Abstract
Background:
Type 1 diabetes mellitus in children is associated with various medical, psychological, emotional, social, and organizational hurdles. Patient-centered disease management should address all patient-relevant issues in an individualized, systems-oriented, and multidisciplinary approach.
Case:
A 10-year-old girl with type 1 diabetes mellitus, a developmental disorder with motor and sensory dysfunction and dyscalculia was cared for full-time by her mother and an assistant nurse. Receiving standard intensified insulin therapy, she still had poor glucose control with frequent mild and severe hypoglycemic episodes. She was socially isolated and not able to attend peer activities and was frustrated with her situation. The mother was substantially stressed, and the child-mother relationship was endangered.
The girl and her family were referred to an integrated, patient-centered, and highly individualized, multidisciplinary diabetic care program that offered self-management education courses and psychosomatic care. A core element was to switch the main focus from technical management and laboratory data to the girl and her specific problems, wishes, goals, needs, and conditions. The child became an active partner in management and decisions. The program offered age-appropriate activities. Consequently, the girl was able to successively self-manage her disease, resulting in a substantial improvement in glucose control, quality of life, satisfaction, and the relationship between mother and daughter.
Conclusion:
Increasing technical sophistication in diabetes management tends to lay the focus on biomedical outcomes. Improved medical and psychosocial results may be achieved when the patient and his or her needs, hurdles, goals, and psychological and social issues are made central to the care he or she receives.
Key Words: Diabetes care management, diabetes mellitus type 1, self-management education course, pediatrics, patient-centered care, blood glucose self- monitoring, case report
抽象
背景:儿童 1 型糖尿病与各种医 疗、心理、情感、社会和组织障碍 有关。以患者为中心的疾病管理应 以一种个性化、面向系统的多学科 方法解决所有与患者相关的问题。
病例:一名患有 1 型糖尿病、发 育障碍、运动和感觉功能障碍及计 算障碍的 10 岁女孩由她的母亲和 一名助理护士全职护理。她正接受 标准的强化胰岛素治疗,但血糖控 制能力仍是很差,频繁出现轻度和 重度低血糖症状。她在社交上感到 孤立,无法参加同伴活动,对自己 的处境感到沮丧。母亲感到重大的 压力,危及到母女关系。
女孩及其家人被转介接受一种综 合性、以患者为中心、高度个性 化的多学科糖尿病护理计划,该 计划提供自我管理教育课程及身 心护理。核心要素是将主要焦点 从技术管理和实验室数据转移至 该名女孩自身及其特定问题、愿 望、目标、需求和状况。孩子开 始积极参与管理和决策。该计划 提供适龄活动。因此,女孩随后 能自行管理她的疾病,导致血糖 控制能力、生活质量、满意度以 及母女关系均得到明显改善。
结论:糖尿病管理中日益增加的 技术复杂性,往往将焦点聚集在 生物医学成果上。把患者及其需 求、障碍、目标、心理和社交问 题作为护理的核心,才能实现医 疗和心理方面的改善。
SINOPSIS
Fundamentación: La diabetes mellitus de tipo 1 en niños conlleva diversas dificultades de tipo médico, psicológico, emocional, social y organizativo. El tratamiento de la enfermedad centrado en el paciente debe abordar todas las cuestiones de importancia para este, con un enfoque individualizado, orientado al sistema y multidisciplinar.
Caso: Niña de 10 años con diabetes mellitus de tipo 1, trastorno del desarrollo con disfunción motriz y sensorial y acalculia, atendida en todo momento por su madre y una enfermera auxiliar. Aunque recibía un tratamiento estándar con insulina intensificado, presentaba un mal control de la glucosa, con frecuentes episodios hipoglucémicos de leves a graves. Se encontraba socialmente aislada, no podía asistir a las actividades de los niños de su edad y su situación le provocaba frustración. La madre presentaba un nivel de estrés considerable, y la relación madre-hija peligraba.
La niña y su familia fueron derivados a un programa de tratamiento de la diabetes integrado, centrado en el paciente, multidisciplinar y muy individualizado, que ofrecía cursos educativos sobre la gestión de la diabetes por el paciente y atención psicosomática. Un elemento fundamental consistía en desplazar el foco de atención de la gestión técnica y los datos de laboratorio a la niña y sus problemas específicos, sus deseos, objetivos, necesidades y enfermedades. La niña pasó a tener un papel activo en la gestión y en la toma de decisiones. El programa ofrecía actividades adecuadas para su edad. Como resultado, la niña fue capaz de gestionar su enfermedad en lo sucesivo, lo que dio lugar a una sustancial mejora en el control de la glucosa, la calidad de vida, la satisfacción y la relación entre madre e hija.
Conclusión: El aumento de la sofisticación técnica en el tratamiento de la diabetes tiende a centrar la atención en los resultados biomédicos. Puede obtenerse una mejora de los resultados médicos y psicosociales cuando el centro de atención se enfoca en el paciente y sus necesidades, dificultades, objetivos y problemas psicológicos y sociales.
INTRODUCTION
Type 1 diabetes mellitus is a serious common chronic disease in childhood with increasing incidence.1 It is caused by insulin deficiency usually following autoimmune destruction of the insulin-producing pancreatic beta cells. To prevent the many serious short-term and long-term complications associated with the disease, careful daily and lifelong management maintaining glucose control is essential. Continuous blood glucose monitoring, carbohydrate counting, multiple insulin injections per day, and adjustment for various activities, however, interfere with the routine of daily life. Families are often overwhelmed by the complexities, organizational obstacles, and life-threatening complications of the disease.
The cornerstone of diabetic care is comprehensive case management including intense education to enable self-management adjusted for the child's age and developmental stage and with assistance from caring and knowledgeable adults.2-7 This allows for an increasingly flexible and independent lifestyle and participation in school and peer activities.8 Still, the medical, emotional, psychological, social, and organizational needs of the children and their parents are highly complex, and the indispensable ongoing parental involvement affects the parent-child relationship.8 These complex issues are often only partly dealt with in diabetes management, which tends to focus on laboratory measurements and the sophisticated technical aspects of care.9 As a consequence, in many instances, optimal management is not achieved, blood glucose is not well controlled, children become unhappy and frustrated, and their healthy development and emotional maturation are endangered.
Gemeinschaftskrankenhaus Herdecke, an integrative anthroposophic hospital in Germany, has a large pediatric department that provides pediatric endocrinology and diabetic care, child and adolescent psychiatry, and psychosomatic medicine. A patient-centered diabetic care program offers an integrated, individualized, systems-oriented, and multidisciplinary approach, including full-time education courses. Many of the patients suffer from serious adherence problems, often complicated by behavioral, emotional, or developmental problems or by psychiatric disorders, with poor metabolic control. This article presents the application of a patient-centered approach for a diabetic child.
HISTORY AND PRESENTING CONDITION
A girl was diagnosed with insulin-dependent Type 1 diabetes mellitus at the age of 8 years (2009); she also had a developmental disorder with motor and sensory dysfunctions (treated with occupational and physical therapy). She had dyscalculia and was normally intelligent and talented and visited a school for physically handicapped children. She was overweight but not obese (body mass index [BMI] 21.8, ie, 90th-97th percentile). She had asthma that had been well controlled for years (using oral ketotifen, inhalative salmeterol, and a fluticasone aerosol inhaler). She lived with her mother, a gerontological nurse; had infrequent contact with her father, a bus driver; and had three older half-siblings. The parents were divorced. Major diagnoses of her family were cardiovascular and neoplastic diseases (cardiac infarction, carotid stenosis, atherosclerosis, hypertension, and renal carcinoma) and atopic dermatitis.
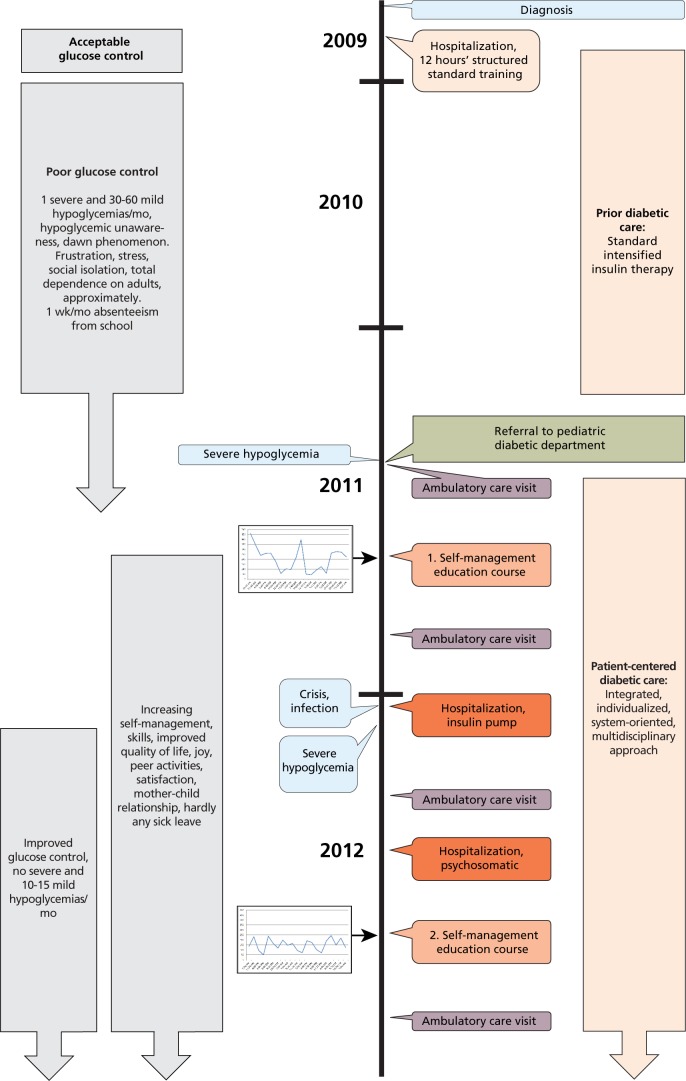
The girl had been treated with intensified insulin therapy according to standards, and she and her mother had initially received 12 hours of structured standard training in diabetes management (Figure 1). After the first 6 weeks, diabetes management and glycemic control had become very difficult. Blood glucose levels fluctuated drastically, and no clear rules and guidance for adjustment of insulin dosage were available or taught. Thirty to 60 mild and approximately one severe hypoglycemias occurred per month, and the latter had to be treated with glucagon. Along with her perceptual difficulties, the girl suffered from hypoglycemic unawareness. Especially during physical activities, the metabolic situation often got out of control. Injecting insulin at the same site repeatedly had caused a local lipohypertrophy, leading to unpredictable insulin pharmacokinetics (eg, delayed bioavailability, increased insulin effects during physical activities, and increased blood flow).
Figure 1 Timeline of interventions and outcomes.
Caring for her daughter and monitoring blood glucose levels on an hourly or bihourly basis kept the mother occupied around the clock. She was considerably worried. Her engagement in other activities and personal interests was severely hampered. During school, the girl was constantly accompanied by an assistant nurse who monitored blood glucose and food intake, injected insulin, and called the mother hourly or bihourly. This resulted in maximum stress for the mother, complicated her work duties and her new relationship, and made her feel completely helpless, as though she were at the mercy of her daughter's glycemic levels and behavior.
The child played a passive role; she had no confidence in her abilities to share the management of her diabetes. The constant company of the assistant nurse sitting beside her in the classroom and complete lack of independence thwarted normal social interaction with peers and the ability to make friends and participate in normal activities; it endangered her psychosocial development and healthy self-esteem. Although actually of a cheerful character, the girl was frustrated, unhappy, and depressed in view of her difficult life situation, the “stupid” injections, the impossibility of self-determined activities, the many restrictions and limitations, and the exclusion from her peers. For instance, she was not allowed to swim due to the risk of hypoglycemia and drowning. She was threatened by severe hypoglycemia and endangered whenever she was without the support of accompanying adults; she was completely dependent.
At the age of 10 (May 2011), during a severe hypoglycemia, she was admitted to a hospital and then referred to the Pediatric Endocrinology and Diabetes Department of the Gemeinschaftskrankenhaus Herdecke, where she has been treated since then.
At the first consultation, besides her diabetic status, the physical examination showed sensory dysfunctions, including difficulties in spatial perception and in perception of her own movement. A slight generalized hypotonia was found, a left-sided tendency to walk on tiptoe rather than on the heel and a slight one-sided muscular spasm. No birth trauma or infections were reported. No other physical abnormalities were found. Auscultation of the lung was normal. Her mental, cognitive, and emotional status was completely normal. Her glucose levels fluctuated substantially (Figure 2) with a fasting plasma glucose of 45 mg/dL to 500 mg/dL. HbA1c was 7.9%. Due to her condition, she missed about 1 week of school per month.
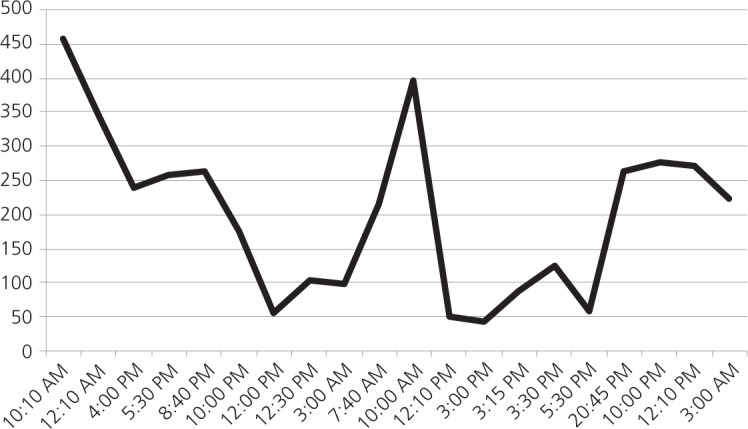
Figure 2 Blood glucose level (mg/dL) on 2 consecutive days at the beginning of the first diabetic training, August 2011.
INTERVENTION
During the following year and a half, the girl had altogether four ambulatory diabetes care consultations, two more hospitalizations, two diabetes self-management education courses, and continuous close telephone contact. During the education courses and hospitalizations, she also received art therapy—therapeutic sculpturing to improve her perception, in particular her perception of form and her ability to deal with Gestalt—and eurythmy therapy to improve her motor abilities and her developmental retardation, to help her learn about herself in a nonverbal manner, and to develop self-confidence.
First Diabetes Self-management Education Course
After initial consultation, the girl was admitted to the self-management education course for children of elementary-school age (August 2011). Organized according to a structured curriculum and time schedule and based on international standards2-4,6,7 and integrating elements of behavioral therapy, this course primarily pursues a patient-centered, highly individualized and systems-oriented approach. It primarily focuses on the children's needs and characteristics.
For 1 week, a group of diabetic children live together in a kind of youth hostel. The atmosphere is recreational, with child-appropriate activities such as circus activities, leisure time and trips, mimicking normal daily life. The companionship and developing friendships with other children with diabetes brings a sense of normalcy to this condition. Struggling with similar difficulties and learning certain skills together relieves feelings of isolation in the children. Additionally, they are cared for by young adults who also have diabetes and are able to manage their condition. The education of all aspects of diabetes management—details on the disease, physiologic responses, blood glucose monitoring and interpretation, food intake, calculating and injecting insulin, and other relevant information and skills—is integrated into normal daily life and leisure activities. The goal is to unobtrusively train the children in managing the disease but not making it the focus of their lives. The starting point for the training is the child's respective problems, wishes, expectations, and goals, and his or her cultural, social, and family background. It makes intense use of the child's healthy resources, which often have to be discovered first. In all steps, the child is an active participating partner. Every day, the individual learning units are planned and discussed with the child: for instance, learning the consequences of physical activities on their glucose control and how to prepare for it, such as eating in advance. Learning new skills is rewarded: During social gatherings in the evening, the child is allowed to choose a small toy out of a box while the other children applaud. Punishments are avoided. No activity is forbidden; everything (eg, swimming) is allowed, but children are prepared for it and supervised. The training is provided by a multidisciplinary team: pediatric diabetes specialists, an endocrinologist, a diabetes adviser, a dietitian, a pediatric nurse, a teacher, and a child and adolescent psychiatrist. Parents as well as siblings and close friends are integrated within the training process, but they do not accompany the children during the course.
The girl was trained in diabetes self-management. She learned to inject herself using varying injection sites. Considering her perceptional difficulties, she was intensely trained to notice and correctly interpret hypoglycemia symptoms, to handle her metabolic status during physical activities, to adhere to schedules for blood glucose monitoring, and to calculate the insulin dosage. This was particularly difficult due to her dyscalculia. To help her, specific schemata and tables were developed: in the tables, the counted carbohydrates were allocated to a specific factor for multiplication (eg, 30 g carbohydrates x 1.5) and then adapted to the blood glucose level. The multiplication factor varied by individual and during the day and has to be repeatedly adapted for the child. This schema enabled the girl to determine the appropriate insulin dosage, which enabled her self-management despite her dyscalculia. Other unfavorable habits and their potential disadvantages were discussed from the girl's point of view, and new arrangements were made (eg, reducing the large amount of food intake in the evening). The girl participated in all decisions and planning of all details, and all discussions took place when the child felt emotionally comfortable. Goals were written down. If goals could not be reached, reasons were discussed and the intent recalled but without any hint of blaming, and achievement of the goal was rewarded.
During the course, parents are trained for 1 day as well. Meanwhile, the children go on an excursion and learn how to handle metabolism during intense outdoor activities. The parents are informed about their children's new competences and are trained for their part. Together with other parents, they attend a discussion and support group with a child and adolescent psychiatrist on topics related to the care of children with chronic diseases: the necessity to guide children and to increase their autonomy; the necessity to develop confidence in the children's ability, to encourage them, and to allow the children to make mistakes; the persistent anxiety of the parents, such as concerns about making mistakes and fear of hypoglycemia and its potential fatal consequences. In the case of this girl, her mother's anxiety was in a constant conflict with any autonomous activities of the daughter. The parents are also informed during the course about hypoglycemia and its treatment by the body's own glucagon, by glucagon injections or by oral carbohydrates, and they are informed that hypoglycemia rarely leads to death or permanent damage. Lay information on hypoglycemia has often deeply worried the parents. Parents are further supported by guidebooks.10,11
During the course, the girl developed well; she enjoyed learning and was proud of her new skills and competencies. On the last day, she performed a little artistic circus feat. While before the training course she had played a rather passive role in her care and was primarily cared for by others, she was now in the center of care and actively participated in and increasingly self-managed her metabolic situation, which gave her great pleasure. Her mother was happy about and proud of her daughter's new competencies.
Hospitalization
Six months after this first educational training course, the girl was readmitted to the hospital. During an infection, her metabolic situation had gotten out of control. Again the mother was very anxious, fearful for her daughter and afraid of making mistakes. She was heavily burdened by the exhausting situation. As the glucose control was still difficult and as the girl also had high glucose levels in the morning, an insulin pump was agreed upon. The mother was skeptical about whether her daughter would be able to handle the pump. The girl was trained in managing the pump. The basal rate of the pump (Paradigm Veo, Medtronic, Minneapolis, Minnesota) was adapted for different types of days: for weekends with few activities (8.8 units short-acting analogue, insulin aspart/day), for school days with intense activities (3.1 insulin units/day), and for days in between (3.8 insulin units/day). To further optimize the pump's effectiveness, the circadian basal rate was individually adapted based on a fasting test (Figure 3). The pump's calculator also supported the girl in calculating her bolus dosages. With this support, glucose control was substantially improved. As the girl still had difficulties recognizing hypoglycemic symptoms, a sensor for continuous glucose monitoring also was introduced (sensor-augmented insulin-pump therapy, Medtronic MiniLink Continuous Glucose Monitoring system). However, after some months of usage, the girl rejected this sensor and limited its use to specific situations; its frequent beeping provoked constant tension and undermined the confidence in her own management. In her view, the sensor was more a nuisance than a help.
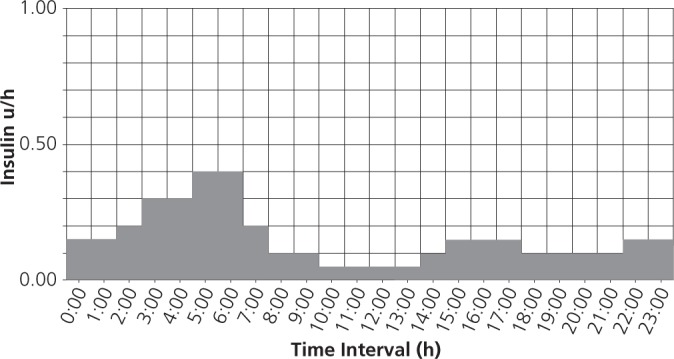
Figure 3 Individually adapted circadian basal rate of the insulin pump.
During this training, the persistent anxiety and fear of the mother became obvious again, and she had difficulty dealing with the increasing autonomy of the child. The girl, on the other hand, was in the conflict of pursuing independence and competence but also wanting to avoid troubling and frightening her mother by making mistakes. Furthermore, the school as well as the nursing assistant, who still accompanied the girl constantly, declined to change any practices and did not accept or support the increasing autonomy and self-competence of the girl. Therefore, the girl was admitted to the psychosomatic department of the hospital in May 2012. The intent was to help the girl achieve a level of independence and self-competence appropriate for her age and to establish a stable mother-daughter relationship not based on anxiety. During this hospitalization, the girl was further trained in diabetes management in the school of the hospital. Her mother and father had regular consultations and were both trained further in diabetes management tailored to the needs of their daughter. Her school teacher and nursing assistant, as well as a close friend and peer of the girl, also were trained. On weekends, the girl tried staying at home and applying the newly learned abilities and interaction with her mother in her everyday situation. For this purpose, goals for each weekend were document at the beginning of the weekend, and the respective successes and failures were reported at the end. All successes were rewarded (eg, when the girl remembered on her own to measure blood glucose or to inform her mother).
Second Diabetes Self-management Education Course
During summer 2012, the child attended the diabetes self-management education course a second time. In the introductory consultation, when individual goals are set, the child responded to the questions about hurdles of her diabetic condition with, “Nothing; I can live well with it.” The mother reported some limitations as spontaneity was still somewhat affected (a frequent response from parents); however, she now had full confidence in her daughter's skills and competence; she was managing her condition well. In the group of diabetic peers, the girl noticed how well she was able to handle the situation and how well she was integrated into the group. This strengthened her self-confidence. During the course, the recognition of hypoglycemia was again taught intensely with a special program. She explored her feelings at the beginning of hypoglycemic situations and discovered a feeling of warmth, which occurred regularly in these situations. Furthermore, she performed certain exercises, which she could manage under normal conditions but not during the hypoglycemic situation (eg, walking backward or calculating five times-tables backward. This was an easy test, one she could conduct everywhere to recognize a hypoglycemia beginning. The girl was also trained to self-manage lunch in school and to involve a school friend who was also integrated in the training course.
Diary, Ambulatory Diabetes Care, Telephone Consultations
In the program, the children continuously keep a handwritten diary, recording items such as the following: blood glucose levels, food intake (carbohydrates), special events, hypoglycemias and management, injected units of insulin per amount of carbohydrates and measured glucose level, illnesses, physical activities, and excursions. This is also a tool for self-reflection and learning. During ambulatory diabetes care, the child first meets the diabetes adviser: basic measurements are made, injection sites inspected, the diary and its special noted events reviewed. Details and hurdles of diabetes management are discussed, training elements reiterated, technical devices supplied or organized. Afterward, the child is seen by the doctor (a pediatric diabetes specialist). Here, management of diabetes and of everyday situations is discussed, new steps to be learned are outlined, and difficulties are identified and discussed. Laboratory results (particularly HbA1c) are reviewed only at the very end to prevent them from being the primary focus. Parents and children also have the ability to call the diabetes specialist or diabetes adviser as often as they have questions or worries. This reassures families and reduces stress tremendously.
OUTCOME
After these complex treatments and training courses, the patient's metabolic control substantially improved (Figure 4). The girl is now increasingly able to self-manage her diabetes according to her age and to seek help when necessary. The school still insisted on a nursing assistant, the involvement of whom, however, is now unobtrusive and discrete. Also in school, the girl manages her condition mainly by herself. She gets along in school very well, can attend all school activities (including a forest group and school trip), is a good pupil, and requires hardly any sick leave anymore. She has gained motor skills, can engage in sports and other leisure activities, and goes swimming. Her social activities have increased. Her improved self-esteem is apparent in all areas, and she has developed into a cheerful child. She is fully supported by her mother and collaborates well with her. The mother is proud of her daughter and her development. The mother's work situation is much more relaxed, as she is not constantly contacted anymore. Both the girl and her mother are highly satisfied with the course of the disease and its management.
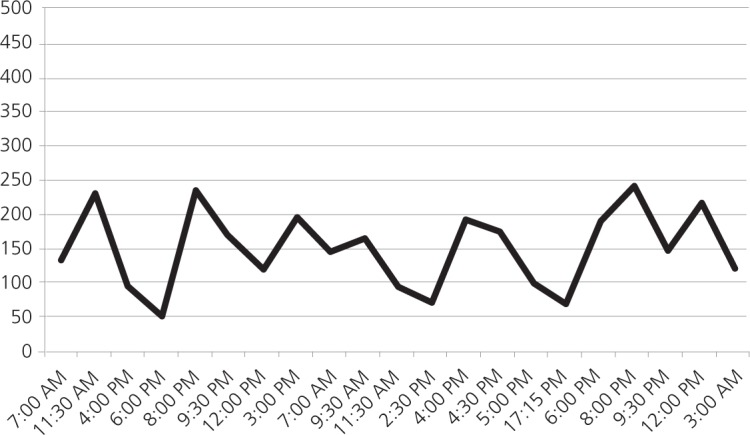
Figure 4 Blood glucose level (mg/dL) on 2 consecutive days after first diabetic training, improved self-management including insulin pump, psychosomatic treatment for May 2012; representative of the following months.
Mild hypoglycemias are now reduced to 10 to 15 per month. The previously frequent severe hypoglycemias had occurred once during the treatment and training period (during school, despite the company of the nurse assistant; see Figure 1) and had been treated with glucagon injection. Since then, no severe hypoglycemia has occurred. Her fasting plasma glucose is now 70 mg/dL to 150 mg/dL, and her HbA1c is 7.0%. With an appropriate set of guidelines, the glycemic control has improved substantially. The girl can now handle hyper- and hypoglycemia herself and recognizes hypoglycemic episodes much better. The fluctuations in blood glucose levels have diminished, including during physical exercises. The overweight remained largely unchanged (BMI now 23.3, 90th-97th percentile). No adverse effects or adverse or unanticipated events were observed.
DISCUSSION
The difficult metabolic situation, deep frustration, and stress of a diabetic child and his or her parent(s) could be substantially improved by completely changing the focus of diabetic care. Initially and despite standard medical care, there had been strong fluctuations of the blood glucose levels with frequent hypoglycemic episodes and complete dependency of the girl on adults, which had led to anxiety and social isolation. The girl had played a passive role in her care. Medical information and standardized training had been provided on an intellectual, theoretical level, not specifically accounting for the child's individual situation and her developmental and healthy capacities.
The core of the presented intervention was to switch the primary focus of the diabetic care directly onto the child and her context, needs, wishes, competences, and hurdles, and an age-appropriate, active partnership. This also meant that monitoring, laboratory data, and technical aspects of management were removed from the center of the focus to become secondary, supportive, and less obtrusive. Through systems-oriented care, all of the relevant issues were addressed within the same process. The training and its schedule evolved out of the daily needs and specific characteristics of this child. The child—rather than her glucose levels—was the focus of interest.
Patient-centered care is a ubiquitously recognized goal in diabetes care; still, one of the greatest challenges is turning this often rather rhetorical goal into a clinical reality. The increasing technical sophistication and the focus being laid on measuring and recording biomedical outcomes threatens to distract practitioners from compassion, communication, and the health outcomes that matter to children.12 Children have a varied experience of being involved in their care and in fact usually occupy a marginal role. Decisions are often made by parents or healthcare professionals while children tend to be seen as inactive, passive, or incompetent. Age, maturity, and a presumed lack of the cognitive abilities to understand medical terminology and complex treatment information are seen as major constraints on their active participation. However, children express a strong desire to be engaged and have their voices heard in decisions.13,14 With appropriate medical care and diabetes training, children can gain high levels of understanding and skill and are able to make informed decisions in their own best interest, even at a young age.15
Pediatric diabetes education still has to identify how best to support children and adolescents—how to integrate intensive insulin dose adjustment into daily routines; adequately teach the various necessary skills; delegate and share responsibility for daily self-management tasks; find a workable balance between delegating too much responsibility too soon or being too protective; enhance the communication skills required for continued parent and adolescent motivation and empowerment; and prevent families from entering the vicious circle of frustration and diabetes burnout12—thus enabling good quality of life, healthy development, emotional maturation, and the diabetic children's key goals: to be “normal” and “get on with their lives.”15
Self-management education courses that are attended by the children full-time in a normal child-adequate setting are essential to this pursuit. They facilitate really getting to know the child, discovering his or her strengths and recourses, and identifying skills the child will be able to manage. An exact knowledge of the child's abilities is indispensable when helping him or her to take on far-reaching responsibilities. Also, the behavioral modifications that are intended by the training process will work only when it takes place in an atmosphere and setting resembling normal everyday life. Furthermore, the necessary trust to address all prevailing problems depends on the familiarity and comfort of the setting. The close contact to peers and young adults struggling with and managing the same condition is of great support for the children and their growing self-esteem. Neither the ambulatory nor the hospital setting suits this purpose, as neither is adequate for the child nor resembles daily life. Isolated ambulatory visits provide advice to the parents but without any real connection to the child. Hospitalization constrains children's active participation in their care. Although they are willing to endure hospitalization in order to get better, they express fear and anxiety about and a dislike for hospitalization.13
In the case of this patient, her strengths were maximally used. This was possible because her strengths and weaknesses were well known: she was normally intelligent and very cautious; her weak points were dyscalculia (low numeracy skills are adversely associated with diabetes control16), perceptional difficulties, and activity-dependent poor control of the metabolism. Addressing these, in addition to placing her and her specific wishes and troubles in the center of care, enabled individually targeted training with an optimal result. Today, her glucose is under much better control, her life has regained flexibility, and her self-esteem has improved, enabling good development and emotional maturity. An insulin pump was optimal for this girl and substantially improved the metabolic situation, but its successful introduction was dependent on the precise estimation of the girl's abilities. Some may support a more forceful recommendation of the sensor; however, this conflicts with our patient-centered decision model. We further regard the art therapy and eurythmy therapy as helpful in the process of emotional maturation, as they improved the patient's motor and sensory functions, especially self-perception and bodily perception. However, we cannot prove this assertion within this case. Other reports and studies support our assumption.17-20
Diabetes self-management education courses as well as insulin pumps are well investigated and considered state-of-the-art in diabetic care.2-7 Still, the optimal integration of the technical diabetes interventions into patient-centered care—the rhetoric having not yet turned into clinical reality12—does obviously go beyond guidelines and trials. Outlining strategies for the individualization of care may depend on many transparent examples published as case reports. While numbers and techniques as well as guidelines are generalizable, the patients and their specific characteristics, hurdles, goals, needs, strengths, and weaknesses differ extensively and require individually tailored approaches.
To provide insight into the individualized multi-faceted procedure of patient-centered approaches, case reports seem to be the optimal tool. The same is true regarding compassionate support for patient-centered diabetes care, where first-person narratives can transport much more information than can “scientific knowledge.”21
The patient-centered diabetic care detailed in this report is pursued in all our patients. The patient described in this case report is not exceptional with regard to diagnosis, treatment, course of disease, or outcome. Most of our patients have an even more complex history and conditions, which are difficult to present in a single article. This is especially the case when we are contacted by patients with complicated, ongoing conditions with maladjustments and comorbidities and who often are in the vulnerable period of puberty and need multidisciplinary care.
A limitation of our case report is the not entirely precise or detailed information about diabetes management before the patient was referred to our department; however, the information presented by the patient's mother was sufficient for an optimal diabetes management. The other limitation is that we do not know the cause of the girl's developmental disorder. Overall, we regard the general benefit of the patient-centered diabetes care as obvious in our case.
We want to encourage use of the patient-centered and systems-oriented approach in pediatric diabetic care. Additional elements of art interventions—painting, sculpting, music, or movement—also may be helpful in the complex care of children and adolescence. More research and in-depth evaluation are needed for the specific contribution of the arts in improving healthcare in children.
Acknowledgments
We are thankful to the Mahle-Stiftung, Hauschka-Stiftung, and Jonas-Stiftung for their support of case reporting.
Informed Consent
The patient and her mother gave consent to publish this case report. The mother read the article and confirmed its content.
Disclosures Drs Kienle, Meusers, and Quecke have no conflicts of interest to disclose. Dr Hilgard is a member of the advisory board for DiaPort at Roche Diagnostics GmbH, Mannheim, Germany.
Contributor Information
Gunver S. Kienle, Institute for Applied Epistemology and Medical Methodology, University of Witten/Herdecke, Germany.
Michael Meusers, Department of Child and Adolescent Psychiatry and Neurology, Gemeinschaftskrankenhaus, Herdecke, Germany.
Birgit Quecke, Department of Integrative Pediatric and Adolescent Medicine, Psychosomatic Medicine, Gemeinschaftskrankenhaus, Germany.
Dörte Hilgard, Department of Integrative Pediatric and Adolescent Medicine, Pediatric Diabetology/Endorcrinology, Gemeinschaftskrankenhaus, Germany.
REFERENCES
- 1.Patterson CC, Dahlquist GG, Gyürüs E, Green A, Soltész G; EURODIAB Study Group Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–20: a multicentre prospective registration study. Lancet. 2009;373(9680):2027–33 [DOI] [PubMed] [Google Scholar]
- 2.International Society for Pediatric and Adolescent Diabetes, International Diabetes Federation Global IDF/ISPAD guideline for diabetes in childhood and adolescence. International Diabetes Federation: Brussels; 2011. http://www.ispad.org/content/2011-global-idfispad-guideline-diabetes-childhood-and-adolescence Accessed February 26, 2013. [Google Scholar]
- 3.Haak T, Kellerer M. editors. Deutsche Diabetes Gesellschaft, Arbeitsgemeinschaft für Pädiatrische Diabetologie: Diagnostik, Therapie und Verlaufskontrolle des Diabetes mellitus im Kindes- und Jugendalter. Mainz, Rhineland-Palatinate, Germany: Kirchheim; 2009 [Google Scholar]
- 4.Lange K, Sassmann H, Von Schütz W, Kordonouri O, Danne T. Prerequisites for age-appropriate education in type 1 diabetes: a model programme for paediatric diabetes education in Germany. Pediatr Diabetes. 2007October;8Suppl 6:63–71 [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association: Standards of medical care in diabetes—2013 Diabetes Care. 2013;36(1):S11–S66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hürter P, Lange K, Jastram HU, et al. Diabetes- Buch für Kinder. Diabetes bei Kindern: ein Behandlungs- und Schulungsprogramm. Mainz, Rhineland-Palatinate, Germany: Kirchheim & Co GmbH; 2005 [Google Scholar]
- 7.Hiort O, Danne T, Wabitsch M. Pädiatrische Endokrinologie und Diabetologie. Heidelberg, Germany: Springer; 2010 [Google Scholar]
- 8.Silverstein J, Klingensmith G, Copeland K, et al. Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care. 2005;28(1):186–212 [DOI] [PubMed] [Google Scholar]
- 9.Diabetes UK Emotional and psychological support and care in diabetes (March2010). http://www.diabetes.org.uk/Professionals/Publications-reports-and-resources/Reports-statistics-and-case-studies/Reports/Emotional-and-Psychological-Support-and-Care-in-Diabetes/ Accessed February 26, 2013.
- 10.Bartus B, Holder M. Diabetes bei Kindern: Mit Freude groß werden - sicher in Alltag, Schule und Freizeit. Stuttgart, Germany: Trias; 2012 [Google Scholar]
- 11.Hürter P, Von Schütz W, Lange K. Kinder und Jugendliche mit Diabetes: Medizinischer und psychologischer Ratgeber für Eltern. Heidelberg, Germany: Springer; 2011 [Google Scholar]
- 12.Murphy HR. Education, technology and psycho-technological approaches to type 1 diabetes. Pract Diabetes. 2012;29(6):247–251a [Google Scholar]
- 13.Coyne I, Hayes E, Gallagher P, Regan P. Giving children a voice: investigation of children's experiences of participation in consultation and decision-making in Irish hospitals. Office of the Minister for Children, Dublin, Ireland: The National Children's Strategy Research Series; 2006. http://www.dcya.gov.ie/viewdoc.asp?fn=/documents/Research/Giving_Children_a_Voice.pdf Accessed February 26, 2013. [Google Scholar]
- 14.Coyne I. Children's participation in consultations and decision-making at health service level: A review of the literature. Int J Nurs Stud. 2008November;45(11):1682–9 [DOI] [PubMed] [Google Scholar]
- 15.Alderson P, Sutcliffe K, Curtis K. Children as partners with adults in their medical care. Arch Dis Child. 2006April;91(4):300–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marden S, Thomas PW, Sheppard ZA, Knott J, Lueddeke J, Kerr D. Poor numeracy skills are associated with glycaemic control in type 1 diabetes. Diabet Med. 2012May;29(5):662–9 [DOI] [PubMed] [Google Scholar]
- 17.Schwab JH, Murphy JB, Andersson P, et al. Eurythmy therapy in anxiety—a case report. Altern Ther Health Med. 2011;17:58–65 [PubMed] [Google Scholar]
- 18.Hamre H, Witt C, Glockmann A, Willich SN, Ziegler R, Kiene H. Eurythmy therapy in chronic disease: a four year prospective cohort study. BMC Public Health. 2007;7:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bussing A, Ostermann T, Majorek M, Matthiessen PF. Eurythmy therapy in clinical studies: A systematic literature review. BMC Complement Altern Med. 2008;8:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kienle GS, Kiene H, Albonico HU. Anthroposophic medicine: effectiveness, utility, costs, safety. Stuttgart, Germany; New York: Schattauer Verlag; 2006 [Google Scholar]
- 21.Kumagai AK, Murphy EA, Ross PT. Diabetes stories: use of patient narratives of diabetes to teach patient-centered care. Adv Health Sci Educ Theory Pract. 2009August;14(3):315–26 [DOI] [PubMed] [Google Scholar]