Abstract
Introduction
Over recent years, the popularity of videogames has gone beyond youth and gamers and is slowly entering the field of professional healthcare. Exergames are an attractive alternative to physical therapy. The primary aim of this pilot study was to explore the user experience (usability, satisfaction, level of motivation, and game experience) of the patient with the “PlayMancer” exergame. The secondary aim was to explore the progression of the performed motor skills (walking velocity, overhead reach ability, and cervical range of motion) and the clinical changes (to physical condition, disability, and pain intensity) in a group of patients with chronic musculoskeletal pain using an exergame for 4 weeks.
Materials and Methods
In the European PlayMancer project, an exergame for physical rehabilitation of chronic pain patients was developed. This exergame is controlled by relevant motions of the patient's body captured by a motion suit and several infrared cameras. In three different integrated minigames, the patient can train the following motor skills: Walking velocity, overhead reaching, and neck mobility.
Results
Ten patients participated in this study and completed the 4 weeks of gaming. Patients rated the usability of the exergames as good (score of 78.5 [standard deviation 9.7; range, 60.0–97.5]) on the System Usability Scale, and the game motivated all patients to perform their exercises. Patients enjoyed playing and were pleased with both the game environment and the game play. Overall, the patients made a progression in the examined motor skills during the minigames over the 4 weeks of gaming.
Conclusions
The “PlayMancer” exergame is a potential tool for achieving physical rehabilitation because it motivates patients to perform their exercises and as a result increases their motor skills and physical condition.
Introduction
The growing popularity of videogames is not limited to youth and gamers but has also entered the field of healthcare and physical rehabilitation.1 Serious games have been developed to be played to exercise and train specific motor skills. These are known as exergames and are an attractive alternative to conventional face-to-face physical therapy.2,3 The use of games in rehabilitation is believed to improve patients' motivation because the challenging game environment is considered to be both motivating4 and distracting.5 This is especially necessary in physical rehabilitation, where patients are required to follow training protocols that are generally perceived as boring because of the high degree of repetition. Therefore, attractive games have the potential to increase the compliance with physical rehabilitation protocols. Furthermore, games challenge patients to play repeatedly to beat their personal best score and thereby increase their treatment intensity. The repetitive nature of games is thought to be a key mechanism in promoting motor skills learning in exergames and has the potential to positively influence physical performance6,7 in patients, especially those with significant physical impairments.5
Although promising, commercial exergames are designed primarily for entertainment, not specifically to train impaired patients in a professional rehabilitation setting.8 Practice shows there are several limitations when introducing existing commercial exergames into professional rehabilitation settings. First, commercial exergames are developed for the general public, and the norms are matched to the performance of generally healthy gamers. In most cases, it is not possible to change these norms and to personalize the game for an impaired patient. As a result, the game becomes too hard to play, which can lead to frustration. Second, the level of energy expenditure reported for commercial exergames cannot be compared with levels of energy expenditure typically achieved during physical therapy,6,7 and the requested motor skills are too general and not sufficiently pathology-specific. Third, the game output of commercial exergames focuses on the game performance—for example, time or a high score—and not the patient's performance on motor skills. Therefore, the physiotherapist cannot monitor the progression of the patient in terms of the performed motor skills.
In the PlayMancer project (FP7-ICT-215839-2007),9 an exergame (the “PlayMancer” game) for physical rehabilitation for patients suffering from chronic pain was developed by clinical and technical professionals working closely together. The design and technical characteristics of the “PlayMancer” exergame have been described before.10,11 The overall aim of the game is to improve the patient's physical condition. This exergame is controlled by relevant motions of the patient's body. These motions are captured by a motion suit and several infrared cameras and by recording muscle activation levels. Before starting the exergame, the difficulty level of the game is matched to the ability level of the individual patient, and individual goals are configured to motivate a progression in terms of the performed motor skills.
The progression of the patient can also be monitored by a therapist. In three different minigames, the patient can train the following motor skills: Walking velocity, overhead reaching, and neck mobility. This choice of motor skills is not arbitrary. Previous studies have shown that patients with chronic low back pain have lower preferred walking velocity compared with controls12 and that their physical activity deteriorates because of a lack of use and deconditioning.13 By walking, chronic low back pain patients can improve their physical condition and increase their walking velocity. Furthermore, patients with neck/shoulder pain have a reduced ability to reach overhead due to their pain.14 Besides, patients with neck/shoulder pain demonstrate a decreased range of motion compared with asymptomatic controls15,16 and benefit from increasing their neck mobility by exercising.
This study is believed to be the first evaluation of a serious exergame for patients suffering from chronic pain and concerns a stage 1–2 evaluation, according to the staged approach of telemedicine evaluation proposed by DeChant et al.17 The primary aim of this pilot study was to explore the user experience—in terms of usability, satisfaction, level of motivation, and game experience—of patients playing the “PlayMancer” exergame. The secondary aim of this pilot study was to explore the progression in terms of the performed motor skills (walking velocity, overhead reach ability, and cervical range of motion [CROM]) and the clinical changes (physical condition, level of disability, and pain intensity) brought about in chronic musculoskeletal pain patients playing the “PlayMancer” exergame over 4 successive weeks.
Materials and Methods
Study design and subjects
Patients were recruited from a local physical therapy practice and by an advertisement in the newsletter of a patient association for chronic pain patients. Interested patients could contact the researcher and received an information letter concerning the study. Only those patients 18 years and older and with low back pain or pain in the neck/shoulder region for at least 12 weeks (without specific pathological causes) were included. Patients were excluded if they (1) had an insufficient understanding of the Dutch language, (2) had visible impairment that inhibits the perception of the screen on which the game is projected, or (3) were receiving (physical) therapy for their physical complaint at the time of the study. Because of the explorative character of this study no sample size calculation has been conducted beforehand. To be able to answer the objectives of this study, the goal is to include at least 10 patients. The medical ethical committee approved the study. All patients gave their informed consent prior to participation.
The “PlayMancer” exergame
In this game, the patient embarks on a quest to investigate a newly discovered island. After a first inspection, it seems that the island has been previously inhabited. To find out more about the former inhabitants of this island, the player has to play a series of minigames. By playing these minigames, artifacts can be collected. Artifacts represent points, and these, at fixed quantities, unlocked new information about the island's former civilization. Figure 1 gives a view of the “PlayMancer” exergame, which consists of three minigames:
“Temple of Magupta.” In this minigame, the patient has to control an avatar, who is walking through a collapsing tunnel. On the way, certain artifacts can be found and collected, while falling debris has to be avoided. Lateral movement of the avatar is controlled by the patient's speech, while the patient's voluntary walking velocity on a treadmill controls forward movement of the avatar. The underlying goal of this minigame is to improve walking velocity and thereby the overall physical conditions of the patients.
“Face of Cronos.” In this minigame, the avatar is climbing a rock face. To help the avatar climb the rock wall, the patient has to reach overhead for a virtual handgrip. Once that goal is reached, the avatar climbs the face. An artifact is earned as a reward for every successful overhead reach. Additionally, the patient receives real-time feedback about the muscle tension in both trapezius muscles. The patient is instructed to relax as quickly and as much as possible in between movements, in order to gain consciousness about his or her muscle tension. The underlying goal of this minigame is to improve overhead reaching ability.
“Three Wind Gods.” In this minigame, the patient has to reproduce sequences of head movements that are shown by three characters. These movements, corresponding to the characters, are flexion–extension, rotation, and lateral flexion–extension of the neck. For every successful reproduction of a movement, an artifact is earned as a reward. The overall goal of this minigame is to improve the patient's neck mobility.
FIG. 1.
A view of the “PlayMancer” game. Color images available online at www.liebertonline.com/g4h
Game input
Relevant motions of the patient's body and muscle activation levels control the “PlayMancer” exergame. The motion capture (MoCap) system10 consists of a tight-fitting suit (a jacket, a pair of trousers, and a cap) with 36 reflective markers attached to it, to track the patients' movements while playing (Fig. 2), and eight infrared cameras (IOtracker),18 positioned at every top and bottom corner of the lab. Easy-to-put-on suits were available for male and female patients and in various sizes (small, medium, large, and extra large). The suits were washable. At the start of the treatment a clean suit was provided to every patient; on the patient's request the suit was washed during the treatment period. Furthermore, surface electromyography electrodes are placed on both left and right upper trapezius muscles, on the halfway point of the line between the spinous process of C7 and the acromion. A reference electrode is placed over the spinous process of C7,19 and the signal is sent to a computer wirelessly.
FIG. 2.
The “PlayMancer” suit. Color images available online at www.liebertonline.com/g4h
Treatment protocol
The patients were asked to visit the Roessingh Research and Development lab (Enschede, The Netherlands) and to play the “PlayMancer” exergame for 4weeks with a (average) frequency of one or two times a week. After 4 weeks of training with this frequency, first clinical changes can be expected. In addition, this amount of sessions is expected to enable patients to give a good reliable judgment concerning their experience.
During every game session, a therapist assisted the patient. The first gaming session was focused on the calibration of the MoCap system and to assist the patient become acquainted with the “PlayMancer” game. Subsequently, by using the baseline and goal-setting module, the individual baseline values were assessed, and individual goals were configured for each motor skill. This module also automatically updates the baseline values of the patient if the patient performs at beyond the baseline level. Then the patient was introduced to the minigames, and the aim of every minigame was explained. During subsequent sessions, the patients played every minigame at least three times. Depending on the primary complaint (low back or neck/shoulder pain) or patient's preference, a minigame might be played more than three times. Each gaming session lasted between 45 and 60 minutes.
Measurements
User experience
ISO 9241-210 defines user experience as “a person's perceptions and responses that result from the use or anticipated use of a product, system or service.” To assess the user experience of the game, there was a focus on usability, satisfaction, level of motivation, and gaming experience. The usability of the game was assessed against the System Usability Scale (SUS).20 The SUS presented 10 statements about the perceived usability of the game. Patients could indicate on a scale of 0–4 to what extent the presented statements were true for them. To obtain the final SUS score, the sum of the patients' answers was multiplied by 2.5. The SUS score ranges from 0 to 100 (low and high usability, respectively). The English version of the SUS was translated into Dutch, as there was no validated Dutch version available.
The overall satisfaction with the game was assessed by a request to rate the game on a scale from 0 to 10 (low and high usability, respectively) and an open-ended question asking about the overall experience of the game.
The level of motivation was assessed by posing two questions. For the first question, patients rated on a 7-point Likert scale, ranging from “demotivating” to “motivating,” their level of motivation related to the “PlayMancer” game. The second question was answered with yes or no: “Did the 'PlayMancer' game motivate you to perform your exercises?”
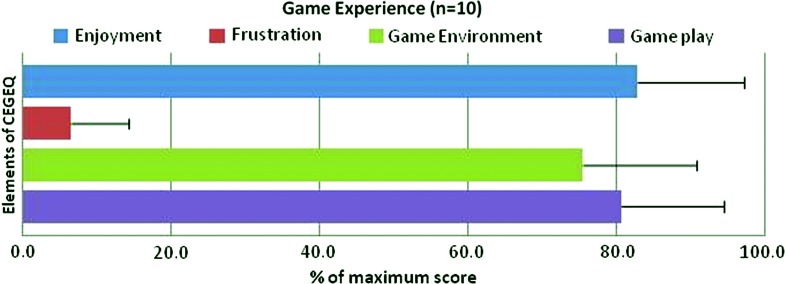
The game experience of the patients during gaming was assessed by the enjoyment, frustration, environment (graphics and sounds), and game play (scenario and rules) scale of the Core Elements of Gaming Experience Questionnaire (CEGEQ).21 This questionnaire presents 17 statements. Patients could indicate on a scale ranging from 0 to 7 to what extent these statements were true for them. The summed score per category gave a view of each patient's overall gaming experience. The English version of the CEGEQ was translated into Dutch, as there was no validated Dutch version available. All the questionnaires were assessed immediately after 4 weeks of gaming (post-test).
Game output
The progression on the performed motor skills was assessed by analyzing the game data. After every game session, the game data were saved in a patient-specific folder. In this folder were saved the walking velocity (“Temple of Magupta”), the movement time and velocity and three-dimensional wrist position (“Face of Cronos”), and the rotation of the head around the three axes (“Three Wind Gods”), as well as other game data.
Clinical changes
The physical condition of the patient was assessed by the 6-minute walk test.22 The objective of this test is to walk as far as possible for 6 minutes on a flat surface such as a hallway. During the test, patients were permitted to slow down, to stop, and to rest if necessary.
The subjectively experienced disability of patients with pain was assessed by a generic disability questionnaire, namely, the Pain Disability Index (PDI).23 The PDI is a self-rating scale. Answers are provided on a categorized 11-point scale with “not disabled” and “fully disabled” at the extremes. In a chronic pain population, the psychometric properties of the PDI appeared to be sufficient.23
Pain intensity of the back region or neck/shoulder region was assessed by means of a visual analog scale (VAS).24 Patients were asked to rate their experienced level of pain during the last month. The VAS consists of a 10-cm horizontal line with “no pain” on the left and “worst pain ever” on the right extremity of the line. Psychometric properties have proven to be sufficient.
The 6-minute walk test, PDI, and VAS were assessed prior to (pre-test) and immediately after 4 weeks of gaming (post-test).
Analysis
To assess the user experience, the mean scores post-test of the assessed questionnaires were calculated. Because of the pilot characteristics of this study, all patients were asked to play all three minigames, even if the motor skill(s) requested in the minigames did not correspond with their needs. For this reason the progression on the performed motor skills of the game are presented separately for the whole group and for the patients with a significant impaired function for these motor skills.
For the “Temple of Magupta” minigame, the average walking speeds for each game week are presented. The average walking speed was calculated over the total “Temple of Magupta” minigame, per session. For the “Face of Cronos” minigame, the average overhead reaching heights, wrist position, for each game week are presented. The wrist position was determined as the maximum wrist height per movement. This position was relative to the shoulder. The maximum height of every reach was defined as the point, between the start and end of a movement, in which the velocity of the wrist was 0 m/second. For every game session, an average value was calculated to describe the reaching heights. For the “Three Wind Gods” minigame, the average range of motion (in degrees) of the cervical axial rotation from left to right (no movement) for each game week is presented. For every game session, an average value was calculated to describe the CROM. Data processing and calculation were done using Matlab software (version R2008b; MathWorks, Natick, MA).
To investigate the changes of game output over the weeks, mixed-model analysis for repeated measures was used. Time of measurement (week) was used as a within-subjects factor. Post hoc comparisons were made when required, and Sidak's adjustments were used to correct for multiple tests. At a group level, the overall clinical effect of the “PlayMancer” game over time (pre-test versus post-test) on physical condition, disability, and pain intensity was analyzed using a paired nonparametric test (Wilcoxon). SPSS version 19.0 software (SPSS, Inc., Chicago, IL) was used for statistical testing. Alpha was set at 0.05 to test for statistical significance.
Results
Ten patients (two male and eight female) participated in this study. All patients met the predefined inclusion criteria and completed the 4 weeks of gaming. The mean age was 54.9 years (standard deviation [SD] 11.8; range, 27–68). Six of the patients reported primary neck/shoulder complaints, and four patients reported primary low back complaints. The average pain intensity of the patients was 5.9 (SD 2.1), and the average disability score was 27.3 (SD 13.5), indicating mild to moderate disability levels. All patients were able to walk without a walking aid. Four of the patients were employed and worked for 28–40 hours per week, three of the patients were retired, and three patients were unemployed (Table 1).
Table 1.
Demographic Characteristics of the Included Patients
| Characteristic | Value |
|---|---|
| Age (years) | 54.9 (SD 11.8; range, 27–68) |
| Gender | 20% male |
| 80% female | |
| Complaints | 60% neck/shoulder pain |
| 40% low back pain | |
| Pain intensity | 5.9 (SD 2.1; range, 1.6–8.0) |
| Disability score | 27.2 (SD 13.5; range, 6–55) |
| Work status | 40% employed |
| 30% retired | |
| 30% unemployed |
SD, standard deviation.
User experience
With respect to the reliability analysis of the SUS, Cronbach's alpha of the 10 items was 0.5, indicating poor reliability. The usability of the “PlayMancer” exergame was rated good (SUS score ≤71.425), with a mean SUS score of 77.5 (SD 9.5; range, 60.0–97.5).
The overall satisfaction with the “PlayMancer” exergame was high. The patients gave the exergame an average rating of 7.6 (SD 0.7; range, 6–8) out of 10. Four patients responded to the open question about the overall experience of the exergame. The patients stated:
The game distracted me, I was less aware of the pain and therefore I was able to relax and play the game. (Patient number 3)
I liked to play the game. (Patient number 4)
The “Temple of the Mapugta” mini-game I enjoyed most, the other two games I enjoyed less. These mini-games were insufficiently stimulating for me. (Patient number 5)
Playing the game caused distraction from my pain, therefore I was able to execute the requested exercises better; I walked longer and stretched my neck more. (Patient number 9).
Nine of the 10 patients found the “PlayMancer” exergame a motivating exergame; one patient gave a neutral answer. All the patients found that the exergame motivated them to perform the requested motor skills.
The outcomes on game experience are presented in Figure 3. With respect to the reliability analysis of the CEGEQ, Cronbach's alpha of the 17 items was 0.9, indicating good reliability. Patients enjoyed playing the “PlayMancer” exergame and considered that it did not lead to frustration. The high scores seemed to indicate that the patients were satisfied with the game environment (graphics and sounds) and game play (scenario and rules).
FIG. 3.
Overview of overall scores on the Core Elements of Gaming Experience Questionnaire (CEGEQ) subscales of enjoyment, frustration, game environment, and game play. Color images available online at www.liebertonline.com/g4h
Progression on performed motor skills
The results on the progression in performed motor skills (walking velocity, reach height, and CROM) are presented first for the whole group and second for those patients with relevant impairment.
Walking velocity
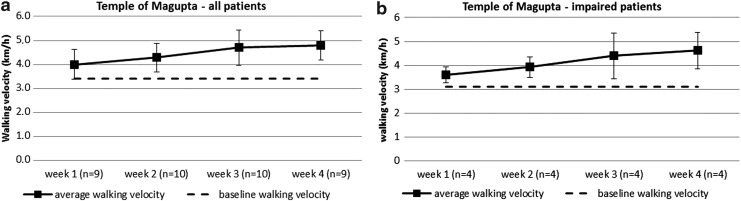
Group
Mixed-model analysis for repeated measures showed that the scores on walking velocity did not change significant over time (P≥0.22). The average baseline (voluntary) walking velocity was 3.4 km/hour (range, 2.5–4.5). In the first week, the average walking velocity during gaming was 4.0 km/hour (SD 0.6; range, 3.2–5.2), and in the final week the average walking velocity during gaming increased to 4.8 km/hour (SD 0.6; range, 3.7–5.6) (Fig. 4a).
FIG. 4.
Average walking velocity of (a) all patients and (b) the patients with an impaired walking velocity during the “Temple of Magupta” minigame.
Impaired patients
Four patients (numbers 2–4 and 10) had an impaired walking velocity of 4.2 km/hour or less on the 6-minute walk test performed pre-test.26 Looking at their walking velocity during playing the game, game data showed an average baseline walking velocity of 3.1 km/hour (range, 2.5–3.5). In the first and final weeks these values were 3.6 km/hour (SD 0.3; range, 3.2–4.0) and 4.6 km/hour (SD 0.8; range, 3.7–5.3), respectively (Fig. 4b).
Reach heights
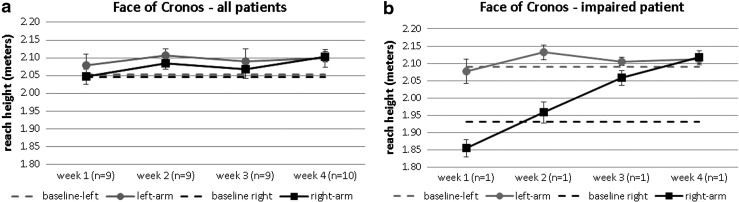
Group
Mixed-model analysis for repeated measures showed that the scores on reach height did not change significant over time (P≥0.17). The average baseline reach heights for the left and right arms were 2.05 m (range, 1.91–2.16) and 2.05 m (range, 1.93–2.14), respectively. For the left arm, the average reach height in the first week of gaming was 2.08 m (SD 0.03; range, 2.02–2.13). In the final game week, the average reach height of the left arm increased to 2.10 m (SD 0.02; range, 1.98–2.15). For the right arm, the average reach height in the first week was 2.05 m (SD 0.02; range, 1.85–2.15). In the final game week, the average reach height of the left arm increased to 2.10 m (SD 0.01; range, 2.03–2.17) (Fig. 5a).
FIG. 5.
Reach height overhead reaching of (a) all patients and (b) the patient with an impaired reach height during the “Face of Cronos” minigame.
Impaired patient
Only one patient (number 2) had in the first week a discrepancy of overhead reach height between the left and right arm. The reach height of the right arm was 23 cm under the reach height of the left arm. The reach height of the right arm of this patient in the first week was 1.85 m, and this increased to 2.12 m in the final week (Fig. 5b).
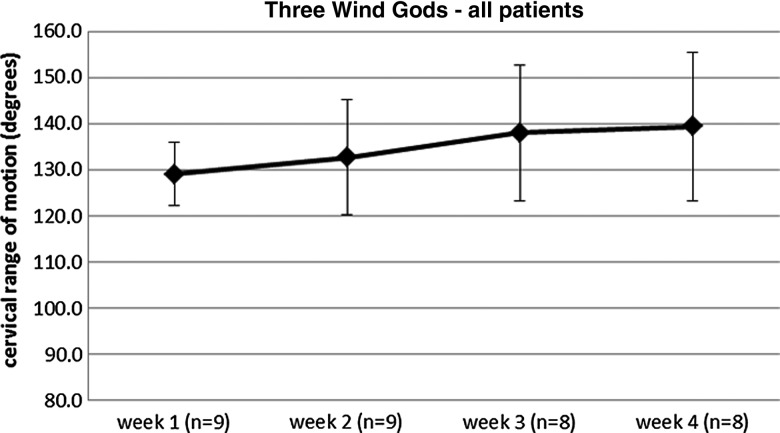
CROM
Group/impaired patients
Mixed-model analysis for repeated measures showed that the CROM scores changed significant over time (P≤0.03). During the first week, the CROM for cervical axial rotation, from left to right, during gaming was 129.1° (SD 6.8; range, 119.9°–138.5°). The CROM for cervical axial rotation, from left to right, of a healthy patient is 151.7°16; all patients had an impaired CROM (≤151.7°). During the final gaming week, the CROM increased to 139.5° (SD 16.1; range, 121.0°–161.2°) (Fig. 6). During the final week, three patients (numbers 2, 4, and 9) reached the CROM cutoff point (>151.7°) for healthy patients.16
FIG. 6.
Cervical range of motion of all patients (all had impaired motion) during the “Three Wind Gods” minigame.
Clinical effectiveness
The physical condition of the patients was assessed by using the 6-minute walk test. Pre-test, the average walking distance was 445 m (SD 77). At post-test, the average walking distance increased by 20 m to 465 m (SD 46). However, this difference was not significant (P=0.212). The PDI decreased by almost 1 point at post-test. The difference between pre-test and post-test scores for disability was not significant (P=0.505). After 4 weeks of gaming, the perceived pain intensity of the patients decreased from 59 (SD 21) on a 100-mm VAS to 50 (SD 24) to 50 (SD 24) (Table 2). Again, this average difference was not significant (P=0.284).
Table 2.
Outcome on Pain Intensity, Pain Disability, and 6-Minute Walk Test
| |
Mean (SD) |
|
|---|---|---|
| Pre-test | Post-test | |
| Pain intensity | 59 (21) | 50 (24) |
| Pain disability index | 27.2 (13.5) | 26.3 (15.0) |
| 6-minute walk test | 445 (77) | 465 (46) |
There were no significant differences between pre-test and post-test scores (P≥0.212).
SD, standard deviation.
Discussion
This pilot study focused on a first evaluation of the “PlayMancer” exergames for patients suffering from chronic musculoskeletal pain. The primary aim was to explore the user experience of the patients with the exergame. The secondary aim of this pilot study was to explore the progression in terms of the performed motor skills (walking velocity, overhead reach ability, and CROM) and the clinical changes (physical condition, disability, and pain intensity) brought about in chronic pain patients using the exergame for 4 weeks. Patients experienced the “PlayMancer” exergame as positive. They rated the usability of the exergames as good, and the exergames clearly motivated patients to perform their exercises. Furthermore, patients enjoyed playing the exergame and liked the game environment and game play. Despite the short training period, overall the patients made a nonsignificant progression in terms of the requested motor skills in the minigames during the 4 weeks of gaming, especially those patients with impaired motor skills. After 4 weeks of gaming, generally patients were capable of walking faster and reaching higher and experienced an increase in neck mobility.
Based on this, it is expected that gaming has a true potential for physical rehabilitation also in the future, especially when used in combination with telemedicine applications that enable home-exercising. Home-based exercise programs are known to be effective,27 but the overall low conformance with such programs remains problematic.28 It is known that a higher conformance to a rehabilitation program has a more positive effect on clinical outcomes.29 Exergames, such as the “PlayMancer” exergame, encourage patients to perform their exercises, so they have the potential to overcome the generally low compliance with the home-based exercise programs. Another positive aspect of the “PlayMancer” exergame is the availability of game data. These data provide the therapist with detailed information on the progression of a patient in terms of the various trained motor skills. By using the available game data, the therapist can better align the game session to the needs of the individual patient, and the transparency of the treatment is increased, which matches the current trend in healthcare. However, none of the commercially available exergames currently provides the healthcare professional with this type of game output.
Previous randomized controlled trials have shown the potential of games for helping to rehabilitate stroke patients,30–32 patients with acquired brain injury,33 and young patients with cerebral palsy.34 Clinical trials to test the benefits of exergames in rehabilitation are necessary before such games are incorporated into rehabilitation programs.35 This pilot study is a first step toward the implementation of exergames in the physical rehabilitation of chronic musculoskeletal pain patients.36 The framework for telemedicine evaluation proposed by DeChant et al.17 was used, and in line with this framework, the presented pilot study was a stage 1–2 evaluation. In the terminology of DeChant et al.,17 the evaluation of an application starts with an evaluation of the technical efficacy (accuracy and reliability) of the application and an evaluation of the primary objective of the application in terms of access, quality, or cost (stage 1–2). During the subsequent deployment, a comprehensive evaluation is necessary, using multiple end points such as the quality, accessibility, and costs of this healthcare approach (stage 3). The final step in the evaluation of an application is to examine whether the overall evaluation of an application in one system can also apply in other settings (stage 4).17 Even though this framework is designed for telemedicine evaluation, it can be adopted for evaluation of serious games in healthcare. This framework can help other researchers to organize the evaluation of their serious (exer)games in a clinical setting. Although the sample size of this pilot study is low and there was no control group, it still extends the knowledge about the use of exergames in the physical rehabilitation of chronic pain patients.37
By playing the “PlayMancer” game, patients made a progression in the requested motor skills. In rehabilitation a progression of 15 percent is often considered as clinically relevant.38 Given our results on a group level, the progression made on walking velocity is clinically relevant. On an individual level 70 percent of the patients made a clinically relevant progression on walking velocity, 10 percent of the patients made a clinically relevant progression on reach height, and 30 percent of the patients made a clinically relevant progression on CROM. A next step in the evaluation of the “PlayMancer” exergame is to compare it with conventional physiotherapy for patients suffering from chronic musculoskeletal pain and to compare them on clinical benefit, user experience, and costs (stage 3).
The following adjustments could increase the potential of the “PlayMancer” game as a tool with rehabilitation purpose. First, the current version of the “PlayMancer” game only involves three minigames, and an increase of the number of minigames would be desirable. With more minigames available, a game session with the “PlayMancer” exergame could be better adjusted to the rehabilitation goals of the individual patient, and that patient's treatment protocol can be refined. Second, the duration of the treatment protocol in this study was 4 weeks. Patients visited the Roessingh Research and Development lab to play the “PlayMancer” game one or two times a week over 4 weeks. Because of the positive effects of intensity, frequency, and duration of training on physical fitness,39 it can be assumed that extending the treatment protocol (for example, duration of 6 weeks instead of 4 weeks and frequency of at least twice a week) could further positively influence the outcome. A final suggestion is to adjust the game for remote physical rehabilitation. In the current setting, patients were dependent on the availability of the therapist and the Roessingh Research and Development lab to play the game. Besides, an extensive MoCap system was needed to generate input for the game. For a remote physical rehabilitation setting, there must be an easy-to-use and cheap alternative for this MoCap system, such as the Microsoft® (Redmond, WA) Kinect®. In a previous study, the Microsoft Kinect was integrated into the “PlayMancer” game and tested as an alternative low-cost MoCap system. In this setting, two of the “PlayMancer” minigames (“Temple of Magupta” and “Face of Cronos”) could be controlled by the requested motor skills.10 Concerning the “PlayMancer” game as a tool for remote physical rehabilitation, a next step is to evaluate the game in combination with more easy-to-use motion capturing systems in a home setting and see if the outcome on accessibility and quality are comparable with the outcomes of this study. Our existing knowledge about telerehabilitation suggests that the “PlayMancer” exergame has the potential to increase the quality and accessibility of healthcare and perhaps with lower costs. Patients can play the exergame during a self-scheduled time span in their own environment. This would fit with the current trend of self-management of the patient.40
One of the limitations of this study is the use of nonvalidated Dutch versions of the SUS and CEGEQ because no other validated Dutch questionnaires to assess usability and game experience were available. Given the Cronbach's alpha of these questionnaires, the reliability of the SUS and CEGEQ were indicated as poor and good, respectively. Therefore the use of this Dutch version of the CEGEQ is allowed, but for the future use of the current Dutch version of the SUS should be reconsidered.
In conclusion, the “PlayMancer” exergame has demonstrated preliminary potential efficacy in a small sample of adults with musculoskeletal pain and could be a novel tool for achieving physical rehabilitation because it motivates patients to perform their exercises, and as a result, their motor skills and physical condition both improve.
Acknowledgments
Special thanks go to Michiel Minten for his assistance in carrying out this study, and we want to thank Cris Voldum, Jens Juul Jacobsen, Jeppe H. Nielsen, and Jørgen Krabbe from Serious Games Interactive for the implementation of the game. This work was funded by the European Union within the PLAYMANCER project (FP7-ICT-215839).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Kharrazi H. Lu A. Gharghabi F. Coleman W. A scoping review of health game research: Past, present, and future. Games Health J. 2012;1:153–164. doi: 10.1089/g4h.2012.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maloney A. Threlkeld K. Cook W. Comparative effectiveness of a 12-week physical activity intervention for overweight and obese youth: Exergaming with “Dance Dance Revolution.”. Games Health J. 2012;1:96–103. doi: 10.1089/g4h.2011.0009. [DOI] [PubMed] [Google Scholar]
- 3.Biddiss E. Irwin J. Active video games to promote physical activity in children and youth: A systematic review. Arch Pediatr Adolesc Med. 2010;164:664–672. doi: 10.1001/archpediatrics.2010.104. [DOI] [PubMed] [Google Scholar]
- 4.Lange B. Flynn SM. Rizzo AA. Game-based telerehabilitation. Eur J Phys Rehabil Med. 2009;45:143–151. [PubMed] [Google Scholar]
- 5.Kato PM. Video games in health care: Closing the gap. Rev Gen Psychol. 2010;14:113–121. [Google Scholar]
- 6.Graves L. Stratton G. Ridgers ND. Cable NT. Comparison of energy expenditure in adolescents when playing new generation and sedentary computer games: Cross sectional study. BMJ. 2007;335:1282–1284. doi: 10.1136/bmj.39415.632951.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Graves LE. Ridgers ND. Stratton G. The contribution of upper limb and total body movement to adolescents' energy expenditure whilst playing Nintendo Wii. Eur J Appl Physiol. 2008;104:617–623. doi: 10.1007/s00421-008-0813-8. [DOI] [PubMed] [Google Scholar]
- 8.Taylor MJ. McCormick D. Shawis T, et al. Activity-promoting gaming systems in exercise and rehabilitation. J Rehabil Res Dev. 2011;48:1171–1186. doi: 10.1682/jrrd.2010.09.0171. [DOI] [PubMed] [Google Scholar]
- 9.Playmancer. 2008. http://playmancer.unige.ch/ [Sep 7;2013 ]. http://playmancer.unige.ch/
- 10.Schonauer C. Pintaric T. Kaufmann H, et al. Chronic pain rehabilitation with a serious game using multimodal input. 2011 International Conference on Virtual Rehabilitation (ICVR); ETH Zurich Science City, Switzerland: Rehab Week Zurich; Jun 27–29, 2011. p. 8. [Google Scholar]
- 11.Schönauer C. Kaufmann H. Jansen-Kosterink S, et al. Design eines Serious Games für die Rehabilitation von chronischen Rückenschmerzen. 6th Vienna Games Conference, Future and Reality of Gaming (FROG); Oct 12–13;2012 ; in press. [Google Scholar]
- 12.Spenkelink CD. Hutten MM. Hermens HJ. Greitemann BO. Assessment of activities of daily living with an ambulatory monitoring system: A comparative study in patients with chronic low back pain and nonsymptomatic controls. Clin Rehabil. 2002;16:16–26. doi: 10.1191/0269215502cr463oa. [DOI] [PubMed] [Google Scholar]
- 13.Hasenbring M. Marienfeld G. Kuhlendahl D. Soyka D. Risk factors of chronicity in lumbar disc patients. A prospective investigation of biologic, psychologic, and social predictors of therapy outcome. Spine (Phila Pa 1976) 1994;19:2759–2765. doi: 10.1097/00007632-199412150-00004. [DOI] [PubMed] [Google Scholar]
- 14.Sandlund J. Roijezon U. Bjorklund M. Djupsjobacka M. Acuity of goal-directed arm movements to visible targets in chronic neck pain. J Rehabil Med. 2008;40:366–374. doi: 10.2340/16501977-0175. [DOI] [PubMed] [Google Scholar]
- 15.Woodhouse A. Vasseljen O. Altered motor control patterns in whiplash and chronic neck pain. BMC Musculoskelet Disord. 2008;9:90. doi: 10.1186/1471-2474-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sjolander P. Michaelson P. Jaric S. Djupsjobacka M. Sensorimotor disturbances in chronic neck pain—Range of motion, peak velocity, smoothness of movement, and repositioning acuity. Man Ther. 2008;13:122–131. doi: 10.1016/j.math.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 17.DeChant HK. Tohme WG. Mun SK, et al. Health systems evaluation of telemedicine: A staged approach. Telemed J. 1996;2:303–312. doi: 10.1089/tmj.1.1996.2.303. [DOI] [PubMed] [Google Scholar]
- 18.Pintaric T. Kaufmann H. Affordable infrared-optical pose-tracking for virtual and augmented reality. In: Zachmann G, editor. IEEE VR Workshop on Trends and Issues in Tracking for Virtual Environments. Aachen: Shaker Verlag; 2007. pp. 44–51. [Google Scholar]
- 19.Hermens HJ. Freriks B. Disselhorst-Klug C. Rau G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000;10:361–374. doi: 10.1016/s1050-6411(00)00027-4. [DOI] [PubMed] [Google Scholar]
- 20.Brooke J. SUS—A quick and dirty usability scale. In: Jordan PW, editor; Thoma B, editor; Weerdmeester BA, editor. Usability Evaluation in Industry. London: Taylor & Francis; 1995. pp. 189–194. [Google Scholar]
- 21.Calvillo-Gámez E. Cairns P. Cox A. Assessing the core elements of the gaming experience. In: Bernhaupt R, editor. Evaluating User Experience in Games. London: Springer; 2010. pp. 47–71. [Google Scholar]
- 22.ATS statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 23.Tait RC. Chibnall JT. Krause S. The Pain Disability Index: Psychometric properties. Pain. 1990;40:171–182. doi: 10.1016/0304-3959(90)90068-O. [DOI] [PubMed] [Google Scholar]
- 24.Gift A. Visual Analogue Scales: Measurement of subjective phenomena. Nurs Res. 1989;38:286–288. [PubMed] [Google Scholar]
- 25.Bangor A. Kortum P. Miller J. Determining what individual SUS scores mean: Adding an Adjective Rating Scale. J Usability Stud. 2009;4:114–123. [Google Scholar]
- 26.Keefe FJ. Hill RW. An objective approach to quantifying pain behavior and gait patterns in low back pain patients. Pain. 1985;21:153–161. doi: 10.1016/0304-3959(85)90285-4. [DOI] [PubMed] [Google Scholar]
- 27.Liu WT. Wang CH. Lin HC, et al. Efficacy of a cell phone-based exercise programme for COPD. Eur Respir J. 2008;32:651–659. doi: 10.1183/09031936.00104407. [DOI] [PubMed] [Google Scholar]
- 28.Steele BG. Belza B. Cain KC, et al. A randomized clinical trial of an activity and exercise adherence intervention in chronic pulmonary disease. Arch Phys Med Rehabil. 2008;89:404–412. doi: 10.1016/j.apmr.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Cramer JA. Benedict A. Muszbek N, et al. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: A review. Int J Clin Pract. 2008;62:76–87. doi: 10.1111/j.1742-1241.2007.01630.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kowalczewski J. Chong SL. Galea M. Prochazka A. In-home tele-rehabilitation improves tetraplegic hand function. Neurorehabil Neural Repair. 2011;25:412–422. doi: 10.1177/1545968310394869. [DOI] [PubMed] [Google Scholar]
- 31.Saposnik G. Teasell R. Mamdani M, et al. Effectiveness of virtual reality using Wii gaming technology in stroke rehabilitation: A pilot randomized clinical trial and proof of principle. Stroke. 2010;41:1477–1484. doi: 10.1161/STROKEAHA.110.584979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yavuzer G. Senel A. Atay MB. Stam HJ. ''Playstation Eyetoy games'' improve upper extremity-related motor functioning in subacute stroke: A randomized controlled clinical trial. Eur J Phys Rehabil Med. 2008;44:237–244. [PubMed] [Google Scholar]
- 33.Gil-Gomez JA. Llorens R. Alcaniz M. Colomer C. Effectiveness of a Wii balance board-based system (eBaViR) for balance rehabilitation: A pilot randomized clinical trial in patients with acquired brain injury. J Neuroeng Rehabil. 2011;8:30. doi: 10.1186/1743-0003-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wade W. Porter D. Sitting playfully: Does the use of a centre of gravity computer game controller influence the sitting ability of young people with cerebral palsy? Disabil Rehabil Assist Technol. 2012;7:122–129. doi: 10.3109/17483107.2011.589485. [DOI] [PubMed] [Google Scholar]
- 35.McCallum S. Gamification and serious games for personalized health. Stud Health Technol Inform. 2012;177:85–96. [PubMed] [Google Scholar]
- 36.Leon AC. Davis LL. Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45:626–629. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arain M. Campbell MJ. Cooper CL. Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol. 2010;10:67. doi: 10.1186/1471-2288-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions: Overview and methodology. Phys Ther. 2001;81:1629–1640. [PubMed] [Google Scholar]
- 39.Kwakkel G. Impact of intensity of practice after stroke: Issues for consideration. Disabil Rehabil. 2006;28:823–30. doi: 10.1080/09638280500534861. [DOI] [PubMed] [Google Scholar]
- 40.Kennedy A. Rogers A. Bower P. Support for self care for patients with chronic disease. BMJ. 2007;335:968–970. doi: 10.1136/bmj.39372.540903.94. [DOI] [PMC free article] [PubMed] [Google Scholar]