Abstract
Introduction
Self-medication can contribute to the inappropriate use of antibiotics in respiratory tract infections (RTI). This phenomenon has not been well described, particularly in Poland. The aim of our study was to describe the prevalence of antibiotic self-medication for RTI, to explore factors influencing antibiotic use without prescription, and to determine the available sources of such antibiotics.
Material and methods
A self-administered questionnaire completed by patients presenting to family medicine clinics at Lodz and Wroclaw from 1st March to 15th May 2010.
Results
A total of 891 patients in ten clinics completed the survey (response rate, 89.1%). Overall, 41.4% (n = 369) of patients reported self-medication with an antibiotic for RTI. The most common reason for antibiotic self-medication was a belief that antibiotics treat the majority of infections, including influenza and influenza-like illnesses (43.9%; n = 162). The predominant sources of antibiotics for self-medication were antibiotics from previous prescriptions stored by the patient at home (73.7%, n = 272), those received from a pharmacy without prescription (13.5%; n = 50), or from family members and friends (12.7%; n = 47).
Conclusions
Antibiotic self-medication for RTI was common in this population. This may be due to the belief that the antibiotics treat the majority of infections. A recommendation to either ask patients to return unused antibiotics to the physician's office or to dispense antibiotics in the exact amount which is necessary for an individual course, as well as the targeted education of pharmacy personnel and the general population, appear to be justified.
Keywords: antibiotics, self-treatment, respiratory tract infections, available sources of antibiotics
Introduction
The increase in resistance to antimicrobial drugs represents an important clinical and social problem [1, 2]. Many patients presenting to family medicine clinics have already started self-medication with antimicrobial agents [3]. Self-medication, defined as the administration of a therapeutic agent without a physician's prescription, can contribute to the inappropriate use of antibiotics without clinical indication. The most common reasons for self-medication in Europe are ‘sore throat’ and bronchitis [4, 5].
Symptoms of the common cold usually resolve within 7 to 10 days (with some symptoms possibly lasting for up to 3 weeks) without treatment [6, 7]. Nevertheless, coryzal symptoms, cough or fever may prompt patients to make therapeutic decisions without a consultation with a health care professional [3]. Self-medication is related to the overuse of antimicrobial drugs [8, 9].
Due to possible complications as well as growing bacterial resistance, antimicrobial therapy should be used only upon a physician's recommendation [10, 11] and if feasible following microbiology tests, particularly when streptococcal pharyngitis is suspected [12, 13]. Previous studies have revealed that self-medication with antibiotics is commonly encountered both in the United States (US) and in Europe, predominantly in cases of common cold and upper respiratory tract infections [4, 14]. Using unnecessary or inappropriate antibiotics can cause adverse effects, and lead to increasing numbers of drug-resistant microorganisms [15]. An estimated 142,505 visits were made each year to US emergency departments for drug-related adverse events attributable to systemic antibiotics. Antibiotics were responsible for 19.3% of all emergency department visits for drug-related adverse events, particularly allergic reactions [16]. The prevalence of self-medication is high in eastern and southern Europe and low in northern and western Europe [4, 5, 17].
The aim of our study was to describe the prevalence of antibiotic self-medication for respiratory tract infections, to explore factors influencing antibiotic use without prescription, and to determine the available sources of such antibiotics.
Material and methods
The study included data from 891 adults (304 men/587 women) presenting to 5 family medicine clinics in Lodz and 5 in Wroclaw and surroundings between 1st March and 15th May 2010. All physicians collaborated with vocational training units locally. Nurses asked each consecutive patient presenting to family physicians’ office and able to give their voluntary informed consent to fill in an anonymous questionnaire and return it to the collection box; 100 study questionnaires were distributed per clinic. The questionnaire included 8 questions relating to demographic characteristics, self-treatment methods for managing infections, patterns of taking antibiotics and available sources of antibiotics without a physician's prescription.
Statistical analysis
Data are shown as number (n) and proportion (%). A χ2 test was used to evaluate the statistical significance between the particular subgroups. Statistical analysis was performed using SPSS statistical package (SPSS 16.0, Chicago, USA).
Results
Out of 891 study questionnaires, 616 (69.1%) were obtained from participants from urban areas (including 436 [70.8%] from Lodz, and 180 [29.2%] from Wroclaw), and 275 (30.9%) from rural areas (in the vicinity of Wroclaw). The majority of respondents (28.6%; n = 255) were 30-45 years old (including 24.8%; n = 153 urban, vs. 37.1%; n = 102 rural) or 46-60 years old (35.4%; n = 315) (including 36.9%; n = 227 urban, vs. 32.0%; n = 88 rural). The age group of 18-29 years old was smaller (18.3%; n = 163) (including 17.4%; n = 107 vs. 20.4%; n = 56 urban participants vs. rural, respectively). The age group above 60 years old (17.7%; n = 158) was the smallest (including 20.9%; n = 129 vs. 10.5%; n = 29 urban patients vs. rural, respectively). Female participants predominated both in the urban and rural groups (64.4%; n = 397 vs. 69.1%; n = 190, respectively).
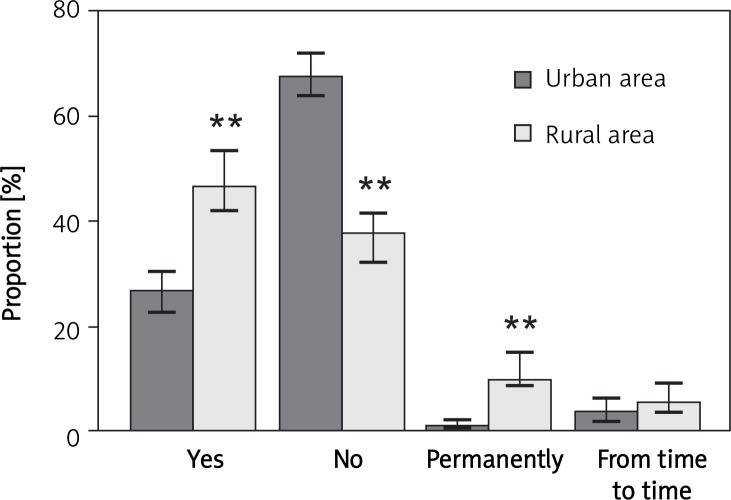
A total of 369 participants (41.4%) reported taking antibiotics without consulting a physician. This was more common in rural areas, at 171 (62.2%) of 275 respondents in comparison to 198 (32.1%) of 616 from urban areas (p < 0.001; Figure 1). In both groups, the great majority of respondents acquired this antibiotic as tablets left over from previously used packs kept in their home medical kits, or, less often, from friends and family members. In addition, respondents from rural areas more frequently purchased antibiotics from a pharmacy without a prescription (Table I). The majority of persons who used antibiotics without consulting a physician agreed that the antibiotics were not effective against all respiratory tract infections. However, as many as 43.9% (n = 162) of respondents from this group believed that antibiotics were effective in the treatment of influenza and influenza-like illnesses. Conversely, the majority of 522 persons who reported not taking antibiotics without a physicians’ recommendation believed that the antibiotics were not effective either in the treatment of influenza or other infections. In addition, a significantly higher percentage of participants in this group believed that the physician should prescribe antibiotics only if there was a medical need for such a decision (Table II).
Figure 1.
Patients’ answers to the question “Have you ever taken antibiotics without your physician's recommendation?”
Data presented as percentage of answers related to populations of patients from urban (n = 616) and rural (n = 275) areas. Error bars represent 95% confidence interval (CI). RTI – respiratory tract infections; **p < 0.001 vs. urban area
Table I.
Sources of antibiotics used without a physician's prescription
| Urban area, n (%) | Rural area, n (%) | |
|---|---|---|
| Home | 162 (83.1) | 110 (62.1)# |
| From family/friends | 22 (11.3) | 25 (14.1) |
| From a pharmacy without a prescription | 8 (4.1) | 42 (23.7)# |
| Other | 3 (1.5) | 0 (0) |
p < 0.0001
Table II.
Patients’ age and opinion about prescribing and effectiveness of antibiotic therapy
| Self-treatment with antibiotics n (%) | Treatment with antibiotics with GP's recommendation n (%) | |
|---|---|---|
| Age [years] | ||
| 18-29 | 58 (35.6) | 105 (64.4) |
| 30-45 | 125 (49.0) | 130 (51.0) |
| 46-60 | 143 (45.4) | 172 (54.6) |
| > 60 | 43 (27.2) | 115 (72.8) |
| Does your family physician prescribe antibiotics...? | ||
| When needed | 243 (65.3) | 442 (87.4)# |
| Too often | 40 (10.8) | 34 (6.7)* |
| Too seldom | 42 (11.3) | 20 (4.0)# |
| When asked | 47 (12.6) | 10 (2.0)# |
| Are antibiotics effective against flu and flu-like diseases? | ||
| Yes | 162 (43.9) | 170 (32.6)** |
| No | 125 (33.9) | 203 (38.9) |
| I don't know/other | 82 (22.2) | 149 (28.5) |
| Are antibiotics effective against all infections? | ||
| Yes | 110 (29.8) | 61 (11.7)# |
| No | 154 (41.7) | 277 (53.1)** |
| I don't know/other | 105 (28.5) | 184 (35.2) |
p < 0.05
p < 0.001
p < 0.0001
Discussion
In Poland, antibiotics are prescribed very often for respiratory tract infections. Previous studies have revealed that in Lodz, approximately 72% of adult patients who presented with symptoms typical for a lower respiratory tract infection received an antibiotic [18, 19]. Even more frequent use of antibiotics for acute RTI has been reported in south-eastern Poland, including some rural areas [20, 21].
Data from our study confirmed frequent use of antibiotics without a physician's recommendation, especially in the rural environment. This latter finding may be related to a lower level of education in the rural population of Poland, a factor that has been associated with more frequent antibiotic self-medication [17].
Our findings differ from those of a recent multicenter European study, in which no difference was noted in the use of antibiotics without a physician's consultation between inhabitants of urban and rural areas [4]. In contrast, the results of a study from Lithuania indicated that the use of antibiotics without a prescription was 1.61-fold more frequent in rural than urban populations [9]. Published medical research on this topic relates mostly to the general population. According to a Spanish survey, 41% of participants had taken antibiotics (over the past 6 months) which had been acquired from a pharmacy without a physician's prescription [22]. Also, the findings of a US study indicated that the main source of self-medication with antibiotics were antibiotics kept at home, which were subsequently used by as many as 17% of patients [14]. In the population of Malta, as many as 19% of persons reported self-treatment with antibiotics [23]. In contrast, according to data from the northern part of Israel, almost 25% of survey respondents kept antibiotics at home, but only 17% would use them without a physician's consultation [24]. In our study we found that 4.1% of respondents from urban areas acquired their antibiotics from a pharmacy without a prescription, while as many as 23.7% of rural inhabitants did so (while in a Spanish study, conducted in a general population, about 32.1% of participants did so) [25].
It should be emphasized that the respondents’ knowledge about antibiotic therapy use was incomplete. Similarly, the results of a European survey [26] indicated that as many as 53% of respondents gave an incorrect answer to the question ‘do antibiotics kill viruses?’, and 47% of them expressed the opinion that antibiotics were effective against cold and flu. In our study, 43.9% of patients who used antibiotics without a physician's recommendation believed that antibiotics treated influenza and influenza-like infections. Data from our study and most other surveys indicate the need for conducting further studies in this field, as well as for educating patients about adverse effects and harmful consequences of inappropriately applied antimicrobial therapy.
In conclusion, many patients use antibiotic self-medication for RTI. This may be due to the common belief that antibiotics treat the majority of infections. A recommendation to either ask patients to return unused antibiotics to the physician's office or to dispense antibiotics in the exact amount which is necessary for an individual course, as well as the targeted education of pharmacy personnel and the general population, appear to be justified.
Acknowledgments
The authors wish to thank the family physicians and their teams involved in data collection and Dr. Andrew Stewardson for reviewing the manuscript.
References
- 1.Lipsitch M, Samore MH. Antimicrobial use and antimicrobial resistance: a population perspective. Emerg Infect Dis. 2002;8:347–54. doi: 10.3201/eid0804.010312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harbarth S, Samore MH. Antimicrobial resistance determinants and future control. Emerg Infect Dis. 2005;11:794–801. doi: 10.3201/eid1106.050167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vanden Eng J, Marcus R, Hadler JL, et al. Consumer attitudes and use of antibiotics. Emerg Infect Dis. 2003;9:1128–35. doi: 10.3201/eid0909.020591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grigoryan L, Haaijer-Ruskamp FM, Burgerhof JG, et al. Self-medication with antimicrobial drugs in Europe. Emerg Infect Dis. 2006;12:452–9. doi: 10.3201/eid1203.050992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grigoryan L, Burgerhof JG, Degener JE, et al. Determinants of self-medication with antibiotics in Europe: the impact of beliefs, country wealth and the healthcare system. J Antimicrob Chemother. 2008;61:1172–9. doi: 10.1093/jac/dkn054. [DOI] [PubMed] [Google Scholar]
- 6.Gwaltney JM, Jr, Hendley JO, Simon G, Jordan WS., Jr Rhinovirus infections in an industrial population. II. Characteristics of illness and antibody response. JAMA. 1967;202:494–500. [PubMed] [Google Scholar]
- 7.Gwaltney JM. The common cold. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practices of infectious diseases. 5th ed. New York: Churchill Livingstone; 2000. pp. 651–6. [Google Scholar]
- 8.Al-Bakri AG, Bustanji Y, Yousef AM. Community consumption of antibacterial drugs within the Jordanian population: sources, patterns and appropriateness. Int J Antimicrob Agents. 2005;26:389–95. doi: 10.1016/j.ijantimicag.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 9.Berzanskyte A, Valinteliene R, Haaijer-Ruskamp FM, Gurevicius R, Grigoryan L. Self-medication with antibiotics in Lithuania. Int J Occup Med Environ Health. 2006;19:246–53. doi: 10.2478/v10001-006-0030-9. [DOI] [PubMed] [Google Scholar]
- 10.Thomas JK, Forrest A, Bhavnani SM, et al. Pharmacodynamic evaluation of factors associated with the development of bacterial resistance in acutely ill patients during therapy. Antimicrob Agents Chemother. 1998;42:521–7. doi: 10.1128/aac.42.3.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of beta-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998;279:365–70. doi: 10.1001/jama.279.5.365. [DOI] [PubMed] [Google Scholar]
- 12.Chiappini E, Regoli M, Bonsignori F, et al. Analysis of different recommendations from international guidelines for the management of acute pharyngitis in adults and children. Clin Ther. 2011;33:48–58. doi: 10.1016/j.clinthera.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 13.Hryniewicz W, Ozorowski T, Radzikowski A. Warsaw, Poland: National Medicines Institute; Recommendations for Management of Community-Acquired Respiratory Tract Infections-2010. http://www.antybiotyki.edu.pl/pdf/RekomendacjeA42009.pdf. [Google Scholar]
- 14.Richman PB, Garra G, Eskin B, Nashed AH, Cody R. Oral antibiotic use without consulting a physician: a survey of ED patients. Am J Emerg Med. 2001;19:57–60. doi: 10.1053/ajem.2001.20035. [DOI] [PubMed] [Google Scholar]
- 15.Gleckman RA, Czachor JS. Antibiotic side effects. Semin Respir Crit Care Med. 2000;21:53–60. doi: 10.1055/s-2000-9928. [DOI] [PubMed] [Google Scholar]
- 16.Shehab N, Patel PR, Srinivasan A, Budnitz DS. Emergency department visits for antibiotic-associated adverse events. Clin Infect Dis. 2008;47:735–43. doi: 10.1086/591126. [DOI] [PubMed] [Google Scholar]
- 17.Grigoryan L, Burgerhof JG, Haaijer-Ruskamp FM, et al. Is self-medication with antibiotics in Europe driven by prescribed use? J Antimicrob Chemother. 2007;59:152–6. doi: 10.1093/jac/dkl457. [DOI] [PubMed] [Google Scholar]
- 18.Godycki-Cwirko M, Hood K, Nocun M, Muras M, Goossens H, Butler CC. Presentation, antibiotic management and associated outcome in Polish adults presenting with acute cough/LRTI. Fam Pract. 2011;28:608–14. doi: 10.1093/fampra/cmr019. [DOI] [PubMed] [Google Scholar]
- 19.Butler CC, Hood K, Verheij T, et al. Variation in antibiotic prescribing and its impact on recovery in patients with acute cough in primary care: prospective study in 13 countries. BMJ. 2009;338:b2242. doi: 10.1136/bmj.b2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Panasiuk L, Lukas W, Paprzycki P. Empirical first-line antibioticotherapy in adult rural patients with acute respiratory tract infections. Ann Agric Environ Med. 2007;14:305–11. [PubMed] [Google Scholar]
- 21.Panasiuk L, Lukas W, Paprzycki P, Verheij T, Godycki-Ćwirko M, Chlabicz S. Antibiotics in the treatment of upper respiratory tract infections in Poland. Is there any improvement? J Clin Pharm Ther. 2010;35:665–9. doi: 10.1111/j.1365-2710.2009.01136.x. [DOI] [PubMed] [Google Scholar]
- 22.Väänänen MH, Pietilä K, Airaksinen M. Self-medication with antibiotics – does it really happen in Europe? Health Policy. 2006;77:166–71. doi: 10.1016/j.healthpol.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Borg MA, Scicluna EA. Over-the-counter acquisition of antibiotics in the Maltese general population. Int J Antimicrob Agents. 2002;20:253–7. doi: 10.1016/s0924-8579(02)00194-2. [DOI] [PubMed] [Google Scholar]
- 24.Raz R, Edelstein H, Grigoryan L, Haaijer-Ruskamp FM. Self-medication with antibiotics by a population in northern Israel. Isr Med Assoc J. 2005;7:722–5. [PubMed] [Google Scholar]
- 25.Orero González A, Ripoll Lozano MA, González Núñez J. Analysis of automedication with antibiotics in Spain [Spain] Enferm Infecc Microbiol Clin. 1998;16:328–33. [PubMed] [Google Scholar]
- 26.Special Eurobarometer 338. Antimicrobial Resistance. http://ec.europa.eu/health/antimicrobial_resistance/docs/ebs_338_en.pdf.