologic Studies Depression scale; ADL activities of daily living; IADL instrumental activities of daily living
Figure 1.
Elevated depressive symptoms (4+), no symptoms (0), and severe symptoms (6+): Total and by age group, 1998 to 2008.
Table 2.
Adjusted Logistic Regression Models for HRS (1998–2008)
| CESD = 0 (no symptoms | CESD 4+ (elevated symptoms) | CESD 6+ (severe symptoms) | |
|---|---|---|---|
| Prevalence ratio (CI) | Prevalence ratio (CI) | Prevalence ratio (CI) | |
| Male | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Female | 0.95*** (0.93, 0.98) | 1.14*** (1.09, 1.19) | 1.18** (1.07, 1.30) |
| White/Other | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Hispanic | 0.91** (0.86, 0.97) | 1.33*** (1.20, 1.48) | 1.50*** (1.31, 1.71) |
| Black | 0.93** (0.89, 0.97) | 0.94 (0.87, 1.01) | 0.92 (0.82, 1.04) |
| Education 0–11 years | 0.85*** (0.83, 0.88) | 1.23*** (1.16, 1.29) | 1.21*** (1.11, 1.32) |
| Education 12 years | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Education 13–15 years | 1.07*** (1.03, 1.10) | 0.92* (0.85, 0.99) | 0.91 (0.81, 1.03) |
| Education 16 years | 1.14*** (1.10, 1.18) | 0.76*** (0.70, 0.83) | 0.69*** (0.59, 0.80) |
| Net worth ≤ $65,293 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Net worth $65,293–$222,461 | 1.11*** (1.08, 1.14) | 0.85*** (0.80, 0.90) | 0.81*** (0.75, 0.88) |
| Net worth $222,462–$572,099 | 1.15*** (1.11, 1.20) | 0.80*** (0.75, 0.86) | 0.73*** (0.65, 0.82) |
| Net worth > $572,099 | 1.19*** (1.15, 1.24) | 0.71*** (0.65, 0.78) | 0.64*** (0.55, 0.75) |
| Married/partnered | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Separated/divorced | 0.82*** (0.77, 0.86) | 1.47*** (1.36, 1.59) | 1.56*** (1.41, 1.73) |
| Widowed | 0.80*** (0.78, 0.82) | 1.47*** (1.39, 1.55) | 1.52*** (1.38, 1.69) |
| Never married | 0.86*** (0.79, 0.93) | 1.39*** (1.17, 1.64) | 1.41* (1.09, 1.81) |
| Working full time | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Working part time | 0.97 (0.94, 1.00) | 1.08 (0.99, 1.18) | 1.10 (0.95, 1.27) |
| Retired | 0.88*** (0.85, 0.91) | 1.29*** (1.18, 1.41) | 1.47*** (1.29, 1.68) |
| Other employment status | 0.79*** (0.74, 0.83) | 1.53*** (1.41, 1.67) | 1.79*** (1.57, 2.03) |
| Normal/under weight | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Overweight | 0.98 (0.96, 1.01) | 0.96 (0.90, 1.01) | 0.91* (0.84, 0.98) |
| Obese | 0.94** (0.91, 0.98) | 1.00 (0.95, 1.06) | 0.92 (0.85, 1.01) |
| Never smoked | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Past smoker | 0.98 (0.96, 1.01) | 1.07* (1.01, 1.14) | 1.11* (1.01, 1.21) |
| Current smoker | 0.87*** (0.83, 0.90) | 1.29*** (1.19, 1.40) | 1.32*** (1.17, 1.50) |
| Non-drinker | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Drinks 1–4 days/week | 1.05*** (1.03, 1.08) | 0.92** (0.88, 0.97) | 0.86** (0.79, 0.94) |
| Drinks 5–7 days/week | 1.06** (1.03, 1.10) | 0.93 (0.85, 1.02) | 0.93 (0.80, 1.08) |
| 0 ADL | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1 ADL | 0.59*** (0.56, 0.62) | 1.79*** (1.69, 1.90) | 2.20*** (1.98, 2.44) |
| 2–5 ADL | 0.45*** (0.42, 0.49) | 2.21*** (2.08, 2.35) | 2.89*** (2.62, 3.20) |
| 0 IADL | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1 IADL | 0.65*** (0.61, 0.68) | 1.61*** (1.53, 1.71) | 1.54*** (1.41, 1.68) |
| 2–5 IADL | 0.64*** (0.58, 0.70) | 1.82*** (1.69, 1.97) | 1.75*** (1.56, 1.96) |
| 0 chronic conditions | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1–3 chronic conditions | 0.84*** (0.82, 0.86) | 1.43*** (1.33, 1.55) | 1.71*** (1.49, 1.96) |
| 4+ chronic conditions | 0.67*** (0.64, 0.71) | 1.76*** (1.59, 1.94) | 2.16*** (1.83, 2.57) |
| Telephone interview | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Face to face interview | 1.02 (1.00, 1.04) | 1.04* (1.00, 1.08) | 1.03 (0.97, 1.11) |
*p < 0.05, **p < 0.01, ***p < 0.001
CESD Center for Epidemiologic Studies Depression scale; ADL activities of daily living; IADL instrumental activities of daily living
Table 3.
Overall and Age-specific Adjusted Prevalence Ratios (10-year change) from Logistic Regression Models†
| Age | 1998 prevalence (%) | 2008 prevalence (%) | PD | PR | |
| CESD = 0 | 55–59 | 38.9 (37.4, 40.4) | 40.8 (38.5, 43.1) | 1.9 (−0.5, 4.3) | 1.05 (0.99, 1.11) |
| No symptoms | 60–64 | 42.0 (40.3, 43.7) | 46.1 (43.6, 48.6) | 4.1 (0.7, 7.6) | 1.10* (1.02, 1.18) |
| 65–69 | 42.4 (40.5, 44.3) | 51.6 (50.1, 53.2) | 9.3 (6.8, 11.8) | 1.22*** (1.16, 1.29) | |
| 70–74 | 42.4 (40.7, 44.2) | 51.6 (49.9, 53.2) | 9.1 (6.9, 11.4) | 1.22*** (1.16, 1.27) | |
| 75–79 | 40.1 (37.8, 42.4) | 49.8 (48.0, 51.7) | 9.8 (6.8, 12.7) | 1.24*** (1.16, 1.33) | |
| 80–84 | 40.2 (37.7, 42.6) | 49.7 (47.2, 52.2) | 9.6 (6.0, 13.2) | 1.24*** (1.14, 1.34) | |
| 85+ | 40.9 (37.4, 44.5) | 52.1 (49.3, 54.8) | 11.1 (6.4, 15.8) | 1.27*** (1.15, 1.41) | |
| Total | 40.9 (39.8, 42.0) | 47.4 (46.2, 48.5) | 6.5 (5.2, 7.8) | 1.16*** (1.13, 1.19) ◊ | |
| Age | 1998 prevalence (%) | 2008 prevalence (%) | PD | PR | |
| CESD = 4+ | 55–59 | 18.9 (17.3, 20.5) | 20.0 (18.4, 21.7) | 1.2 (−1.1, 3.4) | 1.06 (0.95, 1.19) |
| Elevated symptoms | 60–64 | 15.8 (14.4, 17.2) | 16.1 (14.4, 17.8) | 0.2 (−2.1, 2.6) | 1.02 (0.88, 1.17) |
| 65–69 | 15.7 (14.2, 17.1) | 13.3 (12.1, 14.5) | −2.4 (−4.4, −0.3) | 0.85* (0.74, 0.97) | |
| 70–74 | 14.2 (13.0, 15.5) | 12.3 (11.2, 13.5) | −1.9 (−3.6, −0.2) | 0.87* (0.76, 0.98) | |
| 75–79 | 13.1 (11.6, 14.6) | 12.6 (11.5, 13.7) | −0.5 (−2.4, 1.4) | 0.96 (0.84, 1.11) | |
| 80–84 | 14.3 (12.6, 15.9) | 9.6 (08.4, 10.8) | −4.7 (−6.9, −2.4) | 0.67*** (0.56, 0.81) | |
| 85+ | 10.6 (09.1, 12.2) | 9.2 (08.1, 10.3) | −1.4 (−3.4, 0.6) | 0.87 (0.72, 1.05) | |
| Total | 15.3 (14.4, 16.1) | 14.2 (13.5, 15.0) | −1.0 (−1.8, −0.2) | 0.93* (0.88, 0.98) ◊◊ | |
| Age | 1998 prevalence (%) | 2008 prevalence (%) | PD | PR | |
| CESD = 6+ | 55–59 | 8.7 (7.5, 9.8) | 11.8 (10.5, 13.1) | 3.1 (1.4, 4.9) | 1.36*** (1.15, 1.61) |
| Severe symptoms | 60–64 | 6.7 (5.6, 7.7) | 8.3 (7.0, 9.5) | 1.6 (−0.1, 3.2) | 1.24 (1.00, 1.54) |
| 65–69 | 6.0 (5.1, 6.9) | 6.6 (5.7, 7.5) | 0.6 (−0.8, 2.0) | 1.10 (0.88, 1.36) | |
| 70–74 | 5.4 (4.7, 6.2) | 5.5 (4.7, 6.3) | 0.1 (−1.1, 1.2) | 1.01 (0.82, 1.25) | |
| 75–79 | 4.4 (3.6, 5.2) | 5.1 (4.5, 5.8) | 0.7 (−0.2, 1.7) | 1.17 (0.95, 1.43) | |
| 80–84 | 4.3 (3.5, 5.1) | 3.5 (2.9, 4.1) | −0.8 (−1.8, 0.2) | 0.82 (0.64, 1.05) | |
| 85+ | 3.0 (2.4, 3.6) | 2.8 (2.2, 3.4) | −0.2 (−1.2, 0.8) | 0.94 (0.67, 1.32) | |
| Total | 5.8 (5.4, 6.3) | 6.8 (6.3, 7.3) | 1.0 (0.4, 1.6) | 1.17** (1.06, 1.28) ◊◊◊ |
CESD Center for Epidemiologic Studies Depression scale; PD prevalence differences, PR prevalence ratios
† PR is prevalence ratio for year, entered as a continuous variable and coded such that PR refers to 10-year change. For purposes of estimating prevalence, the recycled prediction method is used. Models include year, age group, year*age group interaction, and all covariates in Table 2
*p < 0.05, **p < 0.01, ***p < 0.001
◊ CESD = 0: Adjusted Wald test, F(6,51) = 6.69, p < 0.0001
◊◊ CESD = 4+: Adjusted Wald test: F(6,51) = 4.79, p = 0.0006
◊◊◊ CESD = 6+: Adjusted Wald test, F(6,51) = 3.12, p = 0.0111
No Depressive Symptoms
Unadjusted prevalence of having no symptoms (in a given wave) increased over time from 40.1 % to 47.8 %, indicating an increase of 7.7 % from 1998 to 2008 (PD: 7.7 %; 95 % CI: 6.2–9.2) with a PR of 1.19 (95 % CI: 1.15–1.23). Subgroups with higher prevalence of no symptoms included: men, Whites, those with education beyond high school, higher net worth, married, working, not obese, drank at least one day per week, no ADL and IADL limitations, and no chronic medical conditions (Table 2).
Adjusted analyses (Table 3) found a 16 % relative increase of having no symptoms from 40.9 % to 47.4 % (PR: 1.16, 95 % CI: 1.13–1.19). We found significantly greater increases in having no symptoms as age increased in all age groups 60+ relative to those aged 55–59.
Elevated Symptoms
Unadjusted prevalence of elevated symptoms decreased from 15.5 % to 14.2 % from 1998 to 2008, indicating an overall decline of 1.3 % (PD: 1.3 %; 95 % CI: 0.3–2.2) and PR of 0.92 (95 % CI: 0.86–0.98). In adjusted analyses, subgroups with higher prevalence of elevated symptoms included: women, Hispanics, those with less than a high school education, lower net worth, not married, not working, current smokers, those who did not drink, or those who drank 5–7 days a week, worse ADL and IADL scores, and more chronic medical conditions (Table 2).
Adjusted analyses (Table 3) found a 7 % relative reduction of elevated symptoms over the decade from 15.3 % to 14.2 % (PR: 0.93, 95%CI: 0.88–0.98). Overall, we found consistently greater reductions in elevated symptoms as age increased, with significant declines in those aged 65–69 (15.7 % to 13.3 %), 70–74 (14.2 % to 12.3 %), and 80–84 (14.3 % to 9.6 %). The decline was most pronounced among those aged 80–84 (PR: 0.67, 95 % CI: 0.56–0.81).
Severe Depressive Symptoms
Unadjusted prevalence of severe symptoms increased over time from 5.9 % to 6.8 %, indicating an overall increase of 0.9 % from 1998 to 2008 (PD: 0.9 %; 95 % CI: 0.2–1.6) with a PR of 1.15 (95 % CI: 1.03–1.28). Subgroups with higher prevalence of severe symptoms were the same as those with elevated symptoms (Table 2).
Adjusted analyses (Table 3) found a 17 % relative increase in severe symptoms from 5.8 % to 6.8 % (PR: 1.17, 95 % CI: 1.06–1.28). This increase was limited to those aged 55–59, with the adjusted probability of severe symptoms increasing from 8.7 % to 11.8 % (PR: 1.36, 95 % CI: 1.15–1.61).
DISCUSSION
In a nationally representative sample of older adults, we observed a significant decrease between 1998 and 2008 in the prevalence of depressive symptoms, which appeared to be driven primarily by decreasing prevalence of depressive symptoms among those aged 80–84. This suggests an age-dependent downward trend in symptom burden, extending previous research indicating increased late-life depression diagnoses and treatment during this period.1,2 This study advances prior work by examining a large, nationally representative sample over a decade, with more frequent symptom assessments.
This is the first study of which we are aware to examine temporal trends in the prevalence of no and severe symptoms by age, which can enrich our understanding of trends in late-life depressive symptoms. We found the largest changes in symptom prevalence at the ends of the age spectrum. The proportion of respondents with no symptoms increased significantly across all age groups, except those aged 55–59. In contrast, although the prevalence of severe depressive symptoms increased overall across the study period, the increase was confined to the 55–59 age category. This distribution of effects has potentially important ramifications; it implies that there may be a severely ill population subgroup that is either not being treated adequately or is treatment refractory. Finding an overall increase in the proportion of individuals with no symptoms indicates that an elevated symptom burden may be increasingly concentrated in a smaller proportion of the population, such as those individuals in late middle-age. More data tying population treatment patterns to severity are necessary to better understand these findings.
Finding a larger symptom burden over time in the young-old compared to oldest-old is consistent with some literature suggesting a potential cohort effect on symptoms, such that later born cohorts may be more likely to suffer from depressive disorders.30,31 A review examining studies between 1976 and 1998 reported that age was associated with less depression, controlling for other factors.32 The Duke Establishment of a Population for Epidemiologic Studies of the Elderly (EPESE) data found that symptoms were lower in the oldest-old; however, this study did not examine time trends.6
The only study we found assessing an age-by-year interaction in depressive symptoms 33 examined an earlier time period (1992–2003) and had contrary findings. That study found a significantly increasing symptom burden over time and a significant age-by-time interaction, indicating increasing depression each year among adults over age 75 in an Australian sample; however, this analysis used longitudinal data rather than repeated cross-sections, and included those living in the community and residential care.7 Given differences in methods and populations, the two studies are not comparable.
Contextualizing Findings
It is challenging to place our findings in context of existing literature due to significant differences in research designs across studies. Fombonne et al. suggested that potential explanations for challenges in identifying depressive symptom trends could include: heterogeneity in definitions of mood and instrumentation, dearth of prospective studies from multiple birth cohorts, focus on lifetime rather than current prevalence rates (which could be changing in different directions), and limitations including undetected artifacts or study methods effects.34
Age-period-cohort models may provide a useful framework for understanding our findings. Although it is always challenging to identify which of these three effects is taking place, this study held age constant at each study wave; therefore, a combination of period and cohort effects must explain our results. Period effects could include changing attitudes towards depression and/or treatment availability.1 If we had observed parallel changes (e.g. declines) in symptoms over time, we could attribute these findings to period effects. However, since we found variation in the rate of symptom decline (e.g. greater declines in the oldest old) it appears that a cohort effect was also present, such that earlier born cohorts had larger changes in symptom burdens. It is possible that earlier born cohorts had larger shifts in attitudes towards depression diagnosis and treatment than later born cohorts during the study. However, we cannot be certain to what extent period or cohort experiences came into play, as we do not have direct knowledge of cohort differences in treatment preferences or stigma, or period effects including changes in access to and use of psychotherapy or medications. Our findings are consistent with research indicating increasing aggressiveness of late-life depression treatment during the study period, and relatively larger increases in the oldest-old (85+) compared to younger-old (65–84).2
Unlike studies focused on clinic-based samples, population-based studies such as ours provide the best assessment of overall symptomatology. This is relevant because depression is underdiagnosed and undertreated in older adults; many older individuals never receive any acknowledgment of depressive symptoms.35 This study suggests that the presence and severity of depressive symptoms are not uniform across middle-aged and older adults, and may be changing over time. Our findings challenge conventional wisdom general internists may have regarding late-life depression (e.g. that it is highest in the oldest old). Although our findings suggest that depressive symptoms among older adults have declined, the overall prevalence of depressive symptoms remains high; thus, assessment and adequate treatment of depression in primary care should remain important goals for primary care providers.
Subgroup Findings
Many of our findings are consistent with other literature (e.g. higher rates of depressive symptoms among women, low income, low education, unmarried, smoker, physical limitations, chronic conditions, and psychiatric problems); a few subgroup findings merit discussion. These include higher rates of depressive symptoms among Hispanic respondents, those who abstained from drinking alcohol, and retired respondents.
Hispanic older adults receive lower rates of antidepressant and psychotherapy treatment than White or Black older adults,2 which could perhaps explain our finding of higher levels of depressive symptoms in that population. Other studies have found elevated depressive symptoms in Hispanic older adults compared to older adults of other ethnicities.36 Research indicates that moderate alcohol use among older adults can be associated with lower depression levels than abstinence or higher levels of alcohol use.37
The relationship between depression and retirement is complex; some older adults may become depressed then retire,38,39 others may retire then become depressed.40–42 Retirement may be liberating, leading to decreased symptoms.42,43 Our finding that retired older adults are more depressed than those who are working is consistent with some, yet not all literature.
Limitations
The CES-D8 is not a diagnostic instrument; it assesses depressive symptomatology. We could not account for treatment or other clinical characteristics including patient history of depression, so while the declining depressive symptom burden we observed may be related to increased diagnosis and/or treatment, this is inferred based on trends observed using other data.
CONCLUSION
Prevalence of elevated depressive symptoms declined 7 % over a decade among adults aged ≥ 55. This trend was most pronounced in those aged 80–84. We found large increases in those without any depressive symptoms and overall increases in those with the most severe symptoms (largely limited to those aged 55–59). Although the decline in elevated symptoms over time may be related to increased treatment, an increase in those with severe symptoms could indicate that a subgroup of respondents was not accessing or responding to treatment, or that increased recognition and treatment did not decrease the prevalence of severe symptoms. Future research is needed to unpack the relationships between symptom trends and age groups, and link symptom changes to diagnosis and treatment changes over time, to target effective treatments to those who would benefit most among the growing number of older adults. For primary care providers, we note several important conclusions from our study. There are large differences in the prevalence of depressive symptoms across age categories and time, although the general trend has been an overall improvement in symptoms. Although recognition of improvements in outcomes is important, equally important is the fact that different patient age subgroups have had significantly different changes in symptoms; better recognition and treatment of depression in these groups is warranted. Finally, careful, repeated measurement of depressive symptoms is important, given our findings that the prevalence of the most severe symptoms has not improved over time; those with severe symptoms may require more aggressive treatment and referral if treatment responses are not observed.
Acknowledgements
Funding Support
This study was funded by the National Institute on Aging (P01 AG031098) and the Department of Veterans Affairs, Health Services Research and Development (CD2 07-206-1 and VA IIR 10-176-3). The Health and Retirement Study is funded by the National Institute on Aging (U01 AG09740) and performed at the Institute for Social Research, University of Michigan.
Conflicts of Interest
The authors declare that they do not have any conflicts of interest.
REFERENCES
- 1.Marcus SC, Olfson M. National Trends in the Treatment for Depression From 1998 to 2007. Arch Gen Psychiatry. 2010;67(12):1265–73. doi: 10.1001/archgenpsychiatry.2010.151. [DOI] [PubMed] [Google Scholar]
- 2.Akincigil A, Olfson M, Walkup JT, Siegel MJ, Kalay E, Amin S, et al. Diagnosis and treatment of depression in older community-dwelling adults: 1992–2005. Journal of the American Geriatric Society. 2011;59(6):1042–51. doi: 10.1111/j.1532-5415.2011.03447.x. [DOI] [PubMed] [Google Scholar]
- 3.Mulsant BH, Ganguli M. Epidemiology and diagnosis of depression in late life. Journal of Clinical Psychiatry. 1999;60:9–15. doi: 10.4088/JCP.v60n0104. [DOI] [PubMed] [Google Scholar]
- 4.Department of Health and Human Services, Administration on Aging. Older adults and mental health issues and opportunities: Department of Health and Human Services, Administration on Aging2001.
- 5.Alexopoulos GS, Borson S, Cuthbert BN, Devanand DP, Mulsant BH, Olin JT, et al. Assessment of late life depression. Biol Psychiatry. 2002;52(3):164–74. doi: 10.1016/S0006-3223(02)01381-1. [DOI] [PubMed] [Google Scholar]
- 6.Blazer D, Burchett B, Service C, George LK. The association of age and depression among the elderly: an epidemiologic exploration. J Gerontol. 1991;46(6):M210–5. doi: 10.1093/geronj/46.6.M210. [DOI] [PubMed] [Google Scholar]
- 7.Anstey KJ, von Sanden C, Sargent-Cox K, Luszcz MA. Prevalence and risk factors for depression in a longitudinal, population-based study including individuals in the community and residential care. American Journal of Geriatric Psychiatry. 2007;15(6):497–505. doi: 10.1097/JGP.0b013e31802e21d8. [DOI] [PubMed] [Google Scholar]
- 8.Beekman AT, Geerlings SW, Deeg DJ, Smit JH, Schoevers RS, de Beurs E, et al. The natural history of late-life depression: a 6-year prospective study in the community. Arch Gen Psychiatry. 2002;59(7):605–11. doi: 10.1001/archpsyc.59.7.605. [DOI] [PubMed] [Google Scholar]
- 9.Chen L, Eaton WW, Gallo JJ, Nestadt G. Understanding the heterogeneity of depression through the triad of symptoms, course and risk factors: a longitudinal, population-based study. J Affect Disord. 2000;59(1):1–11. doi: 10.1016/S0165-0327(99)00132-9. [DOI] [PubMed] [Google Scholar]
- 10.Fiske A, Gatz M, Pedersen NL. Depressive symptoms and aging: The effects of illness and non-health-related events. Journals of Gerontology Series B-Psychological Sciences and Social Sciences. 2003;58(6):P320–P8. doi: 10.1093/geronb/58.6.P320. [DOI] [PubMed] [Google Scholar]
- 11.Weissman MM, Bland RC, Canino GJ, Faravelli C, Greenwald S, Hwu H-G, et al. Cross-National Epidemiology of Major Depression and Bipolar Disorder. JAMA. 1996;276(4):293–9. doi: 10.1001/jama.1996.03540040037030. [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 13.Mattisson C, Bogren M, Horstmann V, Tambs K, Munk-Jorgensen P, Nettelbladt P. Risk factors for depressive disorders in the Lundby cohort - A 50 year prospective clinical follow-up. J Affect Disord. 2009;113(3):203–15. doi: 10.1016/j.jad.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 14.Katz MM, Secunda SK, Hirschfeld RMA, Koslow SH. Nimh Clinical Research Branch Collaborative Program on the Psychobiology of Depression. Arch Gen Psychiatry. 1979;36(7):765–71. doi: 10.1001/archpsyc.1979.01780070043004. [DOI] [PubMed] [Google Scholar]
- 15.Murphy JM, Laird NM, Monson RR, Sobol AM, Leighton AH. A 40-year perspective on the prevalence of depression: the Stirling County Study. Arch Gen Psychiatry. 2000;57(3):209–15. doi: 10.1001/archpsyc.57.3.209. [DOI] [PubMed] [Google Scholar]
- 16.Juster FT, Suzman R. An Overview of the Health and Retirement Study. J Hum Resour. 1995;30(Supplement):S7–S56. doi: 10.2307/146277. [DOI] [Google Scholar]
- 17.Sample Sizes and Response Rates. Ann Arbor, MI: University of Michigan; 2011. [Google Scholar]
- 18.Ofstedal MB, Weir DR, Kuang-Tsung C, Wagner J. Updates to HRS Sample Weights. Ann Arbor, MI: University of Michigan; 2011. [Google Scholar]
- 19.Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics. 1999;11(2):139–48. doi: 10.1017/S1041610299005694. [DOI] [PubMed] [Google Scholar]
- 20.Steffick DE. Documentation of Affective Functioning Measures in the Health and Retirement Study. Ann Arbor, MI: University of Michigan; 2000. [Google Scholar]
- 21.Mojtabai R, Olfson M. Major depression in community-dwelling middle-aged and older adults: prevalence and 2- and 4-year follow-up symptoms. Psychol Med. 2004;34(4):623–34. doi: 10.1017/S0033291703001764. [DOI] [PubMed] [Google Scholar]
- 22.Steffick DE, Wallace RB, Herzog AR, Ofstedal MB, Fonda S, Langa K. Documentation of Affective Functioning Measures in the Health and Retirement Study. Ann Arbor, MI: HRS Health Working Group, Survey Research Center, University of Michigan; 2000. [Google Scholar]
- 23.Han B. Depressive symptoms and self-rated health in community-dwelling older adults: a longitudinal study. J Am Geriatr Soc. 2002;50(9):1549–56. doi: 10.1046/j.1532-5415.2002.50411.x. [DOI] [PubMed] [Google Scholar]
- 24.Turvey CL, Schultz SK, Beglinger L, Klein DM. A Longitudinal Community-Based Study of Chronic Illness, Cognitive and Physical Function, and Depression. American Journal of Geriatric Psychiatry. 2009;17(8):632–41. doi: 10.1097/JGP.0b013e31819c498c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aneshensel CS, Frerichs RR, Clark VA, Yokopenic PA. Measuring depression in the community: a comparison of telephone and personal interviews. Public Opinion Quarterly. 1982;46(1):110–21. doi: 10.1086/268703. [DOI] [PubMed] [Google Scholar]
- 26.Kleinman LC, Norton EC. What's the Risk? A Simple Approach for Estimating Adjusted Risk Measures from Nonlinear Models Including Logistic Regression. Heal Serv Res. 2009;44(1):288–302. doi: 10.1111/j.1475-6773.2008.00900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pfeiffer PN, Glass J, Austin K, Valenstein M, McCarthy JF, Zivin K. Impact of Distance and Facility of Initial Diagnosis on Depression Treatment. Health Services Research. 2011; Early View. doi:10.1111/j.1475-6773.2010.01228.x [DOI] [PMC free article] [PubMed]
- 28.Zivin K, Campbell DG, Lanto AB, Chaney EF, Bolkan C, Bonner LM, et al. Relationships between mood and employment over time among depressed VA primary care patients. General Hospital Psychiatry. 2012;34(5):468–77. doi: 10.1016/j.genhosppsych.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 29.Heeringa S, Connor JH. Technical Description of the Health and Retirement Survey Sample Design. Ann Arbor, MI: University of Michigan, Institute for Social Research; 1995. [Google Scholar]
- 30.Weissman MM, Wickramaratne P, Greenwald S, Hsu HY, Ouellette R, Robins LN, et al. The Changing Rate of Major Depression - Cross-National Comparisons. Jama-Journal of the American Medical Association. 1992;268(21):3098–105. doi: 10.1001/jama.1992.03490210080039. [DOI] [PubMed] [Google Scholar]
- 31.Compton WM, Conway KP, Stinson FS, Grant BF. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991-1992 and 2001–2002. Am J Psychiatry. 2006;163(12):2141–7. doi: 10.1176/appi.ajp.163.12.2141. [DOI] [PubMed] [Google Scholar]
- 32.Jorm AF. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychol Med. 2000;30(1):11–22. doi: 10.1017/S0033291799001452. [DOI] [PubMed] [Google Scholar]
- 33.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 34.Fombonne E. Increased Rates of Depression - Update of Epidemiologic Findings and Analytical Problems. Acta Psychiatr Scand. 1994;90(3):145–56. doi: 10.1111/j.1600-0447.1994.tb01571.x. [DOI] [PubMed] [Google Scholar]
- 35.Lebowitz BD, Pearson JL, Schneider LS, Reynolds CF, 3rd, Alexopoulos GS, Bruce ML, et al. Diagnosis and treatment of depression in late life. Consensus statement update. JAMA. 1997;278(14):1186–90. doi: 10.1001/jama.1997.03550140078045. [DOI] [PubMed] [Google Scholar]
- 36.Black SA, Markides KS, Miller TQ. Correlates of depressive symptomatology among older community-dwelling Mexican Americans: the Hispanic EPESE. The journals of gerontology. Series B, Psychological sciences and social sciences. 1998;53(4):S198–208. doi: 10.1093/geronb/53B.4.S198. [DOI] [PubMed] [Google Scholar]
- 37.Lang I, Wallace RB, Huppert FA, Melzer D. Moderate alcohol consumption in older adults is associated with better cognition and well-being than abstinence. Age and Ageing. 2007;36(3):256–61. doi: 10.1093/ageing/afm001. [DOI] [PubMed] [Google Scholar]
- 38.Doshi JA, Cen L, Polsky D. Depression and retirement in late middle-aged U.S. workers. Heal Serv Res. 2008;43(2):693–713. doi: 10.1111/j.1475-6773.2007.00782.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Karpansalo M, Kauhanen J, Lakka TA, Manninen P, Kaplan GA, Salonen JT. Depression and early retirement: prospective population based study in middle aged men. Journal of Epidemiology and Community Health. 2005;59(1):70–4. doi: 10.1136/jech.2003.010702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Butterworth P, Gill SC, Rodgers B, Anstey KJ, Villamil E, Melzer D. Retirement and mental health: analysis of the Australian national survey of mental health and well-being. Social Science and Medicine. 2006;62(5):1179–91. doi: 10.1016/j.socscimed.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 41.Buxton JW, Singleton N, Melzer D. The mental health of early retirees– national interview survey in Britain. Social Psychiatry and Psychiatric Epidemiology. 2005;40(2):99–105. doi: 10.1007/s00127-005-0866-5. [DOI] [PubMed] [Google Scholar]
- 42.Charles KK. Is retirement depressing - labor force inactivity and psychological well-being in later life. Cambridge, MA: National Bureau of Economic Research2002 July. Report No.: 9033.
- 43.Drentea P. Retirement and mental health. Journal of Aging and Health. 2002;14(2):167–94. doi: 10.1177/089826430201400201. [DOI] [PubMed] [Google Scholar]