Abstract
Health coaching (HC) is a process holding tremendous potential as a complementary medical intervention to shape healthy behavior change and affect rates of chronic lifestyle diseases. Empirical knowledge of effectiveness for the HC process, however, is lacking. The purposes of this paper are to present the study protocol for the Ithaca Coaching Project while also addressing research design, methodological issues, and directions for HC research. This is one of the first large-scale, randomized control trials of HC for primary prevention examining impact on physical and emotional health status in an employee population. An additional intent for the project is to investigate self-determination theory as a theoretical framework for the coaching process. Participants (n=300) are recruited as part of a campus-wide wellness initiative and randomly assigned to one of three levels of client-centered HC or a control with standard wellness program care. Repeated measures analyses of covariance will be used to examine coaching effectiveness while path analyses will be used to examine relationships between coaching processes, self-determination variables, and health outcomes. There is a great need for well-designed HC studies that define coaching best practices, examine intervention effectiveness, provide cost:benefit analysis, and address scope of practice. This information will allow a clearer definition of HC to emerge and determination of if, and how, HC fits in modern-day healthcare. This is an exciting but critical time for HC research and for the practice of HC.
Key Words: Self-determination theory, wellness, wellness coaching, health or lifestyle or disease management intervention
抽象
健康辅导研究:Ithaca 辅导项 目、研究设计及未来方向 作为一种补充医疗干预方法,健 康辅导 (HC) 流程拥有巨大潜 力,可促使健康行为改变并降低 慢性疾病患病率。但缺少有关 HC 流程有效性的经验知识。本 文旨在介绍 Ithaca 辅导项目的 研究方案,同时还就研究设计、 方法问题、HC 研究方向进行讨 论。这是首批考察 HC 基础预防 及其对员工群体的身体和情感健 康状况影响的大型随机对照试验 之一。该项目的另外一个目的是 研究自我决定理论作为辅导流程 的理论框架。作为校园健康倡议 的一部分,招募(n ≥ 300 名) 参与者,并将其随机分配至三个 等级的以患者为中心 HC之一或 标准健康计划护理对照组。重复 协方差测量分析将用于考察辅导 的有效性,路径分析将用于考察 辅导过程、自我决定变量和健康 结果之间的关系。现在极需一项 精心设计的 HC 研究以确定最佳 辅导实践、检查干预的有效性、 提供成本效益分析及讨论实践范 围。此信息将使 HC 拥有更为明 确的定义,且将有助于确定 HC 是否及如何融入现代医疗。这将 是 HC 研究和实践激动人心的关 键时刻。
SINOPSIS
La formación sanitaria (FS) es un proceso que posee un enorme potencial como intervención médica complementaria para lograr un cambio conductual saludable y reducir los índices de enfermedades crónicas. Sin embargo, se carece de conocimientos empíricos acerca de la eficacia del proceso de la FS. La finalidad de este artículo consiste en presentar el protocolo de estudio del proyecto de formación sanitaria Ithaca, al mismo tiempo que se abordan el diseño de la investigación, los aspectos metodológicos y el rumbo de la investigación de la FS. Se trata de uno de los primeros ensayos controlados y aleatorizados a gran escala para examinar la FS dirigida a la prevención primaria y su impacto sobre el estado de salud físico y emocional de una población de empleados. Una intención adicional del proyecto es la de investigar la teoría de la autodeterminación como marco teórico para el proceso de formación. Se está reclutando a los participantes (n 1 300) dentro de una iniciativa de bien-estar a lo largo del campus y se les está asignando, de forma aleatoria, a uno de tres niveles de FS centrada en el cliente o a un grupo de control que recibe atención a través de un programa de bienestar estándar. Se utilizarán análisis de covarianza con medidas repetidas para examinar la eficacia de la formación y se emplearán análisis de trayectorias para estudiar las relaciones entre procesos de formación, variables de autodeterminación y resultados sanitarios. Existe una gran necesidad de estudios de FS bien diseñados que establezcan buenas prácticas de formación, investiguen la eficacia de las intervenciones, elaboren un análisis de la relación entre costes y beneficios, y aborden el campo de aplicación. Estos datos permitirán definir con mayor claridad la FS para que emerja y contribuirán a averiguar si la FS encaja en la atención sanitaria moderna y de qué manera lo hace. Nos hallamos en un momento interesante pero crítico de la investigación y el ejercicio de la FS.
INTRODUCTION
The coaching industry certifies thousands of professionals each year as executive coaches, life coaches, and now health coaches. The corporate world and entertainment industry adopted the concept early on but now coaching is gaining further traction as the medical community begins to embrace coaching practices. Health and wellness coaching (HC) is a booming professional option founded on sound theory but a scant empirical data base. If HC is to sustain long-term growth and be accepted by the medical community as an effective health intervention, well-designed randomized clinical trials (RCTs) investigating coaching are needed. The advancement of HC is therefore dependent on deriving data supporting its effectiveness for improving health status. Moreover, a clinical process such as coaching is better understood and academically accepted when it rests on a sound theoretical framework. While logic identifies several theories (eg, Self-Determination Theory [SDT]; Social Cognitive Theory) that underlie successful coaching, there is little research existing to clearly identify a theoretical basis within which HC operates. Better understanding of how coaching might drive behavior change (eg, via SDT) will lead to greater mechanistic understanding and acceptance of the coaching process. The purpose of this paper is to present the Ithaca Coaching Project as an example of an RCT studying the effectiveness and process of HC. In addition, this article addresses research design considerations, discusses methodological challenges, and identifies future directions for HC research.
ITHACA COACHING PROJECT
Rationale and Logic
Chronic disease, typically brought on by poor lifestyle decisions, is the primary cause of death and disability in the United States. Epidemiological data on more than 1.5 million claims indicated that heart disease, cancer, back/neck pain, other chronic pain, high cholesterol, hypertension, intestinal difficulties, diabetes, sleeping problems, arthritis, obesity, anxiety, depression, and allergies are the top reasons for medical, pharmacy, absenteeism, and presenteeism costs.1,2 Therefore, lifestyle-related disorders are the primary reason for poor employee health. Loeppke aptly points out that poor health raises medical costs while reducing productive capacity creating a cost burden for businesses.3 It is unlikely that the typical worker understands healthcare is consuming up to 25% of their potential salary and value to their company.4 According to a recent report,5 a summary of seven cost analysis studies revealed a $3.48 return on investment (ROI) for each corporate dollar spent on wellness programming. The workplace is therefore an excellent venue to study healthcare cost and wellness issues that challenge contemporary society.
Despite human suffering and healthcare cost burdens, people largely do not make healthy choices. Most people easily recognize maximizing wellness is a personal and societal priority because culturally available means (eg, television, websites, magazines, newspapers) as well as scientific publications, deliver the message daily. Yet many are not willing or able to manage a meaningful behavior change to positively impact their wellness. Findings from our previous work indicate that eliminating barriers of cost and improving access to information and wellness programming does not readily improve health status in an employee population.6 In recent years, the emergence of HC as a discipline and profession offers a new strategic prospect for promoting healthy behavior change. There are indications that HC is effective at promoting positive behavior changes.7–9 However, there are no large-scale RCTs using HC for primary prevention in a typical employee population. In this era of spiraling health-care costs, keeping the population free of chronic lifestyle-related disease is a crucial objective for workplace budget directors. Using coaching techniques to enhance wellness possesses tremendous untested potential as a mechanism to improve the population's health and keep employee healthcare costs in check.
Study Relevance and Objectives
The Ithaca Coaching Project is relevant because it is one of the first large-scale RCTs to examine HC for primary prevention and aims to provide data describing the effectiveness of coaching on behavior changes and health outcomes in an employee population. This project also examines theoretical foundations and the importance of theory application during implementation of HC. For example, understanding the role of SDT will allow a coach to gauge how much to emphasize strategies that develop autonomous motivation or competence in their clients. The future of coaching as a health and wellness intervention and as a profession is dependent on gathering such information that provides empirical evidence for the effectiveness of HC and allows codification of the process.
Specifically, the primary purpose of this research is to determine if HC enhances desired behavior change in an employee population such that greater wellness goal achievement, health status, and job performance are realized compared to a control. A secondary purpose of this project is to determine if SDT and particularly autonomous motivation and need satisfaction are foundational factors in the HC process.
Design and Methodology
The Ithaca Coaching Project is a four-group, randomized control study with each participant placed into one of three levels of coaching or a control/crossover group. The project is expected to be ongoing for 2.5 years but conducted for each participant in a 12-month timeframe with assessments every 3 months. Therefore, the project is a 4 (groups) x 5 (times) repeated measures factorial design examining group differences on outcome measures over 12 months. Outcome data on goal achievement, health status, job performance, and coaching processes are made at program entry and then again at 3, 6, 9, and 12 months. Figure 1 illustrates group and participant flow through the protocol of this longitudinal study. All data collection is single-blinded with those taking measures unaware which participants are receiving the coaching intervention. This study was approved by the Ithaca College Institutional Review Board on Human Subjects Research.
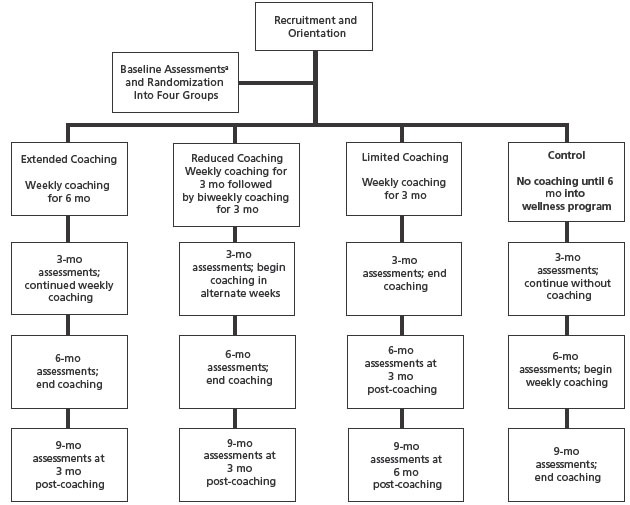
Figure 1 Group flow through Ithaca Coaching Project study protocol. All groups received a final assessment of outcome measures at 12 months.
a Outcome measures for assessments are further detailed in Table 1.
Setting and Participants.
Ithaca College employs more than 1400 people functioning as faculty, administration, support staff, and physical plant workers representing a broad spectrum of socioeconomic and educational backgrounds. As a newly available employee benefit, the office of human resources announced a campus-wide wellness initiative branded Mind, Body, Me (MBM). MBM is a multifaceted program with an educational component, health trackers, health risk appraisal, and small incentives (eg, coffee mug, T-shirt) for healthy behaviors. MBM is well promoted in campus literature, and employees sign up to enter the program in flights (ie, a group of employees entering the MBM program as a cohort) of 50 to 55 participants, with a new flight starting every 3 months. Employees are invited into the MBM program according to campus division (eg, Physical Plant, School of Music); however, any employee can ask to enter the program before their division is invited. The Ithaca Coaching Project is described to participants during MBM orientation. To be part of the coaching study, participants must be benefits-eligible employees of Ithaca College, between the ages of 18 and 65 years, and English-speaking with access to Internet and telephone services. Exclusion from the study occurs when a participant presents on their health risk appraisal (HRA) with a diagnosed Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) mental health disorder, though a treating physician can override exclusionary criteria via written notice provided to the patient. Other highly consuming conditions (eg, pregnancy, hemodialysis treatment, cancer diagnosis) that might obscure the coaching treatment also are exclusionary or reasons for withdrawal if such a condition arises over the intervention period. In other words, a “highly-consumig” condition is judged to present a potentially more significant and unpredictable effect on study outcomes than the coaching treatment might. At this point, we have removed only four participants from the study due to pregnancy. However, many functionally limited (eg, back pain) and high-risk (eg, diabetics, metabolic syndrome) participants have been and will be part of the final data analysis.
Recruitment, Sample Size, Stratification, and Randomization.
At an MBM flight orientation, a new member will schedule baseline assessments and be exposed to the assets available to them at no fee (eg, wellness clinic, fitness facility, group and personal exercise, website with education information and health trackers, periodic seminars). New MBM members also are given the opportunity to be part of the Ithaca Coaching Project during orientation with the promise of at least 3 months of free HC. The expectation for the coaching study is to recruit more than 300 participants over an 18-month period. A generalized a priori power analysis was performed using G*Power software (Heinrich-Heine-Universität Düsseldorf, Germany) given a four-group, repeated measures study design with numerous outcome variables. Assuming 15% to 20% attrition, the goal is to collect complete data on 240 to 255 participants in 30 months. This sample size estimate yields 85% to 90% power and type I error of 5% while also meeting the need for a large sample (>200) when performing a predictive path analysis. On entry into the coaching study, participants are randomly placed into one of four groups after stratification using age, gender, HRA score, and readiness to change health behavior. Readiness to change is measured with a simple question based on the Transtheoretical Model asking about desire to undertake new healthy behaviors. Stratification is finalized by ensuring that no significant between-group differences exist on each of these key baseline variables.
Health Coaching Intervention.
Participation in the study is in one of three levels of HC treatment or a control/crossover group. All coaching is conducted telephonically, and the three treatment arms are Extended Coaching (EC), Reduced Coaching (RC), and Limited Coaching (LC). The EC group receives 30 to 40–minute sessions of weekly coaching for 6 months; the RC receives the same for three months followed by a second 3-month period with coaching reduced to only two 30 to 40–minute sessions per month; and the LC group receives only the first 3 months of weekly coaching, after which coaching access is discontinued. Coach-client contacts (eg, email, text, phone) between scheduled coaching sessions might occur as needed; however, these interactions are only for logistical purposes (eg, to arrange meeting time) and not intended for use as a coaching mechanism. The control group has access to all benefits of the MBM program (eg, educational materials, seminars, exercise facility access), encouraging them to improve wellness; however, they are not offered HC. On program entry, the controls have an HRA review with a health professional and are asked to set personal health-related goals; no coaching strategies are employed in this session. After 6 months, the control group crosses over to treatment and is provided with 3 months of weekly coaching. All subjects are involved in the study for 12 months, with measurements made at baseline, 3-, 6-, 9-, and 12-month time-points. This design allows us to gain insight into the effects associated with varying the extent, or dose, of the coaching treatment. The study design also permits examining the stability of any coaching effect over time after treatment discontinuation.
Health Coaches.
HC is standardized using only experienced (>1 year posttraining) coaches who are similarly trained (ie, 3 months of basic coach training via Wellcoaches Corp, Wellesley, Massachusetts) and who possess a health-related bachelor's degree or above. This coach training uses a client-centered approach that, among other strategies, emphasizes relationship building, motivational interviewing, development of self-efficacy, and goal setting/achievement.10 In addition to basic training, all 13 coaches employed in this project took part in a 12-week advanced coach training program (90 min/wk) emphasizing understanding of mindfulness, autonomous motivation, positivity, and character strengths. After this extensive orientation, coaches met monthly for 6 months with the project principal investigator and will continue to meet bimonthly for the duration of the project. Regular coach communication is encouraged to potentially improve our process with each incoming flight of participants. An intervention check is employed for each client session, allowing coaches to record coaching strategies implemented. Intervention oversight is possible through coach supervision using a web-based review of coach notes and speaking with coaches to review record-keeping and coaching strategies.
Outcome Measures.
Outcome variables divide into four primary areas describing physical health status, emotional health status, job-related factors, and coaching-related factors (Table). Measurements include HRA, low-density lipoprotein (LDL) cholesterol, glucose, blood pressure, body mass index (BMI), body weight, waist circumference, and fitness (cardio-respiratory, strength, and flexibility capacities). The HRA is provided by ENI (Binghamton, New York) with their Health Risk Manager system used to assign participant health-risk scores based on questions about risk factors (eg, smoking, substance abuse) and lifestyle habits (eg, minutes of exercise, fruit/vegetable consumption). Goal achievement (percent attainment) is determined by coach-client discussion every 3 months in all groups, with the coach ultimately entering a score of 0% to 100% for each of the client's goals. A readiness for health behavior change scale is assessed, as are outcomes related to SDT involving measures of autonomy, competence, self-regulation, and autonomous vs controlled motivation (Self-regulation Questionnaire, SRQ).11 Productivity (presenteeism and absenteeism using World Health Organization Health and Work Perfor mance Questionnaire, HPQ12), job satisfaction (Michigan Organizational Assessment Ques tionnaire Job Satisfac tion Subscale, MOAQ-JSS13), and employee morale will be measured as well as life satisfaction (Satisfaction With Life Scale, SWLS14), wellness program satisfaction, health satisfaction (SF-815), stress (Psychological Stress Measure, PSM-916), pain management (modified Brief Pain Inventory, BPI17), and self-efficacy (PCS18). Program participation (eg, enrolling in wellness clinic, exercise program adherence) also will be tracked. All measures are made at the start and at 3-month intervals during the intervention period, so that five sets of measures will be collected on each participant over 1 year.
Table.
Four Outcome Domains for the Ithaca Coaching Project
| Outcome Domains | Baseline | 3-mo | 6-mo | 9-mo | 12-mo |
|---|---|---|---|---|---|
| 1) Physical health status | |||||
| Measures | |||||
| HRA score | ✓ | ✓ | ✓ | ✓ | ✓ |
| Blood pressure (systolic and diastolic) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Cholesterol (total, HDL, LDL) | ✓ | ✓ | ✓ | ||
| Glucose | ✓ | ✓ | ✓ | ||
| Cardiorespiratory capacity—estimated VO2 max | ✓ | ✓ | ✓ | ✓ | ✓ |
| Strength (handgrip test) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Flexibility (sit and reach test) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Body mass index | ✓ | ✓ | ✓ | ✓ | ✓ |
| Body weight | ✓ | ✓ | ✓ | ✓ | ✓ |
| Waist circumference | ✓ | ✓ | ✓ | ✓ | |
| 2) Emotional health status | |||||
| Measures | |||||
| Life satisfaction | ✓ | ✓ | ✓ | ✓ | ✓ |
| Health satisfaction | ✓ | ✓ | ✓ | ✓ | ✓ |
| Mindfulness | ✓ | ✓ | ✓ | ✓ | ✓ |
| Stress | ✓ | ✓ | ✓ | ✓ | ✓ |
| Pain | ✓ | ✓ | ✓ | ✓ | ✓ |
| 3) Job-related factors | |||||
| Measures | |||||
| Job satisfaction | ✓ | ✓ | ✓ | ✓ | ✓ |
| Employee morale | ✓ | ✓ | ✓ | ✓ | ✓ |
| Presenteeism | ✓ | ✓ | ✓ | ✓ | ✓ |
| Absenteeism | ✓ | ✓ | ✓ | ✓ | ✓ |
| 4) Coaching-related factors | |||||
| Measures | |||||
| SDT (autonomy, competence, self-regulation) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Self-efficacy | ✓ | ✓ | ✓ | ✓ | ✓ |
Abbreviations: HDL, high-density lipoprotein; HRA, health risk appraisal; LDL, low-density lipoprotein; SDT, self-determination theory; VO2 max, maximum oxygen consumption.
Data Analyses.
This study addresses four research questions with the following statistical analyses:
-
Does HC impact health, emotional status, or jobrelated factors more than simple access to wellness-promoting activities (ie, general MBM availability)?
Examining between group differences over time in the various health and wellness measures (eg, BMI, fitness, job satisfaction, stress) will determine if HC affected outcomes. General linear model analyses (eg, repeated-measure analysis of variance, RMANOVA) will be used for these comparisons.
-
Does level of HC impact health, emotional status, or job-related factors?
Examining the effect size generated from each of the three treatment groups will indicate the impact and dose-response relationship the intervention is likely to have at an individual, sample, or population level. Assuming a beneficial health impact in 3 months, the additional trials (over the second 3 months) begin to address how much coaching is needed to maintain desirable behaviors while continuing to monitor health status.
-
Does HC have a theoretical foundation related to SDT-demonstrated enhancing need satisfaction and autonomous motivation?
Using structural equation modeling and path analysis the effect of coaching on need satisfaction, motivation, and behavioral outcomes will be simultaneously examined and the relationships among these variables teased out. An example of findings that might result from such structural equation modeling is seen in Figure 2.
-
Does HC impact healthy behavior outcomes after 6 months of standard wellness care intervention?
Examining the crossover control group, will allow determination of coaching effectiveness after participants have had 6 months of opportunities for standard wellness care intervention (ie, MBM program) that did not include HC. General linear model analyses (eg, RMANOVA) will be used for these comparisons.
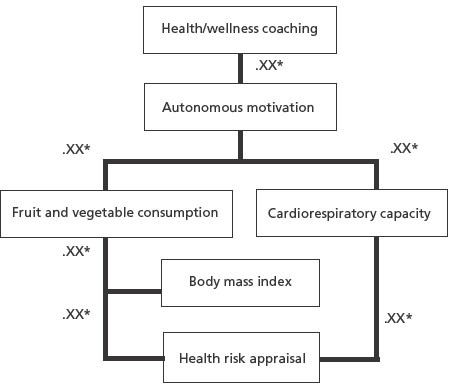
Figure 2 Speculative results of path analysis showing indirect effects with mediator variables between health coaching and health risk appraisal.
Note: These results are conjecture to display an example of the path model. .XX* indicates strength of a significant relationship with values unknown in this speculative example.
DISCUSSION
The Ithaca Coaching Project aims to study HC using a tightly designed RCT while providing a high level of standardization in the coaching process. If coaching is going to be accepted into the existing healthcare system, it must not only be viewed as a valuable intervention but the process must also be clearly defined. That is, health coaches must possess a common core of knowledge and ascribe to a similar set of effective, evidence-based intervention strategies. Others have called for standardization of health coaching and concluded that uniform training and credentialing are imperative to define the scope of practice for the HC profession.19 Such standardization and the research process are essential to understanding coaching best practices and identifying scope of practice. Relevant HC-related research can progress only if we share a common definition of the coaching process and future studies use appropriate research designs.
Health Coaching Research Design Considerations
Well-planned prospective intervention trials using well-established, reliable, and valid outcomes are needed to advance the HC knowledge base. These studies need to focus on a standardized coaching process emphasizing a client-centered, theory-based practice as more fully described elsewhere in a systematic review by Wolever et al.20 Experimental trials (by definition) should use appropriate control groups and whenever feasible, apply randomization for subject assignment to coaching conditions. Future researchers are advised to consider the implications of their recruitment strategies. For example, when answering the call for a “coaching study,” subjects expect to receive HC and likely will be disappointed if assigned to the control group. A disgruntled control group can undermine data collection and augment attrition. The Ithaca Coaching Project attempts to avoid this problem by promising our controls other wellness-related services (ie, the MBM program) and 3 months of coaching after a 6-month coach-free period. Another advertising strategy is to promote the study as a lifestyle intervention without mentioning “coaching.” However, this minor deception may be undone quickly in circumstances with coworker interaction.
Another recruitment-related issue for future coaching studies is the need to carefully consider readiness to change, as this presents a potential built-in bias in the recruitment process. Volunteers answering the call for inclusion in a “coaching study” are implicitly conveying they are prepared for change in some lifestyle variable. Accordingly, volunteers will express varying levels of motivation to start new healthy behaviors but few will be stuck in the pre-contemplation stage. Such positive bias must be considered when estimating the generalizability of the results. The Ithaca Coaching Project attempts to minimize this bias by measuring readiness to change and then stratifying before randomization to ensure all four groups start the study with similar levels of readiness to begin new healthy behaviors. Stratifying addresses one potential bias, but another methodological issue occurs as a function of participation in a longitudinal coaching study. With random group assignment, an occasional participant in the treatment group is resistant to coaching (“Just don't want to do it”), while another resists ending treatment at the stated termination point (“Right now, I can't imagine my life without my coach”). The Ithaca Coaching Project announces clear study expectations, and participants are enrolled only if they are willing to follow the protocol for their group assignment. Fortunately, these problems are the exceptions in our experience but do indicate potential difficulties inherent in designing RCT studies of the HC process.
When studying HC, it is logical that health-related goal achievement should be a primary outcome variable. Goal setting is a major strategy used by health coaches, and goal achievement is an important objective of the coaching process. Yet here lies a methodological trap for researchers. A basic tenet of the coaching process is to facilitate and evoke behavior change processes inherent to the client while not imposing externally controlling strategies.10 In other words, good HC is client-centered, and therefore the process does not allow for a required schedule when establishing personal goals. Sadly, this coaching tenet potentially conflicts with the good research practice of establishing a baseline, applying a standard treatment, and measuring related outcomes. We find that some clients establish many goals quickly while others take several sessions to determine a single, self-relevant goal. Thus, during a 12-week intervention, some clients may work on multiple goals for 12 weeks while others may address a single goal for 12 weeks and still others address one personal goal for 8 weeks and another goal for 6 weeks. Moreover, using the client-centered coaching approach, it is also common for a goal to be modified or dropped altogether, for a variety of plausible reasons (eg, “Work demands became too much,” “I began taking care of my aging parents,” “I was arrested”). Accordingly, the critical outcome measure of goal achievement sometimes can appear to the researcher as a moving target.
Future Directions in Health Coaching Research
It is apparent that there are difficulties to be recognized and addressed when doing HC research. Studies are seldom perfect, but investigators must strive to carefully consider design issues and produce high-quality data that can be accepted by scientific and medical communities. Future studies of coaching should carefully consider all aspects of methodological design and make decisions appropriate for the specific objectives, populations, and outcomes being examined. There is a wealth of critical work remaining for researchers who are willing to take on potential study design and measurement challenges to advance the knowledge base of HC practice.
Future studies of HC are needed to examine strategies of the coaching process, eg, Is increasing self-efficacy essential to the process of behavior change? To health outcomes? How much goal review is required for client success? Which components of the coaching process are best matched to which client characteristics, at which times? Can a certain type of motivational interviewing reflection style improve client response more than another? Until a working definition of HC is clearly presented and widely disseminated, such questions cannot be addressed consistently.20 Qualitative research examining themes and processes of coaching from perspectives of both coach21,22 and client are needed to more completely understand effective coaching. We also need studies of determinants of appropriate health coach dosing, eg, Is effective coaching dose related to stage of change or initial self-efficacy? Are 30- or 60-minute or open-ended sessions best for maximizing adherence to lifestyle changes or other outcomes? Number of sessions per month? Number of months to optimize cost:benefit? Moreover, HC investigations addressing specific populations (frail elderly, obese children, time-pressured employees) or specific outcomes (eg, living independence, happiness) will help to define scope of practice and effectiveness for the coaching profession. In the process, perhaps the most pressing concern is that a clear definition of HC emerges and evolves. This is an exciting time for researchers and practitioners in HC. There is much to do for abundantly important information and meaningfully critical intervention to be realized.
CONCLUSIONS
The Ithaca Coaching Project is now into a second year of recruitment with 262 participants already enrolled in the study. The plan is to enter one more flight of 50 to 55 participants and complete the study after following that final group for 12 months. This project is one of the first large-scale RCTs to examine HC for primary prevention. There is a great need for projects with similar and other well-conceived research designs addressing a plethora of exciting HC-related questions. The expectation is that we will learn much about the HC process and the effectiveness of coaching as an intervention for changing behavior and producing positive health-related outcomes. As a result, a clear definition and understanding of HC will emerge. With this knowledge, HC can be properly considered for integration into the healthcare system.
Acknowledgments
The Ithaca Coaching Project would not have taken shape without the support and vision of Mark Coldren and Robin Davis from the Ithaca College Office of Human Resources. Thanks to Dr Miranda Kaye and Frank Micale for their invaluable help in the planning of the project. A special thank you to Dr Ruth Wolever for her expert review of this article.
Finally, a score of students and hundreds of participants must be acknowledged as they are giving their best as this project marches forward.
Disclosure The Ithaca Coaching Project was supported in part by a grant from the Institute of Coaching, McLean Hospital, a Harvard Medical School affiliate. The author completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and disclosed no other potential conflicts of interest.
REFERENCES
- 1.Loeppke R, Taitel M, Richling D, et al. Health and productivity as a business strategy. J Occup Environ Med. 2007;49(7):712–21 [DOI] [PubMed] [Google Scholar]
- 2.Loeppke R, Taitel M, Haufle V, Parry T, Kessler RC, Jinnett K. Health and productivity as a business strategy: A multiemployer study. J. Occup Environ Med. 2009;51(4):411–28 [DOI] [PubMed] [Google Scholar]
- 3.Loeppke R. The value of health and the power of prevention. Intern J Workplace Health Manage. 2008;1(2):95–108 [Google Scholar]
- 4.Goldhill D. The health benefits that cut your pay. The New York Times. February17, 2013:SR6 [Google Scholar]
- 5.Annand-Keller P, Lehmann D, Milligan K. Effectiveness of corporate well-being programs. J Macromarketing. 2009;29(3):279–302 [Google Scholar]
- 6.Sforzo GA, Kaye M, Calleri D, Ngai N. Free choice access to multipoint wellness education and related services positively impacts employee wellness: A randomized and controlled trial. J Occup Environ Med. 2012;54(4):471–7 [DOI] [PubMed] [Google Scholar]
- 7.Jaarsma T, van der Wal MH, Lesman-Leegte I, et al. Effect of moderate or intensive disease management program on outcome in patients with heart failure. Arch Intern Med. 2008;168(3):316–24 [DOI] [PubMed] [Google Scholar]
- 8.Anshel M, Brinthaupt T, Kang M. The disconnected values model improves mental well-being and fitness in an Employee wellness program. Behav Med. 2010;36(4):113–22 [DOI] [PubMed] [Google Scholar]
- 9.Prochaska JO, Evers KE, Castle PH, et al. Enhancing multiple domains of well-being by decreasing multiple health risk behaviors: a randomized clinical trial. Popul Health Manag. 2012;15(5):276–86 [DOI] [PubMed] [Google Scholar]
- 10.Moore M, Tschannen-Moran B. Coaching psychology manual. Baltimore, MD: Lippincott, Williams & Wilkins; 2010 [Google Scholar]
- 11.Ryan RM, Connell JP. Perceived locus of causality and internalization: Examining reasons for acting in two domains. J Pers Soc Psychol. 1989;57(5):749–61 [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, Barber C, Beck A, et al. The World Health Organization Health and Work Performance Questionnaire (HPQ). J Occup Environ Med. 2003;45(2):156–74 [DOI] [PubMed] [Google Scholar]
- 13.Bowling NA, Hammond GD. A meta-analytic examination of the construct validity of the Michigan Organizational Assessment Questionnaire Job Satisfaction Subscale. J Vocational Behav. 2008;73(1):63–77 [Google Scholar]
- 14.Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. J Pers Assess. 1985February;49(1):71–5 [DOI] [PubMed] [Google Scholar]
- 15.Ware JE, Kosinski M, Dewey JE, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-8 health survey. Lincoln, RI: Quality Metric Inc, 2001 [Google Scholar]
- 16.Lemyre L, Lalande-Markon MP. Psychological stress measure (PSM-9): Integration of an evidence-based approach to assessment, monitoring, and evaluation of stress in physical therapy practice. Physiother Theory Pract. 2009;25(5-6):453–62 [DOI] [PubMed] [Google Scholar]
- 17.Cleeland CS. Measurement of pain by subjective report. In: Chapman CR, Loeser JD, editors. Issues in pain management. Advances in pain management. Vol 12 New York,: Raven Press; 1989:391–403 [Google Scholar]
- 18.Williams GC, Deci EL. Internalization of biopschosocail values by medical students: A test of self-determniation. J Pers Soc Psychol. 1996April;70(4):767–79 [DOI] [PubMed] [Google Scholar]
- 19.Wolever RQ, Eisenberg DM. What is health coaching anyway? Arch Intern Med. 2011;171(22):2017–18 [DOI] [PubMed] [Google Scholar]
- 20.Wolever RQ, Simmons LA, Sforzo G, et al. A systematic review of the literature on health and wellness coaching through 2012: defining and operationalizing a key behavioral intervention in health care. Global Adv Health Med. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolever RQ, Caldwell KL, Wakefield JP, et al. Integrative health coaching: An organizational case study. Explore (NY). 2011;7(1):30–6 [DOI] [PubMed] [Google Scholar]
- 22.Caldwell KL, Grey J, Wolever RQ. The process of patient empowerment in integrative health coaching: How does it happen? Global Adv Health Med. 2013. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]


