Abstract
Background and aims
Integrating psychiatric services within substance abuse treatment settings is a promising service delivery model, but has not been evaluated using random assignment to psychiatric treatment setting and controlled delivery of psychiatric care. This study evaluates the efficacy of on-site and integrated psychiatric service delivery in an opioid-agonist treatment program on psychiatric and substance use outcomes.
Design
Participants at the Addiction Treatment Services (ATS) were assigned randomly to receive on-site and integrated substance abuse and psychiatric care (on-site: n=160) versus off-site and non-integrated substance abuse and psychiatric care (off-site: n=156), and observed for 1 year. On-site participants received all psychiatric care within the substance abuse program by the same group of treatment providers. The same type and schedule of psychiatric services were available to off-site participants at a community psychiatry program.
Setting
All participants received routine methadone maintenance at the ATS program in Baltimore, Maryland, USA.
Participants
Participants were opioid-dependent men and women with at least one comorbid psychiatric disorder as assessed by the Structured Clinical Interview for DSM-IV and confirmed by expert clinical reappraisal.
Measurements
Outcomes included psychiatric service utilization and retention, Hopkins Symptom Checklist Global Severity Index (GSI) change scores, and urinalysis test results.
Findings
On-site participants were more likely to initiate psychiatric care (96.9% vs. 79.5%, p < 0.001), remain in treatment longer (195.9 vs. 101.9 days; p < 0.001), attend more psychiatrist appointments (12.9 vs. 2.7; p < 0.001), and have greater reductions in GSI scores (4.2 vs. 1.7; p = .003) than off-site participants; no differences were observed for drug use.
Conclusions
On-site and integrated psychiatric and substance misuse services in a methadone treatment setting may improve psychiatric outcomes compared with off-site and non-integrated substance misuse and psychiatric care. However, this might not translate into improved substance misuse outcomes.
Introduction
Substance abuse treatment incorporating daily methadone and weekly counseling is generally effective in reducing the harmful consequences of opioid dependence disorder [1,2]. Approximately half of treatment-seeking opioid-dependent patients also have a comorbid psychiatric disorder [3,4]. These comorbid conditions are associated with increased levels of psychiatric distress and greater impairment in psychosocial functioning [3,5-7], and can reduce the effectiveness of substance abuse treatment [8,9]. Many of the psychiatric syndromes common in drug-dependent patients can be managed effectively with existing psychiatric therapies [10], although considerable variability in outcomes has been observed in placebo-controlled medication trials [11,12].
One common strategy used by substance abuse programs to help patients with psychiatric problems is to refer them to psychiatric treatment providers in the community [4]. Unfortunately, this intervention has a high failure rate. Most of the patients referred to psychiatric treatment providers miss their appointment for intake evaluation, and many who complete the intake evaluation miss subsequent sessions and discontinue psychiatric care. A report by Pringle et al. [13] noted that more than 90% of these patients fail to gain access to adequate amounts of psychiatric care, and many fail to attend even routine substance abuse counseling sessions [14]. These problems have stimulated considerable discussion in the field on how to deliver adequate amounts of psychiatric care to more of these patients.
The integration of substance abuse and other psychiatric services in a substance abuse treatment setting is a promising approach to improve patient adherence to and outcomes from these services [15]. The most notable benefit to an integrated approach is that patients already coming to the substance abuse program will have more convenient access to psychiatric services, thereby improving utilization of these resources. Because psychiatric service utilization has a strong positive relationship with treatment response [16-18], patients treated within an on-site and integrated service delivery setting could be expected to achieve better psychiatric and drug use outcomes compared to those treated in separate clinical settings.
Published randomized studies of integrated care have been conducted largely in psychiatric settings and have compared integrated approaches (psychiatric and substance abuse services in a single setting) to standard care (psychiatric services only). These studies provide some support for integrated care [19-21] but have important limitations. One of these limitations is the absence of studies that control for the amount of psychiatric and substance abuse services available to participants in order to evaluate the effects of treatment setting on outcomes. For example, no controlled trials were found evaluating the efficacy of on-site and integrated substance abuse and psychiatric services to off-site treatment approaches. While considerable methodological challenges exist in controlling the type and amount of psychiatric services available within and outside of a substance abuse treatment program, the absence of these studies is a limitation in the field [15,19].
The present study reports on a randomized trial that controls for the amount of psychiatric services offered within versus outside a methadone treatment program. Opioid-dependent patients with comorbid psychiatric disorders (n=316) were assigned randomly to receive a standard set of psychiatric services (i.e., psychiatrist appointments; individual and group therapy; pharmacotherapy) within a methadone program (on-site) versus a community psychiatry program on the same campus (off-site); all participants received substance abuse treatment within the same methadone program [22]. Participants randomized to the on-site versus off-site psychiatric condition were expected to have higher rates of psychiatric treatment initiation and utilization, lower amounts of psychiatric distress, and less drug use.
Methods
Participants
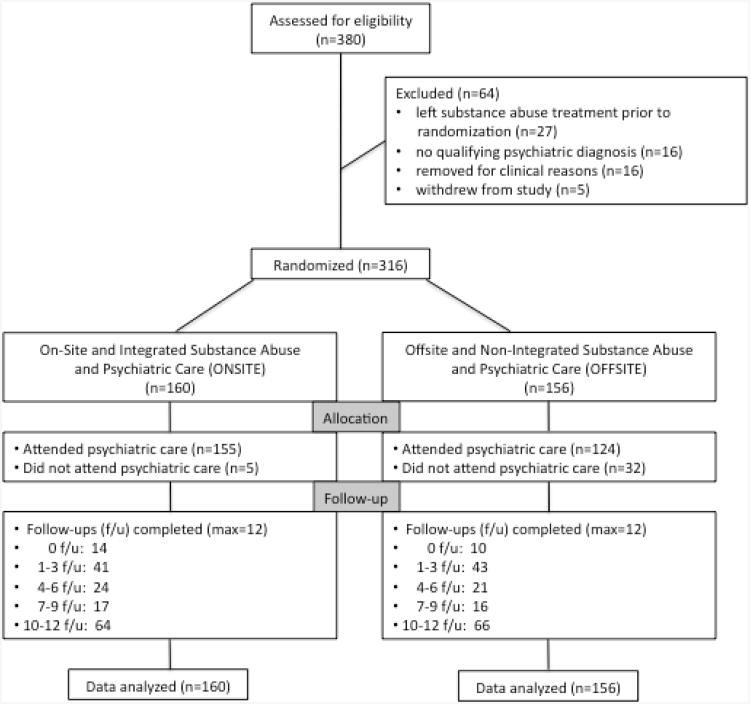
A total of 380 opioid-dependent patients in the Addiction Treatment Services (ATS) program in Baltimore Maryland provided informed written consent to participate in the study. Most of these enrollees (83%, n=316) were randomized to treatment condition (Figure 1). Comparisons of randomized and non-randomized enrollees on demographic variables found one significant difference - fewer randomized participants were classified as minority (43.8% vs. 58.5%; χ2=4.73, df=1, p=0.030). The majority of participants (61%) were in methadone treatment for at least 60 days, remaining participants were new admissions. Study eligibility criteria were: (i) DSM-IV criterion for Opioid Dependence and Center for Substance Abuse Treatment guidelines for methadone maintenance, (ii) DSM-IV criterion for a current psychiatric diagnosis eligible for treatment reimbursement within Maryland's public mental health system, and (iii) interest in receiving treatment for the psychiatric problem. Exclusion criteria were: (i) pregnancy, (ii) acute medical or psychiatric problems that required urgent attention, or (iii) evidence of an organic mental disorder or other cognitive impairment likely to interfere with comprehension of study procedures and participation. The Johns Hopkins Institutional Review Board approved the study.
Figure 1. Consort Diagram.
Table 1 shows the demographics characteristics, psychiatric and substance use diagnostic profiles in the sample (prevalent in >10%, with exception of psychotic disorders), and baseline urinalysis results. Approximately half of the sample (47%) had more than one current Axis I psychiatric diagnosis. Major depression was the most common diagnosis, followed by post-traumatic stress disorder. Cocaine dependence was the most prevalent substance use disorder after opioid dependence.
Table 1. Demographic, psychiatric1, and substance use disorder1 characteristics at baseline.
| Characteristic | Overall (n=316) | ONSITE2 (n=160) | OFFSITE2 (n=156) |
|---|---|---|---|
|
| |||
| M (SE) or % | M (SE) or % | M (SE) or % | |
|
| |||
| Demographics | |||
|
| |||
| Gender (%) | |||
| Male | 37.7% | 37.5% | 37.8% |
| Female | 62.3% | 62.5% | 62.2% |
|
| |||
| Race (%) | |||
| White | 58.5% | 57.5% | 59.6% |
| Minority3 | 41.5% | 42.5% | 40.4% |
|
| |||
| Age (years) | 39.8 (0.49) | 40.2 (0.71) | 39.4 (0.68) |
|
| |||
| Education (highest grade completed) | 11.0 (0.12) | 11.14 (0.17) | 10.88 (0.17) |
|
| |||
| Married (%) | 17.1% | 16.9% | 17.3% |
|
| |||
| Employed (%) | 14.6% | 12.5% | 16.7% |
|
| |||
| Psychiatric Disorders | |||
| Current Axis I disorder | 97.5% | 98.8% | 96.2% |
|
| |||
| More than 1 Axis I disorder | 46.8% | 47.5% | 46.2% |
|
| |||
| Current psychotic disorder | 4.1% | 4.4% | 3.9% |
| Schizophrenia | 1.0% | 1.3% | 0.6% |
| Schizoaffective disorder | 3.2% | 3.1% | 3.2% |
|
| |||
| Current mood disorder | 76.0% | 79.4% | 72.4% |
| Major Depression | 50.0% | 50.0% | 50.0% |
| Bipolar I | 13.9% | 15.6% | 12.2% |
| Dysthymia | 11.7% | 13.8% | 9.6% |
|
| |||
| Current anxiety disorder | 54.1% | 53.1% | 55.1% |
| Posttraumatic stress disorder | 22.0% | 20.4% | 23.7% |
| Panic disorder | 16.5% | 18.8% | 14.1% |
| Social Phobia | 13.3% | 11.9% | 14.7% |
| Generalized anxiety disorder | 10.8% | 11.9% | 9.6% |
|
| |||
| Axis II disorder | 58.9% | 62.5% | 55.1% |
|
| |||
| Antisocial personality disorder (APD) | 33.9% | 39.4% | 28.2% |
|
| |||
| Other Axis II (not including APD) | 44.3% | 49.4% | 39.1% |
|
| |||
| Substance Use Disorders | |||
|
| |||
| Alcohol | 9.8% | 12.5% | 7.1% |
| Sedative | 13.9% | 17.5% | 10.3% |
| Cocaine | 29.1% | 31.9% | 26.3% |
|
| |||
| Urinalysis Results | |||
|
| |||
| Opioid-positive (%) | 21% (0.02) | 21% (0.03) | 22% (0.03) |
| Cocaine-positive (%) | 28% (0.02) | 31% (0.03) | 25% (0.03) |
| Sedative-positive (%) | 13% (0.02) | 15% (0.02) | 12% (0.02) |
Diagnoses determined using the Structured Clinical Interview for the DSM-IV. With the exception of psychotic disorders, only psychiatric disorders prevalent in at least 10% of in > 10% of the sample are included.
ONSITE: Onsite Integrated Substance Abuse and Psychiatric Care; OFFSITE: Offsite Non-integrated Substance Abuse and Psychiatric Care
Most minority participants (n = 131) were African American (n = 102; 77.9%); others were classified as Native American (n = 23; 17.6%), Hispanic (n = 3; 2.3%), Asian (n = 2; 1.5%), or Pacific Islander (n = 1; 0.7%).
Assessments
The Structured Clinical Interview for DSM-IV (SCID-I and SCID-II, [23]) was administered during the second week of baseline evaluation. The SCID-I utilizes a decision tree for making current and life-time DSM-IV diagnoses; the SCID-II provides information for diagnoses of personality disorder. The Hopkins Symptom Checklist (SCL-90-R [24,25]) was administered at baseline and monthly to measure self-reported psychiatric distress (using a 0-4 Likert Scale); the summary Global Severity Index (GSI) score used in the study is the average rating given to all 90 items and correlates highly to the individual scales. Participants taking psychiatric medications completed a four-question self-report measure (Self-Report Measure of Medication Adherence-SMMA; [26]) each month that used a four-point Likert Scale to assess adherence to medications (lower scores indicating greater adherence). Study conditions completed a similar mean number of follow-up assessments (on-site: M=6.7 vs. off-site: M=6.9).
Interviewers completed an assessment training protocol used in our program for more than a decade to establish and sustain good rater reliability [27]. Psychiatric diagnoses based on the SCID were clinically reappraised by a study investigator, who also screened participants for suicidal ideation, thought disorder, delusions, and hallucinations. Participants submitted urine samples for drug testing once per week using a modified random schedule (Monday, Wednesday, or Friday). Samples were obtained under direct observation (a one-way mirror) and tested at a certified laboratory that employed thin-layer chromatography (TLC) and enzyme multiplied immunoassay technique (EMIT) testing for the presence of opioids, cocaine, and benzodiazepines.
Procedure
Participants were stratified on gender and duration of present episode of substance abuse treatment (0-60 days versus >60 days). Research assistants randomized participants using a computerized generated program to one of two psychiatric service delivery conditions: 1) on-site and integrated substance abuse and psychiatric care (on-site; n=160) versus 2) off-site and non-integrated substance abuse and psychiatric care (off-site; n=156). Participants in the on-site condition were offered psychiatric care within the ATS program. Service integration was accomplished by having the same providers of substance abuse treatment also provide the psychiatric care. Off-site participants were offered the same type and schedule of psychiatric services at the Community Psychiatry Program located on the same campus.
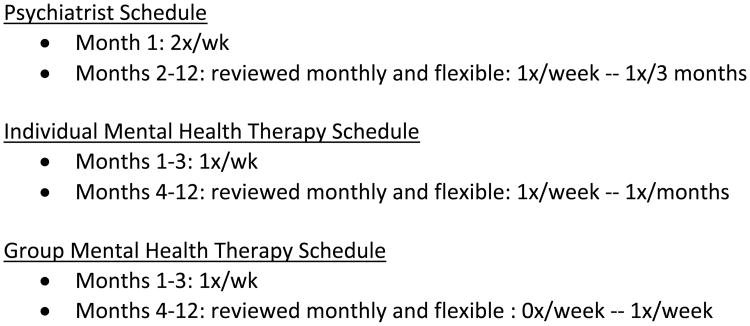
A standardized psychiatric treatment protocol (Figure 2) was used in both the on-site and off-site psychiatric treatment settings, developed by the investigator team and the medical director of the Community Psychiatry Program. While the content of the psychiatric sessions varied to some extent across staff and treatment settings, controlling the amounts of psychiatric services offered in both settings allowed us to evaluate the effects of psychiatric service location on outcomes.
Figure 2.
Standardized psychiatric treatment protocol used at the Addiction Treatment Services (ONSITE) and Community Psychiatry Program (OFFSITE) treatment settings.
Neither participants nor staff was blind to the study design and participants were followed-up to 12 months. The initial psychiatric treatment episode for participants in both conditions was ended when participants failed to attend any scheduled psychiatric sessions for 8 consecutive weeks. However, multiple psychiatric treatment episodes were possible within the 12-month evaluation, and participants discontinuing their initial episode of care could resume psychiatric care in the same setting at another point in time.
Psychiatric treatment conditions
On-site
Participants were scheduled to attend initial psychiatric treatment sessions with the primary counselor and the attending psychiatrist within 4 days following random assignment. Board-certified psychiatrists in the substance abuse program used the first session to confirm the SCID diagnosis and formulate the initial care plan using the standard psychiatric treatment protocol developed for both conditions. Psychiatric services were offered in addition to the routine substance abuse treatment schedule and were provided by the same group of providers. Primary counselors (BA or MA degree) provided the individual mental health sessions (approximately 40 minutes), utilizing supportive and directive therapeutic approaches [28]. Participants were also scheduled to attend a weekly 60-minute group therapy session during the first 3 months of care to provide additional support and psychiatric illness education.
Off-site
The referral and psychiatric treatment processes and procedures for these participants paralleled the approach used in the on-site condition. Research staff provided off-site participants with an intake appointment at the Community Psychiatry Program within 4 days of random assignment, and gave them the phone number to confirm the appointment. On the day of intake, the community psychiatry admissions coordinator arranged for participants to meet with a psychiatrist and their individual therapist. Psychiatrists conducted a standard evaluation to confirm the diagnostic profile produced by the SCID interview and expert clinical reappraisal, and formulated the initial treatment plan using the same psychiatric treatment protocol in off-site participants. Mental health therapists (MA degree with license/certification) provided individual therapy (40 minutes) using supportive and directive approaches. During the first 3 months, participants were also scheduled for a weekly psychoeducational group (60 minutes).
Access to psychiatric medications
On-site and off-site participants were provided with comparable access to prescribed psychiatric medications. Prescriptions were submitted to a single pharmacy that delivered the medications to the ATS program within 48 hours. Participants in the on-site versus off-site condition were more likely to begin pharmacotherapy (90% vs. 82%; χ2=4.61, df=1, p=0.032); SSI antidepressants (e.g., Celexa) were prescribed most often (60%), followed by heterocyclic antidepressants (39%; e.g., Elavil) and atypical antipsychotics (28%; e.g., Seroquel).
Staff training and fidelity to psychiatric treatment protocol
Substance abuse and community psychiatry staff attended an annual series of six seminars on the treatment of substance users with co-occurring psychiatric disorders using the common psychiatric treatment protocol, led by study investigators (e.g., RKB and VK) and other faculty members. Psychiatrists and therapists in both treatment settings completed forms weekly to document all psychiatric service contacts (including session length). These forms were given to research support staff who monitored adherence to the psychiatric treatment protocol on a weekly basis.
To compare ratios of scheduled psychiatric sessions per month, t-tests were used to assess fidelity to the psychiatric treatment schedule for those initiating psychiatric care (on-site: n=155; off-site: n=124). On-site and off-site participants were scheduled to attend a similar number of individual (on-site: M=3.9; SE = 0.03 vs. off-site: M=3.8; SE=0.03; t=1.39 (df=277), p=0.164) and group psychiatric sessions per month (on-site: M=3.9; SE = 0.04 vs. off-site: M=3.8; SE=0.05; t=1.76 (df = 277), p=0.079), although on-site participants were scheduled for more psychiatrist appointments per month (on-site: M=2.4; SE=0.06 vs. off-site: M=1.4; SE=0.06, t=12.44 (df=277), p<0.001).
Substance abuse treatment
All participants received routine methadone treatment in the ATS program. The program uses an adaptive treatment approach [22] that increases systematically the number of counseling sessions for participants with persistent drug use and missed counseling sessions. Behavioral contingencies are used in this approach to help motivate attendance to counseling sessions and reduced drug use; these contingencies include common aspects of methadone treatment (e.g., early versus later medication dispensing times, access to medication take-home doses) [29, 30]. Psychiatrists in the program prescribed methadone to all participants. Mean methadone dose for the combined sample was 77.2 mg, and similar across psychiatric treatment conditions (on-site: M=76.3 mg; SE=2.1 vs. off-site: M=78.3 mg; SE=1.9; F(1, 311)=0.33, p=0.567).
Data analysis
Power analyses (alpha=0.05; power=0.80) conducted prior to the study demonstrated that the sample (n=316) was sufficient to evaluate primary outcomes of psychiatric distress and substance use. Analyses used an intent-to-treat approach.
The primary outcome of psychiatric distress was evaluated by examining condition differences in changes in GSI scores from baseline (Time 1) to the mean GSI score over the 12-month follow-up (Time 2). For participants without GSI follow-up scores (on-site: n=14; off-site: n=10), baseline GSI scores were imputed at follow-up to assume no change. Three on-site participants with no baseline GSI were excluded. Mixed models, controlling for baseline differences in GSI scores, evaluated condition differences in these change scores [31]. These analyses were chosen to simplify interpretation of results due to participant variability in initiation, duration, and completion of psychiatric and substance abuse treatment during the 1-year observation period. Analyses conducted without imputation yielded similar results and are not reported. For secondary psychiatric outcomes, a survival analysis evaluated days to the first psychiatric intake session, with those failing to initiate treatment censored at 365 days. Results are reported using hazards ratios (HR) and 95% confidence intervals. This survival analysis was repeated using only those initiating psychiatric care with similar findings. For the primary outcome of psychiatric service utilization, analyses of variance (ANOVA) compared conditions on rates of scheduled and attended psychiatric services. ANOVAs compared conditions for total days of psychiatric treatment participation, censored at the last day of the study. Logistic regression compared conditions on the proportion of participants completing psychiatric treatment. ANOVAs evaluated condition differences in SMMA scores, averaged over the follow-up for those receiving medication and completing at least one SMMA (on-site: n=135; off-site: n=94).
For the primary outcome of substance use, Generalized Estimating Equations (GEE) compared conditions on the likelihood of obtaining opioid, cocaine, and benzodiazepine positive samples. While participants remained in the study, all missing urine samples were coded as “any drug”-positive, but were not assigned a specific drug class. ANOVAs compared conditions on rates of scheduled and attended substance abuse counseling and days of substance abuse treatment.
Results
Psychiatric service utilization and retention
Table 2 shows that on-site participants were more likely to complete the initial psychiatric intake and attend it in fewer days than off-site participants. on-site participants also had more mean days of psychiatric treatment, and were more likely to complete the 1-year episode. In addition, on-site participants attended more overall psychiatric sessions than off-site participants, primarily because they attended more psychiatrist sessions. No condition differences were found for utilization of individual or group psychiatric therapy sessions, or self-reported adherence rates to psychiatric medications.
Table 2. Psychiatric and substance use outcomes by study conditions over one year.
| Outcomes | ONSITE1 (n=160) | OFFSITE1 (n=156) | χ2 or t (df) | p-value | OR2 or HR2 (95% CI2) |
|---|---|---|---|---|---|
|
| |||||
| M(SE) or % | M(SE) or % | ||||
|
| |||||
| Psychiatric outcomes | |||||
|
| |||||
| Service utilization3 | |||||
| Psychiatrist appointments | 12.9 (0.7) | 2.7 (0.2) | t(314)=13.07 | <.001 | -- |
| Individual sessions | 9.9 (0.9) | 8.6 (0.8) | t(314)=1.05 | 0.296 | -- |
| Group sessions | 0.5 (0.1) | 0.5 (0.1) | t(314)= −0.06 | 0.950 | -- |
|
| |||||
| Initiated treatment | |||||
| Completed intake | 96.9% | 79.5% | χ2(1)=113.16 | <.001 | 3.95 (3.07-5.09) |
| Days to intake | Median=5.0 | Median=31.0 | |||
|
| |||||
| Treatment retention | |||||
| Treatment days | 195.9 (10.9) | 101.9 (9.7) | t(314)=6.42 | <.001 | -- |
| Completed 1-year | 34.4% | 12.8% | χ2(1)=20.27 | <.001 | 3.56 (2.01-6.31) |
|
| |||||
| Medication adherence | |||||
| SMMA4 | 0.99 (0.08) | 0.91 (0.10) | t(227)=0.58 | 0.560 | -- |
|
| |||||
| Substance use outcomes | |||||
|
| |||||
| Urinalysis results3 | |||||
| Opioid-positive | 17.3% | 15.8% | χ2(1)=0.40 | 0.527 | 1.11 (0.80-1.55) |
| Cocaine-positive | 22.7% | 20.3% | χ2(1)=0.79 | 0.374 | 1.15 (0.84-1.57) |
| Sedative-positive | 14.5% | 15.0% | χ2(1)=0.04 | 0.844 | 0.96 (0.64-1.44) |
|
| |||||
| Treatment retention | |||||
| Treatment days | 226.6 (10.8) | 228.7 (10.7) | t(314)= −0.14 | 0.891 | -- |
| Completed 1-year | 41.3% | 41.0% | χ2(1)=0.002 | 0.968 | 0.99 (0.63-1.55) |
|
| |||||
| Service utilization | |||||
| Individual sessions | 21.2 (1.2) | 22.2 (1.2) | t(314)=−0.60 | 0.551 | -- |
| Group sessions | 43.6 (4.2) | 39.7 (3.9) | t(314)=0.67 | 0.503 | -- |
ONSITE: Onsite Integrated Substance Abuse and Psychiatric Care; OFFSITE: Offsite Non-integrated Substance Abuse and Psychiatric Care
OR: Odds ratio; HR: Hazards Ration; CI: Confidence interval
denotes primary study outcomes
Self-report Measure of Medication Adherence (ONSITE: n=135; OFFSITE: n=94)
Psychiatric distress scores
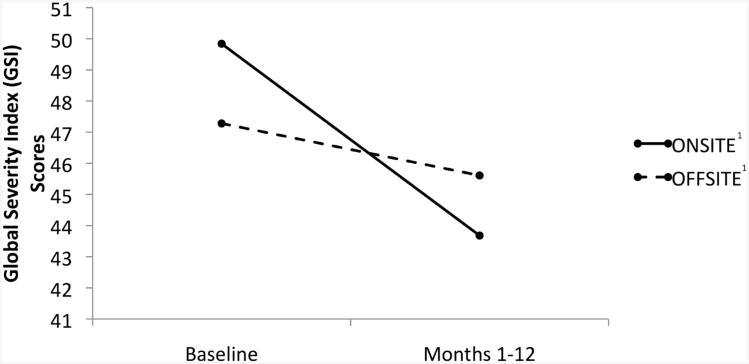
Analysis of covariance (ANCOVA) showed that on-site participants had lower follow-up mean SCL-90R GSI scores (on-site: M=43.3; SE=0.56 vs. off-site: M=45.5; SE=0.56); F (1, 286)=7.76, p=0.006). Figure 3 shows that participants in both conditions achieved significant reductions in GSI scores over time compared to baseline (on-site: t=7.13, df=314, p<0.001; off-site: t=2.86, df=314, p=0.005), although on-site participants attained much larger reductions in GSI change scores (on-site: M=4.21; SE=0.59 vs. off-site: M=1.70; SE=0.60; F (1, 314)= 8.89, p=0.003).
Figure 3.
Mean Global Severity Index (GSI) scores at baseline and Months 1-12 across study conditions (on-site: n=157 vs. off-site: n=156), with baseline GSI scores imputed at follow-up for participants with no GSI follow-up scores (on-site: n = 14; off-site: n=10). Three on-site participants with no baseline GSI scores were excluded from these analyses. Both conditions demonstrated significant reductions in GSI scores (on-site: p < .001; off-site: p = .005), with on-site participants having larger change scores (p = .003).
1ONSITE: Onsite Integrated Substance Abuse and Psychiatric Care; OFFSITE: Off-site Non-integrated Substance Abuse and Psychiatric Care
Substance abuse retention, service utilization, drug use
Only 38% of participants remained in substance abuse treatment for the entire year. As shown in Table 2, no condition differences in substance abuse treatment days or urinalysis results were observed, and both conditions had good and comparable rates of substance abuse service utilization.
Discussion
The present study of on-site and integrated versus off-site psychiatric treatment for patients in a methadone program produced mixed results. As expected, participants assigned to the on-site psychiatric condition were more likely to initiate psychiatric care and begin it sooner than those assigned to the off-site condition. Adherence data to the psychiatric treatment schedule produced diverse findings. Overall attendance to scheduled psychiatric services was disappointingly low across treatment conditions, with one exception. Attendance to psychiatrist appointments for evaluation and medication checks was significantly higher in the on-site versus off-site condition. Psychiatric and substance abuse treatment outcomes also produced a divergent set of findings. Participants in the on-site versus off-site condition had significantly greater reductions in psychiatric distress, but no condition differences were found on drug use.
Psychiatric treatment utilization and retention
The higher rate and earlier onset of psychiatric care and better psychiatric treatment retention in the on-site condition support some of the expected benefits of integrated treatment approaches [15], and dovetail with studies reporting positive relationships between good adherence to treatment schedules and improved outcomes [16-18]. Unfortunately, the low overall attendance rate to scheduled psychiatric services in the on-site condition suggests that offering them in a substance abuse treatment setting is unlikely to resolve many of the longstanding adherence problems in these patients. One exception to this pattern was higher utilization of psychiatrist appointments in the on-site condition. While this difference may have contributed to the greater reduction of psychiatric distress in the on-site condition, it may have been too little to achieve expected outcomes in drug use [11].
The fact that participants in both psychiatric treatment conditions had good attendance to the substance abuse treatment schedule despite low overall attendance rates to the psychiatric schedule is interesting, particularly because the substance abuse service schedule was often more intensive than the psychiatric protocol. While speculative, this difference in attendance data could be accounted for partly by the clinic-based attendance reinforcement used to motivate patients to attend their substance abuse counseling sessions [29,30]. Prior studies have shown that contingency management can increase attendance to a wide range of medical appointments, including substance abuse counseling [14,32-34].
Reduction in psychiatric distress
The greater reduction in psychiatric distress reported in the on-site condition extends prior work by focusing on a broader range of psychiatric diagnoses than major depression only [35-37], although major depression in the present sample accounted for half of our cases. Most importantly, this outcome was attained even though the frequency of psychiatric services was controlled across treatment settings. While prior studies focusing on mood disorder reported both positive and negative outcomes, these samples often included patients who complained of depression but did not meet diagnostic criterion for mood disorder [12]. In addition, medication in these studies was offered over a shorter period of time (i.e., 8-12 weeks) and administered without other psychiatric services (e.g., individual or group therapies).
The broader range of psychiatric diagnoses represented in the present study and the flexible and more comprehensive psychiatric service schedule we used addresses some of these limitations [10]. While the overall magnitude of improvement in this study was modest, the good outcomes in comparison to many pharmacotherapy trials support the possible benefits of combining psychiatric medications with appropriate amounts of verbal therapies [38]. The importance of achieving these positive outcomes with opioid-dependent patients is enhanced by the therapeutic nihilism that often excludes these patients from trials evaluating psychiatric treatments [39].
Substance use outcomes
The fact that reductions in psychiatric distress were unrelated to substance use outcomes was unexpected and the reasons for it are uncertain. One explanation is that psychiatric distress is only one of many factors affecting drug use in patients with opioid dependence disorder. It is also possible that reductions in psychiatric distress were too modest to change the highly entrenched patterns of drug use in people seeking methadone treatment. This view is supported by studies noting that larger reductions in psychiatric distress than observed in this report were associated with decreased drug use [11]. Conversely, the fact that all participants achieved significant reductions in psychiatric distress over time might have facilitated similarly good drug use outcomes (about 60% abstinence), and created a “ceiling effect” that limited the ability to detect group differences. Finally, prior studies of integrated care of drug use and other psychiatric problems have been conducted largely in psychiatric settings that provided less substance abuse treatment than described in this report [19,20].
Limitations and summary
One major limitation of the study is the uncertain extent to which findings will generalize to other substance-dependent populations, non-methadone treatment settings, methadone treatment settings offering less intense routine care schedules, and studies using other strategies for integrating psychiatric and substance abuse services. Our decision to control for the type and amount of psychiatric services available to participants, but neither therapy content nor medication choices, introduced unknown error variance across participants and conditions. This limitation, however, was necessary to make the psychiatric treatment protocol acceptable to staff in the community psychiatry program, and it helps extend the external validity of the findings to other community psychiatry programs. Finally, all participants leaving substance abuse treatment were removed from the study. Unfortunately, while the low substance abuse treatment retention rate (38% 1-year retention) is consistent with data from many methadone treatment programs [40], it limited the potential efficacy of psychiatric services in both conditions. It is also important to note that this low retention rate is in a highly selected sample of methadone-treated patients with comorbid psychiatric disorders.
While the study has limitations, it also has significant strengths that meaningfully extend prior work. One of the more important strengths is the randomized design that controlled for the amount of psychiatric treatment services available to participants in order to measure the effects of psychiatric treatment setting on outcomes. This design and its implementation was challenging and required extensive collaborations with staff in the community psychiatry program to develop the common psychiatric treatment protocol and maintain fidelity to it during the study. It should also be noted that the exceptionally good access to the community psychiatry program might underestimate the benefits of on-site care – access to care in community psychiatry programs is considerably less than it was in this study.
Acknowledgments
Dr. Brooner had full access to the data in this study and took responsibility for the integrity of the data and the accuracy of the data analysis. The author's have no conflicts of interest to report in this study, including any financial interests and relationships or affiliations relevant to the content of this report. The study was supported by NIH-NIDA grant R01 DA016375, PI: R. Brooner), we greatly appreciate their support for this project. The authors also thank Kori Kindbom, MA and her research staff for their consistently outstanding work in the conduct of the study. We also thank the patients who agreed to participate, the leaders and staff of the Johns Hopkins Bayview Community Psychiatry Program who made this study design possible, and lastly, the staff of the Baltimore Substance Abuse Services (bSAS) organization, a quasi-public institution overseeing the publicly supported substance abuse treatment network in Baltimore.
Funding Support: This work was supported by NIH-NIDA grant R01 DA016375 (PI: R. Brooner)
Footnotes
Declarations of Interest: None
Clinical trials registration: clinicaltrials.gov NCT00787735
References
- 1.Gowing L, Farrell MF, Bornemann R, Sullivan LE, Ali R. Oral substitution treatment of injecting opioid users for prevention of HIV infection. Cochrane Database Syst Rev. 2011;8 doi: 10.1002/14651858.CD004145.pub4. Art. No.: CD004145. [DOI] [PubMed] [Google Scholar]
- 2.McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 3.Brooner RK, King VL, Kidorf M, Schmidt CW, Bigelow GE. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Arch Gen Psychiatry. 1997;1997;54:71–80. doi: 10.1001/archpsyc.1997.01830130077015. [DOI] [PubMed] [Google Scholar]
- 4.McGovern MP, Xie H, Segal SR, Siembab L, Drake RE. Addiction treatment services and co-occurring disorders. J Subst Abuse Treat. 2006;31:267–275. doi: 10.1016/j.jsat.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Bohnert AS, Ilgen MA, Ignacio RV, McCarthy JF, Valenstein M, Blow FC. Risk of death from accidental overdose associated with psychiatric and substance use disorders. Am J Psychiatry. 2012;169:64–70. doi: 10.1176/appi.ajp.2011.10101476. [DOI] [PubMed] [Google Scholar]
- 6.Cacciola JS, Alterman AI, Rutherford MJ, McKay JR, Mulvaney FD. The relationship of psychiatric comorbidity to treatment outcomes in methadone maintained patients. Drug Alcohol Depend. 2001;61:271–280. doi: 10.1016/s0376-8716(00)00148-4. [DOI] [PubMed] [Google Scholar]
- 7.Carpentier PJ, Krebbe PF, van Gogh MT, Knapen LJ, Buitelaar JK, de Jong CA. Psychiatric comorbidity reduces quality of life in chronic methadone maintained patients. Am J Addict. 2009;18:470–480. doi: 10.3109/10550490903205652. [DOI] [PubMed] [Google Scholar]
- 8.Compton WM, Cottler LB, Jacobs JL, Ben-Abdallah A, Spitznagel EL. The role of psychiatric disorders in predicting drug dependence treatment outcomes. Am J Psychiatry. 2003;160:890–895. doi: 10.1176/appi.ajp.160.5.890. [DOI] [PubMed] [Google Scholar]
- 9.Rounsaville BJ, Weissmann MM, Crits-Chritoph K, Wilber H, Kleber HD. Disgnosis and symptoms of depression in opiate addicts: course and relationship to treatment outcome. Arch Gen Psychiatry. 1982;39:151–156. doi: 10.1001/archpsyc.1982.04290020021004. [DOI] [PubMed] [Google Scholar]
- 10.Practice guideline for the treatment of patient with major depressive disorder. 3rd. Arlington, VA: American Psychiatric Association (APA); 2010. Oct, American Psychiatric Association (APA) p. 152. [Google Scholar]
- 11.Nunes EV, Levin FR. Treatment of depression in patients with alcohol or other drug dependence. JAMA. 2004;291:1887–1896. doi: 10.1001/jama.291.15.1887. [DOI] [PubMed] [Google Scholar]
- 12.Pedrelli P, Iovieno N, Vitali M, Tedeschini E, Bentley KH, Papakostas GI. Treatment of major depressive disorder and dysthymic disorder with antidepressants in patients with comorbid opiate use disorders enrolled in methadone maintenance therapy: A meta-analysis. J Clin Psychopharmacol. 2011;31:582–586. doi: 10.1097/JCP.0b013e31822c0adf. [DOI] [PubMed] [Google Scholar]
- 13.Pringle JL, Emptage NP, Hubbard RL. Unmet needs for comprehensive services in outpatient addiction treatment. J Subst Abuse Treat. 2006;30:183–189. doi: 10.1016/j.jsat.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Kidorf M, King VL, Brooner RK. Counseling and psychosocial services. In: Strain EC, Stitzer ML, editors. The Treatment of Opioid Dependence. Baltimore, MD: Johns Hopkins University Press; pp. 2006pp. 119–150. [Google Scholar]
- 15.Sacks S, Chandler R, Gonzales J. Responding to the challenge of co-occurring disorders: Suggestions for future research. J Subst Abuse Treat. 2008;34:139–146. doi: 10.1016/j.jsat.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Killaspy H, Banerjee S, King M, Lloyd M. Prospective controlled study of psychiaric out-patient non-attendance. Br J Psychiatry. 2000;176:160–165. doi: 10.1192/bjp.176.2.160. [DOI] [PubMed] [Google Scholar]
- 17.Lydecker KP, Tate SR, Cummins KM, McQuaid J, Granholm E, Brown SA. Clinical outcomes of an integrated treatment for depression and substance use disorders. Psychol Addict Behav. 2010;24:453–465. doi: 10.1037/a0019943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stein MD, Solomon DA, Herman DS, et al. Pharmacotherapy plus psychotherapy for treatment of depression in active injection drug users. Arch Gen Psychiatry. 2004;61:152–159. doi: 10.1001/archpsyc.61.2.152. [DOI] [PubMed] [Google Scholar]
- 19.Donald M, Dower J, Kavanagh D. Integrated versus non-integrated management and care for clients with co-occurring mental health and substance use disorders: A qualitative systematic review of randomized controlled trials. Soc Sci Med. 2005;60:1371–1383. doi: 10.1016/j.socscimed.2004.06.052. [DOI] [PubMed] [Google Scholar]
- 20.Drake RE, O'Neal EL, Wallach MA. A systematic review of psychosocial research on psychosocial interventions for people with co-occurring severe mental and substance use disorders. J Subst Abuse Treat. 2008;34:123–138. doi: 10.1016/j.jsat.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 21.Mueser KT, Glynn SM, Cather C, et al. A randomized controlled trial of family intervention for co-occurring substance use and severe psychiatric disorders. Schizophrenia Bulletin. 2012:1–15. doi: 10.1093/schbul/sbr203. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brooner RK, Kidorf M. Using behavioral reinforcement to improve methadone treatment participation. Sci Pract Perspect. 2002;1:38–48. doi: 10.1151/spp021138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis Disorders - Patient Edition(SCID-I/P, Version 2.0) New York State Psychiatric Institute; 1995. [Google Scholar]
- 24.Derogatis LR. SCL-90-R Administration, scoring, and procedures manual II. 2nd. Baltimore, MD: Clinical Psychometric Research; 1983. [Google Scholar]
- 25.Derogatis LR, Cleary P. Confirmation of the dimensional structure of the SCL-90: A study in construct validation. J Clin Psychol. 1977;33:981–989. [Google Scholar]
- 26.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Kidorf M, Disney ER, King VL, Neufeld K, Beilenson PL, Brooner RK. Prevalence of psychiatric and substance use disorders in opioid abusers in a community syringe exchange program. Drug Alcohol Depend. 2004;74:115–122. doi: 10.1016/j.drugalcdep.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 28.Center for Substance Abuse Treatment. Substance abuse treatment for persons with co-occurring disorders. Substance Abuse and Mental Health Services Administration (US) Treatment Improvement Protocol (TIP) Series. 2005 [PubMed] [Google Scholar]
- 29.Brooner RK, Kidorf MS, King VL, et al. Behavioral contingencies improve counseling attendance in an adaptive treatment model. J Subst Abuse Treat. 2004;27:223–232. doi: 10.1016/j.jsat.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 30.Brooner RK, Kidorf MS, King VL, Stoller KB, Neufeld K, Kolodner K. Comparing adaptive stepped care and monetary voucher interventions in the treatment of opioid dependent outpatients. Drug Alcohol Depend. 2007;88S:S14–S23. doi: 10.1016/j.drugalcdep.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Singer JD, Willett JB. Modeling the days of our lives: Using survival analysis when designing and analyzing longitudinal studies of duration and the timing of events. Psychol Bull. 1991;110:268–290. [Google Scholar]
- 32.Bellack AS, Bennett ME, Gearon JS, Brown CH, Yang Y. A randomized clinical trial of a new behavioral treatment for drug abuse in people with severe and persistent mental illness. Arch Gen Psychiatry. 2006;63:426–432. doi: 10.1001/archpsyc.63.4.426. [DOI] [PubMed] [Google Scholar]
- 33.Helmus TC, Saules KK, Schoener EP, Roll JM. Reinforcement of counseling attendance and alcohol abstinence in a community-based dual-diagnosis treatment program: A feasibility study. Psychol Addict Behav. 2003;17:249–251. doi: 10.1037/0893-164X.17.3.249. [DOI] [PubMed] [Google Scholar]
- 34.Sorensen JL, Haug NA, Delucchi KL, et al. Voucher reinforcement improves medication adherence in HIV-positive methadone patients: A randomized trial. Drug Alcohol Depend. 2007;88:54–63. doi: 10.1016/j.drugalcdep.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carpenter KM, Brooks AC, Vosburg SK, Nunes EV. The effect of sertraline and environmental context on treating depression and illicit substance use among methadone maintained opiate dependent patients: a controlled clinical trial. Drug Alcohol Depend. 2004;74:123–134. doi: 10.1016/j.drugalcdep.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 36.Nunes EV, Quitkin FM, Donovan SJ, et al. Imipramine treatment of opiate-dependent patients with depressive disorders. Arch Gen Psychiatry. 1998;55:153–160. doi: 10.1001/archpsyc.55.2.153. [DOI] [PubMed] [Google Scholar]
- 37.Petrakis I, Carroll KM, Nich C, Gordon L, Kosten T, Rounsaville B. Fluoxetine treatment of depressive disorders in methadone maintained opioid addicts. Drug Alcohol Depend. 1998;50:221–226. doi: 10.1016/s0376-8716(98)00032-5. [DOI] [PubMed] [Google Scholar]
- 38.Pampallona S, Bollini P, Tibaldi G, Kupelnick B, Munizza C. Combined pharmacotherapy and psychological treatment for depression: A systematic review. Arch Gen Psychiatry. 2004;61:714–719. doi: 10.1001/archpsyc.61.7.714. [DOI] [PubMed] [Google Scholar]
- 39.Beaulieu S, Saury S, Sareen J, et al. The Canadian network for mood and anxiety treatments (CANMAT) task force recommendations for the management of patient with mood disorders and comorbid substance use disorders. Ann Clin Psychiatry. 2012;24:38–55. [PubMed] [Google Scholar]
- 40.Farre M, Mas A, Torrens M, Moreno V, Cami J. Retention rate and illicit opioid use during methadone maintenance interventions: a meta-analysis. Drug Alcohol Depend. 2002;65:283–290. doi: 10.1016/s0376-8716(01)00171-5. [DOI] [PubMed] [Google Scholar]