Abstract
Background:
Women and adolescent girls bear a significant burden of the global HIV pandemic. Both behavioral and biomedical prevention approaches have been shown to be effective. In order to foster the most effective combination HIV-prevention approaches for women and girls, it is imperative to understand the unique biological, social, and structural considerations that increase vulnerability to acquiring HIV within this population.
Primary Study Objective:
The purpose of this article is to propose novel ideas for personalized biobehavioral HIV prevention for women and adolescent girls. The central argument is that we must transcend unilevel solutions for HIV prevention toward comprehensive, multilevel combination HIV prevention packages to actualize personalized biobehavioral HIV prevention. Our hope is to foster transnational dialogue among researchers, practitioners, educators, and policy makers toward the actualization of the proposed recommendations.
Methods:
We present a commentary organized to review biological, social, and structural factors that increase vulnerability to HIV acquisition among women and adolescent girls. The overview is followed by recommendations to curb HIV rates in the target population in a sustainable manner.
Results:
The physiology of the lower female reproductive system biologically increases HIV risk among women and girls. Social (eg, intimate partner violence) and structural (eg, gender inequality) factors exacerbate this risk by increasing the likelihood of viral exposure. Our recommendations for personalized biobehavioral HIV prevention are to (1) create innovative mechanisms for personalized HIV risk—reduction assessments; (2) develop mathematical models of local epidemics; (3) prepare personalized, evidence-based combination HIV risk—reduction packages; (4) structure gender equity into society; and (5) eliminate violence (both physical and structural) against women and girls.
Conclusions:
Generalized programs and interventions may not have universal, transnational, and crosscultural implications. Personalized biobehavioral strategies are needed to comprehensively address vulnerabilities at biological, social, and structural levels.
Key Words: Women's health, HIV, AIDS, prevention, adolescent
摘要
背景:女性和青春期少女承受着全球 HIV 大流行所带来的显著压力。行为预防方法和生物医学预防方法都已显露出其有效性。为了建立起对女性和少女来说最为有效的HIV 组合预防方法,当务之急是了解提高该人群 HIV 易感性的独特生物、社会和结构考量因素。
主要研究目标: 本文的目的是针对适用于女性和青春期少女的个性化生物行为 HIV 预防提出几种新颖的观点。核心论点即为,我们必须超越 HIV 预防的单层次解决方案,制定出一整套多层次组合的综合性 HIV 预防措施,从而实现个性化的生物行为 HIV 预防。我们希望能够在研究人员、执业医生、教育工作者和政策制定者之间建立起跨国对话关系,以便将所提出的建议付诸实施。
SINOPSIS
Antecedentes:
Sobre las mujeres y las adolescentes recae una carga significativa de la pandemia del VIH. Se ha demostrado que son efectivos tanto los enfoques preventivos conductuales como los biomédicos. Con el fin de promover la combinación más efectiva de enfoques para la prevención del VIH en las mujeres y las adolescentes, resulta obligado entender los factores únicos biológicos, sociales y estructurales que aumentan la vulnerabilidad para contraer el VIH en esta población.
Objetivo principal del estudio:
El objetivo de este artículo es proponer nuevas ideas para la prevención bioconductual personalizada del VIH en las mujeres y las adolescentes. El argumento central es que debemos ir más allá de las soluciones a un único nivel para la prevención del VIH y encaminarnos hacia paquetes combinados de prevención del VIH a múltiples niveles, a fin de actualizar la prevención bioconductual personalizada del VIH. Albergamos la esperanza de fomentar el diálogo transnacional entre investigadores, médicos, educadores y legisladores para llevar a cabo las recomendaciones propuestas.
Métodos:
Presentamos una explicación organizada para revisar los factores biológicos, sociales y estructurales que aumentan la vulnerabilidad para contraer el VIH entre las mujeres y las adolescentes. Esta visión general va seguida de recomendaciones para poner freno de manera sostenible a los índices de VIH en la población objeto.
Resultados:
La fisiología de la parte inferior del sistema reproductor femenino aumenta biológicamente el riesgo de contraer VIH en las mujeres y las adolescentes. Existen factores sociales (p. ej., la violencia de género) y estructurales (p. ej., las desigualdades de género) que exacerban ese riesgo al aumentar las probabilidades de exposición al virus. Nuestras recomendaciones para una prevención bioconductual personalizada del VIH son: (1) crear mecanismos innovadores para realizar evaluaciones personalizadas de la reducción del riesgo de contraer el VIH, (2) desarrollar modelos matemáticos de epidemias locales, (3) preparar paquetes personalizados combinados, basados en pruebas, para la reducción del riesgo de contraer VIH, (4) fomentar estructuras de igualdad de género en la sociedad y (5) eliminar la violencia (física y estructural) contra las mujeres y las adolescentes.
Conclusiones:
Puede ocurrir que los programas e intervenciones generalizados no tengan implicaciones universales, transnacionales y transculturales. Se necesitan estrategias bioconductuales personalizadas para abordar exhaustivamente las vulnerabilidades en los ámbitos biológico, social y estructural.
INTRODUCTION
A glimpse into the future of women's health and HIV: It is 2030. Although an HIV vaccine is only a few years away from being approved, several other biological and behavioral modalities are available for HIV prevention. Women and adolescent girls have access to web-based applications (apps), as well as online appointments with their healthcare providers, to assess and modify their HIV risk behaviors. Theory-informed behavioral interventions have dramatically increased consistent condom use and made strides in the reduction of concurrent sexual relationships. Targeted HIV prevention strategies (developed through sophisticated mathematical modeling) are offered in a personalized, a la carte fashion most suitable to individual risk profiles and preferences. As such, antiretroviral (ARV) treatment as prevention, preexposure prophylaxis (PrEP), microbicides, and male circumcision all have proven to be effective in curbing alarming HIV rates. Further, long-acting ARVs (via injection and oral suspension) were developed and have increased adherence to HIV treatment. Globally, violence against women has been reduced and gender equity has advanced through a combination of effective social gender norm interventions in addition to enforcement of strong legal sanctions. Partnerships also have been forged among nations—with women in positions of political power—to equalize access to needed therapeutics and behavioral intervention strategies and to promote the exchange of “best practice” strategies. This description may sound utopian; however, we argue that these approaches will be necessary to see a sustainable decrease in (and ultimate eradication of) HIV among women and adolescent girls.
In this article, we present a commentary organized to review biological, social, and structural factors that increase vulnerability to HIV acquisition among women and adolescent girls. We strategically chose an a priori focus in these three areas given current advances in HIV-prevention science. First, we provide an overview of HIV among women and adolescent girls. Second, we discuss biological, social, and structural factors that increase vulnerability to HIV infection among women and adolescent girls with a respective focus on health, safety, and equity. Based on this review, we conclude with novel recommendations to actualize personalized biobehavioral HIV prevention and decrease vulnerability to HIV acquisition.
Our article advances the science as we highlight and amalgamate multilevel HIV risk factors that historically have been examined in isolation and subsequently identify unique ways to address these factors simultaneously to achieve the greatest effect. The central argument is that we must transcend unilevel solutions for HIV prevention toward comprehensive, multilevel, combination HIV-prevention packages to realize personalized biobehavioral HIV prevention. Our hope is to foster transnational dialogue among researchers, practitioners, educators, and policymakers toward the actualization of the proposed recommendations.
WOMEN, ADOLESCENT GIRLS AND HIV PREVENTION
Women and adolescent girls bear a great burden of HIV globally as they comprise more than half of those infected with HIV.1 For women of reproductive age, HIV is the leading cause of death.2 Three million of the 4.8 million young people (aged 15-24 y) living with HIV worldwide at the end of 2011 were girls.3 Disease burden is not equally distributed as certain regions and countries are disproportionately affected. For example, in sub-Saharan Africa, almost 70% of all young people (15-24 y) living with HIV are females.3 In the United States as of 2010, 25% of all those living with HIV are women.4 Also in 2010, the rate of new HIV infections (per 100 000 population) among black women was 20 times higher than that of white women, and the rate among Hispanic/Latino women was four times the rate of white women.4 Half of new HIV infections among women in the United States are in those under age 35, and most HIV infections among women are due to heterosexual transmission.5
Despite these statistics, we have rounded a corner in the global HIV pandemic—we now have a variety of multilevel HIV prevention strategies that can reduce HIV acquisition for women and girls. In fact, there are more options available now than at any other point in the history of the epidemic, including condom use and other behavior-change strategies such as partner reduction or delay in sexual initiation, screening and treatment for other sexually transmitted infections (STIs), ARVs taken by those who are HIV-negative, and ARV treatment of people living with HIV as prevention for their partners.6
In the United States, several effective behavioral interventions have been identified by the US Centers for Disease Control and Prevention that target primary HIV prevention for women or girls. These interventions aim to empower women to practice safer sex by improving knowledge and beliefs and building skills to practice safer behaviors. Programs include Sister to Sister, which increases women's knowledge and improves skills such as condom negotiation and refusal skills through a brief one-on-one intervention and role-playing activities7; SiHLE, which emphasizes ethnic and gender pride for black adolescent girls and promotes abstinence, using condoms consistently, having fewer sex partners, and developing healthy relationships8; The Future is Ours, which helps women to understand and personalize their individual risk for HIV and acknowledges the role of intimate partner violence in vulnerability to HIV acquisition9; and Real AIDS Prevention Project, a community mobilization program in high-risk communities aimed at increasing condom use with peer street outreach, small group activities, and local media campaigns.10
Several interventions developed for international use also target similar goals and aim to integrate social and structural factors with HIV prevention. A few notable examples include Stepping Stones, a comprehensive program that offers discussions on a variety of sexual health issues including pregnancy, safer sex, and gender-based violence11; the Intervention with Microfinance for AIDS and Gender Equity (IMAGE) Study, which provides microfinancing solutions along with an HIV and gender training curriculum to women to help reduce gender-based violence and HIV risk behaviors12; and the Sonagachi Project, which was developed to empower sex workers to use health services and STI treatment to reduce HIV incidence and develop their own programs focused on better working conditions and human rights protections.13 Such evidenced-based programs are an integral component of developing comprehensive prevention interventions.
Lessons learned from these projects can be used to strengthen biomedical interventions—particularly given that adherence falls in the behavioral domain— and potentially enhance the efficacy of biological HIV prevention modalities. For example, we have made advances in preexposure prophylaxis (PrEP) as well as postexposure prophylaxis (PEP) medical regimens to reduce HIV risk. Oral ARV regimens have been available for PEP for those with known or possible exposure to HIV-infected fluids, such as an occupational exposure or sexual assault.14 This prevention modality requires exposure recognition and initiating treatment within 72 hours of exposure; adherence to the month-long treatment regimen, however, remains a challenge globally.14 PrEP could fill an important HIV-prevention gap in offering women another option, especially when successfully negotiating mutual monogamy or condom use are challenging or not viable options.15–17 The Centre for the AIDS Program of Research in South Africa (CAPRISA) study was the first trial to find that a 1% vaginal gel formulation of tenofovir was effective in the prevention of HIV acquisition in women; it reduced HIV acquisition by an estimated 39% overall when combined with other comprehensive HIV prevention strategies.15 Data from the Partners PrEP trial also showed that daily oral Truvada (Gilead Sciences, Inc, Foster City, California; emtricitabine/tenofovir disoproxil fumarate, a combination ARV drug already used in HIV treatment) is safe and effective in reducing risk of infection in women in sero-discordant couples when combined with other comprehensive HIV prevention strategies.18 As the relationship between adherence and efficacy is better understood with the completion of more trials,19 it will continue to be important to understand women's preferences related to PrEP use. For example, while some women prefer the lubricating properties of the microbicide gel, others prefer the oral tablet because it allows for discretion not offered by a microbicide gel.20 Moreover, barriers to PrEP adherence often reflect women's unique social conditions such as work schedules, other social responsibilities, and stigma from taking pills in the presence of family or peers.21
Findings initially presented at the International AIDS Conference in 2011 demonstrated the potential to reduce the HIV epidemic by more than 90% if all those infected with HIV were adherent to appropriate ARV treatment; the study was conducted under ideal conditions that also included regular behavioral counseling, provision of condoms, and STI testing and treatment.22 However, these estimates may be overly optimistic in real-world settings where a variety of factors can limit the impact of treatment as prevention, including lack of early testing when infectiousness is high, barriers in access to care, and difficulties with adherence.23 In addition, there are numerous issues that differentially affect women and girls that can accentuate dropout from the treatment cascade24 such as exposure to trauma, depression, pregnancy intention, and stigma.25–28 Therefore, an integration of prevention approaches, informed by an understanding of the gendered context of HIV risk, is needed in order to develop the most effective strategies for women and girls. Given systematic gender inequalities in many locations globally, implementing these strategies in a way that does not exacerbate HIV health disparities, particularly for women and girls, has become our current challenge.29
A MULTILEVEL MODEL OF HIV RISK FOR WOMEN AND ADOLESCENT GIRLS
The HIV epidemic among women and adolescent girls is not homogeneous but rather comprised of many microepidemics defined by multilevel circumstances that coalesce in a localized set of risk factors. In order to develop evidence-based, personalized risk reduction plans for women and adolescent girls, we need to identify the various layers of risk and how they interrelate. However, a challenge for HIV prevention for women and girls is that we often lack reliable data that is disaggre-gated by gender, which precludes our ability to disentangle these relationships. Thus, our potential to document the problems, evaluate interventions, and monitor sustained progress over time is limited—especially among marginalized women and girls. We propose a model for understanding three major contextual dimensions of risk for the target demographic—health (biological), safety (social), and equity (structural)—that also points to avenues for further intervention (Figure).
Figure.
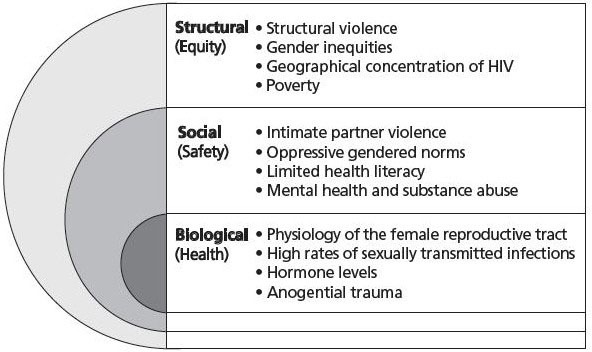
Proposed model to understand biological (health), social (safety), and structural (equity) contexts of HIV risk for women.
The Biological Context of Hiv Risk
In terms of health, there are several factors that increase biological vulnerability for women and adolescent girls. There are generally higher rates of transmission from male-to-female than female-to-male with the exception of uncircumcised males.30 Notably, heterosexual transmission accounts for the greatest number of new HIV infection in sub-Saharan Africa31 and 80% of new HIV infections among women in the United States.32 High rates of STIs among women and girls also make them more susceptible to acquiring HIV.30 STIs may contribute to breaches in the vaginal epithelium allowing HIV to cross this barrier more easily. STIs also may contribute to an increase in activated immune cells (such as CD4+ target cells) within the epithelium, making infection easier.33 In some cases, mucosal shedding associated with some STIs may generate this influx of activated CD4+ cells for months after healing, facilitating the transmission of HIV even after STI treatment.34
These biological risks are not, however, uniform across the lifespan. For example, the developing cervix of the adolescent girl, with greater area of ectopy, also uniquely increases her risk of acquiring HIV and other STIs.35 Women also are more vulnerable to acquiring HIV during pregnancy36; this may be due in part to shifts in levels of estradiol (E2) and progesterone (P4), which modulate the female reproductive tract's ability to protect against STIs while also allowing for pregnancy and fetal development.37 These shifts can induce both structural (increased ectopy) and immunological changes that can increase the risk of HIV acquisition.38
Women's vulnerability to HIV acquisition also may vary during different stages of menstruation. Levels of E2 and P4 correlate with the expression of CD4 and CCR5, a co-receptor necessary for the transmission of HIV,39 on uterine epithelial cells. High E2 levels during the proliferative phase of the menstrual cycle correlate with higher expression of CD4 and CCR5, which may lead to an increased susceptibility to HIV acquisition.40 CD4 and CCR5 expression is decreased during the secretory phase, lowering the risk of HIV acquisition.41 Menopause also may lead to heightened vulnerability for the acquisition of HIV. Structural changes (thinning of vaginal and cervical mucosa) and immunological changes contribute to this increased risk. Postmenopausal women have higher percentages of CCR5 receptors in their blood and cervical cells and thus may be at heightened risk.42
Additionally, lower levels of E2 may result in an inflammatory state with enhanced secretions of cytokines and chemokines that stimulate HIV-1 replication.43 As such, adolescence, stages of menstruation, pregnancy, and menopause are unique risk periods.37
Hormonal contraception also may increase risk for HIV acquisition among women and girls.44 However, according to the World Health Organization (WHO), current evidence is inconclusive and women should continue using hormonal contraceptives and consider adding condom use to reduce risk of HIV.45
Disruptions in the vaginal wall and subsequent inflammation from anogenital trauma during sexual intercourse, such as through forced or coerced sex with an HIV-infected male partner, also are risk factors for HIV acquisition.46,47 Many of these biological factors act synergistically. For example, adolescent girls who experience forced sex may be more vulnerable to HIV acquisition due to the developing cervix and also because adolescent girls experience higher rates of vaginal trauma after sexual violence compared to adult women.46 The impact of these biologic factors is magnified in the context of social and structural inequalities.
The Social Context of Hiv Risk
The complex social structure of HIV risk and transmission is also a gendered experience adding to vulnerability to the acquisition of HIV among women and girls. Oppressive gender norms, violence against women, limited health literacy, and altered partner negotiation abilities due to mental illness and/or substance abuse all differentially impact women and girls and increase risk for HIV acquisition. Further, this risk is inextricably entrenched in race/ethnicity48 and class oppression.49 Prevention interventions should account for this social context of HIV risk.
In terms of safety, 12% of HIV cases among women are due to intimate partner violence.50,51 Globally, 35% of all women have experienced physical and/or sexual violence by an intimate partner or a nonpartner; intimate partner violence is the most common form, affecting 30% of women around the world.52 Violence not only violates human rights; it can increase biological vulnerability to HIV, for example, through trauma to the vaginal wall during forced sex and increase exposure to STIs.53 Increased psychological distress following violence often leads to depression and substance use—known sexual risk factors.54,55 Compared to their non-abusive peers, abusive male partners are engaged in more HIV/STI risk behaviors and therefore expose their female partners to greater HIV/STI risk.56 Women with a history of abuse also are less likely to get tested for HIV.57 In terms of oppressive gender norms, gender power imbalances that favor males make it more difficult for women to negotiate safer sex and have been strongly linked to increased HIV risk through condom nonuse.50,58 For women interested in using microbicide gels, a partner's negative reaction may be an impediment to sustainable/consistent use.59,60
In certain regions of the world, girls are discouraged from learning about their reproductive and sexual health.61 Moreover, culturally embedded notions about femininity (eg, body objectification) may negatively affect sexual health.62 Even though women and adolescent girls are highly vulnerable to HIV infection, in some places they receive less information and know less than males about HIV/AIDS.63 In many societies, both the discussion of and education about sexual matters is frowned upon. Further, in settings where women and girls have limited access to education, their health literacy also is limited.64 Limited health literacy has been linked to women's stigmatizing attitudes toward individuals with HIV, which in turn may lessen women's use of HIV testing and treatment services.65 As a result, millions of people, especially girls and women, remain poorly informed about HIV/AIDS with potentially deadly consequences.
Mental illness and substance abuse also alter social/interpersonal interactions that shape the context of HIV risk among women and adolescent girls. Fear of abandonment by a sexual partner may lead to undesired, unsafe sexual practices,54 and the psychopathology of mental illnesses can skew the relationship between positive beliefs or intentions and subsequent behavior.66,67 Perceived mental health stigma also may contribute to increased rates of HIV/STI sexual risk behaviors.68 Mental health treatment therefore is arguably an important component of comprehensive HIV prevention programming.69 Although significant gains have been made in reducing HIV transmission within the injection drug—using community, women injection drug users (IDUs) still have disproportionately high rates of HIV transmission.70 Many women who use drugs lack the power to negotiate safer sex,71 often rely on partners to procure drugs,72 and are more likely than men to borrow or share injection equipment.73 Many female IDUs lack secure housing, engage in sex work, and report inconsistent condom use.74 In addition to the increased risk women face, female IDUs often face more stigma and have more barriers to accessing care, and few services are tailored to meet the needs of women.75 Services that aim to create a woman-friendly environment free of violence and stigma need to be implemented to better address the needs of this population. Work with men also will be required to achieve gender-transformative advances.76
Structural Factors and Hiv Risk
Structural factors range from laws and policies to the built environment. In essence, they construct the space in which people live, work, and function. Inequities in these macrolevel systems can increase women's vulnerability to HIV infection. Therefore, the promotion of equity in all arenas (eg, education, financial and political) is paramount.
Structural violence is the process by which embedded political and economic practices systematically cause harm or disadvantage to individuals.77 Historically entrenched gender-based inequalities, oppression, and physical violence are structural factors that hold back women and girls from attaining basic life necessities. These include: child marriage, limited access to education, limited control of productive resources, and increased burden of unpaid work.78 Female genital cutting, a common practice in Africa and the Middle East, is another prominent form of ensconced violence against women that affects more than 100 million women worldwide and significantly increases risk for HIV.79 Structural gender inequities often are the root cause for a variety of HIV risk factors such as having older partners, early age at first sexual experience, having a partner who has other partners, decreased negotiating power in a relationship, transactional sex, and sex work.80 Further, the deep-rooted sexual division of labor and power, wherein economic inequities favor men and disadvantage women, may also increase risk for HIV among women and adolescent girls.81 Additionally, cultural factors also may shape how structural oppression is enforced (eg, machismo among Latinos).82 As the culturally situated practice becomes structurally embedded and socially accepted in certain societies, biological risk for HIV also may be increased.
A substantial amount of literature shows that HIV may be concentrated in certain areas, whether it be neighborhoods, countries, or certain geosocial spaces. The emerging construct of community viral load83—a population-level marker of ART-mediated virologic suppression—may explain why rates of HIV are higher in certain demographic groups and regions than others. Further, incarceration, poverty, racism, and limited comprehensive sexual health education programs hamper current efforts.84–87 For example, due to inequitable compensation rates women may have less educational and financial ability to move around, and if they are constrained to an environment where HIV is highly concentrated (eg, a large number of individuals who are HIV positive and/or have high viral loads), they will be more likely to be exposed to HIV. Additionally, poverty not only directly affects where a woman lives and possibly her willingness to engage in transactional sex to support herself and/or her family, but it also may affect her sexual partner's risk factors. For example, wives and partners of migrant men or men who have to travel for work for long time periods away from home may be at heightened risk because of known risk behaviors among their partners (eg, high rates of unprotected sex with casual sexual partners).88–90 Sanctioned violence against women (eg, honor killings91) also may trap them in unhealthy relationships that they might otherwise leave.
RECOMMENDATIONS
Upon review of the relevant literature, our aim was to propose novel ideas for personalized biobehavioral HIV prevention for women and adolescent girls. Further, we hope to foster dialogue among researchers, practitioners, educators, and policymakers toward the actualization of the proposed recommendations. We argue that for effective HIV prevention for women and girls to advance, strategies, policies, and research must promote equity and safety along with biological and behavioral approaches and be informed by a gendered perspective. In recognition of the disproportionate impact of HIV on women and girls, advancing gender equity finally has become integrated as a major platform for several global AIDS organizations such as UNAIDS.29 We must continue to support these efforts in light of shifting priorities in HIV prevention. For example, while biological approaches to HIV prevention are effective and useful, initiation of and adherence to the therapies may be problematic for some groups of vulnerable women and girls if gender inequities remain firmly entrenched. Even with biomedical advances, if women and girls remain subject to oppressive social (eg, intimate partner violence) and structural (eg, poverty) forces that increase their risk for HIV, we may not see a reduction in HIV rates.
Our recommendations are five-fold (Table): (1) create innovative mechanisms for personalized HIV risk—reduction assessments; (2) develop mathematical models of local epidemics; (3) prepare personalized, evidence-based combination HIV risk reduction packages; (4) structure gender equity into society; and (5) eliminate violence (both physical and structural) against women and girls. Each is discussed in more detail below. We must transcend unilevel solutions for HIV prevention and move toward comprehensive, multilevel combination HIV-prevention packages to actualize personalized biobehavioral HIV prevention. Thus, we posit that the following recommendations should be worked on simultaneously and implemented together as a combined strategy.
Table.
Recommendations to Actualize Personalized Biobehavioral HIV Prevention and Decrease Vulnerability to HIV Acquisition
| Recommendations | Main Points |
|---|---|
| 1. Create innovative mechanisms for personalized HIV risk—reduction assessments. |
|
| 2. Develop mathematical models of local epidemics. |
|
| 3. Prepare personalized, evidence-based combination HIV risk reduction packages. |
|
| 4. Structure gender equity into society. |
|
| 5. Eliminate violence (both physical and structural) against women and girls. |
|
Create innovative mechanisms for personalized HiV risk—reduction assessments.
With advancements in mobile technology, we have the ability to connect individuals around the globe at the click of a button or the swipe of a finger. The initial assumption would be that people in resource-limited countries and settings would not have access to this advancement; however, research demonstrates that even people living in the most remote places in the world engage in digital spaces.92,93 HIV prevention science could benefit from the development of innovative mechanisms for personalized HIV risk—reduction assessments using all available technology and resources. This would include apps, telemedicine, and health navigators (people who could coach women and girls in reducing their risk). Further, multimedia approaches would provide a platform to ensure that gender-specific data were readily accessible to define the problem and evaluate solutions. To avoid the pitfalls of mobile health technologies, stringent monitoring and evaluation systems would need to be in place.93
We also must bear in mind that effective new health interventions tend to increase health disparities by increasing the health of wealthier groups more quickly than that of poor groups.94 We should be cognizant of this to ensure that resources flow to hard-to-reach and marginalized women and girls. It is also beneficial to culturally situate interventions to ensure that they are acceptable, available, and appropriate for women and girls in their local context. Using an array of technological and interpersonal strategies would enable the HIV community to more readily identify barriers to the enactment of safer sexual practices while assisting women and girls to modify their plans in real time to maintain their sexual health.
Develop mathematical models of local epidemics.
Mathematical models can be developed to determine the epidemiologic risk profile at the population level, which would have implications for the dissemination of strategies on the ground.95–97 Statistical advances allow for the use of modeling to predict risk and identify modifiable points of intervention. This can be used at the population level to identify the risk profile of a particular region. For example, if an area has a high rate of teen pregnancy, interventions and education may be needed to promote the safety of both adolescent girls and their sexual partners. These models can be used to determine the most effective biobehavioral prevention strategies for a particular geosocial space (eg, village or city). Additionally, the findings can be used to statistically demonstrate what the most effective combination of strategies will be for an individual. Rigorous analytic and assessment techniques will also need to be in place to evaluate the effects.
Prepare personalized, evidence-based combination HIV risk—reduction packages.
One of the things we have learned over the course of the HIV pandemic is that effective HIV prevention strategies, whether biological or behavioral, cannot be uniformly transferred from one person to the next. Personal preference, cultural nuances, and availability of resources are a few of the factors that influence an individual's choice of one prevention method over another. Preparation of personalized, evidence-based combination HIV risk—reduction packages could be a possible solution. In this manner, women and adolescent girls would be given the information and taught the skills they need to make informed choices and provided with an array of options to choose from to best meet their needs. This includes expanding access to and uptake of women-controlled prophylaxis, such as the female condom, which is a highly effective means of HIV prevention.98 Further, incorporation of technology would allow for the creation of a monitoring system to track progress and obtain feedback (eg, what they can implement and where they are challenged).
As noted by Kurth et al,96 getting a handle on the HIV pandemic will require the scaling up of optimal HIV-prevention packages that match the epidemiologic profile on the ground. We extend this idea to include personalizing the dissemination of such a program to meet the individual preferences of the women involved. For example, a woman living in a postconflict region may need access to PEP in the event that she is sexually assaulted. On the other hand, a woman who engages in survival sex to support her family may need microbicides or PrEP and condoms. Adding biomedical prevention strategies to the comprehensive prevention package for women may achieve the greatest results; they should be delivered, however, in an integrated prevention package that includes education, counseling, STI screenings, condom promotion, and side-effect monitoring.99 Adherence also should be emphasized, as it closely relates to level of protection.100 Even with promising biological prevention methods, the social and structural issues we have identified will still need to be addressed.
Structure gender equity into society.
By structuring gender equity into society, we can promote an atmosphere for women (including the most marginalized) to have their voices heard in policy arenas. When women are not “at the table,” their voices are absent from the discussions that will dictate the course of their lives. Programs should be developed to encourage and support girls from young ages to be voiced leaders and agents of change; program evaluation also will be key to determine effectiveness. A global agenda also should advance sexual and reproductive health literacy among women and girls. As a community, we need to promote gender and sexuality education—and the development of woman-controlled methods of HIV prevention. Additionally, gender-informed care should be provided along the entire continuum of prevention modalities.
This goal will require an evaluation of laws (eg, needle exchange programs), policies (eg, inequitable wages), and cultural norms (eg, misogyny) that prevent women and girls from reaching their full health potential. The process will not be immediate; however we can no longer afford to be bystanders on the sidelines. The time has come to address these issues head-on to ensure the health of future generations. As issues and concerns are not uniform among all women and girls, particular attention should be given to the intersectionality of factors such as race, class, religion, and geographic location.
Eliminate violence (both physical and structural) against women and girls.
A major step, which will present a major challenge, will be to eliminate physical and structural violence against women and girls. To initiate this process, interventions men are necessary. As noted earlier, heterosexual transmission accounts for the large majority of HIV infection among women and adolescent girls.5 We need to teach boys and men how to have healthy, intimate relationships with women and girls that do not involve sexual violence or coercion. Further, we need to promote condom use and monogamy to help reduce their risk of acquiring HIV, which would then limit exposure to HIV among women and girls. This requires a shift in cultural gender norms and factors that influence them (eg, media). We also need to examine the ways these challenges overlap with one another; for example, by addressing abuse as an underlying cause of biologic vulnerability or addressing girls' education as a way to foster their independent safer sex decision making.
CONCLUSIONS
Globally, it is important to address HIV-related disparities between regions and within countries, addressing economic, racial, and gender inequities. In essence, ground-level happenings need to be coupled with a population-level epidemiologic profile to achieve the greatest effect. Generalized programs and interventions, however, may not have universal trans-national and crosscultural implications. Personalized biobehavioral strategies are therefore needed to address vulnerabilities at biological, social, and structural levels to decrease disease burden among women and adolescent girls for optimal benefit. Women should be given a variety of options to choose from so they can find an HIV-prevention solution that best suits their needs and risk profile. Decisions also can be made regarding whether it is culturally and ethically appropriate to target areas with high HIV prevalence. Elicitation research should be conducted prior to implementation to determine the feasibility and acceptability of different methods in different areas. HIV risk—reduction plans need to be personalized, and women and girls should be encouraged to actively participate in political bodies in order to be at the table for related decision making. This will require a systematic approach to the implementation of existing and the development of new biobehavioral strategies.
Acknowledgments
This work was supported by the Penn Center for AIDS Research (NIH P30 AI 045008) and by the International Council on Women's Health Issues. The authors wish to acknowledge Maggie Ryan for her assistance with reviewing articles for this paper.
Disclosures The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported none.
REFERENCES
- 1.UNAIDS. [Accessed August 28, 2013];UNAIDS report on global AIDS epidemic2010. http://www.unaids.org/documents/20101123_globalreport_em.pdf
- 2.Ribeiro PS, Jacobsen KH, Mathers CD, Garcia-Moreno C. Priorities for women's health from the Global Burden of Disease study. Int J Gynaecol Obstet. 2008 Jul; 102(1): 82–90 [DOI] [PubMed] [Google Scholar]
- 3.UNICEF. [Accessed August 28, 2013];Adolescents and youth. HIV/AIDS: 2012. http://www.unicef.org/adolescence/index_VOY.html
- 4.US Centers for Disease Control and Prevention. [Accessed August 28, 2013];HIV among women 2013. http://www.cdc.gov/hiv/risk/gender/women/facts/index.html
- 5.US Centers for Disease Control and Prevention. [Accessed August 28, 2013];Estimated HIV incidence in the United States, 2007-2010. HIV surveillance supplemental report 2012. http://www.cdc.gov/hiv/topics/surveillance/resources/reports/#supplemental
- 6.Schwartländer B, Stover J, Hallett T, et al. Towards an improved investment approach for an effective response to HIV/AIDS. Lancet. 2011; 377(9782): 2031–41 [DOI] [PubMed] [Google Scholar]
- 7.Jemmott LS, Jemmott III JB, O'Leary A. Effects on sexual risk behavior and STD rate of brief HIV/STD prevention interventions for African American women in primary care settings. Am J Public Health. 2007; 97(6): 1034–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DiClemente RJ, Wingood GM, Harrington KF, et al. Efficacy of an HIV prevention intervention for African American adolescent girls: A randomized controlled trial. JAMA. 2004; 292(2): 171–9 [DOI] [PubMed] [Google Scholar]
- 9.Erhardt AA, Exner TM, Hoffman S, et al. A gender-specific HIV/STD risk reduction intervention for women in a health care setting: short- and long-term results of a randomized clinical trial. AIDS Care. 2002; 14(2): 147–61 [DOI] [PubMed] [Google Scholar]
- 10.Lauby JL, Smith PJ, Stark M, Person B, Adams J. A community-level prevention intervention for inner city women: results of the women and infants demonstration projects. Am J Public Health 2000; 90(2): 216–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jewkes R, Nduna M, Levin J, et al. Impact of stepping stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ. 2008August7; 337: a506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pronyk PM, Hargreaves JR, Kim JC, et al. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet. 2006; 368(9551): 1973–83 [DOI] [PubMed] [Google Scholar]
- 13.Gangopadhyay DN, Chanda M, Sarkar K, et al. Evaluation of sexually transmitted diseases/human immunodeficiency virus intervention programs for sex workers in Calcutta, India. Sex Transm Dis. 2005; 32(11): 680–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abrahams N, Jewkes R, Lombard C, Mathews S, Campbell J, Meel B. Impact of telephonic psycho-social support on adherence to post-exposure prophylaxis (PEP) after rape. AIDS Care. 2010; 22(10): 1173–81 [DOI] [PubMed] [Google Scholar]
- 15.Karim QA, Karim SS, Frohlich JA, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010; 329(5996): 1168–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Microbicide Trials Network. [Accessed August 28, 2013];MTN statement on decision to discontinue use of oral tenofovir tablets in VOICE, a major HIV prevention study in women 2011. http://www.mtnstopshiv.org/node/3619
- 17.Vissers DC, Voeten HA, Nagelkerke NJ, Habbema JD, de Vlas SJ. The impact of pre-exposure prophylaxis (PrEP) on HIV epidemics in Africa and India: a simulation study. PLoS One. 2008; 3(5): e2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012; 367(5): 399–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Celum C, Baeten JM. Tenofovir-based pre-exposure prophylaxis for HIV prevention: evolving evidence. Curr Opin Infect Dis. 2012; 25(1): 51–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Minnis AM, Gandham S, Richardson BA, et al. Adherence and acceptability in MTN 001: a randomized cross-over trial of daily oral and topical tenofovir for HIV prevention in women. AIDS Behav. 2013; 17(2): 737–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van der Elst EM, Mbogua J, Operario D, et al. High acceptability of HIV pre-exposure prophylaxis but challenges in adherence and use: qualitative insights from a phase I trial of intermittent and daily PrEP in at-risk populations in Kenya. AIDS Behav. 2013; 17(6): 2162–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011; 365(6): 493–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilson DP. HIV treatment as prevention: natural experiments highlight limits of antiretroviral treatment as HIV prevention. PLoS Med. 2012; 9(7): e1001231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011; 52(6): 793–800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Machtinger E, Wilson T, Haberer J, Weiss D. Psychological trauma and PTSD in HIV-positive women: a meta-analysis. AIDS Behav. 2012; 16(8): 2091–100 [DOI] [PubMed] [Google Scholar]
- 26.Machtinger E, Haberer J, Wilson T, Weiss D. Recent trauma is associated with antiretroviral failure and HIV transmission risk behavior among HIV-positive women and female-identified transgenders. AIDS Behav. 2012; 16(8): 2160–70 [DOI] [PubMed] [Google Scholar]
- 27.Finocchario-Kessler S, Dariotis JK, Sweat MD, et al. Do HIV-infected women want to discuss reproductive plans with providers, and are those conversations occurring? AIDS Patient Care STDs. 2010; 24(5): 317–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cook JA, Grey DD, Burke-Miller JK, et al. Illicit drug use, depression and their association with highly active antiretroviral therapy in HIV-positive women. Drug Alcohol Depend. 2007; 89(1): 74–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.UNAIDS. [Accessed August 28, 2013];Getting to zero 2011-2015 strategy: Joint United Nations Programme on HIV/AIDS (UNAIDS) 2010. http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2010/jc2034_unaids_strategy_en.pdf
- 30.National Institute of Allergy and Infectious Disease. [Accessed August 28, 2013];HIV infection in women. 2008. http://www.niaid.nih.gov/topics/hivaids/understanding/population%20specific%20information/pages/womenhiv.aspx
- 31.Case KK, Ghys PD, Gouws E, et al. Understanding the modes of transmission model of new HIV infection and its use in prevention planning. Bull World Health Org. http://www.who.int/bulletin/volumes/90/11/12-102574/en/index.html Accessed August 28, 2013 [DOI] [PMC free article] [PubMed]
- 32.USCenters for Disease Control and Prevention. [Accessed August 28, 2013];HIV/AIDS surveillance report. http://www.cdc.gov/hiv/topics/surveillance/resources/reports/
- 33.Kaushic C, Ferreira VH, Kafka JK, Nazli A. HIV infection in the female genital tract: discrete influence of the local mucosal microenvironment. Am J Reprod Immunol. 2010; 63(6): 566–75 [DOI] [PubMed] [Google Scholar]
- 34.Zhu J, Hladik F, Woodward A, et al. Persistence of HIV-1 receptor—positive cells after HSV-2 reactivation is a potential mechanism for increased HIV-1 acquisition. Nat Med. 2009; 15(8): 886–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Quinn TC, Overbaugh J. HIV/AIDS in women: an expanding epidemic. Science. 2005; 308(5728): 1582–3 [DOI] [PubMed] [Google Scholar]
- 36.Morrison CS, Wang J, Van Der Pol B, Padian N, Salata RA, Richardson BA. Pregnancy and the risk of HIV-1 acquisition among women in Uganda and Zimbabwe. AIDS. 2007; 21(8): 1027–34 [DOI] [PubMed] [Google Scholar]
- 37.Wira CR, Fahey JV, Sentman CL, Pioli PA, Shen L. Innate and adaptive immunity in female genital tract: cellular responses and interactions. Immunol Rev. 2005August; 206: 306–35 [DOI] [PubMed] [Google Scholar]
- 38.Gray RH, Li X, Kigozi G, et al. Increased risk of incident HIV during pregnancy in Rakai, Uganda: a prospective study. Lancet. 2005; 366(9492): 1182–8 [DOI] [PubMed] [Google Scholar]
- 39.Deng H, Liu R, Ellmeier W, et al. Identification of a major co-receptor for primary isolates of HIV-1. Nature. 1996; 381(6584): 661–6 [DOI] [PubMed] [Google Scholar]
- 40.Wira CR, Fahey JV. A new strategy to understand how HIV infects women: identification of a window of vulnerability during the menstrual cycle. AIDS. 2008; 22(15): 1909–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yeaman GR, Howell AL, Weldon S, et al. Human immunodeficiency virus receptor and coreceptor expression on human uterine epithelial cells: regulation of expression during the menstrual cycle and implications for human immunodeficiency virus infection. Immunology. 2003; 109(1): 137–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Meditz AL, Moreau KL, MaWhinney S, et al. CCR5 expression is elevated on endocervical CD4+ T-Cells in healthy postmenopausal women. J Acquir Immune Defic Syndr. 2012; 59(3): 221–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rollenhagen C, Asin S. Enhanced HIV-1 replication in ex vivo ectocervical tissues from post-menopausal women correlates with increased inflammatory responses. Mucosal Immunol. 2011; 4(6): 671–81 [DOI] [PubMed] [Google Scholar]
- 44.Heffron R, Donnell D, Rees H, et al. Use of hormonal contraceptives and risk of HIV-1 transmission: a prospective cohort study. Lancet Infect Dis. 2012; 12(1): 19–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.World Health Organization. [Accessed August 28, 2013];Hormonal contraception and HIV 2012. http://www.who.int/reproductivehealth/topics/family_planning/hc_hiv/en/
- 46.Klot JF, Auerbach JD, Berry MR. Sexual violence and HIV transmission: summary proceedings of a scientific research planning meeting. Am J Reprod Immunol. 2013 Feb; 69Suppl l: 5–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Draughon JE. Sexual assault injuries and increased risk of HIV transmission. Adv Emerg Nurs J. 2012; 34(1): 82–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wyatt GE, Gómez CA, Hamilton AB, Valencia-Garcia D, Gant LM, Graham CE. The intersection of gender and ethnicity in HIV risk, interventions, and prevention: new frontiers for psychology. Am Psychol. 2013; 68(4): 247. [DOI] [PubMed] [Google Scholar]
- 49.Amaro H, Raj A. On the margin: power and women's HIV risk reduction strategies. Sex Roles. 2000; 42(7/8): 723–49 [Google Scholar]
- 50.Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010; 376(9734): 41–8 [DOI] [PubMed] [Google Scholar]
- 51.Sareen J, Pagura J, Grant B. Is intimate partner violence associated with HIV infection among women in the United States? Gen Hosp Psychiatry. 2009; 31(3): 274. [DOI] [PubMed] [Google Scholar]
- 52.World Health Organization. [Accessed August 28, 2013];Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence 2013. http://apps.who.int/iris/bitstream/10665/85239/1/9789241564625_eng.pdf
- 53.Ghosh M, Rodriguez-Garcia M, Wira CR. Immunobiology of genital tract trauma: Endocrine regulation of HIV acquisition in women following sexual assault or genital tract mutilation. Am J Reprod Immunol. 2012; 69(S1): 51–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brawner BM, Gomes MM, Jemmott LS, Deatrick JA, Coleman CL. Clinical depression and HIV risk-related sexual behaviors among African-American adolescent females: unmasking the numbers. AIDS Care. 2012; 24(5): 618–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Teitelman A, Ratcliffe SJ, McDonald CC, Brawner BM, Sullivan CM. Relationships between physical and non-physical forms of intimate partner violence and depression among urban minority adolescent females. Child Adolesc Ment Health. 2011; 16(2): 92–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Decker MR, Seage G, Hemenway D, Gupta J, Raj A, Silverman JG. Intimate partner violence perpetration, standard and gendered STI/HIV risk behaviour, and STI/HIV diagnosis among a clinic-based sample of men. Sex Transm Infect. 2009; 85(7): 555–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Adams JL, Hansen NB, Fox AM, et al. Correlates of HIV testing among abused women in South Africa. Violence Against Women. 2011; 17(8): 1014–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Teitelman AM, Ratcliffe SJ, Morales-Aleman MM, Sullivan CM. Sexual relationship power, intimate partner violence, and condom use among minority urban girls. J Interpers Violence. 2008; 23(12): 1694–712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Domanska CA, Teitelman AM. Factors that affect acceptance of HIV microbicides among women. Collegian. 2012; 19(1): 23–32 [DOI] [PubMed] [Google Scholar]
- 60.Bentley ME, Fullem AM, Tolley EE, et al. Acceptability of a microbicide among women and their partners in a 4-country phase I trial. Am J Public Health. 2004; 94(7): 1159–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.DeJong J, Jawad R, Mortagy I, Shepard B. The sexual and reproductive health of young people in the Arab countries and Iran. Reprod Health Matters. 2005; 13(25): 49–59 [DOI] [PubMed] [Google Scholar]
- 62.Impett EA, Schooler D, Tolman DL. To be seen and not heard: femininity ideology and adolescent girls' sexual health. Arch Sex Behav. 2006; 35(2): 129–42 [DOI] [PubMed] [Google Scholar]
- 63.Li X, Lin C, Gao Z, et al. HIV/AIDS knowledge and the implications for health promotion programs among Chinese college students: geographic, gender and age differences. Health Promot Int. 2004; 19(3): 345–56 [DOI] [PubMed] [Google Scholar]
- 64.UNICEF. [Accessed August 28, 2013];The state of the world's children 2007: women and children, the double dividend of gender equality. http://www.unicef.org/sowc07/
- 65.Mugoya GC, Ernst K. Gender differences in HIV-related stigma in Kenya. AIDS Care. 2013June25[Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 66.Brawner BM, Davis ZM, Fannin EF, Alexander KA. Clinical depression and condom use attitudes and beliefs among African American adolescent females. J Assoc Nurses AIDS Care. 2012; 23(3): 184–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lundberg P, Johansson E, Okello E, Allebeck P, Thorson A. Sexual risk behaviours and sexual abuse in persons with severe mental illness in Uganda: a qualitative study. PloS One. 2012; 7(1): e29748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Elkington KS, Hackler D, Walsh TA, et al. Perceived mental illness stigma, intimate relationships, and sexual risk behavior in youth with mental illness. J Adolescent Res. 2013; 28(3): 378–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Surratt HL, Kurtz SP, Chen M, Mooss A. HIV risk among female sex workers in Miami: the impact of violent victimization and untreated mental illness. AIDS Care. 2012; 24(5): 553–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pinkham S, Malinowska-Sempruch K. Women, harm reduction and HIV. Reprod Health Matters. 2008; 16(31): 168–81 [DOI] [PubMed] [Google Scholar]
- 71.El-Bassel N, Terlikbaeva A, Pinkham S. HIV and women who use drugs: double neglect, double risk. Lancet. 2010; 376(9738): 312–4 [DOI] [PubMed] [Google Scholar]
- 72.Bryant J, Brener L, Hull P, Treloar C. Needle sharing in regular sexual relationships: an examination of serodiscordance, drug using practices, and the gendered character of injecting. Drug Alcohol Depend. 2010; 107(2): 182–7. [DOI] [PubMed] [Google Scholar]
- 73.Evans MJL, Hahn JA, Page-Shafer MK, et al. Gender differences in sexual and injection risk behavior among active young injection drug users in San Francisco (the UFO Study). J Urban Health. 2003; 80(1): 137–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cederbaum JA, Wenzel SL, Gilbert ML, Chereji E. The HIV risk reduction needs of homeless women in Los Angeles. Womens Health Issues. 2013; 23(3): e167–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lambdin BH, Bruce RD, Chang O, et al. Identifying programmatic gaps: inequities in harm reduction service utilization among male and female drug users in Dar es Salaam, Tanzania. PloS One. 2013; 8(6): e67062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dunkle KL, Jewkes R. Effective HIV prevention requires gender-transformative work with men. Sex Transm Infect. 2007; 83(3): 173–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Farmer P. On suffering and structural violence: a view from below. Daedalus. 1996; 125(1): 261–83 [Google Scholar]
- 78.Gupta GR. Plenary. Turning the tide: women and girls. International AIDS Society (AIDS, 2012); July2012; Washington, DC [Google Scholar]
- 79.Diouf K, Nour N. Female genital cutting and HIV transmission:iIs there an association? Am J Reprod Immunol. 2013; 69(S1): 45–50 [DOI] [PubMed] [Google Scholar]
- 80.UNAIDS. [Accessed August 28, 2013];Women, girls, gender equality and HIV. http://www.unaids.org/en/media/unaids/contentassets/documents/factsheet/2012/20120217_FS_WomenGirls_en.pdf
- 81.Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Educ Behav. 2000; 27(5): 539–65 [DOI] [PubMed] [Google Scholar]
- 82.Moreno CL. The relationship between culture, gender, structural factors, abuse, trauma, and HIV/AIDS for Latinas. Qual Health Res. 2007; 17(3): 340–52 [DOI] [PubMed] [Google Scholar]
- 83.Das M, Chu PL, Santos GM, Scheer S, et al. Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PLoS One. 2010; 5(6): e11068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Blankenship KA, West BS, Kershaw TS, Biradavolu MR. Power, community mobilization, and condom use practices among female sex workers in Andhra Pradesh, India. AIDS. 2008; 22: S109–16 [DOI] [PubMed] [Google Scholar]
- 85.Auerbach JD, Parkhurst JO, Cáceres CF. Addressing social drivers of HIV/AIDS for the long-term response: conceptual and methodological considerations.Global Public Health.2011:1–17. [DOI] [PubMed] [Google Scholar]
- 86.Adimora AA, Auerbach JD. Structural interventions for HIV prevention in the United States. J Acquir Immune Defic Syndr. 2010; 55(Suppl 2): S132–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bowleg L, Raj A. Shared communities, structural contexts, and HIV risk: Prioritizing the HIV risk and prevention needs of black heterosexual men. Am J Public Health. 2012; 102(Suppl 2): S173–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Morris M, Podhisita C, Wawer MJ, Handcock MS. Bridge populations in the spread of HIV/AIDS in Thailand. AIDS. 1996; 10(11): 1265. [DOI] [PubMed] [Google Scholar]
- 89.Lichtenstein B, Hook EW 3rd, Grimley DM, St Lawrence JS, Bachmann LH. HIV risk among long-haul truckers in the USA. Cult Health Sex. 2008; 10(1): 43–56 [DOI] [PubMed] [Google Scholar]
- 90.Haour-Knipe M, de Zalduondo B, Samuels F, Molesworth K, Sehgal S. HIV and “people on the move”: six strategies to reduce risk and vulnerability during the migration process. Intl Migration. 2013. doi:10.1111/imig.12063 [Google Scholar]
- 91.Elakkary S, Franke B, Shokri D, Hartwig S, Tsokos M, Püschel K. Honor crimes: review and proposed definition. Forensic Sci Med Pathol. 2013June15[Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 92.Pop-Eleches C, Thirumurthy H, Habyarimana J, et al. Mobile phone technologies improve adherence to antiretroviral treatment in resource-limited settings: a randomized controlled trial of text message reminders. AIDS. 2011; 25(6): 825–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kahn JG, Yang JS, Kahn JS. ‘Mobile’ health needs and opportunities in developing countries. Health Aff (Millwood). 2010; 29(2): 252–8 [DOI] [PubMed] [Google Scholar]
- 94.Victora CG, Vaughan JP, Barros FC, Silva AC, Tomasi E. Explaining trends in inequities: evidence from Brazilian child health studies. Lancet. 2000; 356(9235): 1093–8 [DOI] [PubMed] [Google Scholar]
- 95.Maticka-Tyndale E, Tenkorang EY. A multi-level model of condom use among male and female upper primary school students in Nyanza, Kenya. Soc Sci Med. 2010; 71(3): 616–25 [DOI] [PubMed] [Google Scholar]
- 96.Kurth AE, Celum C, Baeten JM, Vermund SH, Wasserheit JN. Combination HIV prevention: significance, challenges, and opportunities. Curr HIV/AIDS Rep. 2011; 8(1): 62–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lasry A, Zaric GS, Carter MW. Multi-level resource allocation for HIV prevention: A model for developing countries. Eur J Operational Res. 2007; 180(2): 786–99 [Google Scholar]
- 98.Forbes A. Recommendations from “Bringing Gender Home: Implementing Gender-Responsive HIV/AIDS Programming for U.S. Women and Girls.” Womens Health Issues. 2011; 21(6 Suppl): S227–36 [DOI] [PubMed] [Google Scholar]
- 99.Galindo GR, Walker J, Hazelton P, et al. Community member perspectives from transgender women and men who have sex with men on pre-exposure prophylaxis as an HIV prevention strategy: implications for implementation. Implement Sci. http://www.biomedcentral.com/content/pdf/1748-5908-7-116.pdf Accessed August 28, 2013 [DOI] [PMC free article] [PubMed]
- 100.US Centers for Disease Control and Prevention Interim guidance for clinicians considering the use of preexposure prophylaxis for the prevention of HIV infection in heterosexually active adults. Morbid Mortal Wkly Rep (MMWR). 2012; 61(31): 586–9 [PubMed] [Google Scholar]


