Abstract
Vaccination is a key deterrent to influenza and its related complications and outcomes, including hospitalization and death. Using 2006–09 data, we found a small improvement in vaccination rates among nursing home residents, particularly for blacks. Nonetheless, overall vaccination rates remained well below the 90 percent target for high-quality care, and black nursing home residents remained less likely to be vaccinated than whites. Blacks were less likely to be vaccinated than were whites in the same facility and were more likely to live in facilities with lower vaccination rates. Blacks were also more likely to be noted as refusing vaccination. Strategies are needed to ensure that facilities offer vaccination to all residents and to make vaccination more acceptable to black residents and their families.
Influenza can cause serious complications from existing medical conditions among the elderly, resulting in hospitalization and death.1–3 The average number of influenza-related hospitalizations was estimated to be 186,029 a year among people age sixty-five and older between the 1979–80 and 2000–01 flu seasons.1 Also, 90 percent of influenza-related respiratory and circulatory deaths occurred among the elderly between the 1976–77 and 1998–99 flu seasons.3 Influenza among the elderly results in considerable medical costs.4,5 The average annual cost for influenza-related hospitalizations among the elderly was estimated to be $372.3 million during the 1990–96 flu seasons.5
Nursing home residents are vulnerable to influenza and complications because they are frail and live in an environment where the flu virus can easily spread.6–8 The flu vaccination is the single most effective way to prevent influenza and related consequences—including hospitalization and death—among the elderly.2,9
Consistent with the Healthy People 2010 goal of achieving 90 percent flu vaccination rates among the elderly, the Centers for Medicare and Medicaid Services (CMS) set a goal of 90 percent flu vaccination rate in nursing homes. CMS also mandated that all Medicare- or Medicaid-certified nursing homes ensure the vaccination of their residents and report individual vaccination status beginning in 2005.10 In October 2006, CMS also started to require that facility vaccination rates be reported as a quality indicator on the Nursing Home Compare website.11
Nursing home vaccination rates, reported as recently as the 2005–06 flu season, are less than optimal.12,13 The nationwide average flu vaccination rate among nursing home residents was 72 percent during the 2005–06 flu season,12 well below the 90 percent vaccination rate goal.
Flu vaccination rates are particularly low for black nursing home residents, compared with their white counterparts.12,13 For example, using data from the 2004 National Nursing Home Survey, one study reported that the vaccination rate for black nursing home residents was 13 percent lower compared with the rate for white residents.13 According to immunization data from the 2005–06 Minimum Data Set, 65 percent of black residents received flu vaccinations compared with 73 percent of white residents.12 Improving flu vaccination rates in general and reducing racial inequality are both quality improvement goals that are yet to be achieved.
Although published studies have reported racial differences in flu vaccination rates among nursing home residents, few have explored the sources of these differences. Moreover, researchers have focused primarily on overall racial differences in flu vaccination rates among nursing homes without considering that black residents tend to aggregate in some facilities.
These studies consistently reveal differences in vaccination rates along racial lines, which may actually be attributable to differences in the quality of the facilities housing more blacks compared with those housing fewer blacks (that is, between-facility differences). Increasing evidence finds that elderly blacks tend to reside in facilities that have fewer staff members and more quality problems identified by inspections compared to the facilities where their white counterparts reside.14,15 These low-quality facilities may also have low vaccination rates for all of their residents, not only for blacks.
But between-facility differences are only one potential source of racial inequality in nursing home flu vaccination rates. The other, which has not been well studied, is within-facility differences, in which blacks and whites residing in the same nursing home do not receive the same level of care. These two sources of inequality may operate separately or in concert. Better understanding of the relative contribution of each is critical, because different quality improvement strategies are required to resolve them.
For example, educating all residents and their families of the need for and safety of flu vaccinations might be effective in improving overall vaccination rates. However, if existing racial differences are due to individual beliefs about flu vaccination (which leads to within-facility differences), and black residents are approached using the same message or educational style as used for white residents, racial disparities could even be exacerbated by an improvement in vaccination rates among whites but not blacks.
In this article we explore racial differences in flu vaccination rates among nursing home residents, and we untangle the contributions of racial differences between and within facilities. Using data from 2006 to 2009, we examine the sources of racial differences in flu vaccination rates and whether these have changed. We focus on vaccination rates among long-stay nursing home residents (defined as those who stay in nursing homes for at least ninety days), because nursing homes can presumably be held accountable for their receiving the flu vaccine.
This article builds upon the existing literature in two notable ways. First, to the best of our knowledge, this is the first nationwide study to use multiple years of flu vaccination data. Second, our analysis used more recent data (for the 2006–09 flu seasons), allowing us to examine the most recent practice patterns in nursing homes.
Study Data And Methods
DATA AND POPULATION
We used the 2006–09 national Minimum Data Set, as well as data from the 2007–08 Online Survey Certification and Reporting system, to examine racial differences in the receipt of flu vaccinations among long-stay (ninety days or longer) nursing home residents during the 2006–07, 2007–08, and 2008–09 flu seasons. The Minimum Data Set is a federally mandated assessment tool completed upon admission, and regularly thereafter, for all residents of Medicare- or Medicaid-certified nursing home facilities. It captures sociodemographic characteristics of residents and information about their health and physical functioning.
In 2005 CMS modified the Minimum Data Set by including items to document residents’ vaccination status, as well as reasons for not having been vaccinated. Six possible reasons for not receiving flu vaccinations are stipulated: not residing in the facility during that year’s flu season; vaccinated outside of the facility; not eligible for vaccination; vaccination offered and declined; vaccination not offered; and unable to obtain the vaccine. Only one of these reasons can be checked.
The Online Survey Certification and Reporting data summarize facility characteristics, such as hospital affiliation status, based on annual survey inspections conducted by state regulatory authorities. We matched each study subject’s Minimum Data Set to the Online Survey Certification and Reporting data for the facility of residence during the relevant study period.
We excluded hospital-based nursing homes from the study because they predominantly serve postacute patients who are generally in residence for ninety days or less following hospitalization. We excluded people identified as Hispanic because our primary focus was on examining the source of racial—not ethnic—inequality in the receipt of flu vaccinations. Hispanics accounted for only a small proportion of nursing home residents (about 3–4 percent), and only 23 percent of the nursing homes examined had more than one Hispanic resident eligible.16 Residents who were identified as Asians and Pacific Islanders were also excluded, because their numbers were even smaller.
We further restricted our sample to people age sixty-five or older, who had been present in the nursing home for at least ninety days prior to the start of each flu season considered, and who had a follow-up Minimum Data Set assessment or discharge record from the same facility between October 1 and June 30 of the next year. According to the Minimum Data Set user manual, the influenza vaccination status for each year’s flu season would be indicated as part of any type of assessment between October 1 and June 30 the following year.17
DEFINING VACCINATION STATUS
A resident was considered to have received a flu vaccination during a given flu season if his or her last available Minimum Data Set record during the follow-up period (October 1–June 30) indicated receipt of a flu vaccination.
RESIDENTS’ RACE AND OTHER CHARACTERISTICS
Each resident’s race was identified as non-Hispanic black or white, based on the Minimum Data Set.We also identified residents’ basic demographic characteristics, such as sex and age, using the Minimum Data Set, and we adjusted for these characteristics in the regression model. We did not adjust for additional individual characteristics because the Centers for Disease Control and Prevention recommends that all nursing home residents be vaccinated against the flu except those who have severe allergic reactions or complications related to the vaccine.18
ANALYTICAL APPROACH
We examined the flu vaccination rates and the reasons for not being vaccinated during each of the three flu seasons studied. To examine how much of the racial inequality in flu vaccination rates is attributable to differences within facilities versus between facilities, we estimated two different types of models (base logit and conditional fixed-effects logit). The estimates represent the overall racial differences and racial differences within facilities, respectively. We used the difference in the estimates from these two models to test the differences between facilities.19
Because racial differences might vary with the racial mix in the facility, we stratified facilities—with both white and black residents—into quintiles, according to the proportion of black residents in the facility.20 The stratification was based on the nationwide distribution of the proportion of blacks in facilities for each year. Quintile 1 had the lowest proportion of black residents, and quintile 5 had the highest proportion of blacks.
Finally, to test the robustness of the findings and to tease out the racial differences caused by acceptable reasons for not being vaccinated, we excluded the residents recorded as “offered [vaccination] and declined” or “received [vaccination] out of the facility” and repeated our analyses.
LIMITATIONS
Some limitations of the data should be noted. First, the information about vaccination status relies on the Minimum Data Set. Our analysis, therefore, is limited to Medicare- and Medicaid-certified nursing homes. These nursing homes are subject to the CMS mandates to ensure vaccination and to report vaccination rates for the Nursing Home Compare database. Second, although the Minimum Data Set is generally considered to be reliable and valid, the quality of data varies across nursing homes.21,22 However, differences in measures of residents’ status and treatment are less likely to vary within facilities. Furthermore, because CMS publishes the nursing home vaccination rate as a quality indicator, there is no incentive for nursing homes to underreport vaccinations.
Study Results
Exhibit 1 summarizes the flu vaccination rates for the 2006–07, 2007–08, and 2008–09 seasons, overall and by race. These are reported for all nursing homes and for subsets of nursing homes, based on the proportions of black residents in the facility. The analytical samples included approximately 850,000 residents per year residing in more than 14,000 freestanding (nonhospital-based) facilities. About 38–39 percent of the nursing homes did not have any eligible black residents each year. After facilities housing both black and white residents were stratified into quintiles based on the proportion of blacks, the facilities in quintile 1 averaged 1.5 percent black residents and quintile 5 averaged 52.0 percent black residents.
Exhibit 1.
Influenza Vaccination Rates For Black And White Nursing Home Residents, By Proportion Of Blacks In The Facility Over Three Flu Seasons, 2006–09
| 2006–07 flu season (N = 886,786 residents; 14,301 facilities) |
2007–08 flu season (N = 872,592 residents; 14,367 facilities) |
2008–09 flu season (N = 857,740 residents; 14,332 facilities) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall (%) | White (%) | Black (%) | Overall (%) | White (%) | Black (%) | Overall (%) | White (%) | Black (%) | |
| All nursing homes | 81.73 | 82.62 | 75.42 | 82.54 | 83.29 | 77.27 | 82.75 | 83.46 | 77.75 |
| No blacks | 84.89 | 84.89 | — a | 85.08 | 85.08 | — a | 84.97 | 84.97 | — a |
| Quintile 1 | 82.93 | 83.02 | 78.73 | 83.76 | 83.82 | 80.64 | 84.03 | 84.10 | 80.97 |
| Quintile 2 | 82.16 | 82.26 | 80.01 | 82.68 | 82.78 | 80.85 | 82.99 | 83.15 | 79.71 |
| Quintile 3 | 80.80 | 81.08 | 78.12 | 81.83 | 82.13 | 79.03 | 82.17 | 82.52 | 79.10 |
| Quintile 4 | 79.55 | 80.07 | 75.55 | 80.43 | 81.09 | 77.89 | 81.01 | 81.62 | 78.75 |
| Quintile 5 | 75.87 | 78.12 | 73.94 | 78.01 | 79.93 | 76.39 | 78.34 | 80.07 | 76.94 |
| No whites | 63.15 | — a | 63.15 | 73.47 | — a | 73.47 | 71.54 | — a | 71.54 |
source Authors’ analysis of data on nursing home residents from the national Minimum Data Set (2006–09). notes Over the three years, nursing homes with no blacks account for 38–39 percent of all the facilities; nursing homes with no whites account for 0.3–0.4 percent of all the facilities. The stratification by quintiles was based on facilities with both whites and blacks. Quintile 1 represents the lowest proportion of blacks; quintile 5, the highest. Each subgroup accounts for approximately 12 percent of all facilities.
Not applicable.
FLU VACCINATION RATE TRENDS
As shown in Exhibit 1 (the “all nursing home” row), overall flu vaccination rates among long-stay nursing home residents increased gradually over the three flu seasons: from 81.7 percent in the 2006–07 flu season to 82.8 percent in the 2008–09 flu season. The increase in the vaccination rate was proportionately greater for blacks than for whites. Over the three flu seasons studied, vaccination rates increased less than one percentage point (from 82.6 percent to 83.5 percent) for all whites, but by more than two percentage points (from 75.4 percent to 77.8 percent) for all blacks. All of the above changes were statistically significant.
Exhibit 1 also presents vaccination rates across the subgroups of nursing homes. The average vaccination rate was lower in the subgroup of nursing homes with a higher proportion of blacks compared with that in the subgroup of facilities with a lower proportion of blacks and was lowest in the small number of facilities housing only black residents. Over the three flu seasons, improvements in vaccination rates were particularly notable in the subgroup of facilities with high proportions of blacks. For example, although there was almost no change in vaccination rates in facilities with whites only and a 1.1-percentage-point increase in facilities with a very low proportion of blacks (quintile 1), there was a 2.5-percentage-point increase in vaccination rates among facilities with a very high proportion of blacks (quintile 5) and an 8.4-percentage-point increase in facilities housing only black residents (all changes statistically significant). Nonetheless, racial differences persisted into the most recent year of data examined.
PATTERNS OF RACIAL DIFFERENCES
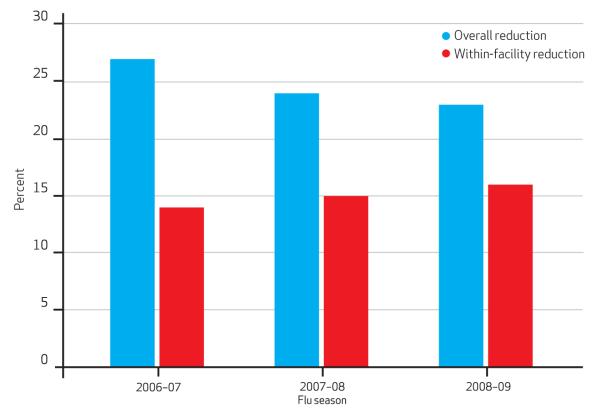
We examined the sources of racial differences in vaccination rates. Exhibit 2 reveals how much less likely blacks were to be vaccinated overall and within a given facility than their white counterparts, adjusting for age and sex. We found blacks were less likely to be vaccinated than whites overall, as well as within the same facility. Over the three flu seasons, the odds of being vaccinated were 14–16 percent lower for blacks than for whites within the same facility (statistically significant).
Exhibit 2. Likelihood Of Receiving Flu Vaccination Among Black Nursing Home Residents Compared To White Residents, 2006–09.
source Authors’ analysis of data on nursing home residents from the national Minimum Data Set (2006–09). notes The percentage indicates the percentage reduction in the odds of receiving vaccination for black residents versus white residents, accounting for the effects of age and sex. All of these numbers are statistically significant (p < 0.01). The overall reductions are statistically significant from the reductions within a facility for each of the three flu seasons (p < 0.01). The sample for each flu season includes only facilities with both eligible black and white residents: 608,296 residents and 8,659 facilities for the 2006–07 flu season; 601,968 residents and 8,767 facilities for the 2007–08 flu season; and 597,063 residents and 8,796 facilities for the 2008–09–flu season. The original odds ratio and confidence intervals related to this exhibit are available in Appendix Table 3. See Note 23 in text.
This within-facility difference persisted (although its magnitude was reduced) even after excluding residents who were either offered but declined vaccination, or were vaccinated outside the facility (see Appendix Table 1).23 We repeated our analyses separately within quintiles of nursing homes and found that differences between vaccination rates for blacks and whites in the same facility were consistently present over the three flu seasons (see Appendix Table 2).23
We also found that variations in vaccination rates between facilities accounted for a large part of the overall racial differences we observed in each of the three flu seasons; that is, racial differences within facilities were statistically significantly smaller than the overall racial differences. For example, as shown in Exhibit 2, in the 2008–09 flu season, the overall odds of being vaccinated were 23 percent lower for blacks than for whites. However, within facilities, the overall odds were 16 percent lower for blacks, a statistically significant decrease.
REASONS FOR NOT RECEIVING FLU VACCINES
The reasons that residents did not receive a flu vaccination were recorded in the Minimum Data Set (Exhibit 3). The most commonly recorded reasons for not being vaccinated were “offered and declined,” followed by “not offered.” Blacks were more likely than whites to have one of these two reasons recorded. Furthermore, blacks were somewhat more likely to have no reason recorded.
Exhibit 3.
Reported Reasons Why Nursing Home Residents Did Not Receive Flu Vaccines, 2006–09
| 2006–07 flu season |
2007–08 flu season |
2008–09 flu season |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Reason reported | Overall (%) |
White (%) |
Black (%) |
Overall (%) |
White (%) |
Black (%) |
Overall (%) |
White (%) |
Black (%) |
| None, resident reported as vaccinated | 81.73 | 82.62 | 75.42 | 82.54 | 83.29 | 77.27 | 82.75 | 83.46 | 77.75 |
| None, although resident not reported as vaccinated |
0.89 | 0.83 | 1.35 | 0.83 | 0.78 | 1.18 | 0.77 | 0.71 | 1.17 |
| Not in facility during this year’s flu season |
0.25 | 0.25 | 0.24 | 0.22 | 0.22 | 0.21 | 0.24 | 0.25 | 0.19 |
| Received outside of this facility | 1.15 | 1.17 | 0.98 | 1.49 | 1.52 | 1.21 | 1.79 | 1.83 | 1.50 |
| Not eligible | 1.02 | 1.04 | 0.84 | 1.01 | 1.05 | 0.71 | 0.99 | 1.03 | 0.73 |
| Offered and declined | 8.55 | 8.05 | 12.16 | 8.69 | 8.18 | 12.31 | 8.93 | 8.37 | 12.88 |
| Not offered | 5.25 | 4.90 | 7.70 | 4.56 | 4.29 | 6.44 | 3.96 | 3.77 | 5.28 |
| Unable to obtain vaccine | 1.16 | 1.14 | 1.32 | 0.66 | 0.66 | 0.66 | 0.57 | 0.58 | 0.52 |
source Authors’ analysis of data on nursing home residents from the national Minimum Data Set (2006–09). note Sample sizes are available in Exhibit 1.
The distribution of some of the reasons changed over time. For example, there was little change between flu seasons in the proportion of blacks or whites noted as having been offered but refusing vaccination. However, the proportion of blacks whose recorded reason for not being vaccinated was “not offered” decreased by a statistically significant 2.4 percentage points over the three flu seasons.
Discussion
Vaccination against the flu is the most effective way to prevent influenza and related consequences, including hospitalization and death, among the elderly.2 Although we observed an encouraging improvement in the rate of flu vaccinations in freestanding nursing homes over the 2006–07 to 2008–09 flu seasons, particularly in facilities with high proportions of black residents, a statistically significant racial difference remains. Consistent with previous studies,12,13,24 we found that black nursing home res idents are less likely to receive flu vaccinations than are white residents.
Our findings extend previous work by revealing that the facility-level vaccination rate in a nursing home tends to decrease as the proportion of black residents increases. Moreover, we found that even within a given nursing home with residents of both races, blacks are less likely than whites to receive flu vaccinations.
REDUCING RACIAL DIFFERENCES WITHIN FACILITIES
Our findings indicate that the observed racial difference in flu vaccination rates is partially attributable to racial differences within facilities. That is, blacks are less likely to be vaccinated than whites—even though they reside in the same facility and, therefore, should be treated the same way using available resources. This finding seems to conflict with some studies that found no racial difference within a nursing home in other quality measures such as prevalence of pressure sores and use of physical restraints.25,26
As a quality measure, flu vaccination may be unique. It is a reflection of preventive care and is administrated once a year, while the other quality measures (such as prevalence of pressure sores) typically involve daily care. Unlike the receipt of daily care, which is expected by nursing home residents (such as maintaining physical functional status), the decision to accept the flu vaccination could be affected by personal beliefs and attitudes toward flu vaccinations.27,28 Indeed, our data suggest that blacks are consistently more likely than whites to refuse flu vaccinations when offered.
Although individual preference should be respected, it should be understood that individuals’ perspectives may be influenced by knowledge regarding safety and effectiveness of the flu vaccination.27,29,30 Knowledge and beliefs about flu vaccines can be modified with education and increased trust in health care staff. Provider-patient communication can affect a person’s beliefs and attitude regarding flu vaccination.31 It also has been suggested that poor communication between care providers and black patients might be responsible for their refusing the flu vaccination at higher rates than occurs with white patients.27,32 Improving communication between nursing home staff and residents might help improve black residents’ knowledge about flu vaccines as well as their trust of facility staff—enough to accept the flu vaccination.
The difference in individual preferences may be an important explanation as to why some people don’t want to be vaccinated. Yet other reasons may also help explain the observed racial difference in vaccination rates within facilities. For example, facilities are somewhat more likely to indicate that blacks were “not offered” flu vaccinations than they are for whites. Even after we excluded residents who were offered but declined the flu vaccinations, we still observed racial differences in vaccination rates within a facility.
Unfortunately, we lack information about why blacks are less likely to be offered flu vaccinations compared with whites. Unconscious provider bias has been suggested as one of the potential explanations for the racial differences in flu vaccination rates.32 This bias might help account for the racial differences within facilities.
To completely eliminate racial differences in flu vaccination rates, educational programs that focus on elderly blacks and their families may be necessary. Appropriate incentives may also be important in motivating nursing homes to provide such educational programs.
If facilities were rewarded based on the absence of racial disparities, in addition to overall provider quality, facility management and clinical staff would have a strong incentive to optimize process quality indicators like vaccination rates by universally vaccinating all patients. However, the focus on measuring disparities should not be a barrier to admitting blacks to high-quality facilities that might not typically have black residents.
We also found that the racial differences seen in vaccination rates were attributable to the facilities in which residents live. This suggests that certain resource-poor facilities find it difficult to implement relatively straightforward interventions such as vaccinating all residents.15
REDUCING RACIAL DIFFERENCES BETWEEN FACILITIES
Our findings clearly indicate that site of care (where a resident receives care) strongly influences the likelihood of receiving the flu vaccine. Nursing homes with high proportions of black residents have lower vaccination rates—for both blacks and whites—than do facilities with lower proportions of black residents. The substantial differences between facilities persist even after residents who were noted as having been offered but declined vaccination are excluded.
One approach that might reduce differences between facilities would be to target nursing homes serving a high proportion of blacks, introducing suitable interventions designed to overcome any operational barriers to implementing facilitywide vaccination. These facilities generally have a high proportion of Medicaid residents; therefore, they have less revenue and fewer opportunities to cross-subsidize care with income from more profitable Medicare and private-pay patients.15 Moreover, these facilities are not randomly distributed; rather, they tend to cluster within poor communities.15 Low revenue, insufficient staffing, and poor-quality performance may all contribute to the lower vaccination rates in these facilities.
It is a challenge to promote quality efficiently in these lower-tier nursing homes, especially when public reporting or even pay-for-performance inducements might not be effective because of inadequate financial and human resources and expertise.33 Simply offering subsidies may be costly and ineffective without providing management assistance to make the organizational changes that are needed to promote the overall quality of care in nursing homes.
Recent efforts by Quality Improvement Organizations to help nursing homes introduce and sustain continuous quality improvement programs that would focus on improving vaccination rates, among other things, may be promising. But research is needed on how to effectively integrate this kind of support with either public reporting or pay-for-performance strategies.
Conclusion
Our findings indicate that flu vaccination rates in nursing homes have improved, particularly for black residents, over a fairly short period of time. Nonetheless, racial differences persist. Blacks have lower vaccination rates than whites both because they tend to reside in facilities that have lower vaccination rates in general and because they are less likely to get vaccinated in the same facility where white residents are vaccinated. Strategies that reduce the vaccination rate differences both between and within nursing homes are necessary in order to reduce those disparities and move closer toward the goal of a 90 percent flu vaccination rate for all nursing home residents.
Supplementary Material
Knowledge and beliefs about flu vaccines can be modified with education and increased trust in health care staff.
Acknowledgments
This work was supported in part by National Institute on Aging Grant No. P01AG027296 and in part by Agency for Healthcare Research and Quality (AHRQ) Grant No. HS018462. The National Institute on Aging and AHRQ had no role in the design and conduct of the study, in the collection, management, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Footnotes
An earlier version of this article was presented at the AcademyHealth Annual Research Meeting, June 2011, in Seattle, Washington.
Contributor Information
Shubing Cai, Center for Gerontology and Health Care Research, Brown University, in Providence, Rhode Island. shubing_cai@brown.edu.
Zhanlian Feng, Center for Gerontology and Health Care Research..
Mary L. Fennell, Brown University..
Vincent Mor, Brown University School of Medicine..
References
- 1.Thompson WW, Shay DK, Weintraub E, Brammer L, Bridges CB, Cox NJ, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292(11):1333–40. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- 2.Nichol KL, Nordin J, Mullooly J, Lask R, Fillbrandt K, Iwane M. Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly. N Engl J Med. 2003;348(14):1322–32. doi: 10.1056/NEJMoa025028. [DOI] [PubMed] [Google Scholar]
- 3.Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289(2):179–86. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 4.McBean AM, Babish JD, Warren JL. The impact and cost of influenza in the elderly. Arch Intern Med. 1993;153(18):2105–11. [PubMed] [Google Scholar]
- 5.McBean AM, Hebert PL. New estimates of influenza-related pneumonia and influenza hospitalizations among the elderly. Int J Infect Dis. 2004;8(4):227–35. doi: 10.1016/j.ijid.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 6.Shugarman LR, Hales C, Setodji CM, Bardenheier B, Lynn J. The influence of staff and resident immunization rates on influenza-like illness outbreaks in nursing homes. J Am Med Dir Assoc. 2006;7(9):562–7. doi: 10.1016/j.jamda.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 7.Kingston BJ, Wright CV., Jr Influenza in the nursing home. Am Fam Physician. 2002;65(1):75–8. 2. 1. [PubMed] [Google Scholar]
- 8.Menec VH, MacWilliam L, Aoki FY. Hospitalizations and deaths due to respiratory illnesses during influenza seasons: a comparison of community residents, senior housing residents, and nursing home residents. J Gerontol A Biol Sci Med Sci. 2002;57(10):M629–35. doi: 10.1093/gerona/57.10.m629. [DOI] [PubMed] [Google Scholar]
- 9.Jefferson T, Rivetti D, Rivetti A, Rudin M, Di Pietrantonj C, Demicheli V. Efficacy and effectiveness of influenza vaccines in elderly people: a systematic review. Lancet. 2005;366(9492):1165–74. doi: 10.1016/S0140-6736(05)67339-4. 1. [DOI] [PubMed] [Google Scholar]
- 10.Medicare and Medicaid programs; condition of participation: immunization for long-term care facilities. Final rule. Fed. Regist. 2005;70(194):58834–52. [PubMed] [Google Scholar]
- 11.Centers for Medicare and Medicaid Services . National nursing home vaccination quality measures: user’s manual supplement 2006 [Internet] CMS; Baltimore (MD): [cited 2010 Dec 28]. Avaliable from: http://www.cms.gov/NursingHomeQualityInits/downloads/NHQIVaccinationSupplement.pdf. [Google Scholar]
- 12.Bardenheier BH, Wortley P, Ahmed F, Hales C, Shefer A. Influenza immunization coverage among residents of long-term care facilities certified by CMS, 2005-2006: the newest MDS quality indicator. J Am Med Dir Assoc. 2010;11(1):59–69. doi: 10.1016/j.jamda.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 13.Li Y, Mukamel DB. Racial disparities in receipt of influenza and pneumococcus vaccinations among US nursing-home residents. Am J Public Health. 2010;100(Suppl 1):S256–62. doi: 10.2105/AJPH.2009.173468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith DB, Feng Z, Fennell ML, Zinn JS, Mor V. Separate and unequal: racial segregation and disparities in quality across US nursing homes. Health Aff (Millwood) 2007;26(5):1448–58. doi: 10.1377/hlthaff.26.5.1448. [DOI] [PubMed] [Google Scholar]
- 15.Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82(2):227–56. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The overall flu vaccination rate for Hispanics is 80.30 percent, 81.11 percent, and 81.81 percent for the 2006-07, 2007-08 and 2008-09 flu seasons, respectively.
- 17.Centers for Medicare and Medicaid Services . RAI User’s Manual 2009 [Internet] CMS; Baltimore (MD): [cited 2010 Sep 15]. Available for download from: http://www.cms.gov/NursingHomeQualityInits/50_NHQIMDS20.asp. [Google Scholar]
- 18.Centers for Disease Control and Prevention . Questions and answers: seasonal flu shot [Internet] CDC; Atlanta (GA): [cited 2010 Jul 26]. Available from: http://www.cdc.gov/flu/about/qa/flushot.htm. [Google Scholar]
- 19.Greene WH. Econometric analysis. 5th ed Prentice Hall; Upper Saddle River (NJ): 2002. [Google Scholar]
- 20.The denominator for the calculation of proportion of blacks includes individuals of all races.
- 21.Mor V, Intrator O, Unruh MA, Cai S. Temporal and geographic variation in the validity and internal consistency of the Nursing Home Resident Assessment Minimum Data Set 2.0. BMC Health Serv Res. 2011;11:78. doi: 10.1186/1472-6963-11-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mor V, Angelelli J, Jones R, Roy J, Moore T, Morris J. Inter-rater reliability of nursing home quality indicators in the U.S. BMC Health Serv Res. 2003;3(1):20. doi: 10.1186/1472-6963-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 24.Bardenheier B, Wortley P, Ahmed F, Gravenstein S, Hogue CJ. Racial inequities in receipt of influenza vaccination among long-term care residents within and between facilities in Michigan. Med Care. 2011;49(4):371–7. doi: 10.1097/MLR.0b013e3182054293. [DOI] [PubMed] [Google Scholar]
- 25.Cai S, Mukamel DB, Temkin-Greener H. Pressure ulcer prevalence among black and white nursing home residents in New York state: evidence of racial disparity? Med Care. 2010;48(3):233–9. doi: 10.1097/MLR.0b013e3181ca2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grabowski DC, McGuire TG. Black-white disparities in care in nursing homes. Atl Econ J. 2009;37(3):299–314. doi: 10.1007/s11293-009-9185-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hebert PL, Frick KD, Kane RL, McBean AM. The causes of racial and ethnic differences in influenza vaccination rates among elderly Medicare beneficiaries. Health Serv Res. 2005;40(2):517–37. doi: 10.1111/j.1475-6773.2005.00370.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nowalk MP, Zimmerman RK, Shen S, Jewell IK, Raymund M. Barriers to pneumococcal and influenza vaccination in older community-dwelling adults (2000-2001) J Am Geriatr Soc. 2004;52(1):25–30. doi: 10.1111/j.1532-5415.2004.52006.x. [DOI] [PubMed] [Google Scholar]
- 29.Fiebach NH, Viscoli CM. Patient acceptance of influenza vaccination. Am J Med. 1991;91(4):393–400. doi: 10.1016/0002-9343(91)90157-s. [DOI] [PubMed] [Google Scholar]
- 30.Schneider EC, Cleary PD, Zaslavsky AM, Epstein AM. Racial disparity in influenza vaccination: does managed care narrow the gap between African Americans and whites? JAMA. 2001;286(12):1455–60. doi: 10.1001/jama.286.12.1455. [DOI] [PubMed] [Google Scholar]
- 31.Chi RC, Neuzil KM. The association of sociodemographic factors and patient attitudes on influenza vaccination rates in older persons. Am J Med Sci. 2004;327(3):113–7. doi: 10.1097/00000441-200403000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Fiscella K. Commentary--anatomy of racial disparity in influenza vaccination. Health Serv Res. 2005;40(2):539–49. doi: 10.1111/j.1475-6773.2005.00371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Konetzka RT, Werner RM. Disparities in long-term care: building equity into market-based reforms. Med Care Res Rev. 2009;66(5):491–521. doi: 10.1177/1077558709331813. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.