Abstract
The Heart-Healthy Lenoir Project is a multi-study project designed to reduce the risk burden of heart disease in Lenoir County, North Carolina. This case report examines one client's experience in this project and the impact of health coaching interventions that were used. The client presented with unhealthy lifestyle behaviors and a systolic blood pressure (BP) of more than 200 mmHg. After 1 year of educational group meetings and personalized health coaching, the client was able to reduce her BP to an acceptable range and has adopted many new lifestyle behaviors. This case report demonstrates one way health coaching is being integrated into educational programs and in collaboration with primary care practices.
Key Words: Integrative health coach, hypertension, blood pressure Heart-Healthy Lenoir, integrated, case report, weight loss
抽象
Heart-Healthy Lenoir 项目是 一个旨在减少北卡罗来纳州勒诺 县心脏病风险负担的多研究项 目。该病例报告剖析了该项目中 一名患者的经历和所用健康辅导 干预的影响。该患者的行为表现 出不健康的生活方式,其血压 (BP) 的收缩压高于 200 毫米汞 柱。在参加为期 1 年的集体教 导会议和针对个人的健康辅导之 后,该患者的血压降至可接受的 范围内,并且已经采纳了多种新 的生活方式。本病例报告示证了 健康辅导配合教导计划的一种方 式,而这种方式可为初级护理实 践提供协助。
SINOPSIS
Heart-Healthy Lenoir Project es un proyecto multiestudio diseñado para reducir la carga que supone el riesgo de cardiopatías en el condado de Lenoir, Carolina del Norte (EE. UU.). Este caso clínico examina la experiencia de una cliente de este proyecto y el impacto de las intervenciones de formación sanitaria empleadas. La cliente llevaba un estilo de vida insano y presentaba una presión arterial (PA) sistólica de más de 200 mmHg. Después de 1 año de reuniones con el grupo educativo y de formación sanitaria personalizada, la cliente fue capaz de reducir su PA hasta unos límites aceptables y ha adoptado muchas conductas de estilo de vida nuevas. Este caso clínico demuestra que la formación sanitaria unidireccional se está integrando en los programas educativos en colaboración con consultas de atención primaria.
BACKGROUND
This case discusses a client who is enrolled in the Heart-Healthy Lenoir Project in Lenoir County, North Carolina. The project is funded by a National Institutes of Health (NIH) grant involving community-based, participatory research–based interventions designed to reduce heart disease risk among residents of Lenoir County. The project is being led by researchers from the University of North Carolina at Chapel Hill and East Carolina University, Greenville, North Carolina, in partnership with several primary care practices and other groups in the community. This rural county, located in the coastal plains of North Carolina, is just one community among many that comprise the Stroke Belt of the Southeastern United States. Of the 100 counties in North Carolina, Lenoir County has one of the highest rates of heart disease and stroke-related deaths. Lenoir County is also one of the 40 most economically distressed counties in North Carolina.
The Heart-Healthy Lenoir Project consists of three independent studies. The Community-Based Lifestyle Intervention to Reduce Cardiovascular Disease Risk Study addresses healthy lifestyle issues and includes a weight-loss program. This study includes lifestyle interventions to improve nutrition, physical activity, and weight management with 350 Lenoir County residents. The Lifestyle Intervention Study uses group and individual education, counselling, and phone coaching. Collaboration among healthcare providers and community leaders is a focus of the study. This study has identified and published community resources available to the residents of Lenoir County that could enhance their opportunity for a healthy lifestyle.
The second study, The Practice-Based Enhanced Care Management for Hypertension, aims to improve blood pressure (BP) control by working with primary care providers regarding improved hypertension care through the use of tools to standardize care delivery and guided personal interventions with clients. The second focus of the hypertension study is a client-level intervention that includes pairing each client with a health coach who uses strategic techniques to assist clients in setting goals and increasing self-efficacy in disease management. The study seeks to promote home BP monitoring and improved medication adherence. This leg of the project encourages collaboration between the client being coached and his or her chosen primary care provider. The study enrolled 550 patients from six participating primary care providers.
Lastly, The Genetic Predispositions and Genomic Signatures Study explores the genetic factors associated with cardiovascular disease risk and treatment success.
Presenting Concerns
The client is a 56-year-old African American woman. She is a high school graduate, employed full-time by a home health agency, and divorced. No one under the age of 18 years lives in her home. She does not smoke and does not have diabetes. This client receives primary care at a local federally qualified health center and is uninsured. The client reports that prior to 2011, she was eating well and going to a gym at least 3 days each week. There was a noted reduction in her BP, and she was able to discontinue her antihypertensive medication. The client reports that she gradually stopped going to the gym and paid less attention to her diet, resulting in weight gain and an elevation in her BP. She did not resume the medication regimen for her BP and states that when she joined the project she “was in bad shape.”
CLINICAL FINDINGS
At the time of enrolment, the client's weight was 166.6 lbs, her BP was 208/110 mmHg, total cholesterol was 179, high-density lipoprotein (HDL) was 80, and her hemoglobin A1c (HbA1c) was 5.9%. The client did not have a regular exercise routine and had unhealthy dietary practices. She was not taking medication. The client did not present with any medical issues other than hypertension. Her family history is positive for cardiovascular disease. On the enrollment questionnaire, she rated her health as fair and noted no issues that would limit her ability to increase physical activity. She also reported that she is generally happy and possesses a high activation level toward making lifestyle changes.
DIAGNOSTIC FOCUS AND ASSESSMENT
An assessment and a battery of surveys to measure lifestyle behavior and health risk factors were completed at the time of enrollment. The client had serum laboratory tests for creatinine, estimated glomerular filtration rate, HbA1c, HDL-C, and total cholesterol values drawn at the regional hospital that were then processed by a biomedical laboratory. The project provided her with an Omron Model BP 785 electronic home BP monitor (Omron Corp, Kyoto, Japan). Information was recorded regarding weight, blood tests, and BP as part of the enrollment process. The client has returned every 6 months for new measurements and surveys. She is enrolled in the study for 2 years and completed her initial 12-month measurement in October 2012.
THERAPEUTIC FOCUS AND ASSESSMENT
The client attended four 2-hour group sessions that were designed to equip her with nutritional information and exercise ideas. The project's goals are to assist the client in improving her behavior related to diet and physical activity. An educational notebook was provided to the client with detailed nutritional data, physical activity ideas, and goal-setting tools. The second phase was an intensive 15-week weight-loss program that included five group educational sessions and 10 phone coaching sessions. There were weekly interventions with the five group sessions placed intermittently throughout the phone coaching schedule. Prior to each phone coaching session, the client received a “call sheet” that suggested a possible topic for discussion during the phone session and some handouts to jumpstart the client's thinking. The call sheet was used to prepare her for the call by asking what she would like to focus on, what her biggest worry was, what she still didn't understand, and/or what she was looking forward to. During the call, the client established the focus of the discussion. The phone coach then engaged the client regarding her chosen focus. Each session ended with the client setting a goal for the coming week. During each call, the phone coach collected data including the client's present weight, amount of time she was physically active during the week, number of servings of vegetables and fruits she consumed weekly, and her BP. Figures 1 through 4 show the results of this data collection.
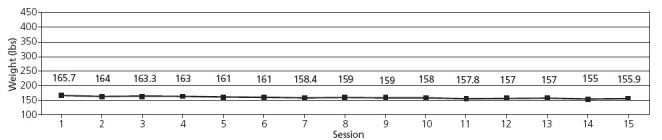
Figure 1 Client's weekly weight reports during the 15-week weight-loss program.
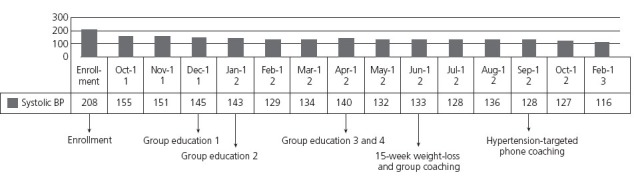
Figure 4 Client's monthly blood pressure (BP) report while in the project and stages of the intervention.
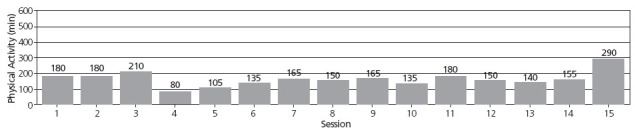
Figure 2 Client's weekly physical activity reports during the 15-week weight-loss program.
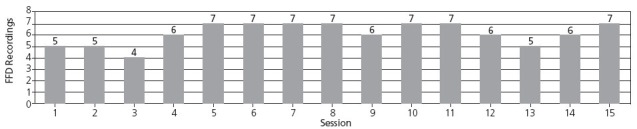
Figure 3 Number of days the client recorded data in a food and fitness diary (FFD) during the 15-week weight-loss program.
At the end of the 15-week intensive intervention, the client received a monthly hypertension-targeted coaching call. During the call, the coach reviewed the client's recent BP readings and medication adherence. The client had an opportunity to participate in active problem solving for any medication adherence issues. The phone coach also explored lifestyle interventions related to hypertension self-management that were previously identified by the client. At the end of each session, the client had an opportunity to set goals toward any area of concern that she chose to work on between coaching sessions. Additionally, the long-term goal, which the client chose during the first hypertension phone coaching call, was reviewed during each coaching call. The coaching calls averaged 20 minutes in both the weight loss and hypertension programs. After each phone coaching session, the phone coach sent the primary care provider a written summary of the session. The same phone coach was used for both the lifestyle and hypertension interventions with this client.
Within the first few months of starting the project, the client was prescribed by her primary care provider 20 mg lisinopril, one tablet daily, to treat her hypertension.
OUTCOMES
At the client's 6-month evaluation in October 2012, she had reduced her weight by 11 lbs (to 155.6 lbs) and had lower BP (112/71). Her total cholesterol was 205, HDL was 57, and HbA1c was 6.1%. Her self-reported weight during her last coaching session in March 2013 was 153.0 lbs, and her BP was 116/73. She reported taking lisinopril and vitamin B complex as directed, walking 10 000 steps daily, and continuing to lose weight at a rate of 1 lb per month. Her weight loss since enrollment totalled 13 lbs. Her BP greatly improved between the initial and final measurements. She continued to struggle with eating more than three servings of vegetables per day. This may explain the increase of her total cholesterol and HbA1c from her enrollment totals. Also of note is a decrease in the client's HDL.
FOLLOW-UP
The client will continue to work with the hyper-tension study health coach for 6 more months. The additional phone coaching will provide her with the opportunity to explore ways to address her cholesterol, which has remained high in spite of weight loss and exercise. The final stage of the weight-loss study, which is a weight-loss maintenance phone coaching program, also will be added to her regimen. It will be important for her to prepare a strategy to address her tendency to consume junk food when life gets busy. She will need to resist the impulse to stop taking her medication when her BP is under control. It is essential that the client remains mindful of her eating habits and the amount of exercise she is getting, which have been vital in her recent success. The maintenance coaching program will assist the client in addressing these barriers and high-risk situations and will increase her opportunity for continued success. Being in both lifestyle and hypertension studies, the client has access to a total of 2 years of coaching support. This brings with it a possibility of her tiring of the coaching process. The client had the same phone coach during her first year of coaching. However, in the new phase, she will be assigned a new coach for weight-loss maintenance, which could help to reduce the likelihood of her tiring of the coaching process. The client is not demonstrating signs of tiring of coaching at this time in the intervention but instead feels it is an important component to her success.
DISCUSSION
The client effectively used resources provided by Heart-Healthy Lenoir and continues with lifestyle changes, positively impacting her weight and BP. During the course of the project, the client moved to a new residence, which affected her healthier lifestyle choices, exercise routine, and weight loss. She also struggled with a forced change in her primary healthcare provider; her new physician has different requirements regarding renewal of her medications, such as monthly visits to the provider prior to granting refills. As a result of the frequency of visits and the cost of the monthly clinic visits, the client has had difficulty getting her medications refilled and was without her hypertension medication at times. Though this client was very successful when she went to a local gym on a regular basis several years ago, she can no longer afford the dues at the gym. An ongoing struggle continues to be the discovery of good exercise routines for aerobic workouts outside of the gym. She does wear a pedometer to measure the total steps taken daily and notes this has been a positive resource to keep her moving. Her limited financial resources are an issue with regard to healthy dietary options as well. However, during the course of the coaching process, she finds ways to purchase healthier foods. She continues to struggle with eating vegetables and needs regular encouragement and accountability to keep her vegetable intake higher. Her lack of moderate aerobic exercise contributes to slow weight loss. She reports a positive view of the project and phone coaching, which she says helped her to make her own changes in dietary choices and physical activity.
The strength of the health coaching component combined with the education provided to the client helped her realize fresh inspiration and understanding of lifestyle changes. In this case, the client felt the support provided by the phone coach was important to help her to adopt new behaviors that she felt were best for her. Health coaching provided the client with the process and support to personalize and actualize the information from the group meetings. The addition of the health coaching component recognizes that clients need help in motivating the emotional side of themselves to do what their rational side knows they need to do to be healthy. Knowledge alone can fall short of creating actual change due to the power of homeostasis within the clients and their environments. Health coaching is uniquely designed to assist in the slow process of change often experienced in clients' lives. It is hard to interpret the impact of phone coaching as a stand-alone intervention in this report due to its integration with the varied components of the project. The client seems to have responded well to the change from intensive health coaching once a week to a monthly intervention.
A takeaway message for health coaching from this report is the integration of health coaching into the different studies and interventions used. Health coaching enhanced the client's applications of the information and skills learned in the educational component of the project. Increased accountability provided via coaching encouraged the client's continued focus on the changes needed for better self-management in using the education from the project and her personal primary care provider. Regular use of goal-setting encouraged the client to move forward, and support from the coach helped the client to overcome barriers to her progress. Health coaching as a stand-alone intervention without the educational component could have had more limited outcomes, as the integration of coaching and education better supported her self-management goals. The group education component provided a solid foundation on which the health coach was able to build. Collaboration between the project and primary care practices created a beneficial team effort toward strengthening the client's self-management goals and struggles. Health coaching availed the provider with an in-home strategy toward adherence to optimal plans of care while personalizing the effort.
CLIENT PERSPECTIVE
The client said that when she started the project she was in “bad shape” and was desperate for a change in her life and health. She said that the project and health coaching resulted in her feeling cared about by the staff. The educational groups made her aware of the kinds of changes she needed to make. She learned a lot about nutrition and good lifestyle behaviors. She stated the health coaching and counseling “help me to use the tools I had been given in the program.” She also stated that the coaching helped her to become aware of her personal behaviors and how to change the behaviors that were working against her. Health coaching provided her with the support she needed to help herself. She stated the program was a “blessing” to her, “made a world of difference,” and gave her a sense someone was “walking beside me as I made these changes.”
This is the perfect place for a coach: not leading or following but walking beside his or her client as a partner on the journey to a better and healthier future.
Disclosures The author completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and disclosed that he is employed by the Heart-Health Lenoir Project and that his institution received a grant form the National Institutes of Health.


