Abstract
Background:
Health coaching is a client-centric process to increase motivation and self-efficacy that supports sustainable lifestyle behavior changes and active management of health conditions. This study describes an intervention offered as a benefit to health plan members and examines health and behavioral outcomes of participants.
Methods:
High-risk health plan enrollees were invited to participate in a telephonic health coaching intervention addressing the whole person and focusing on motivating health behavior changes. Outcomes of self-reported lifestyle behaviors, perceived health, stress levels, quality of life, readiness to make changes, and patient activation levels were reported at baseline and upon program completion. Retrospectively, these data were extracted from administrative and health coaching records of participants during the first 2 full years of the program.
Results:
Less than 7% of the 114 615 potential candidates self-selected to actively participate in health coaching, those with the highest chronic disease load being the most likely to participate. Of 6940 active participants, 1082 fully completed health inventories, with 570 completing Patient Activation Measure (PAM). The conditions most often represented in the active participants were depression, congestive heart failure, diabetes, hyperlipidemia, hypertension, osteoporosis, asthma, and low back pain. In 6 months or less, 89% of participants met at least one goal. Significant improvements occurred in stress levels, healthy eating, exercise levels, and physical and emotional health, as well as in readiness to make change and PAM scores.
Discussion:
The types of client-selected goals most often met were physical activity, eating habits, stress management, emotional health, sleep, and pain management, resulting in improved overall quality of life regardless of condition. Positive shifts in activation levels and readiness to change suggest that health coaching is an intervention deserving of future prospective research studies to assess the utilization, efficacy, and potential cost-effectiveness of health coaching programs for a range of populations.
Key Words: Health coaching, Patient Activation Measure, chronic disease, quality of life
摘要
背景: 健康辅导是一个以患者为 中心的流程,用以提高积极性和 自我效能,并支持可持续的生活 方式行为改变和积极的病症管 理。本研究将介绍一种对健康计 划成员有益处的干预方法,并剖 析参与者的健康和行为结果。
方法:邀请高风险的健康计划登 记者参与针对整个人及关注激励 健康行为变化的电话健康辅导干 预。在基线和计划完成时对自我 报告的生活方式行为、自感健 康、压力水平、生活质量、改变 愿意度及患者积极水平的结果进 行报告。回顾一下,该数据摘自 计划最初 2 年参与者的管理和健 康辅导记录。
成效:114 615 名潜在候选人中不 到 7% 自我选择积极参与健康辅 导,慢性疾病负荷最高的患者参 与几率最大。6940 名积极参与者 中,1082 人完全完成了健康量 表,570 人完成了患者积极度量 表 (PAM)。积极参与者中最常见 的病症是抑郁症、充血性心脏衰 竭、糖尿病、高脂血、高血压、 骨质疏松症、哮喘以及腰痛。在 6 个月或更少的时间内,89% 的参 与者至少实现了一个目标。在压 力水平、健康饮食、锻炼水平及 身体和情感健康、以及改变愿意 度和 PAM 分数上得到明显改善。
讨论:最常见的患者选择的目标 类型为体力活动、饮食习惯、压 力管理、情绪健康、睡眠及疼痛 管理,无论患何种病症,最后都 能提高整体生活质量。积极水平 和改变愿意度出现的积极变化表 明健康辅导是值得进行未来预期 调查研究的干预方法,它可用来 评估健康辅导计划对大范围人群 的使用、效果和潜在的成本效益。
SINOPSIS
Fundamentación:
La formación sanitaria es un proceso centrado en el cliente que incrementa la motivación y la autoeficacia, lo que favorece cambios sostenibles en el estilo de vida y una gestión activa de las condiciones de salud. Este estudio describe una intervención ofrecida como ventaja social para los miembros de un plan de salud y pasa revista a los resultados sanitarios y conductuales de los participantes.
Métodos:
Se invitó a personas de alto riesgo inscritas en un plan de salud a participar en una intervención de formación sanitaria por teléfono dirigida hacia la persona en su conjunto y centrada en la motivación para lograr cambios conductuales relacionados con la salud. Se obtuvieron resultados en cuanto a comportamientos declarados en relación con el estilo de vida, al estado de salud percibido, los niveles de estrés, la calidad de vida, la disposición a realizar cambios y los niveles de activación de los pacientes, tanto en el momento inicial como una vez finalizado el programa. Retrospectivamente, estos datos se extrajeron de documentos administrativos y de formación sanitaria de los participantes durante los 2 primeros años completos del programa.
Resultados:
Menos del 7 % de los 114.615 posibles candidatos se autoseleccionaron para participar activamente en la formación sanitaria, siendo aquellos que presentaban una mayor carga de enfermedad crónica los que mostraron mayor tendencia a participar. De los 6940 participantes activos, 1082 rellenaron íntegramente los inventarios de salud y 570 cumplimentaron el cuestionario de Medición de la activación del paciente (Patient Activation Measure, PAM). Las enfermedades representadas con más frecuencia entre los participantes activos fueron depresión, insuficiencia cardíaca congestiva, diabetes, hiperlipidemia, hipertensión, osteoporosis, asma y lumbalgia. En 6 meses o menos, el 89 % de los participantes lograron al menos un objetivo. Se obtuvieron mejorías significativas en los niveles de estrés, la alimentación sana, los niveles de ejercicio, y la salud física y emocional, así como en la disposición a introducir cambios y en las puntuaciones de PAM.
Discusión:
Los tipos de objetivos seleccionados por los clientes que se consiguieron con más frecuencia fueron la actividad física, los hábitos alimenticios, la gestión del estrés, la salud emocional, el sueño y el control del dolor, lo que dio lugar a una mejora general de la calidad de vida independientemente de la dolencia. Los cambios positivos en los niveles de activación y en la disposición a cambiar indican que la formación sanitaria constituye una intervención que merece futuros estudios de investigación prospectivos para evaluar la utilización, la eficacia y la posible rentabilidad de los programas de formación sanitaria para diversos sectores de población.
INTRODUCTION
During the last decade, the United States has witnessed the accelerated inflation of health care costs and a growing burden of chronic disease including obesity. In 2012, the Centers for Medicare and Medicaid Services projected that health spending will account for 19.6% of the gross domestic product (GDP) in 2021, up from 17.9% in 2010.1 While existing conventional interventions, including disease and case management services, in some instances have improved clinical processes of care, they have not led to significant or sustainable changes in the health-related behaviors that are critical for increasing the health status of Americans and decreasing the cost of healthcare.2 For over a decade, health risk assessments have been in common use but have been inadequately effective in identifying or fostering the self-management strategies necessary for achievement of sustainable improved health behaviors that impact both current health status and future risks.
The new field of health coaching that has emerged in the last decade intentionally applies the concepts of change theory, self-efficacy, patient activation, and motivational interviewing. However, the term health coach is applied to a wide range of practitioners—some who place more emphasis on education, some on navigation, some on advocacy, and some who persist in taking a more directed management approach. The emergence of health and wellness coaching within integrative healthcare3 has perhaps been the most clearly described and has also demonstrated initial efficacy.4 While some early studies suggest effectiveness of this approach, interventions are often not clearly defined or described well in the literature.5 The field of health and wellness coaching is still creating a distinct identity and a model for evaluation that seeks more substantial proof of efficacy and effectiveness.
In 2008, a nonprofit health plan that provides health management services in the upper midwestern United States developed a health coaching program with the goal of impacting the areas of clinical quality, patient satisfaction, and the affordability of healthcare. This new programmatic addition was intended to be a shift from a disease-centric model, which had not optimally achieved the desired endpoints, to a wellnesscentric model. During the last 2 decades, disease management has been an approach to improving or maintaining health in large populations challenged with common chronic illnesses and the reduction of future associated complications of those illnesses. It emphasizes coordinated and comprehensive care built upon evidence-based clinical guidelines, pathways, and algorithms.6 With an emphasis on educational programs for self-management skills, giving feedback to health-care providers, and patient financial incentives to promote adherence to practice guidelines, the dominant focus of such approaches is the disease itself and not specifically the behavior or individualized needs of the patient.7 In contrast, health coaching focuses on the client-identified priorities and goals and seeks to support health behavior change specific to individuals rather than as prescribed only by nature of their illnesses. Health coaching is a relationship-based process of empowerment and support for client-directed lifestyle and behavior changes that is augmented with health education and promotion. Health coaches partner with clients to develop the clients' own goals using tools of active listening and powerful questioning. Health coaching focuses on increasing client-intrinsic motivation and self-efficacy, teaching self-management skills, and providing education to enhance the overall healthcare experience (eg, stress reduction, how to recognize medication side effects, condition-specific education). Health coaches develop a peer relationship that attends to the whole person and supports him or her in the health behavior change process. Table 1 presents features of health coaching compared to a disease and case management approach.
Table 1.
Characteristics of the Health Coaching Approach vs the Disease and Case Management Approach
| Health Coaching Approach | Disease and Case Management Approach |
|---|---|
| Person-focused | Disease-focused |
| Member's agenda | Provider or health plan's agenda |
| Collaborative | Prescriptive |
| Health behavior change | Adherence to treatment |
| Relationship-based | Task-based |
The basis for coaching draws from behavior change theories, including Hibbard's work in patient activation,8,9 the Prochaska and DiClemente Transtheoretical model,10,11 which defines stages of change, and Self-efficacy Theory,12 Health Belief Model,13 and Social Cognitive Theory.12 Communication methods draw from motivational interviewing14 to enhance intrinsic motivation to change and improve treatment adherence and positive psychology15,16 via strengths-based coaching, which is much more powerful than trying to improve weaknesses. Paying attention to people's strengths and not their deficits can give individuals the confidence to make the behavior changes they want and need to live healthier lives.
The creation of such a groundbreaking program required the education of a team of individuals who could deliver such services. Through collaboration with the leaders of an academic graduate program in integrative health coaching at the Center for Spirituality and Healing at the University of Minnesota, a team-based 200-hour educational program for health professionals employed as coaches within the health plan was developed. Approximately 30 individuals with a minimum of a bachelor's degree and healthcare backgrounds in nursing, psychology, social work, exercise physiology, nutrition education, and/or health education were employed and then trained as health coaches. The coaches participated in this custom-designed curriculum in health coaching and have since received ongoing professional development. Having a uniform and consistent training program ensured a common philosophical base for practice across coaches.
Health coaching services have been provided as a benefit to targeted high-risk health plan enrollees and other interested eligible health plan members since the fall of 2008. This paper reports on the observational data that was extracted from administrative and health coaching records that reported the experience of participants during 2009 and 2010, to the extent that it was available, in an effort to generate hypotheses and methods to be used for subsequent prospective, observational, and/or randomized trials. This article includes a description of the intervention, the enrollment process, the demographic and clinical profiles of the participants, and the patterns of engagement in the coaching process. Outcomes comparisons are made between baseline and postcoaching measures of general health, quality of life (QOL), self-reported markers of disease and risk, stress perceptions, and (for clients enrolled after a certain date) patient activation measures (PAM). Approval for this retrospective study was obtained from the University of Minnesota Institutional Review Board.
METHODS
Recruitment and Study Population
The health plan included a membership of approximately one million adults during the study period, representing nearly 30% of the population across the state of Minnesota and counties in North Dakota, South Dakota, and Wisconsin. Membership included individuals from Medicaid, Medicare, and commercial insurance plans. The study included only adults as the Health and Wellness Coaching Program was offered to members between the ages of 18 and 80 years who were not excluded for severe mental health issues (eg, schizophrenia, dementia) or active participation in other health management services, such as healthy pregnancy or smoking cessation programs. Potential participants for health coaching were identified by the health plan using a predictive model indicating the likelihood of benefit from the health and wellness coaching program (due to increased healthcare claims or elevated score on health risk assessments) or were referred by their medical care provider. Eligible members also were offered the opportunity to self-enroll based on their desire to improve their health.
Study Participants
Outcomes data analysis was done on those members who met the following inclusion criteria (Figure 1):
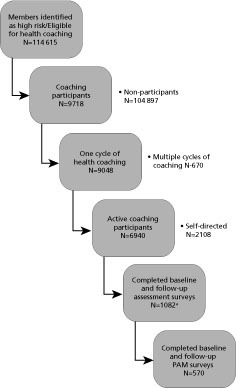
Figure 1 Study participants.
a Baseline surveys were done ±90 days of first health coaching session date and follow-up surveys were done ±90 days of last health coaching session date. Baseline and follow-up survey dates were at least 20 days apart. Abbreviation: PAM, Patient Activation Measure.
Completed the same version of pre-QOL and post-QOL assessment surveys, including questions concerning motivation, confidence, and readiness for change;
participated in coaching for a minimum of 28 days;
completed pre-QOL survey within 90 days prior to coaching and completed post-QOL within 90 days of the last session;
completed pre-QOL and post-QOL survey at least 20 days apart; and
provided PAM scores during the later half of the study period, beginning in October 2009 (only a subset of the study population).
Health Coaching: The Intervention
This program addressed the whole person and focused on health behavior change, increasing intrinsic motivation and self-efficacy, and teaching the member self-management skills and how to become a more empowered and engaged healthcare consumer. Coaching participants were assigned a dedicated health coach who worked with the member to address issues and goals identified by the member (patient-centric) based upon his or her own values and personal vision for health. This holistic perspective included not only the physical but also the mental, emotional, spiritual, and relational aspects of well-being and did not focus on diagnosis, disease complications, or limited symptom management. This is consistent with the model of integrative health coaching (IHC) described by Wolever17 and Edelman,18 with the exception of the application of and referral to nonconventional healthcare providers. The sessions focused on the process of coaching, which is about self-discovery and empowerment, commonly with the setting of self-selected goals. The client, with the support of the coach, was able to generate his or her own health plan. Though the coach may at times have provided information about resources or instruction in a skills practice, the predominant focus of coaching sessions was self-directed and not educational.
The training curriculum for the initial coaches was designed to enable them to develop a collaborative relationship with members in a way that attends to the whole person and supports him or her in the behavior change process. The coaches were trained to use active listening and powerful questioning to partner with members to develop their own goals. The coaching focus was on increasing motivation and self-efficacy, teaching self-management skills, and providing education to enhance the member's overall healthcare experience. Curricular content included the coaching process, therapeutic relationship, authentic communication practices, presence, motivation and behavior change theories, self-awareness, stress management, and emotional intelligence. The training process included extensive experiential practice, including mock telephonic sessions.
The coaching process is relationship-based with members working with the same coach throughout the program unless the member requested otherwise. All interested participants could choose to enroll in either an active coaching track or a self-directed track. The members who participated in active coaching are the subjects of this evaluation. These members engaged in coaching sessions scheduled at their convenience, initiated ad hoc coaching sessions as needed, and actively worked on self-selected goals and health behavior changes. The number and frequency of these calls varied by client choice. Active members remained in the program for approximately 6 months, depending on their needs. On average, these members participated in eight phone sessions (one initial assessment, six coaching sessions, and one end-of-program evaluation session).
Once enrolled, an active coaching client received an assessment that provided information to the coach about the member's needs and goals related to his or her health, helped determine the member's readiness to make lifestyle and behavior changes, and identified the member's level of self-management knowledge, skills, and confidence. The client set his or her own goals and priorities, and most clients set multiple goals. In successive sessions, the member also could choose to change or add goals. The health coach helped clients frame their health improvement goals using SMART (specific, measurable, attainable, relevant, and time-sensitive) language.19
The coach worked with the client to create an individualized health improvement plan with interventions and milestones. Telephonic coaching sessions and personalized educational mailings, proactive coordination and referral to services and resources, and subsequent assessments were tailored to the member's health improvement plan. The health coach guided the member in developing the skillset to build and establish a collaborative and effective relationship with his or her primary care provider and other care providers (eg, doctors, home care providers, social workers) who were part of their healthcare support system. Members received a workbook that addressed health behavior change, stress management, healthful living tips, and several exercises to support the member in the health improvement journey.
Research Methodology
This research is the result of an observational study of the experience of health plan members who participated in a health coaching program between January 1, 2009, and December 31, 2010. Membership data were extracted from the Health Management Data System to include all members who were identified for and/or participated in the health coaching program during the study period.
Descriptive statistics are provided for numbers of members (identified, participated, completed); demographic, psychosocial, and clinical characteristics of participants; and characteristics of coaching sessions (numbers and goals). Pre- and post-intervention levels of measures on patient health assessments were evaluated to determine program effects on self-reported health status, QOL, and PAM. The PAM was put into use as of October 2009.
RESULTS
A total of 114 615 members were identified during the study period. Less than 7% of potential candidates actively participated in health coaching. Compared with the identified and solicited population to whom services were offered but who did not enroll, the enrolled members tended to be older (50-64 y), female, and having more disease conditions (3.38 vs 2.88). The clinical conditions represented more often in the active vs nonparticipating members included depression, congestive heart failure, diabetes, hyperlipidemia, hypertension, osteoporosis, asthma, and low back pain. Commercially insured members were more likely to enroll than were Medicare or Medicaid members, but this could be secondary to differing marketing approaches rather than to actual population differences. For detailed descriptive statistics of members who were identified for, enrolled, or did not enroll in coaching, see the Appendix.
Of the 6940 active participants, the subset of active participants for whom we had complete data (preintervention and postintervention health assessments) was 1082. Among these members, 81% were between the ages of 40 and 65 years old, 70% were female, 80% lived in urban areas, 79% were privately insured, and 19% were on Medicare or Medicaid. The clinical profile of these members showed that 95% had at least one chronic condition. The average number of chronic conditions was 3.4. The top chronic conditions were depression (48%), hypertension (53%), low back pain (47%), hyperlipidemia (53%), asthma (24%), diabetes (24%), and seizure disorders (22%). This subset tended to be slightly older than the group as a whole: 81% were between the ages of 40 and 65 compared to 56% of the total. The clinical profile of these members was representative of the larger group of active participants.
Clients identified one or more goals for themselves in different areas of lifestyle. These are detailed in Table 2. Lifestyle goals were set and sometimes changed or added to by the participants themselves. Ninety-nine percent of active participants had identified at least one such goal. The average number of lifestyle goals identified was seven, and 89% met at least one goal. The most commonly selected goals were in the areas of general QOL, nutrition, and weight loss.
Table 2.
Lifestyle Goals
| Goal Description | Set Goal (%) | Achieved Goal (%) |
|---|---|---|
| Quality of life | 46.8 | 54.3 |
| Nutrition/weight management | 19.4 | 52.3 |
| Medication use | 8.1 | 33.5 |
| Exercise | 7.5 | 65.7 |
| Sleep improvement | 6.7 | 44.5 |
| Work/productivity | 5.3 | 53.6 |
| Safety | 3.4 | 44.0 |
| Tobacco cessationa | 2.8 | 28.7 |
These members were always referred for additional specific tobacco cessation programs as well.
The impact of coaching on client empowerment was assessed using measures of confidence, motivation, readiness for change, and activation. Outcomes are summarized in Table 3 and Figure 2.
Table 3.
Client Empowerment Markers
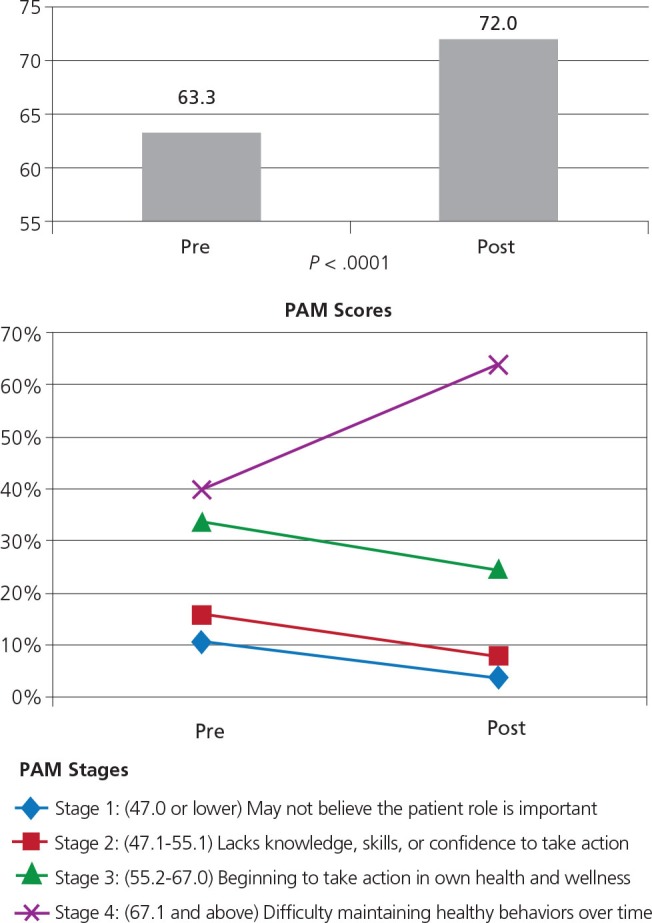
Figure 2 Patient Activation Measure (PAM) scores: N=570.a Active participants completed a before and after PAM; individuals realized an average of an 8 to 9–point increase in PAM scores out of 100.
a The subset of participants for whom we had complete pre- and post-PAM data.
Of the 6940 active participants, full QOL data were collected on 1082 participants and before and after PAM questionnaires were collected from 570. This was explained in part by the late addition of the PAM instrument to the standard coaching procedure (October 2009). PAM scores advanced one to three stages in the postintervention period for 42% of the participants for whom we had data, with an average of an 8 to 9–point increase in total PAM scores, demonstrating increased knowledge or confidence or beginning to take action in health behaviors. An examination of the relationship between number of coaching sessions and change in PAM scores revealed no significant dose-response trend. In an analysis of variance between change in PAM score and number of goals met, we found a strong positive association between change in PAM scores and the number of goals met. An increase of 10 points on PAM was associated with an increasing number of total goals met; however, the clinical significance of this numeric trend is unclear.
In evaluating other differences between the set of clients who completed both before and after PAM and those who did not, we found that those with more chronic disease conditions and those who stayed in coaching longer were less likely to have completed both PAM surveys.
The impact of lifestyle changes and goal achievement on QOL measures is summarized in Table 4. There were many significant improvements, including areas not specifically targeted in the documented goal setting, including decrease in pain, improvement in sleep, better relationships, and general increases in holistic aspects of health.
Table 4.
Changes in Health Status and Quality of Life Measures Pre- and Post-participation in Health Coaching (N=1082)
| Aspect of Health | % Positive Changea |
| Decrease in wanting eating habits to change | 18.3 |
| Increase in limiting fat in foods most of the time | 12.8 |
| Decrease in wanting physical activity to change | 16.3 |
| Increase in being very satisfied with physical activity level | 20.9 |
| Decrease in pain interfering with normal activity | 10 |
| Increase in sleeping well | 10.6 |
| Decrease in loss of interest in doing things most of the time | 8.1 |
| Decrease in high levels of stress | 11.9 |
| Decrease in high levels of relationship stress | 5.9 |
| Increase in good relationship health | 9.2 |
| Increase in self-rated good physical health | 11.6 |
| Increase in self-rated good emotional health | 15.4 |
| Increase in self-rated good social health | 7.5 |
| Increase in self-rated good spiritual health | 6.4 |
P < .001
DISCUSSION
The intention that led to the development and implementation of a health coaching program was to refocus the approach in population health management to be one that is patient-centric and wellness-focused. Health coaching shifted the focus from a directive disease management approach to a more collaborative and self-directed process, resulting in significant improvements in patients' QOL and potentially decreasing the long-term healthcare needs of individuals with chronic disease. Research on the health coaching process—including identifying the optimal population; the timing and length of intervention; predictors of success; role of intrinsic and extrinsic motivators; impact of specific coach/client relationship; and demonstration of increased achievement of sustainable behavioral changes (over other supportive interventions)—is still in its infancy. It was our intention through this retrospective analysis to identify trends and generate data that would inform larger, more definitive prospective studies.
It was also one of the heath plan's goals to evaluate the receptivity on the part of a high-risk population to accept health coaching at a similar or higher rate than disease management. Given the size of the eligible pool of members to whom this service was offered, the percentage that chose to participate was remarkably small and self-selected. While growing public familiarity with the practice of health coaching may increase consumer interest, health coaching, within this pilot, did not appear to be a service sought out from their health plan by the majority of clients with disease challenges. This is consistent with disease management program offerings that have reported low percentages of participating members out of the eligible pool.20 This may be due to the lack of awareness or understanding of the offered service, though it is possible that factors like the level of intrinsic motivation, existing engagement in self-directed health efforts, and intensity of disease also influence the likelihood of voluntary participation. These issues will require further examination to specify the factors that influence voluntary participation. It was notable that in this study, the more significant the chronic disease load, the more likely clients were to voluntarily participate in coaching. This is congruent with the findings of Buntin et al, who noted that diabetic patients who were sicker by disease markers were more likely to volunteer for a coaching intervention.20
While members were not required to set working goals, 99% identified at least one goal. Indeed, most (93%) had three or more goals, and 89% of these individuals met at least one goal. While the content of the goal varied, we found significant increases in the percentage of individuals who indicated higher motivation and confidence in their ability to make changes. Per the Prochaska model,10 more than a third of those coached reported increased levels of readiness to change. Additionally, the PAM shifted upward, with significantly more clients having moved through initiating action into maintenance. Because of the relatively small numbers for whom we had complete PAM data, it was not possible to identify a correlation between particular incoming activation levels and likelihood of success with the coaching intervention. This is an area that is ripe for further exploration.8,21
The nature of lifestyle goals, which were client-selected and often successfully met, encompassed areas of physical activity, eating habits, stress management, emotional health, sleep, and pain management. These aspects of health impact the QOL of all individuals regardless of disease specifics. This strongly suggests that the intervention of health coaching has the potential to be widely effective across categories of illness. Indeed, the higher the disease load, the more effective—and necessary—health coaching may be.
One of the interpretive limitations of such a retrospective analysis is that the number of clients for whom we had completed before and after data was small relative to the total number of participants. Preselecting validated and consistent instruments, training all practitioners on the importance of gathering the data, and having a system in place to support consistent data collection efforts (with prompts and reminders) would be critical aspects of any prospective study that seeks to demonstrate both the effectiveness and cost impact of a coaching intervention.
Dose-response studies of coaching for specific clinical conditions and goal types also would be very helpful for both greater clinical understanding and resource management. We did find that the more chronically ill and those who participated in coaching the longest were the groups least likely to have complete before and after PAM data for analysis. This situation points again to the importance of complete data collection in a prospective study. Nine percent of participants moved in a negative direction in the PAM quadrants after participation, a trend that may be explained by the coaching process resulting in increased client self-awareness and/ or more honest assessment of actual behaviors.
The overall impact of this health coaching program did measurably improve the participants' self-reported health status and QOL. Participants reported improvements in stress levels, motivation and confidence to make change, and PAM. These findings were not specific to any particular health issue. While the coaching intervention is not disease-specific in content or structure, future well-powered and prospective studies that examine the clinical and cost-effectiveness of a current usual care, disease and case management model vs a health coaching intervention as well as health coaching vs usual care in specific illness populations (eg, metabolic syndrome, diabetes, chronic back pain) would be informative in determining the best approaches for both clinical practices and third-party payors. Future studies will focus on both the content and process of the coaching intervention associated with achievement of not only self-reported outcomes but also on biometrics, such as lab studies, body mass index, weight, blood pressure, etc.
In summary, this was a preliminary observational study to generate hypotheses for future research. The participation rates for this intervention, which was offered to patients within the benefits of their health plan, were surprising low and deserve further exploration. Based upon the findings of this initial analysis, this commercial health and wellness coaching program has the potential to improve the health of the population it serves and reduce overall health-related expenditures in selected populations. Further exploration of innovations in the delivery of coaching services and tailored approaches for specific topics and populations are needed.
Acknowledgment
The studies described were funded by a grant from the Medica Research Institute.
Appendix.
Sample Characteristics of Health Plan Population Identified for Health Coaching (N = 114 615) and Enrolled at Member Level
| Characteristic | Didn't Enroll n = 104 897 | Enrolled n = 9718 | Significance t test/chi square |
|---|---|---|---|
| Demographics | |||
| Age, y | |||
| Average age for < 65 yrs | 44.9 | 49.2 | <.0001 |
| 18-25 | 10.30% | 5.25% | <.0001 |
| 26-29 | 7.51% | 4.47% | <.0001 |
| 30-39 | 18.14% | 12.96% | <.0001 |
| 40-49 | 21.95% | 21.26% | 0.1133 |
| 50-59 | 26.74% | 34.29% | <.0001 |
| 60-64 | 10.33% | 16.27% | <.0001 |
| 65 and older | 5.02% | 5.52% | 0.0349 |
| Gender (% male) | 36.11% | 30.20% | <.0001 |
| Rural/urban (% rural) | 16.16% | 16.38% | 0.5804 |
| Insurance type (% fully insured) | 84.45% | 83.35% | 0.0043 |
| Health Status | |||
| Risk Score - ACG-DxRx | |||
| Mean Number of conditions | 2.88 | 3.38 | <.0001 |
| % with any condition(of the 20) at any point | 91.03% | 94.38% | <.0001 |
| Age-related macular degeneration | 0.64% | 0.88% | 0.004 |
| Bipolar disorder | 4.59% | 4.77% | 0.3944 |
| Congestive heart failure | 4.63% | 5.48% | 0.0001 |
| Depresseion | 47.69% | 51.09% | <.0001 |
| Diabetes | 17.47% | 21.34% | <.0001 |
| Glaucoma | 5.19% | 7.66% | <.0001 |
| HIV | 0.79% | 0.67% | 0.1866 |
| Hyperlipidemia | 37.42% | 47.17% | <.0001 |
| Hypertension | 43.44% | 51.13% | <.0001 |
| Hypothyroidism | 11.44% | 15.54% | <.0001 |
| Immunosuppressed after transplant | 0.58% | 0.72% | 0.0883 |
| Inflammatory heart disease | 6.76% | 8.35% | <.0001 |
| Osteoporosis | 4.61% | 7.23% | <.0001 |
| Parkinson's disease | 2.67% | 3.48% | <.0001 |
| Persistent asthma | 25.32% | 28.87% | <.0001 |
| Rheumatoid arthritis | 4.41% | 5.44% | <.0001 |
| Schizophrenia | 3.50% | 3.16% | 0.3231 |
| Seizure disorder | 19.35% | 20.98% | 0.0001 |
| Chronic obstructive pulmonary disease | 4.41% | 5.22% | 0.0002 |
| Low back pain | 42.82% | 48.45% | <.0001 |
| Market Segment/Insurance Status | |||
| Non-government/Individual (n = 1188) | 0.98% | 1.63% | <.0001 |
| Fully insured | 0.98% | 1.63% | |
| Commercial (n = 74 008) | 64.49% | 65.39% | 0.0762 |
| Fully insured | 48.96% | 48.74% | |
| Self insured | 15.54% | 16.65% | |
| Govt (n = 39398) | 34.51% | 32.95% | 0.002 |
| Fully insured | 34.51% | 32.95% | |
| Self insured | 0% (n = 1) | 0.00% | |
Abbreviation: ACG, Adjusted Clinical Group.
The ACG-ĐRxDx combines diagnostic and medication codes to build a risk score.
Disclosures Drs Lawson, Jonk, O'Connor, and Eisenberg disclosed receipt of financial support from the University of Minnesota. Drs Sundgaard Riise and Kreitzer declared no potential conflicts of interest.
Contributor Information
Karen L. Lawson, University of Minnesota Center for Spirituality and Healing, United States.
Yvonne Jonk, University of Minnesota School of Public Health, United States.
Heidi O'Connor, University of Minnesota School of Public Health, United States.
Kirsten Sundgaard Riise, Medica Research Institute, United States.
David M. Eisenberg, Harvard School of Public Health, Boston, Massachusetts, and Samueli Institute, Alexandria, Virginia, United States.
Mary Jo Kreitzer, University of Minnesota Center for Spirituality and Healing, United States.
REFERENCES
- 1.Keehan SP, Cuckler GA, Sisko AM, et al. National health expenditure projections: modest annual growth until coverage expands and economic growth accelerates. Health Affairs. 2012;31(7):1600–12 [DOI] [PubMed] [Google Scholar]
- 2.Mattke S, Seid M, Ma S. Evidence for the effect of disease management: is $1 billion a year a good investment? Am J Manag Care. 2007;December;13(12):670–6 [PubMed] [Google Scholar]
- 3.Horrigan B, Lewis S, Abrams DI, Pechura C. Integrative medicine in America—how integrative medicine is being practiced in clinical centers across the united states. Global Adv Health Med. 2012;1(3):18–94 [Google Scholar]
- 4.Wolever RQ, Caldwell KL, Wakefield JP, et al. Integrative health coaching: an organizational case study. Explore (NY). 2011;7(1):30–6 [DOI] [PubMed] [Google Scholar]
- 5.Wolever RQ, Eisenberg DM. What is health coaching anyway? standards needed to enable rigorous research. Arch Intern Med. 2011;171(22):2017–8 [DOI] [PubMed] [Google Scholar]
- 6.Ellrodt G, Cook DJ, Lee J, Cho M, Hunt D, Weingarten S. Evidence-based disease management. JAMA. 1997;278(20):1687–92 [PubMed] [Google Scholar]
- 7.Weingarten SR, Henning JM, Badamgarav E, et al. Interventions used in disease management programmes for patients with chronic illness—which ones work? meta-analysis of published reports. BMJ. 2002;325(7370):925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood). 2013;32(2):207–14 [DOI] [PubMed] [Google Scholar]
- 9.Greene J, Hibbard JH. Why does patient activation matter? an examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012;27(5):520–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prochaska JO, Velicer WF. Behavior change: the transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48 [DOI] [PubMed] [Google Scholar]
- 11.Werch CE, Ames S, Moore MJ, Thombs D, Hart A. Health behavior insights: the transtheoretical/stages of change model: Carlo C. DiClemente, PhD. Health Promot Pract. 2009;10(1):41–8 [DOI] [PubMed] [Google Scholar]
- 12.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–64 [DOI] [PubMed] [Google Scholar]
- 13.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Behav. 1984;11(1):1–47 [DOI] [PubMed] [Google Scholar]
- 14.Miller WR, Rollnick S. Motivational interviewing: preparing people for change. 1st ed.New York: Guilford Press; 2002:428 [Google Scholar]
- 15.Biswas-Diener R. Personal coaching as a positive intervention. J Clin Psychol. 2009;65(5):544–53 [DOI] [PubMed] [Google Scholar]
- 16.Seligman ME, Steen TA, Park N, Peterson C. Positive psychology progress: empirical validation of interventions. Am Psychol. 2005;60(5):410–21 [DOI] [PubMed] [Google Scholar]
- 17.Wolever RQ, Dreusicke M, Fikkan J, et al. Integrative health coaching for patients with type 2 diabetes: a randomized clinical trial. Diabetes Educ. 2010;36(4):629–39 [DOI] [PubMed] [Google Scholar]
- 18.Edelman D, Oddone EZ, Liebowitz RS, et al. A multidimensional integrative medicine intervention to improve cardiovascular risk. J Gen Intern Med. 2006;21(7):728–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bovend'Eerdt TJ, Botell RE, Wade DT. Writing SMART rehabilitation goals and achieving goal attainment scaling: a practical guide. Clin Rehabil. 2009;23(4):352–61 [DOI] [PubMed] [Google Scholar]
- 20.Buntin MB, Jain AK, Mattke S, Lurie N. Who gets disease management? J Gen Intern Med. 2009;24(5):649–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blash L, Dower C, Chapman S. PeaceHealth's team fillingame uses patient activation measure to customize the medical home. UCSF Center for the Health Professions Research Abstracts; http://www.futurehealth.ucsf.edu/Content/11660/2011_05_PeaceHealth%27s_Team%20Fillingame_Uses_Patient_Activation_Measures_to_Customize_the_Medical_Home.pdf Accessed April 22, 2013. [Google Scholar]


