Abstract
Obesity (and its related comorbidities) is one of the fastest-growing health concerns facing the United States and shows no sign of abating.1 The Centers for Disease Control and Prevention calculated that nearly 36% of American adults were obese in 2010 and estimates that this number will reach 44% by 2018.
The current standard of care for the management of patients with obesity in primary care is often a general recommendation by the physician to lose weight through improved nutrition and increased physical activity. Educational materials may be provided along with a referral to a dietician, nutritionist, or weight management program. Health coaching as an obesity intervention has yet to be fully integrated into primary care practice but has proven to be effective in corporate wellness and behavioral weight loss programs.2–5
Key Words: Obesity, case report, health coaching
INTRODUCTION
Obesity (and its related comorbidities) is one of the fastest-growing health concerns facing the United States and shows no sign of abating.1 The Centers for Disease Control and Prevention calculated that nearly 36% of American adults were obese in 2010 and estimates that this number will reach 44% by 2018.
The current standard of care for the management of patients with obesity in primary care is often a general recommendation by the physician to lose weight through improved nutrition and increased physical activity. Educational materials may be provided along with a referral to a dietician, nutritionist, or weight management program. Health coaching as an obesity intervention has yet to be fully integrated into primary care practice but has proven to be effective in corporate wellness and behavioral weight loss programs.2–5
The Ambulatory Practice of the Future (APF) at Massachusetts General Hospital (MGH), Boston, puts the patient at the center of a highly collaborative team focusing on wellness and prevention while providing acute and chronic care. A major component of the partnership is the engagement of the patient in setting personal wellness goals and the use of health coaches. Health coaches enable meaningful patient participation and create a context that allows the primary care team to understand wellness and disease from the patient's perspective.
THE CASE
A 34-year-old pediatrician who had been over-weight since the third grade and obese since high school was referred to health coaching for weight loss. He reached his maximum weight of 265 lbs (body mass index [BMI] 38) at the age of 29 years, during his residency. Despite his own efforts to lose weight by improving his diet and incorporating regular exercise, he often felt hopeless: “Even when I worked hard and lost 20 to 30 lbs, I would still feel fat, so I just stopped trying to diet.”As a new patient to APF, he was referred for health coaching.
On intake the patient's weight was 216 lbs with a calculated BMI of 31. His waist:hip ratio was .96 (107.5 cm waist and 114 cm hip). His blood pressure was 145/77 mmHg, and his resting heart rate was 77 beats per minute. He reported averaging 60 minutes per week of vigorous exercise and ate out often for convenience and for enjoyment on the weekends.
Methods
Over 12 months, the patient participated in 10 health coaching sessions, which included three office visits and seven phone-based (virtual) visits (Figure). Notably, the patient was out of touch with his coach for several weeks after his initial visit until he was reengaged through email. The health coaching approach at APF that is used with all patients is as follows:
Figure.
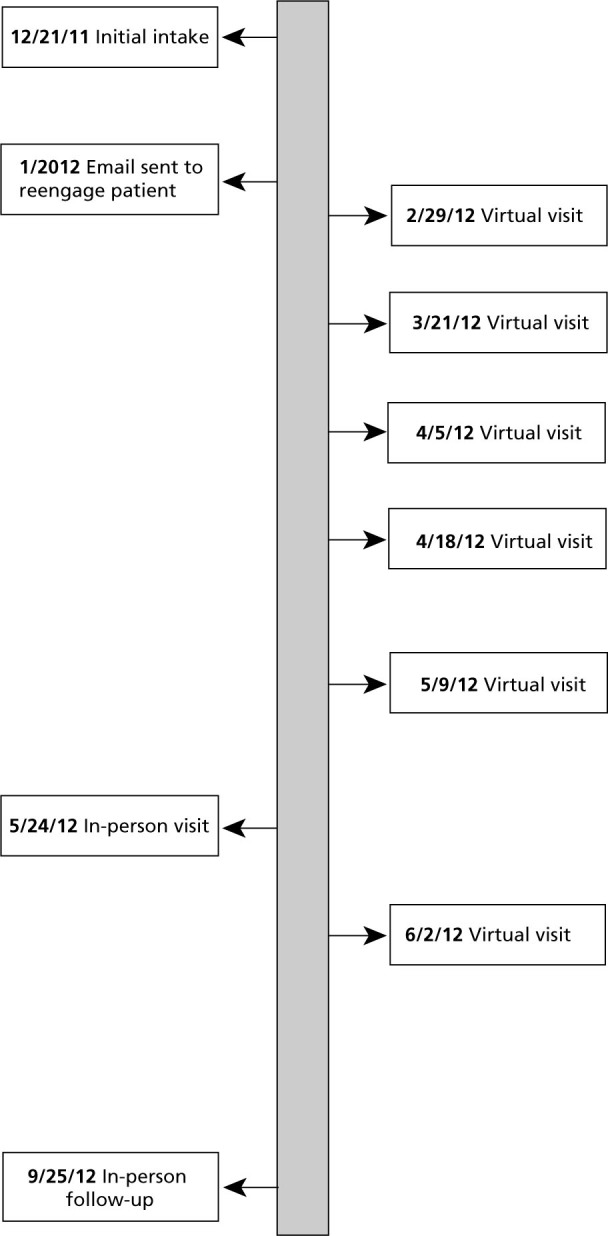
Timeline of in-person visits and virtual visits.
- Initial health coaching intake (60 min)
- – Further orientation of the health coaching approach is provided to the patient
- – A vision of where the patient would ideally like to see himself in a year is created
- – Three-month goals were made to start working toward this ideal vision
- – Two-week goals were made to start working toward the patient's 3-month goals
- Phone-based visits (15 min–30 min)
- – Review short-term goals and assess progress and challenges
- – Set new short-term goals
- – Virtual visits incorporate motivational interviewing, appreciative inquiry, self-efficacy, and problem-solving techniques to promote behavioral activation
- Follow-up office visits (45 min)
- – Three-month goals are reviewed
- – New 3-month goals are made based on progress and the patient's experience including reflection on adjusting initial goals and strategies to achieve success
Follow-up
After 9 months in the APF program, the patient weighed 166 lbs (23% total body weight loss) and had lowered his BMI to 24; his waist:hip ratio was .87 (84 cm waist and 96.5 cm hip)—an almost 10% reduction. The patient's blood pressure was 121/76 mmHg, and his resting heart rate was 58 beats per minute (Table).
Table.
Comparison of Baseline Data and Outcomes After 9 Months
| Intake | After 9 Mo of Coaching | |
|---|---|---|
| Weight | 216 lbs | 165 lbs |
| Body mass index | 31 | 24 |
| Waist circumference | 107.5 cm | 84 cm |
| Hip circumference | 114 cm | 96.5 cm |
| Hip:waist ratio | .96 | .87 |
| Blood pressure | 145/77 | 120/80 |
| Resting heart rate | 77 BPM | 58 BPM |
Abbreviation: BPM, beats per minute.
The patient reported an average of 210 minutes of moderate to vigorous exercise each week and noted significant improvements in his eating and exercise habits:
I think diet was more important in the first 6 months, but once I lost some weight I felt like my exercise tolerance improved a lot faster. About 6 months in, my weight loss started to flatten out, but then I increased my exercise by running and starting a regular weight training routine at the gym. At that point I was really feeling the payoff from the hard work, which made it easier to keep pushing forward. Having sessions with a coach helped me come up with ideas on how to reach my goals, and the follow-up sessions gave me pressure to stay on track.
Eighteen months after intake, the patient has maintained a weight of 165 lbs, and his vital signs were stable. He says,
I don't have to try to eat healthy now or worry about what the scale shows; healthy eating and exercise are just part of my routine, which makes weight maintenance much easier. I'm at a healthy weight for the first time in my life, and nearly every aspect of my life has improved. Achieving my weight loss goal was a great boost to my self-confidence, and that confidence has helped me at work and in my personal life.
DISCUSSION
Health coaching influenced how this pediatrician approaches both his own and his patients' wellness: “I used to provide education and guidelines to patients as a solution to their health problems and it never worked; telling patients they need to change isn't enough.”Although having longer visits to connect with patients isn't an option, he has made more frequent follow-up visits part of his practice:
I have been having my patients set short-term goals and have been following up with them a month later to help keep them motivated. Investing in a health coach to work with patients on weight loss helps to improve their health and reduce future costs. Promoting weight loss now is much more cost-effective than paying for diabetes care in the future.
This case illustrates the use of health coaching to support sustained weight loss. To further demonstrate the efficacy of health coaching as a sustainable weight loss intervention in a larger population, we have conducted a study with a sample size of 60 patients. The preliminary analyses show an average BMI reduction from 31 to 26 over 12 months. This result will be compared to a control group, and a cost and scalability analysis will be calculated. The APF program is a practice caring primarily for employees and their adult dependents insured via MGH.
We believe that health coaching will become increasingly integrated into primary care practice and offers the promise to provide effective tools for engaging patients in health outcomes across a broad range of chronic health issues. The challenge will to be to create increased awareness and understanding within primary care of the health coaching model and create reimbursement mechanisms that support this approach. Health coaching shows promise in lowering future healthcare costs and productivity loss for employers.6
Disclosures The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and none relevant to this article were disclosed.
Contributor Information
Ryan Sherman, The Ambulatory Practice of the Future, Massachusetts General Hospital, Boston, United States..
Ben Crocker, The Ambulatory Practice of the Future, Massachusetts General Hospital, Boston, United States..
Diana Dill, Working Together for Health, Belmont, Massachusetts, United States..
David Judge, The Ambulatory Practice of the Future, Massachusetts General Hospital, Boston, United States..
REFERENCES
- 1.Centers for Disease Control and Prevention Adult obesity facts. http://www.cdc.gov/obesity/data/adult.html Accessed May 24, 2013
- 2.Appel LJ, Clark JM, Yeh HC, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011November24;365(21):1959–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumanyika SK, Fassbender JE, Sarwer DB, et al. One-year results of the Think Health! study of weight management in primary care practices. Obesity (Silver Spring). 2012June;20(6):1249–57 [DOI] [PubMed] [Google Scholar]
- 4.Merrill RM, Aldana SG, Bowden DE. Employee weight management through health coaching. Eat Weight Disord. 2010;15(1-2):e52–9 [DOI] [PubMed] [Google Scholar]
- 5.Terry PE, Seaverson EL, Staufacker MJ, Tanaka A. The effectivness of a work-site telephone-based weight management program. Am J Health Promot. 2011;25(3):186–9 [DOI] [PubMed] [Google Scholar]
- 6.Herman P. Evaluating the economics of complementary and alternative medicine. Global Adv Health Med. 2013;2(2):56–63 [DOI] [PMC free article] [PubMed] [Google Scholar]


