Abstract
This study examined the efficacy of teaching emotional self-regulation techniques supported by heart rhythm coherence training (emWave Personal Stress Reliever) as a means to quickly lower blood pressure (BP) in patients diagnosed with hypertension. Previous studies have demonstrated systemic reductions in BP in both high stress populations and patients diagnosed with hypertension using this approach, but to the best of our knowledge, an investigation of their ability to produce immediate reductions in BP had not been published in the medical literature.
The study was a randomized controlled design with 62 hypertensive participants who were divided into three groups. Group 1 was taking hypertensive medication, was taught self-regulation technique, and used heart rate variability coherence (HRVC) training devices. Group 2 was not yet taking medication and was trained in the same intervention. Group 3 was taking hypertensive medication but did not receive the intervention and was instructed to relax between the BP assessments.
An analysis of covariates was conducted to compare the effectiveness of three different interventions on reducing the participants' BP. The use of the self-regulation technique and the HRVC-monitoring device was associated with a significantly greater reduction in mean arterial pressure in the two groups who used the intervention as compared with the relaxation-plus-medication group. Additionally, the group not taking medication that used the intervention also had a significantly greater reduction in systolic BP than the relaxation- plus-medication group.
These results suggest that self-regulation techniques that incorporate the intentional generation of positive emotions to facilitate a shift into the psychophysiological coherence state are an effective approach to lowering BP. This approach to reducing BP should be considered a simple and effective approach that can easily be taught to patients to quickly lower their BP in stressful situations. The technique should be especially useful when hypertensive patients are experiencing stressful emotions or reactions to stressors. It is possible that the BP reductions associated with the use of the technique leads to a change in the physiological set-point for homeostatic regulation of BP. Further studies should examine if large scale implementations of such heart-based coherence techniques could have a significant impact on reducing risk of mortality and morbidity in hypertensive patients.
Key Words: Hypertension, blood pressure, anxiety, stress, coronary heart disease, heart attack, stroke, kidney disease, coherence, HeartMath, function, balance
摘要
本研究考察了以心律和谐训练 (emWave 个人压力释放器)为支持 传授自我调节情绪技巧以快速降低 高血压患者血压 (blood pressure, BP) 的效果。此前研究证实,高压 力人群和被确诊的高血压患者使用 这种方法均可降低全身血压 (BP) ,而在此之前他们并没有接受过立 即降低血压 (BP) 的能力调研。
本研究的设计是将 62 名高血 压参与者分为三组进行随机对照研 究。第 1 组服用高血压药物,被 传授自我调节技巧,并使用心率变 异性和谐 (heart rate variability coherence, HR VC) 训练设备。 第 2 组未服药,但接受相同的干 预训练。第 3 组服用高血压药 物,但不接受干预训练,并被指示 在血压 (BP) 评估之间保持放松。
本研究进行了共变数分析,比 较三种不同的干预措施对降低参与 者血压 (BP) 的有效性。就平均动 脉压而言,采用干预措施的两个小 组较采用放松加药物治疗的小组显 著降低,显示出其与使用自我调节 技巧和心率变异性和谐 (HR VC) 监 测设备存在联系。此外,就收缩血 压 (BP) 而言,采用未服药但接受 干预措施的小组也比采用放松加药 物治疗的小组显著降低。
这些结果表明,自我调节技巧 采用有意识调动积极情绪的手段帮 助达到身心和谐的状态,是降低血 压 (BP) 的一种有效方法。这种降 低血压 (BP) 的方法被认为是一种 可以轻松教会患者在紧张的情况下 迅速降低血压 (BP) 的简单而有效 的方法。这种技巧在高血压患者情 绪紧张或应对压力时特别有用。使 用该技巧降低血压 (BP) 可能会导 致血压 (BP) 稳态调节生理设定点 的变化。如果大规模实施这种基于 内心的和谐技巧可能显著降低高血 压患者的死亡率和发病率风险,则 应实施进一步的研究。
SINOPSIS
Este estudio examinó la eficacia de enseñar las técnicas de auto-regulación emocional, apoyadas por el entrenamiento de la coherencia de ritmos del corazón (emWave Personal Stress Reliever), como medio para reducir con rapidez la presión arterial (PA) en pacientes diagnosticados con hipertensión. Los estudios previos han demostrado reducciones sistémicas de la PA tanto en poblaciones con alto estrés como en pacientes diagnosticados con hipertensión, después de usar este enfoque pero no se ha investigado todavía la capacidad de causar reducciones inmediatas de la PA.
El estudio se llevó a cabo con 62 participantes hipertensos mediante un diseño controlado aleatorizado, que los dividió en tres grupos. El grupo 1 estaba tomando medicación para la hipertensión, se le enseñó la técnica de auto-regulación y utilizó aparatos de entrenamiento de coherencia de la variabilidad de la frecuencia cardiaca (heart rate variability coherence, HRVC). El grupo 2 no tomaba todavía ninguna medicación y se entrenó en el mismo procedimiento. El grupo 3 estaba tomando medicación para la hipertensión, pero no recibió la intervención y se le enseñó a relajarse entre las evaluaciones de la PA.
Se realizó un análisis de covarianza para comparar la eficacia de los tres tipos distintos de intervención para reducir la PA de los participantes. El uso de la técnica de auto-regulación y del aparato de control de la HRVC se asoció a una reducción significativamente mayor de la media de la presión arterial en los dos grupos que utilizaron la intervención, en comparación con el grupo con la medicación y la relajación. Además, el grupo que no tomaba medicación, pero que utilizó la intervención, mostró también una reducción significativamente mayor en la PA sistólica que el grupo con la medicación y la relajación.
Estos resultados sugieren que las técnicas de auto-regulación, que incorporan la generación intencional de emociones positivas para facilitar un cambio hacia el estado de coherencia psicofisiológico son un enfoque eficaz para reducir la PA. Este enfoque para reducir la PA se debe considerar un planteamiento simple y eficaz, que puede enseñarse fácilmente a los pacientes, para reducir rápidamente su PA en situaciones de estrés. Esta técnica debería ser útil especialmente en los casos en los que los pacientes hipertensos sufren emociones estresantes o reacciones ante situaciones de estrés. Es posible que las reducciones de la PA, asociadas al uso de la técnica, causen un cambio en el punto fisiológico establecido, que controla la regulación homeostática de la PA. Los estudios adicionales deberían examinar si las implementaciones a gran escala de dichas técnicas de coherencia basadas en el ritmo cardíaco podrían tener un impacto significativo en la reducción del riesgo de mortalidad y morbilidad en los pacientes hipertensos.
Hypertension is considered one of the most prominent public health issues faced by the world today. It affects approximately 1 in 4 adults,1 and current trends suggest that the number of adults diagnosed with high blood pressure (BP) is increasing.2 High BP is a major risk factor for death and disability related to coronary heart disease, heart attacks, strokes, kidney disease, and vascular complications.1 In addition, high systolic BP has been linked with decreased cognitive performance, memory loss, and the loss of healthy brain tissue.3,4 Conversely, reducing BP in hypertensive individuals has been found to significantly reduce the risk of death and disability and is therefore a critically important factor in long-term health and wellness.4–7
There is considerable evidence to suggest that high BP is linked to persistent stress and the ways in which people cope.8–12 Behavioral interventions that reduce stress and sympathetic arousal have been shown to be effective nonpharmacological treatments for hypertension; such treatments have been associated with clinically significant and sustainable BP reductions as well as lowered health-care costs.13–18
Interventions utilizing HeartMath self-regulation techniques and heart rhythm coherence monitoring technology to reduce stress and increase physiological stability and efficiency have been shown in a number of previous studies to significantly improve key markers of health and wellness, such as immune function,19 autonomic nervous system (ANS) function and balance,20,21 reductions in stress hormones,22 and reductions in both systolic and diastolic BP. For example, in a population of correctional officers with high work-place stress, reductions in total cholesterol, glucose, and both systolic and diastolic BP, as well as significant reductions in overall stress, anger, fatigue, and hostility, were found, which resulted in projected savings in annual health-care costs of $1179 US per employee.23 Another workplace study of employees with clinical diagnoses of hypertension showed significant reductions in BP and a wide range of stress measures.24 Reduced healthcare utilization and costs were also found in a study of pastors who used the coherence monitoring device (emWave) to support learning of the stress self-regulation tools. In addition to a number of significant improvements in stress and well-being measures, the group receiving the HeartMath training showed an overall decrease in health-care costs of 3.8% (resulting in an annual cost savings of $585 US per participant); the control group had a 9% increase in health-care costs. The largest reduction in costs was related to reductions in medication for treating hyper-tension.25 The studies briefly described above focused on long-term BP reductions; however, potential reductions of BP that may be directly associated with use of the techniques and the coherent state have not been previously investigated. This study was therefore undertaken to determine if immediate reductions in BP were associated with positive emotions and the coherent state. The research team believed that such a study would help inform a physiologically based theory of why positive emotions and the coherent state can lead to long-term reductions in BP and healthcare costs.
Our theoretical framework is grounded in the existence of a dynamic communication network between the cognitive, emotional, and physiological systems wherein the physiological state of coherence is reflected in increased harmony and a global order, viewed as a distinctive mode of function. Both positive and negative emotions are deeply rooted under our physiological processes that are related to fluidity and strain (stress) of the life process.26,27 Many of the difficult situations and challenges that one faces that can result in stressful feelings such as anger, irritation, anxiety, etc, have been linked to increased risk of heart attacks, hypertension, and cardiovascular disease.28 On the other hand, positive emotions are associated with increased efficacy and stability in cardiovascular functioning.26,29,30 Thus, techniques that allow patients to self-regulate emotions and induce a state of coherence may provide a novel nonpharmacological approach that can help control acute BP increases and hypertension.
The Institute of HeartMath (IHM) introduced the term physiological coherence to describe the degree of order, harmony, and stability in the various rhythmic activities within living systems over any given time period.20 This harmonious order signifies a more coherent system whose efficient or optimal function is directly related to the ease and flow in life processes. By contrast, an erratic, discordant pattern of activity denotes an incoherent system whose function reflects stress and inefficient utilization of energy in life processes.20,26,27,31 In our experience in working with patients, we have also observed that positive emotions as opposed to negative emotions such as anxiety and anger are indeed reflected in heart rhythm patterns that are more coherent.
Physiological correlates of this coherence mode include a shift in autonomic balance toward increased parasympathetic activity, increased heart-brain synchronization, increased vascular resonance, and entrainment between diverse physiological oscillatory systems.26
Based on the understanding of the physiological interactions between heart, brain, and emotional physiology, IHM has developed series of techniques to provide a systematic process that enables people to shift into a more coherent state and increase their ability to better self-regulate stress and improve performance.32–34 Most of these techniques include the intentional generation of a heartfelt positive emotional state combined with a shift in attentional focus to the area of the heart (where many people subjectively experience positive emotions). This shift in feeling allows the coherence mode to emerge naturally and helps to reinforce the inherent associations between physiological coherence and positive feelings. The coherent state indeed appears to be associated with the patient's subjective feeling of positive emotions. We have found that although the breathing rhythm can be used to induce a more coherent state, for some patients, the induction of a positive feeling was the key to their success in both shifting to a more coherent state and sustaining it for longer periods. These changes in rhythmic patterns are independent of heart rate (HR); that is, one can have a coherent or incoherent pattern at higher or lower HRs. Thus, it is the pattern of the rhythm (the ordering of changes in rate over time) rather than the rate (at any point in time) that is most directly related to emotional dynamics and physiological harmony.
The techniques used in the study draw on HeartMath's interventions that have been shown to be effective in reducing BP in individuals with hypertension. The objective of this training was to teach patients the ability to shift into a more coherent state in stressful situations in order to reduce acute BP increases.24 Learning self-regulation skills can be facilitated with the use of heart rhythm coherence feedback monitors that display heart rhythm in real time and determine the level of heart rhythm coherence achieved. Heart-rate variability (HRV) coherence feedback has been shown to significantly improve outcomes in a number of clinical populations such as patients with posttraumatic stress disorder,35–37 depression,38,39 asthma,40–43 congestive heart failure,44,45 hypertension,24 anxiety,33 fibromyalgia,46 and insomnia.47
The device used in this study was the emWave Personal Stress Reliever (PSR) (Figure 1), which helps patients acquire the self-regulation skills for reducing emotional stress by displaying their level of heart rhythm coherence in real time as they practice the techniques. The device uses either a fingertip or ear lobe sensor to detect the pulse wave. The device records the HR on a beat-to-beat basis (the interbeat interval). As patients practice the techniques, they can readily see and experience the changes in their heart rhythm patterns, which generally become smoother and more sine wave-like as they feel appreciation and other positive emotions. The real-time physiological feedback also essentially takes the guesswork out of the process of self-inducing a positive emotional state, resulting in greater consistency and effectiveness in practicing emotional shifts.
Figure 1.

The emWave Personal Stress Reliever.
METHODS
The sample investigated in this study was selected at random from the cardiac center registry at the Prince Sultan Cardiac Center in Hufuf, Saudi Arabia, for potential inclusion in the study. The inclusion criteria for hypertension were a systolic BP of greater than 140 or a diastolic BP of greater than 90. Sixty-two patients were recruited to participate in the study. Prior to the experiment, the examiner explained to the patients the aim of the study and the procedures they would be asked to participate in.
This population of confirmed hypertension patients was then randomly divided into 3 groups. Group 1 (n = 30) was currently taking hypertensive medication as prescribed by their physicians, was taught the self-regulation technique called Quick Coherence (QC),34 and practiced with the emWave PSR device (HeartMath LLC, Boulder Creek, California). Group 2 (n = 12) was not yet taking any medication to control hypertension and was given the same training and emWave practice. Group 3 (n = 20) was taking medication as prescribed and was asked to use a method of relaxation that was familiar to them.
The sex ratio was almost 50:50: 32 males vs 30 females. The age range of participants was between 24 and 85 years (mean age 55), and body mass index (BMI) ranged from 20 to 51 with a mean of 33 kg/m2. Most of the participants were nonsmokers, and the number of diabetic patients was approximately equal among the 3 groups.
Patients were instructed to sit on a chair and rest for 10 minutes after which their BP, HR, and oxygen saturation (SpO2) were measured. During the data collection procedure, the patient was asked to stay calm and rest the mind and body from any emotional concerns. Once the baseline data had been collected, the participants in groups 1 and 2 were reconnected to an emWave device and asked to use the steps of the QC technique to activate a positive feeling and increase their heart rhythm coherence levels as reflected in the emWave device. The technique has 3 basic steps: first, patients focus attention in the area of the heart; second, patients focus attention to the center of the chest and pretend they are breathing through this area; third, patients intentionally activate a positive feeling, such as appreciation or care for someone or some place. The emphasis is put on actually experiencing the positive feeling. The emWave PSR device has an indicator light that shows the current level of coherence as either red (low coherence), blue (medium coherence), or green (high coherence). The indicator changes from red to blue or green as patients successfully increase their coherence level. While rhythmic breathing exercises can help lower HR and have a calming effect, shifting attitudes and emotions neutralize and counter the effects of stress by actively adding to the process a positive feeling such as appreciation, care, or compassion.
After the patients had practiced using the QC technique for a 5-minute period, their BP, HR, and SpO2 were again measured in same manner. For group 3, relaxation plus medication, the same data collection procedures were followed, with the exception that patients in this group were asked to sit quietly and to practice using a familiar method of relaxing for a 5-minute period.
We observed that only focusing on rhythmic breathing was difficult for some patients to maintain for more than about 1 minute. However, when these individuals were able to intentionally invoke a positive emotional state, they were usually able to maintain a more coherent state for greater periods of time. When patients in groups 1 and 2 were having difficulty achieving the coherence state, the examiner encouraged them to try to forget about the hospital environment and to imagine themselves gathered with their families in a natural setting (eg, at a farm or in a park) and experience how that felt. In some cases, patients were also asked to recite Islamic prayers aloud. They were then asked to stop their tongue movements and focus only on the abstract meaning of the words and how they felt in their hearts (the Imam Ghazali method for contemplation) until they reached a state of transcendence wherein they felt connected to a higher power beyond themselves. When they were able to evoke a positive feeling, participants were typically able to shift into a more coherence state much easier.
Statistical Analysis and Results
Baseline characteristics for the 3 groups are presented in Table 1. A chi-square test was first used to compare the baseline characteristic of the 3 groups on gender, smoking status (nonsmoker, ex-smoker, and smoker), and diabetic status. The gender balance between the 3 groups did not significantly differ (χ2 = 0.07, P = .97). Smoking status also did not differ significantly between the groups (χ2 = 2.747, P = .601), nor did the ratio of diabetics (χ2 = 0.523, P = .770).
Table 1.
Baseline Characteristics of the Three Groups
| Group 1 (N = 30) | Group 2 (N = 12) | Group 3 (N = 20) | |
|---|---|---|---|
| Age, years (SD) | 54.8 (11.91) | 51.0 (16.30) | 50.5 (9.44) |
| Gender, % male | 53 | 50 | 50 |
| Smoking status | |||
| Nonsmoker, % | 80 | 67 | 75 |
| Ex-smoker, % | 3 | 17 | 5 |
| Smoker, % | 17 | 17 | 20 |
| Diabetic, % | 50 | 50 | 60 |
A single-factor analysis of variance comparison was used to test baseline differences for participants age, systolic and diastolic BP, mean arterial pressure (MAP, systolic + [2 × diastolic]/3), HR, and SpO2. There were no significant differences in the ages of the participants in the 3 groups (F = 0.906, P = .410) or BP measure, as shown in Table 2.
Table 2.
Baseline Comparisons of Three Groups' Outcome Measures
| Systolic BP (mm Hg) | Diastolic BP (mm Hg) | MAP (mm Hg) | Heart Rate (BPM) | SpO2 % | |
|---|---|---|---|---|---|
| Group 1 (N = 30) | |||||
| Mean | 156.90 | 87.67 | 111.26 | 79.30 | 98.00 |
| SEM | 4.07 | 3.00 | 2.87 | 2.93 | 0.35 |
| Lower 95% CI | 148.56 | 81.53 | 105.39 | 73.31 | 97.29 |
| Upper 95% CI | 165.24 | 93.81 | 117.14 | 85.29 | 98.71 |
| Group 2 (N = 12) | |||||
|---|---|---|---|---|---|
| Mean | 142.50 | 81.42 | 101.78 | 78.67 | 98.67 |
| SEM | 5.60 | 3.77 | 4.08 | 5.71 | 0.51 |
| Lower 95% CI | 130.18 | 73.11 | 92.79 | 66.09 | 97.54 |
| Upper 95% CI | 154.82 | 89.73 | 110.76 | 91.24 | 99.79 |
| Group 3 (N = 20) | |||||
|---|---|---|---|---|---|
| Mean | 153.20 | 93.65 | 113.50 | 80.10 | 98.60 |
| SEM | 4.33 | 3.30 | 3.07 | 2.68 | 0.28 |
| Lower 95% CI | 144.14 | 86.74 | 107.07 | 74.49 | 98.00 |
| Upper 95% CI | 162.26 | 100.56 | 119.93 | 85.71 | 99.20 |
| Between-groups ANOVA | |||||
|---|---|---|---|---|---|
| Mean Sq | 881.39 | 576.29 | 550.79 | 8.24 | 2.99 |
| F | 2.07 | 2.45 | 2.56 | 0.03 | 1.06 |
| P < | NS | NS | NS | NS | NS |
Abbreviations: ANOVA, analysis of variance; BP, blood pressure; BPM, beats per minute; CI, confidence interval; MAP, mean arterial pressure; NS, not significant; SEM, standard error of the mean; Sq, square.
A 1-way between-groups analysis of covariance was conducted to compare the effectiveness of 3 different interventions on reducing the participant BP (Table 3). The independent variable (grouping factor) was intervention type (group 1, coherence training plus currently taking hypertensive medication; group 2, coherence training alone; and group 3, relaxation plus currently taking hypertensive medication). The dependent variables consisted of systolic and diastolic BP, MAP, HR, and SpO2 taken after the intervention was completed. Participants' preintervention measurements of systolicand diastolic BP, MAP, HR, and SpO2 were used as the covariates. Bonferroni adjustment for between-groups pairwise comparisons are presented in Table 4.
Table 3.
Results of the Between-groups Analysis of Covariance
| Post-study Between-groups Results | |||||
|---|---|---|---|---|---|
| Systolic BP (mm Hg) | Diastolic BP (mm Hg) | MAP (mm Hg) | Heart Rate (BPM) | SpO2 % | |
| Group 1 (N = 30) | |||||
| Mean | 137.75 | 82.35 | 101.01 | 78.43 | 98.84 |
| SEM | 2.12 | 1.12 | 1.14 | 1.27 | 0.22 |
| Lower 95% CI | 133.51 | 80.11 | 98.74 | 75.90 | 98.40 |
| Upper 95% CI | 141.98 | 84.59 | 103.29 | 80.97 | 99.28 |
| Group 2 (N = 12) | |||||
|---|---|---|---|---|---|
| Mean | 132.49 | 82.22 | 99.72 | 77.44 | 98.55 |
| SEM | 3.34 | 1.80 | 1.82 | 2.00 | 0.33 |
| Lower 95% CI | 125.80 | 78.61 | 96.07 | 73.43 | 97.88 |
| Upper 95% CI | 139.18 | 85.83 | 103.37 | 81.45 | 99.21 |
| Group 3 (N = 20) | |||||
|---|---|---|---|---|---|
| Mean | 144.00 | 86.35 | 105.70 | 78.14 | 98.58 |
| SEM | 2.52 | 1.40 | 1.38 | 1.55 | 0.26 |
| Lower 95% CI | 138.95 | 83.55 | 102.94 | 75.03 | 98.06 |
| Upper 95% CI | 149.05 | 89.14 | 108.47 | 81.25 | 99.09 |
| Between-groups ANCOVA | |||||
|---|---|---|---|---|---|
| Mean Sq | 516.41 | 104.07 | 172.45 | 4.19 | 0.53 |
| F | 4.06 | 2.78 | 4.61 | 0.09 | 0.40 |
| P < | .05 | NS | .05 | NS | NS |
| Eta Sq | 0.125 | 0.087 | 0.139 | 0.003 | 0.014 |
Abbreviations: ANCOVA, analysis of covariance; BP, blood pressure; BPM, beats per minute; CI, confidence interval; MAP, mean arterial pressure; NS, not significant; SEM, standard error of the mean; Sq, square.
Table 4.
Preintervention-to-postintervention Mean Differencesa
| Mean Difference | |||||
|---|---|---|---|---|---|
| Systolic BP (mm Hg) | Diastolic BP (mm Hg) | MAP (mm Hg) | Heart Rate (BPM) | SpO2 % | |
| Group 1 vs Group 2 | |||||
| Mean | 5.26 | 0.13 | 1.29 | 0.99 | 0.29 |
| SEM | 4.01 | 2.12 | 2.16 | 2.37 | 0.40 |
| P < | NS | NS | NS | NS | NS |
| Group 1 vs Group 3 | |||||
|---|---|---|---|---|---|
| Mean | –6.25 | –4.00 | –4.69 | 0.29 | 0.26 |
| SEM | 3.29 | 1.79 | 1.78 | 2.00 | 0.34 |
| P < | NS | NS | .05 | NS | NS |
| Group 2 vs Group 3 | |||||
|---|---|---|---|---|---|
| Mean | –11.51 | –4.13 | –5.98 | –0.70 | –0.03 |
| SEM | 4.19 | 2.32 | 2.32 | 2.54 | 0.42 |
| P < | .05 | NS | .05 | NS | NS |
Bonferroni adjustment for multiple comparisons.
Group 1, intervention + current medication. Group 2, intervention only.
Group 3, relaxation + current medication.
Abbreviations: BP, blood pressure; BPM, beats per minute; MAP, mean arterial pressure; NS, not significant; SEM, standard error of the mean.
Preliminary checks were conducted, and no violation of the assumptions of homogeneity of regression slopes was found. As shown in Table 3, after adjusting for preintervention scores, there was a significant difference between intervention groups on postintervention systolic BP (F = 4.06, P > .05), a solid medium effect (partial eta squared = .125). As shown in Table 4, the pairwise comparisons show a between-group difference; postintervention in systolic BP for group 2 (coherence training alone), which was significantly lower than that of group 3 (relaxation plus current medication) (P < .05). There was also a significant difference between groups on postintervention MAP (F = 4.61 P > .05), partial eta squared = .139, indicating a strong effect with group 1 (coherence training plus current medication) having significantly lower MAP than group 3 (relaxation plus medication), (P < .05). Postintervention MAP was also significantly lower in group 2 (coherence training alone) than group 3 (relaxation plus current medication), (P < .05). No significant between-group differences were found for diastolic BP, HR, or SpO2. The preintervention-to-postintervention changes in systolic, diastolic, and MAP are illustrated in Figure 2.
Figure 2.
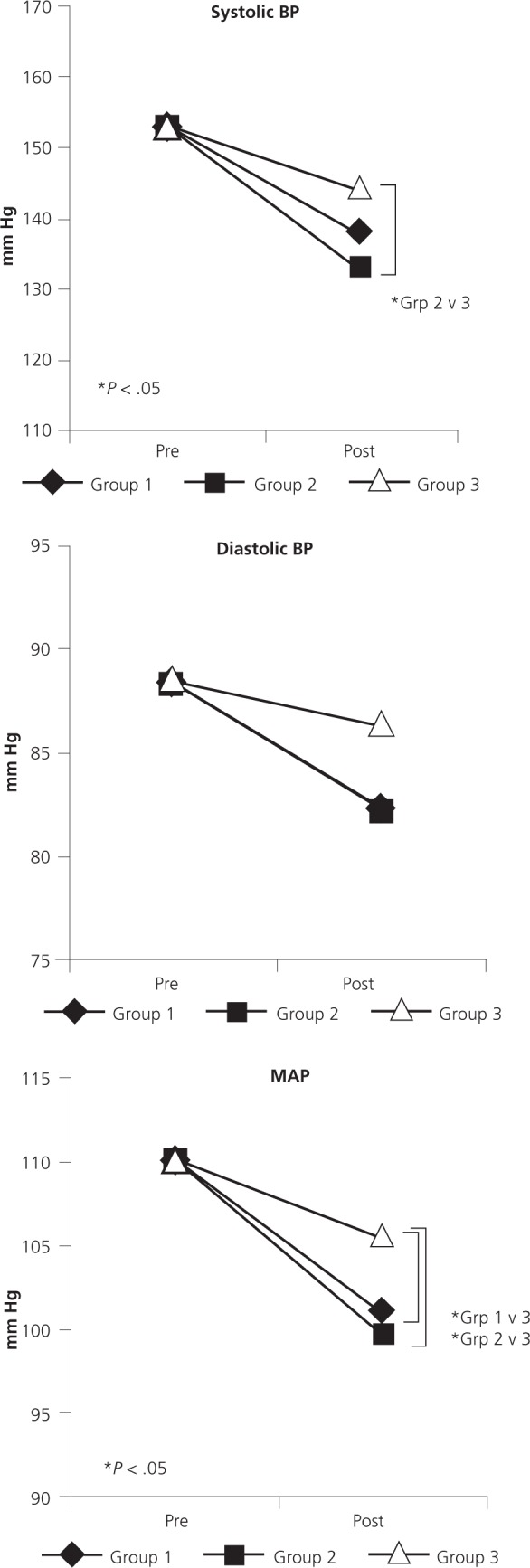
Preintervention-to-post intervention changes in systolic, diastolic, and mean arterial blood pressure (BP).
Abbreviation: MAP, mean arterial pressure.
DISCUSSION
This study was designed to evaluate a short-term BP reduction strategy in confirmed hypertensive patients who were briefly taught how to intentionally shift to and maintain a more coherent state by self-generating a heart-focused positive emotional state, facilitated via the handheld emWave device.
The results showed that use of the QC technique was associated with significant short-term reductions in BP and that patients could quickly learn and use the technique to shift into a more coherent state. We also found that using the emWave device was a highly effective method to facilitate to the patient's ability to make the shift, as it provided an objective measure of their success in achieving coherence.
Patient levels of emotional stress are clearly an important and modifiable risk factor for acute and chronic adverse cardiovascular disorders. Even though there are only a few well-controlled studies of stress-reduction in the management of patients with or at risk for cardiovascular disease, ample evidence exists for a strong and consistent association of acute and chronic psychological stress with cardiovascular risk factors such as hypertension and insulin resistance and with outcomes such as ischemia, arrhythmia, and pump failure.28 There is no doubt that stressful situations can cause BP to spike temporarily, but there is no widespread agreement yet that a consistent pattern of these stress-related transient BP increases can cause long-term high BP. In other words, can all those short-term stress-related BP spikes add up to changing an internal BP set-point and cause high BP in the long term?
Physiological set-point models have a long history in medicine and were expanded to include emotional experience, perception, and behavior by Karl Pribram in the late 1960s.48 Simply put, in Pribram's model, a memory or stable pattern of activity is formed and maintained in the neural architecture of the brain as we gain experience both in internal self-regulation and in interacting with the external environment. These stable patterns are updated and modified as we encounter new experiences and learn how a certain action usually leads to a specific result. All ongoing or current sensory input to the brain from both the internal and external sensory systems is compared to these stable patterns. These stable patterns create a set of “expectancies” against which breathing, eating, drinking, sleeping, alertness and sexual and other behaviors are evaluated.
Pribram also suggested that physiological control systems work in the same way and that neural circuits at the brain stem level regulate the patterns or set-points to which physiological parameters such as BP or respiration rate are compared. Importantly, he also showed that there are significant interactions between the neural systems that contain the set-points that regulate emotion and behavior and the systems that regulate physiological systems. The degree of match or mismatch between current inputs and the set-point then regulates and controls the level of activity (arousal) in the descending branches of the autonomic system.
Monitoring the alterations in the rates, rhythms, and patterns of afferent traffic is a key function of the cortical and emotional systems in the brain. Pribram was well aware of the influence of afferent input from the heart and other organ systems in determining the set-points, or what becomes the familiar pattern, as far back as 1969, when he wrote
Visceral feedback constitutes, by the nature of its receptor anatomy and diffuse afferent organization, a major source of input to this biasing mechanism; it is an input which can do much to determine set-point. In addition, cardiovascular and autonomic events are repetitiously redundant in the history of the organism. They vary recurrently, leading to stable habituations; this is in contrast to external changes which vary from occasion to occasion. Habituation to visceral and autonomic activity makes up, therefore, a large share…of the stable base-line from which the organism's reactions can take off.48(p322)
These set-points establish a background against which BP, hormonal balance, and all regularly recurring behaviors are initiated and maintained. For example, when we sense a mismatch between our actual HR and the habituated HR, we generate a feeling (eg, excitement or anxiety if HR is accelerated). The specific feeling experienced may reflect the nature of the mismatch. Importantly, a mismatch may be registered not only due to changes in HR but also due to changes in the pattern of the afferent traffic.
Although input originating from many different bodily organs and systems is involved in the processes that ultimately determine emotional experience, it has become clear that the heart plays a particularly important role. The heart is the primary and most consistent source of dynamic rhythmic patterns in the body. Furthermore, the afferent networks connecting the heart and cardiovascular system with the brain are far more extensive than the afferent systems associated with other major organs.
Additionally, the heart is particularly sensitive and responsive to changes in a number of other psychophysiological systems. For example, heart rhythm patterns are continually and rapidly modulated by changes in the activity of either branch of the ANS, and the heart's extensive intrinsic network of sensory neurons also enables it to detect and respond to variations in hormonal rhythms and patterns.49 In addition to functioning as a sophisticated information processing and encoding center,50 the heart is also an endocrine gland that produces and secretes hormones and neurotransmitters.51–55 Thus with each beat, the heart not only pumps blood but also continually transmits dynamic patterns of neurological, hormonal, pressure, and electromagnetic information to the brain and throughout the body.26
The repeating rhythmic patterns generated by the heart, whether they are ordered or disordered, become familiar to the brain. At the brain-stem level, these patterns are compared to set-points that control BP, affect respiration rate, and control the flow of activity in the descending branches of the ANS. From there, these signals cascade up to a number of subcortical centers—such as the thalamus, hypothalamus, and amygdala—that are involved in the processing of emotion.
Recent findings confirm that there is indeed a set-point for mean long-term BP that is regulated by the nervous system rather than the generally accepted model that the renal output curve determines the set-point for long-term arterial BP regulation. Osborn has provided compelling arguments for a central nervous system–based set-point for long-term arterial BP56 and in recent articles by Zanuto et al,57,58 it was shown that when all of the cardiovascular receptors (baro-, chemo-, and cardiopulmonary) are deinnervated, sustained hypertension results. Zanuto has also provided evidence that nucleus tractus solitarius acts as a compactor and controls the set-point for mean atrial BP, which is consistent with Pribram's model. In addition to physiological causes, they also point out that hypertension can be caused by a set-point shift due to influences for higher-level pathways, such as behavioral activities and autonomic responses to stress and emotional situations. It is our perspective that if set-points that are maintained in the higher levels of the brain are not reset, medications such as beta-blockers that target downstream pathways may result in other physiological systems being activated in order to maintain BP at the set-point.
If it is possible to shift the set-point around which multiple physiological systems attempt to regulate mean BP upward, it should also be possible to shift the set-point downward. We hypothesize that a resetting of set-point in the neural architecture can be accomplished through a constant pattern of activating a positive emotional state and shifting into a more coherent state, which in turn decreases BP. As previous studies have shown, practice of heart-focused emotional self-regulation techniques has resulted in systemic reductions in BP and shown to be an effective treatment approach to reducing hypertension.23,24 Therefore, this study was intended to determine if use of the techniques and the coherent state in particular could be associated with significant short-term reductions in BP. This was of interest to us because coherence training offers a novel nonpharmacological modality that could be used to control hypertension and improve self-regulation of stress.
In addition to the behavioral and physiological perspectives described above, the association of heart focus and positive emotions with the coherent state was particularly attractive to us due to the highly regarded beliefs and traditional knowledge that exists in our Islamic culture, especially in Sufism. It is worthy of mention that the strongly held view that the heart holds the secrets and mysteries that link the body with the mind and soul are also present in many of the ancient wisdoms and world's cultures such as Judaism's Yesod, Christian and Buddhist mysticism, and Indian (Prana) and Chinese healing systems.59 Given the central role of the heart in creating coherence and positive emotions, it is not surprising that one of the strongest common threads uniting the views of diverse cultures and religious and spiritual traditions throughout human history has been the universal regard for the human heart as the source of love, wisdom, intuition, and positive emotions. Sadly, the ability to incorporate such strong views and beliefs held by many of our patients into the treatment process to facilitate the healing process is missing in most modern medicine approaches.
The exploration of new paradigms for the prevention and treatment of heart diseases (eg, hypertension) based on the new perspectives of the wider role of the heart or what many call the spiritual heart or intuitive heart in healing, spirituality, has been extensively discussed in numerous presentations during 3 successive international “Heart: The King of Organs” conferences organized by Al Abdulgader in Saudi Arabia, which have attracted luminaries in this area from around the world.
A new generation of scientists like McCraty and colleagues at IHM are taking seriously the perspective that the heart is more than a pump that sustains life.26,27,48,60–66 It is my perspective that there is much to be gained by scientific inquiries that connect modern medicine with traditional and spiritual ideas about the heart, and this study with hypertensive patients is one part of an ongoing effort to explore this vision and adopt new clinical approaches. It is possible to capitalize on the mysteries of the heart that connect cognitive, emotional, and physiological processes in the treatment of patients with a wide range of health challenges such as hypertension.
CONCLUSIONS
The results of this study suggest that self-regulation techniques that incorporate the intentional generation of positive emotions and increased psychophysiological coherence are an effective approach to lowering acute BP. The coherent state can be facilitated and easily measured in clinical settings with the emWave heart rhythm coherence monitoring device. Outcomes were achieved within a relatively brief timeframe among a diverse patient population. We also found that paced breathing was difficult for some patients to maintain for more than about 1 minute. However, when these individuals were able to intentionally invoke a positive emotional state, they were typically able to maintain a more coherent state for greater periods of time. Clearly, positive emotions can shift the heart's pattern of activity into a more coherent mode that results in increased physiological efficiency, greater emotional stability, and reduced BP among hyper-tensive patients.
We hypothesize that a consistent pattern of short-term BP reduction in combination with emotional shifts can result in the lowering of an internal set-point of BP, which would explain previous studies that have associated use of the self-regulation techniques with systemic reductions in BP. Self-regulation and heart rhythm coherence training offer a novel nonpharmaco-logical modality that is culturally appropriate and could be used to control hypertension and improve self-regulation of stress. This approach to reducing BP should be considered a simple and effective to approach that can easily be taught to patients. The techniques should be especially useful when hypertensive patients are experiencing stressful emotions or reactions to stressors.
Further studies should examine if large-scale implementation of such heart-based coherence techniques could have a significant impact on reducing risk of mortality and morbidity in hypertensive patients. Such implementations could contribute important findings that have the potential to improve the quality of human life globally.
Acknowledgments
We deeply appreciate the generous participation and help of all the patients and their family members who made this work possible. We are greatly thankful to Dr Babiker Osman, Bader Al Anazi, Nora Al Muzafar, and Joan Kristine Estigoy, for all their help in the successful completion of the study.
REFERENCES
- 1.No authors listed The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (NIH Publication No. 98-4080). Bethesda: National Institutes of Health; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program; 1997 [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) State-specific trends in self-reported blood pressure screening and high blood pressure–United States, 1991-1999. MMWR Morb Mortal Wkly Rep. 2002May31;51(21):456–60 [PubMed] [Google Scholar]
- 3.Swan GE, DeCarli C, Miller BL, et al. Association of midlife blood pressure to late-life cognitive decline and brain morphology. Neurology. 1998October;51(4):986–93 [DOI] [PubMed] [Google Scholar]
- 4.Launer LJ, Masaki K, Petrovitch H, Foley D, Havlik RJ. The association between midlife blood pressure levels and late-life cognitive function. The Honolulu-Asia Aging Study. JAMA. 1995December20;274(23):1846–51 [PubMed] [Google Scholar]
- 5.MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease. Part 1. Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990March31;335(8692):765–74 [DOI] [PubMed] [Google Scholar]
- 6.Thijs L, Fagard R, Lijnen P, Staessen J, Van Hoof R, Amery A. A meta-analysis of outcome trials in elderly hypertensives. J Hypertens. 1992October;10(10):1103–9 [DOI] [PubMed] [Google Scholar]
- 7.No authors listed Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. Hypertension Detection and Follow-up Program Cooperative Group. JAMA. 1979December7;242(23):2562–71 [PubMed] [Google Scholar]
- 8.Linden W. Psychological perspectives of essential hypertension: etiology, maintenance, and treatment. Basel: S Karger AG; 1984 [Google Scholar]
- 9.Shapiro AP. Hypertension and stress: a unified concept. Mahwah (NJ): Lawrence Erlbaum Associates; 1996 [Google Scholar]
- 10.Steptoe A. Stress mechanisms in hypertension. Postgrad Med J. 1986July;62(729):697–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Henry JP, Stephens PM, Ely DL. Psychosocial hypertension and the defence and defeat reactions. J Hypertens. 1986December;4(6):687–97 [DOI] [PubMed] [Google Scholar]
- 12.Markovitz JH, Matthews KA, Kannel WB, Cobb JL, D'Agostino RB. Psychological predictors of hypertension in the Framingham Study. Is there tension in hypertension? JAMA. 1993November24;270(20):2439–43 [PubMed] [Google Scholar]
- 13.Ward MM, Swan GE, Chesney MA. Arousal reduction treatments for mild hypertension: a meta-analysis of recent studies. In: Julius S, Bassett DR, editors. Behavioral factors in hypertension. Amsterdam: Elsevier North Holland Publishers; 1987. p. 285–302 [Google Scholar]
- 14.Chesney MA, Agras WS, Benson H, et al. Nonpharmacologic approaches to the treatment of hypertension. Circulation. 1987July;76(1 Pt 2):I104–9 [PubMed] [Google Scholar]
- 15.Charlesworth EA, Williams BJ, Baer PE. Stress management at the worksite for hypertension: compliance, cost- benefit, health care and hypertension-related variables. Psychosom Med. 1984Sep-Oct;46(5):387–97 [DOI] [PubMed] [Google Scholar]
- 16.Weiss SM. Stress management in the treatment of hypertension. Am Heart J. 1988August;116(2 Pt 2):645–9 [DOI] [PubMed] [Google Scholar]
- 17.Mathias CJ. Management of hypertension by reduction in sympathetic activity. Hypertension. 1991April;17(4 Suppl):III69–74 [DOI] [PubMed] [Google Scholar]
- 18.Linden W, Chambers LA. Clinical effectiveness of non-drug therapies for hypertension: A meta-analysis. Ann Behav Med. 1994; 16:35–45 [Google Scholar]
- 19.Rein G, Atkinson M, McCraty R. The physiological and psychological effects of compassion and anger. J Adv Med. 1995;8(2): 87–105 [Google Scholar]
- 20.Tiller WA, McCraty R, Atkinson M. Cardiac coherence: a new, noninvasive measure of autonomic nervous system order. Altern Ther Health Med. 1996January;2(1):52–65 [PubMed] [Google Scholar]
- 21.McCraty R, Atkinson M, Tiller WA, Rein G, Watkins AD. The effects of emotions on short-term power spectrum analysis of heart rate variability. Am J Cardiol. 1995November15;76(14):1089–93 [DOI] [PubMed] [Google Scholar]
- 22.McCraty R, Barrios-Choplin B, Rozman D, Atkinson M, Watkins AD. The impact of a new emotional self-management program on stress, emotions, heart rate variability, DHEA and cortisol. Integr Physiol Behav Sci. 1998Apr-Jun;33(2):151–70 [DOI] [PubMed] [Google Scholar]
- 23.McCraty R, Atkinson M, Lipsenthal L, Arguelles L. New hope for correctional officers: an innovative program for reducing stress and health risks. Appl Psychophysiol Biofeedback. 2009December;34(4):251–72 [DOI] [PubMed] [Google Scholar]
- 24.McCraty R, Atkinson M, Tomasino D. Impact of a workplace stress reduction program on blood pressure and emotional health in hypertensive employees. J Altern Complement Med. 2003June;9(3):355–69 [DOI] [PubMed] [Google Scholar]
- 25.Bedell W. Coherence and hearlth care cost—RCA acturial study: a cost-effectivness cohort study. Altern Ther Health Med. 2010Jul-Aug;16(4):26–31 [PubMed] [Google Scholar]
- 26.McCraty R, Atkinson M, Tomasino D, Bradley RT. The coherent heart: heart-brain interactions, psychophysiological coherence, and the emergence of system-wide order. Integral Rev. 2009December;5(2):10–115 [Google Scholar]
- 27.McCraty R, Childre D. Coherence: bridging personal, social, and global health. Altern Ther Health Med. 2010Jul-Aug;16(4):10–24 [PubMed] [Google Scholar]
- 28.Brotman DJ, Golden SH, Wittstein IS. The cardiovascular toll of stress. Lancet. 2007September22;370(9592):1089–100 [DOI] [PubMed] [Google Scholar]
- 29.Fredrickson BL. Cultivating positive emotions to optimize health and well-being. Prev Treatment. 2000;3(1): Article 0001a [Google Scholar]
- 30.Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J Pers Soc Psychol. 2003February;84(2):365–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCraty R, Childre D. The grateful heart: the psychophysiology of appreciation. In: Emmons RA, McCullough ME, editors. The psychology of gratitude. New York: Oxford University Press; 2004. p. 230–56 [Google Scholar]
- 32.Childre DL, Martin H. The HeartMath solution. San Francisco: HarperSanFrancisco; 1999 [Google Scholar]
- 33.Childre D, Rozman D. Overcoming emotional chaos: eliminate anxiety, lift depression and reate security in your life. San Diego: Jodere Group; 2002 [Google Scholar]
- 34.Childre D, Rozman D. Transforming stress: the HeartMath solution to relieving worry, fatigue, and tension. Oakland: New Harbinger Publications; 2005 [Google Scholar]
- 35.Vanderbilt D, Young R, MacDonald HZ, Grant-Knight W, Saxe G, Zuckerman B. Asthma severity and PTSD symptoms among inner city children: a pilot study. J Trauma Dissociation. 2008;9(2):191–207 [DOI] [PubMed] [Google Scholar]
- 36.Zucker TL, Samuelson KW, Muench F, Greenberg MA, Gevirtz RN. The effects of respiratory sinus arrhythmia biofeedback on heart rate variability and posttraumatic stress disorder symptoms: a pilot study. Appl Psychophysiol Biofeedback. 2009June;34(2):135–43 [DOI] [PubMed] [Google Scholar]
- 37.Ginsberg JP, Berry ME, Powell DA. Cardiac coherence and posttraumatic stress disorder in combat veterans. Altern Ther Health Med. 2010Jul-Aug;16(4):52–60 [PubMed] [Google Scholar]
- 38.Siepmann M, Aykac V, Unterdörfer J, Petrowski K, Mueck-Weymann M. A pilot study on the effects of heart rate variability biofeedback in patients with depression and in healthy subjects. Appl Psychophysiol Biofeedback. 2008December;33(4):195–201 [DOI] [PubMed] [Google Scholar]
- 39.Karavidas MK, Lehrer PM, Vaschillo E, et al. , Preliminary results of an open label study of heart rate variability biofeedback for the treatment of major depression. Appl Psychophysiol Biofeedback. 2007March;32(1):19–30 [DOI] [PubMed] [Google Scholar]
- 40.Lehrer P, Vaschillo E, Lu SE, et al. Heart rate variability biofeedback: effects of age on heart rate variability, baroreflex gain, and asthma. Chest. 2006February;129(2):278–84 [DOI] [PubMed] [Google Scholar]
- 41.Lehrer P, Smetankin A, Potapova T. Respiratory sinus arrhythmia biofeedback therapy for asthma: a report of 20 unmedicated pediatric cases using the Smetankin method. Appl Psychophysiol Biofeedback. 2000September;25(3):193–200 [DOI] [PubMed] [Google Scholar]
- 42.Lehrer PM, Vaschillo E, Vaschillo B, et al. Biofeedback treatment for asthma. Chest. 2004August;126(2):352–61 [DOI] [PubMed] [Google Scholar]
- 43.Lehrer PM, Vaschillo E, Vaschillo B, et al. Heart rate variability biofeedback increases baroreflex gain and peak expiratory flow. Psychosom Med. 2003Sep-Oct;65(5):796–805 [DOI] [PubMed] [Google Scholar]
- 44.Swanson KS, Gevirtz RN, Brown M, Spira J, Guarneri E, Stoletniy L. The effect of biofeedback on function in patients with heart failure. Appl Psychophysiol Biofeedback. 2009June;34(2):71–91 [DOI] [PubMed] [Google Scholar]
- 45.Luskin F, Reitz M, Newell K, Quinn TG, Haskell W. A controlled pilot study of stress management training of elderly patients with congestive heart failure. Prev Cardiol. 2002Fall;5(4):168–72 [DOI] [PubMed] [Google Scholar]
- 46.Hassett AL, Radvanski DC, Vaschillo EG, et al. A pilot study of the efficacy of heart rate variability (HRV) biofeedback in patients with fibromyalgia. Appl Psychophysiol Biofeedback. 2007March;32(1):1–10 [DOI] [PubMed] [Google Scholar]
- 47.McLay RN, Spira JL. Use of a portable biofeedback device to improve insomnia in a combat zone, a case report. Appl Psychophysiol Biofeedback. 2009December;34(4):319–21 [DOI] [PubMed] [Google Scholar]
- 48.Pribram KH, Melges FT. Psychophysiological basis of emotion. In: Vinken PJ, Bruyn GW, editors. Handbook of clinical neurology. Amsterdam: North-Holland Publishing Company; 1969. p. 316–41 [Google Scholar]
- 49.Armour JA, Ardell JL, editors. Neurocardiology. New York: Oxford University Press; 1994 [Google Scholar]
- 50.Armour JA. Neurocardiology: anatomical and functional principles. Boulder Creek (CA): Institute of HeartMath: 2003 [Google Scholar]
- 51.Cantin M, Genest J. The heart as an endocrine gland. Clin Invest Med. 1986November;9(4):319–27 [PubMed] [Google Scholar]
- 52.Gutkowska J, Jankowski M, Mukaddam-Daher S, McCann SM. Oxytocin is a cardiovascular hormone. Braz J Med Biol Res. 2000June;33(6):625–33 [DOI] [PubMed] [Google Scholar]
- 53.Huang MH, Friend DS, Sunday ME, et al. An intrinsic adrenergic system in mammalian heart. J Clin Invest. 1996September15;98(6):1298–1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mukoyama M, Nakao K, Hosoda K, et al. Brain natriuretic peptide as a novel cardiac hormone in humans. Evidence for an exquisite dual natriuretic peptide system, atrial natriuretic peptide and brain natriuretic peptide. J Clin Invest. 1991April;87(4):1402–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cantin M, Genest J. The heart as an endocrine gland. Sci Am. 1986February;254(2):76–81 [DOI] [PubMed] [Google Scholar]
- 56.Osborn JW. The sympathetic nervous system and long-term regulation of arterial pressure: what are the critical questions? Clin Exp Pharmacol Physiol. 1997January;24(1):68–71 [DOI] [PubMed] [Google Scholar]
- 57.Zanutto BS, Frias BC, Valentinuzzi ME. Blood pressure long term regulation: a neural network model of the set point development. Biomed Eng Online. 2011June21;1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zanutto BS, Valentinuzzi ME, Segura ET. Neural set point for the control of arterial pressure: role of the nucleus tractus solitarius. Biomed Eng Online. 2010January11;9:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Alberti FB. Matters of the heart, history, medicine, and emotion. Oxford: Oxford University Press; 2010 [Google Scholar]
- 60.McCraty R. The energetic heart: bioelectromagnetic communication within and between people. In: Rosch PJ, Markov MS, editors. Bioelectromagnetic medicine. New York: Marcel Dekker; 2004. p. 511–532 [Google Scholar]
- 61.McCraty R, Atkinson M, Bradley RT. Electrophysiological evidence of intuition: Part 1. The surprising role of the heart. J Altern Complement Med. 2004February;10(1):133–43 [DOI] [PubMed] [Google Scholar]
- 62.McCraty R, Atkinson M, Bradley RT. Electrophysiological evidence of intuition: Part 2. A system-wide process? J Altern Complement Med. 2004April;10(2):325–36 [DOI] [PubMed] [Google Scholar]
- 63.Pearce JC. The biology of transcendence: a blueprint for the human experience. Rochester (VT): Park Street Press; 2002 [Google Scholar]
- 64.Pearsall P. The heart's code: tapping the wisdom and power of our heart energy. New York: Broadway Books; 1998 [Google Scholar]
- 65.Russek LG, Schwartz GE. Energy cardiology: a dynamical energy systems approach for integrating conventional and alternative medicine. Adv J Mind-Body Health. 1996; 12(4):4–24 [Google Scholar]
- 66.Tiller WA. Science and human transformation: subtle energies, intentionality and consciousness. Walnut Creek, CA: Pavior Publishing; 1997 [Google Scholar]


