Abstract
No studies have examined the applicability of varying methods for identifying youth at high risk of unintended pregnancies and contracting HIV. This study compares sociodemographic characteristics and sexual behaviors of youth (ages 15-24) in Port-au-Prince, Haiti surveyed using three different study methodologies. The three study methodologies are compared in terms of their utility for identifying high risk youth and utility for program planning. The three study methodologies are: a representative sample of youth from the 2005/6 Demographic and Health Survey (HDHS); a 2004 facility-based study; and a 2006/7 venue-based study that used the Priorities for Local AIDS Control Efforts (PLACE) method. The facility-based and PLACE studies included larger proportions of single, sexually experienced youth and youth who knew someone with HIV/AIDS than the HDHS. More youth in the PLACE study had multiple sexual partners in the last year and received money or gifts for sex compared to youth in facilities. At first and last sex, more PLACE youth used contraception including condoms. Pregnancy experience was most common in the facility-based data; however, more ever-pregnant PLACE youth reported ever terminating a pregnancy. Program managers seeking to target prevention activities should consider using facility- or venue-based methods to identify and understand the behaviors of high-risk youth.
Introduction
Research on sexual risk-taking among youth ages 15-24 in developing countries frequently focuses on participants in population-based, household surveys, representative at the national, regional or city levels. These studies have demonstrated varying results in terms of demographic factors associated with risk of HIV transmission among youth. For example, some population-based studies indicate that among sexually experienced youth, those who are less educated and from rural areas are less likely to use condoms and other forms of contraception, increasing their risk of contracting HIV or experiencing an unintended pregnancy (Adih and Alexander 1999; Eggleston 1998; Koenig et al. 2004; Prata et al. 2006; Voeten et al. 2004). Other factors associated with sexual risk-taking among youth include age at sexual debut (Geary et al. 2006; Thurman et al. 2006), experience of forced first sex (Geary et al. 2006; Koenig et al. 2004; Maharaj and Munthree 2006), and low self-efficacy (Adih and Alexander 1999; Boer and Mashamba 2007). While population-based studies provide a comprehensive perspective on risk factors for transmission and prevalence of HIV, sexually transmitted infections (STIs), and unintended pregnancies, they often fail to offer clear strategies for prevention programs because they do not examine youth access and use of specific reproductive health (RH) services. In addition, population-based studies often include large proportions of sexually inexperienced youth who are not yet at risk of adverse RH outcomes, such as HIV, STIs, and unintended pregnancies, and thus are often dropped from analyses (ORC Macro n.d.).
An alternative approach to understanding the risk of having an unintended pregnancy or HIV transmission among youth is to collect data in health facilities serving youth, such as HIV voluntary counseling and testing (VCT) centers and RH clinics (Bailey et al. 2003; Horizons Program et al. 2001; Meyer-Weitz et al. 2000; Newmann et al. 2005; Reynolds and Kimani 2006; Varga 1997). Most youth visiting these clinical sites are sexually experienced, increasing the sample of at-risk youth surveyed. Another advantage of collecting data in clinical sites is that it is possible to obtain information on receipt and quality of health services. Data from clinical sites can demonstrate which clients are exposed to the risk of contracting HIV because they do not use condoms, have multiple sexual partners or initiated sexual activity at an early age. Additionally, findings from facility-based studies of youth can be used to develop programmatic recommendations to improve youth’s RH knowledge, attitudes and skills, and reduce risky sexual behavior. While facility-based studies can provide the information described above, one limitation of these studies is the inability to characterize family planning and VCT needs of youth not visiting clinical sites. Youth outside of health facilities may have less need for clinical services or they may experience barriers to accessing clinical services.
A novel approach to identifying individuals at high risk of contracting and transmitting HIV is the Priorities for Local AIDS Control Efforts (PLACE) method, a rapid assessment monitoring tool used to identify high-risk venues where AIDS prevention programs could be focused and determine the extent of risk-taking within these venues (Weir et al. 2004; Weir et al. 2003). The PLACE method focuses on sites where new sexual partnerships are formed because the pattern of new partnerships in a community shapes its HIV epidemic (Anderson 1999). This method was developed to respond to gaps in information provided to local- and district-level program planners from nationally representative surveys. Such surveys are not cost-effective for obtaining a depth of understanding on risk-taking behaviors, particularly when those engaged in the highest risk behaviors (concurrent partnerships, non-use of condoms, sex in exchange for goods or money and sex with older/younger partners) are only a subsample of the total population or clustered in certain geographic areas (MEASURE Evaluation Project 2005; Weir et al. 2004). Findings from a PLACE study can be used to inform or develop HIV prevention programs situated in high-risk sites. The PLACE approach also has its limitations including: a) it may not represent all high-risk persons if some more hidden or dangerous sites are not included in the sample because they are not named by key informants or interviewers are unable to collect data due to safety concerns, and b) at the time of interview, some respondents may be under the influence of alcohol or drugs and thus may not provide an accurate portrayal of their sexual risk-taking and health-seeking behaviors or be unable to participate in the survey.
While previous research has examined differences in the prevalence of HIV between clinic-based and population-based samples (Changalucha et al. 2002; Dandona et al. 2006; Fylkesnes et al. 1998), few studies have compared the different methodologies for describing characteristics and risk behaviors of persons at risk of contracting HIV and experiencing unintended pregnancies (Tate et al. 2007). No studies to date have specifically determined the applicability of each method for identifying youth at high risk of adverse RH outcomes (e.g., HIV, STIs and unintended pregnancies) and the utility of each method for program planning for youth. This study compares sociodemographic and sexual behaviors among youth (ages 15-24) in Port-au-Prince (PAP), Haiti surveyed: a) in the 2005/6 nationally representative Demographic and Health Survey; b) for a facility-based study in 2004; and c) as part of a PLACE study in 2006/7. We first describe each study’s methodology and then compare the advantages of one approach over the other for identifying youth at risk of contracting HIV and/or experiencing unintended pregnancy by examining differences in demographic and risk factors among each study’s population; we conclude with a discussion of the types of programmatic recommendations that can come from each method.
Methods
Data Sets
We examine three data sets in this study. First, we use the Haiti Demographic and Health Survey (HDHS), collected between 2005 and 2006 (Cayemittes et al. 2007). The survey includes a nationally representative sample of 10,757 women aged 15-49 and 4,958 men ages 15-59. Using a multistage sampling design, a random sample of enumeration areas was selected, followed by systematic selection of a random sample of households from a listing of all households in the selected enumeration areas. All eligible women in the sampled households were approached and asked to participate in the interview. In half of the households, all eligible men were invited to participate. Women and men who consented to be interviewed were asked the survey questions by trained interviewers. The surveys provide data on the demographic, socioeconomic and cultural characteristics of women and men in Haiti. For the analyses presented here, we selected the subsample of young women and men ages 15-24 interviewed in the PAP metropolitan area and compared it with the two other data sets that focus on PAP youth. A total of 970 female youth ages 15-24 and 345 male youth from PAP are included in the HDHS study sample (weighted sample sizes are 1,385 and 530, respectively). The HDHS data are compared to the other data sources on background demographic characteristics and sexual experience.
The second dataset is from a facility-based study that occurred in 2004 with youth clients of four youth centers and one RH clinic for women of all ages in PAP (Murray et al. 2005). The youth centers are places where youth go to socialize; play games; learn skills (e.g., computer, English, etc.); obtain information about RH; see a RH provider for family planning, pregnancy tests, prenatal care or STI counseling and testing; and get tested for HIV. The youth centers also distribute condoms to persons who walk up and register at the condom distribution window. The RH clinic included is available to men and women of all ages; however, it generally serves women. At the RH clinic, only youth clients (ages 15-24) were recruited. All facilities included in the study were managed by Fondation pour la Santé Reproductrice et l’Education Familiale (FOSREF), the primary provider of youth RH services in Haiti. The four FOSREF youth centers were selected to represent various neighborhoods of PAP. The FOSREF all-age RH clinic was included because it is the main RH facility serving the urban poor in Cité Soleil, a densely populated PAP slum. FOSREF was also the local implementing partner of the facility-based study and the PLACE data collection described below.
All young women and men ages 15 to 24 visiting the targeted facilities for VCT or RH services during the three-month study period were approached and asked to participate in the exit interview. Clients who visited the facility multiple times during the study period were only interviewed once to avoid duplicate responses. A screening tool was used to ask clients if they had previously been interviewed as part of this study. In addition to youth VCT and RH clients, young persons who visited the four youth centers to obtain free condoms were also asked to participate in the survey. (There was no condom distribution program at the RH clinic.) A total of 807 young women and 478 young men were interviewed in the multiple sites. Only a small number of young women and men refused to be interviewed. The study did not collect information on those youth who refused to be interviewed so it is not possible to determine if non-responders were different than responders. Future studies should keep records of non-responders and, when possible, obtain a small amount of information from them (e.g., gender, age, and reason for visit). Because few men (n=35) accessed RH services and few women (n=39) visited the condom distribution program, these participants were dropped from the analysis. The final analyses are based on 583 female clients of RH services, 168 female clients of VCT, 197 male clients of VCT and 242 male recipients of condoms from the youth centers.
The third data set was collected using the PLACE methodology; this study was undertaken by the MEASURE Evaluation Project in collaboration with FOSREF between 2006 and 2007 (Speizer et al. 2007). Because the PLACE methodology is a new method, we describe it in greater depth than the other two methods. The PLACE method has five main steps. In the first step, the project team engages local stakeholders to help identify the priority areas for a rapid assessment of HIV risk-taking and prevention approaches. Stakeholders review existing data on the HIV epidemic and use this information to identify the study area, known as a priority prevention area (PPA). For this application of the PLACE methodology, the emphasis was on youth sexual risk-taking, so we were seeking a PPA with a large population of youth engaged in sexual risk-taking. The selected PPA included two adjacent neighborhoods in PAP: Bizoton and Thor. The second step uses knowledgeable community-informant interviewing to identify venues where residents of the PPA meet sexual partners. Community informants were defined as men and women knowledgeable about the movement and behavior of young people in the area. A list of ten types of community informants that were sought (e.g., taxi drivers, truck drivers, hotel managers, teachers, police officers) was created with input from the stakeholders prior to undertaking field work. Interviewers were instructed to try to find a pre-determined number of each type of community informant. In a two-week period, a total of 494 community informants were asked and willing to identify locations where youth go to meet sexual partners. These community informants identified 1,686 sites.
In the third step, the list of venues from community informants is reviewed to determine which sites represent unique locations. Data were entered and cleaned to eliminate duplicate locations. A total of 303 unique venues were identified. Of these, 257 were in the PAP metropolitan area. Interviewers visited each reported venue to verify its existence and location and to interview a venue representative (such as a bar manager or owner or someone who worked in the vicinity of an outdoor venue) to obtain characteristics of the venue important for HIV prevention. Where someone was not available for interview on the first visit, an appointment was requested for a second visit. Verbal consent for an anonymous interview was obtained prior to completing the survey. Interviewers used closed-ended surveys to obtain information from a venue representative about: the name of the venue and number of years in operation; types of activities occurring in the venue; estimated number of clients at peak times; estimates of daily amount of alcohol consumed; different cadres of staff; patron characteristics, including residence, employment status, age and gender; whether people meet new and previous sexual partners at the venue; extent of AIDS/STI prevention activities on-site, including condoms and posters; and willingness to sell condoms. In addition, a global positioning system (GPS) point was recorded at each site to permit mapping of sites identified and selected for study. Of the 257 sites that were in the PAP area, 155 were found and verified; of these, only 109 were in the targeted PAP neighborhoods of Bizoton and Thor. The most common type of sites identified were transport, public and commercial areas (32%) followed by educational sites (12%), hotels (12%) and isolated/private sites (13%).
Based on the list of all sites identified in Bizoton and Thor and the estimated number of individuals reported to frequent the sites, a systematic sampling approach was used to choose 40 clusters where individual interviews would take place in step 4. In particular, each venue was assigned numbers that corresponded to the estimated number of patrons visiting the site. The systematic sampling approach chooses a random number between 1 and the interval width and selects sites systematically based on that number. Using this selection method, sites that were larger had a higher probability of being selected and some of the largest sites were selected twice (representing two clusters). Two rounds of data collection were undertaken in step 4: the first round mimicked a typical PLACE study, with interviews with site patrons of all ages, and the second round targeted youth and included other RH questions, in addition to the standard HIV-related questions. In the first round of patron interviews, 24 individuals were interviewed at each selected site. Larger sites (those with 50 or more patrons) represented two clusters and therefore twice as many individuals (48 individuals) were interviewed. Interviewers were instructed to select people in a random manner to be interviewed. Interviewers were told to imagine a large X in the middle of the floor and to approach people on the X. When a person was identified, the interviewer asked them to come to a quiet place to be interviewed, such as in a corner or outside. A total of 876 interviews with eligible and consenting individuals socializing at the sites were undertaken in the first round of data collection that was similar to a standard PLACE study. For the first round of data collection, a total of 31 unique sites were included, representing 40 clusters.
The data used in this study come from the second round of data collection that focused specifically on youth and their sexual risk-taking behaviors. About two months after the first round of data collection, interviewers returned to the same sites to interview persons ages 15-24. In each facility, we sought to interview about 12 youth, though 24 youth were interviewed in the larger sites (representing two clusters). A total of 504 youth (237 females and 267 males) were interviewed in Round 2. An additional six sites (for a total of 37) were added at the time of Round 2 data collection, given that six of the original sites tended to be lower-risk sites that were selected based on the frequency of people visiting and not risk-taking behaviors (e.g., school-based sites). Interviewers approached an eligible participant and briefly described the study and asked for verbal consent to participate. If a youth was willing to participate, the interviewer sought a private place in the corner or outside for the interview to take place. The interviewer used a closed-ended questionnaire and asked questions on: socio-demographics; frequency visiting the site; reason for visiting the site; whether the respondent had ever met a sexual partner at the site; sexual behaviors including age at first sex, family planning use at first and last sex, cross-generational and transactional sex, number of sexual partners; pregnancy history; fertility desires; and exposure to HIV prevention programs. Most patrons approached in both rounds of data collection were willing to participate. Unfortunately, no information is available on those persons who refused to be interviewed. Future studies should keep track of the number of individuals who refuse to participate and, if possible, obtain a small number of characteristics such as age, gender, and reason for visiting the venue to permit an assessment of whether non-responders are different than responders.
Variables
Data from the three studies are compared to provide a perspective on youth demographic and sexual behavior characteristics and to demonstrate the different types of programmatic recommendations that can come from each source. Across the three studies, similar demographic questions were included. For the examination of HIV risk-taking behaviors, the presentation focuses on the comparison between the facility-based data and the PLACE data. The main HIV risk-taking behaviors of interest include: sexual experience, age at sexual debut, number of sexual partners in the last year, condom use, and engagement in transactional sex (sex in exchange for money or goods). All measures were included with a similar format in the facility-based and PLACE studies. A question on previous STIs was also included in each study in varying formats. In the PLACE study, youth were asked if they had any of three gender-specific symptoms indicative of an STI in the last four weeks. In the facility-based study, youth were asked if they had had an STI in the last year, without any description of the possible symptoms. While the STI variables are not directly comparable, they do demonstrate patterns that are indicative of risk-taking in the two study populations.
Factors associated with the risk of an unintended or teenage pregnancy were also included in the studies. In the PLACE and facility-based studies, youth were asked about family planning use at first and last sex. Additionally, sexually experienced female youth were asked about (1) pregnancy experience, (2) number of pregnancies, (3) whether they wanted their last pregnancy, and (4) pregnancy termination experience. Male youth were asked comparable questions about whether they ever impregnated a woman and, if so, the number of pregnancies, wantedness of last pregnancy, and whether any of the pregnancies had been terminated.
Analysis
The HDHS data were analyzed using weights and adjusting for the survey sampling design. Because of the different study designs and weights, separate distributions are presented for each study. Chi-square tests are performed to compare, by gender, the PLACE youth to the facility-based youth. A limitation of this analysis is that no significance tests are presented to compare the HDHS to the other two studies on demographic characteristics due to the weights and the survey sampling design used in the HDHS; this makes it difficult to undertake accurate statistical comparisons. All analyses were conducted using Stata/SE 9.2 statistical software.
Results
Demographic Characteristics
In Table 1, demographic characteristics for the HDHS, PLACE and facility-based (by type of facility where surveyed) youth are presented by gender. Union status for females varied considerably across the studies. Female youth surveyed at the RH clinic were mostly married or living together (in union) (61 percent), while smaller proportions of female youth were in union in the HDHS (32 percent) and VCT clinic site (31 percent). Only 6 percent of female youth in the PLACE study were in union. Results were less disparate for male youth, with most males in all four settings not being in union. Both male and female youth in the HDHS were less educated than those in the other studies. A greater percentage of male youth surveyed at VCT sites and condom distribution sites had completed secondary school as compared to male youth in the HDHS; among females, those at the VCT clinics had the highest level of education.
Table 1.
Demographic characteristics of Port-au-Prince youth, by gender and data collection approach
| Demographic Characteristics | Females | Males | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| HDHSb (n=970) |
PLACE (n=237) |
FOSREF facility - RH (n=583) | FOSREF facility - VCT (n=168) | HDHSb (n=345) |
PLACE (n=267) |
FOSREF facility - VCT (n=197) | FOSREF facility - Condom (n=242) | |
| Age | *** | |||||||
| 15-19 | 53.6 | 62.0 | 31.5 | 50.3 | 44.7 | 49.4 | 54.3 | 48.4 |
| 20-24 | 46.4 | 38.0 | 68.5 | 49.7 | 55.3 | 50.6 | 45.7 | 68.5 |
| Marital status | *** | *** | ||||||
| In uniona | 31.6 | 6.0 | 61.0 | 31.3 | 11.9 | 3.8 | 27.1 | 32.3 |
| Not in union | 68.4 | 94.0 | 39.0 | 68.7 | 88.1 | 96.2 | 72.9 | 67.7 |
| Education level | *** | ** | ||||||
| None | 2.5 | 0.9 | 4.4 | 0.6 | 2.0 | 2.0 | 0.0 | 0.0 |
| Primary | 30.8 | 10.3 | 16.9 | 1.8 | 22.2 | 5.3 | 1.5 | 2.5 |
| Secondary | 62.0 | 78.1 | 72.0 | 87.0 | 67.9 | 80.2 | 91.4 | 85.5 |
| Higher | 4.7 | 10.7 | 6.7 | 10.7 | 8.0 | 12.6 | 7.1 | 12.0 |
| Religion | *** | *** | ||||||
| Catholic | 48.4 | 50.2 | 51.0 | 43.7 | 38.3 | 45.1 | 33.9 | 43.8 |
| Protestant | 45.6 | 34.2 | 36.2 | 39.5 | 46.7 | 33.8 | 43.1 | 44.2 |
| Voodooism/none/other | 6.0 | 15.6 | 12.8 | 16.8 | 15.0 | 21.1 | 23.0 | 12.0 |
| Knows someone with HIV/AIDS | ** | *** | ||||||
| No | 84.8 | 71.7 | 60.5 | 57.9 | 84.5 | 65.5 | 46.3 | 46.4 |
| Yes | 15.2 | 28.3 | 39.5 | 42.1 | 15.5 | 34.5 | 53.7 | 53.6 |
| Sexual experience | *** | *** | ||||||
| Never had sex | 37.8 | 32.9 | 8.2 | 11.3 | 15.8 | 18.7 | 1.5 | 1.2 |
| Sexually experienced | 62.2 | 67.1 | 91.8 | 88.7 | 84.2 | 81.3 | 98.5 | 98.8 |
Includes married and in union
HDHS data are weighted and analyzed adjusting for survey sampling; unweighted n’s shown for DHS, weighted n’s are: 1385 for female youth and 530 for male youth.
Notes: Some of the cells have fewer than the total number of observations due to missing data and some columns do not sum to 100% because of rounding. Chi-square comparisons:
p ≤ 0.01;
*p ≤ 0.001 for comparison between distributions for PLACE and joint FOSREF facility-based youth, by gender.
HIV/AIDS exposure is measured by the proportion of respondents that reported knowing someone with HIV/AIDS. Within each of the studies, the proportions of male and female youth who knew someone with HIV/AIDS were similar. For both males and females, a greater proportion of respondents in the facility-based study reported knowing someone with HIV/AIDS than in the HDHS and PLACE studies. While 54 percent of males responded affirmatively to this question in both the VCT and condom distribution facilities, only 35 percent in the PLACE study and 16 percent in the HDHS reported knowing someone with HIV/AIDS. The pattern was similar for female youth, as a greater percentage in the RH (40 percent) and VCT clinics (42 percent) responded affirmatively, compared to the PLACE (28 percent) and HDHS (15 percent) surveys. The differences between the facility-based study and the PLACE study (by gender) were significant for all of the demographic variables included, with the exception of age group for male youth.
While both male and female youth had similar levels of sexual experience in the HDHS and PLACE studies (see Table 1), respondents in the facility-based study had much higher levels of sexual experience, particularly the females. Nearly 92 percent of female youth at the RH clinic and 89 percent at VCT clinics had sexually debuted, compared to 62 percent in the HDHS and 67 percent in the PLACE study. Males were more likely to be sexually experienced than females in the HDHS and PLACE surveys (84 percent and 81 percent, respectively), and nearly all males had initiated sexual activity in the VCT and condom distribution settings.
The differences between the HDHS and the other two studies are generally expected, given that the HDHS captures all female and male youth and not necessarily those at higher risk of HIV, STIs or unintended pregnancies. The remainder of this paper focuses on comparing risk behaviors between the facility-based study methodology and the PLACE methodology in terms of identifying programmatic strategies to reduce the risk of HIV, STI and unintended pregnancies among youth.
Sexual Risk-Taking
Among sexually experienced female youth, the median age of first sex was 16 and the mean was similar in both the PLACE and facility-based data collection approaches (Table 2). The PLACE female youth were significantly more likely to report (1) having had multiple sexual partners in the past year and (2) condom use at last sex as compared to female youth receiving RH or VCT services surveyed in facilities. The majority (74 percent) of female youth in the PLACE study reported experiencing any of three STI symptoms (abdominal pain, vaginal discharge and genital ulcers) in the past four weeks compared with much smaller proportions in the facility-based study that asked about STI experience in the last year, without a description of specific symptoms. Female youth in the PLACE study were also significantly more likely to report transactional sex, with 3 percent giving and 10 percent receiving money or goods in exchange for sex. The corresponding percentages were smaller in the RH and VCT clinics.
Table 2.
Sexual experience and reproductive health behaviors of Port-au-Prince female sexually experienced youth, by data collection approach
| PLACE (n=157) | FOSREF Facility – RH (n=533) | FOSREF Facility - VCT (n=148) | |
|---|---|---|---|
| Age at first sex | |||
| 12 or younger | 8.5 | 4.3 | 4.7 |
| 13 | 5.9 | 5.5 | 3.4 |
| 14 | 12.4 | 9.8 | 12.2 |
| 15 | 13.1 | 17.2 | 16.9 |
| 16 | 17.0 | 16.2 | 21.6 |
| 17 | 16.3 | 16.0 | 22.3 |
| 18-21 | 25.5 | 29.3 | 15.5 |
| 22-24 | 1.3 | 1.8 | 3.4 |
| Mean (median) | 16.0 years (16 years) | 16.4 years (16 years) | 16.2 years (16 years) |
| # of partners in last 12 months | *** | ||
| 0 | 5.7 | 2.5 | 3.4 |
| 1 | 59.2 | 87.5 | 73.7 |
| 2 | 7.6 | 6.8 | 13.5 |
| 3+ | 14.7 | 3.2 | 9.5 |
| (less than 5) | 12.7 | na | na |
| Condom use at last sexa | *** | ||
| No | 40.0 | 79.3 | 57.1 |
| Yes | 60.0 | 20.8 | 43.0 |
| STI experienceb | *** | ||
| No | 25.8 | 84.5 | 90.3 |
| Yes | 74.2 | 15.5 | 9.7 |
| Transactional sex – ever | |||
| Gave money/goods | 3.2* | 0.6 | 0.7 |
| Received money/goods | 10.1*** | 1.9 | 2.0 |
| Used FP at first sex | *** | ||
| No | 56.5 | 87.0 | 75.8 |
| Yes | 43.5 | 13.0 | 24.2 |
| Used FP at last sex | *** | ||
| No | 28.7 | 59.9 | 51.0 |
| Yes | 71.3 | 40.1 | 49.0 |
| Ever pregnant | *** | ||
| No | 76.4 | 31.9 | 71.4 |
| Yes | 23.6 (n=37) | 68.1 (n=363) | 28.6 (n=42) |
| Number of pregnancies | ** | ||
| 1 | 48.6 | 57.9 | 83.3 |
| 2 | 37.1 | 30.9 | 11.9 |
| 3+ | 14.3 | 11.2 | 4.8 |
| Wanted last pregnancy | ** | ||
| No | 48.6 | 70.1 | 82.5 |
| Yes | 51.4 | 29.9 | 17.5 |
| Ever abortion | *** | ||
| No | 41.7 | 78.6 | 57.1 |
| Yes | 58.3 | 21.4 | 42.9 |
Condom use at last sex only asked for youth who had sex in the last year.
Some missing data because people did not know symptoms or did not respond. PLACE asks about experience with three specific symptoms in last 4 weeks, clinic survey only asks if youth ever had an STI in the last year.
Notes: Some cells have fewer observations due to missing data; some columns do not sum to 100% because of rounding. na – not applicable. FP – family planning. Chi-square comparisons:
p ≤ 0.05;
*p ≤ 0.01;
p ≤ 0.001 for comparison between distributions for PLACE and both FOSREF facility-based youth jointly.
Among sexually experienced male youth, the median age of first sex was 13 (facility-based sites) or 14 (PLACE) (see Table 3). A large proportion of males in the PLACE and facility-based studies reported having first sex before the age of 12, ranging from 41 percent to 48 percent; only 26 percent of male youth in the HDHS sexually debuted before age 12 (not shown). A significantly greater proportion of male youth in the PLACE study reported multiple sexual partners in the last year as compared to the facility-based study. Condom use at last sex was highest among men in the PLACE study (70 percent), though it was also high among those surveyed at the condom distribution program (67 percent). STI symptoms (painful urination, urethral discharge or genital ulcers) were also reported more frequently by PLACE respondents (49 percent). While male youth in the PLACE study were more likely to report giving money or goods in exchange for sex (28 percent, not significant), those at the condom distribution program were significantly more likely to report receiving money or goods in exchange for sex (18 percent).
Table 3.
Sexual experience and reproductive health behaviors of Port-au-Prince male sexually experienced youth, by data collection approach
| PLACE (n=212) | FOSREF Facility-VCT (n=193) | FOSREF Facility-Condom (n=233) | |
|---|---|---|---|
| Age at first sex | |||
| 12 or younger | 40.6 | 48.0 | 41.7 |
| 13 | 7.6 | 8.5 | 11.3 |
| 14 | 16.5 | 8.5 | 13.0 |
| 15 | 13.2 | 11.3 | 14.8 |
| 16 | 9.4 | 7.9 | 6.1 |
| 17 | 7.1 | 6.8 | 5.7 |
| 18-21 | 5.7 | 7.9 | 6.1 |
| 22-24 | 0.0 | 1.1 | 1.3 |
| Mean (median) | 13.2 years (14 years) | 12.4 years (13 years) | 12.7 years (13 years) |
| # of partners in last 12 months | *** | ||
| 0 | 5.5 | 14.0 | 2.5 |
| 1 | 23.5 | 28.5 | 33.5 |
| 2 | 8.3 | 15.5 | 15.3 |
| 3+ | 54.4 | 42.0 | 48.7 |
| (less than 5) | 8.3 | na | na |
| Condom use at last sexa | *** | ||
| No | 30.2 | 51.0 | 33.5 |
| Yes | 69.9 | 49.0 | 66.5 |
| STI experienceb | *** | ||
| No | 50.7 | 92.1 | 94.0 |
| Yes | 49.3 | 7.9 | 6.0 |
| Transactional sex – ever | |||
| Gave money/goods | 28.2 | 19.8 | 23.2 |
| Received money/goods | 6.1*** | 12.6 | 18.1 |
| Used FP at first sex | *** | ||
| No | 52.6 | 82.9 | 84.8 |
| Yes | 47.4 | 17.1 | 15.2 |
| Used FP at last sex | *** | ||
| No | 20.8 | 46.6 | 31.8 |
| Yes | 79.2 | 53.4 | 68.2 |
| Ever gotten a woman pregnant | |||
| No | 76.8 | 77.0 | 74.3 |
| Yes | 23.2 (n=49) | 23.0 (n=44) | 25.8 (n=60) |
| Number of pregnancies | |||
| 1 | 52.1 | 63.6 | 67.3 |
| 2 | 14.6 | 20.5 | 18.2 |
| 3+ | 33.3 | 15.9 | 14.5 |
| Wanted last pregnancy | |||
| No | 76.9 | 78.1 | 89.1 |
| Yes | 23.1 | 22.0 | 10.9 |
| Ever abortion | |||
| No | 24.5 | 25.0 | 35.0 |
| Yes | 75.5 | 75.0 | 65.0 |
Condom use at last sex only asked for youth who had sex in the last year.
Some missing data because people did not know symptoms or did not respond. PLACE asks about experience with three specific symptoms in last 4 weeks, clinic survey only asks if youth ever had an STI in the last year.
Notes: Some cells have fewer observations due to missing data; some columns do not sum to 100% because of rounding. na – not applicable. FP – family planning. Chi-square comparisons:
p ≤ 0.05;
p ≤ 0.01;
p ≤ 0.001 for comparison between distributions for PLACE and both FOSREF facility-based youth jointly.
Family Planning and Fertility Behaviors
Female youth in the PLACE study were significantly more likely to report using family planning at first sex (44 percent) and last sex (71 percent) than those surveyed at FOSREF facilities (Table 2). Most of the family planning use was condoms (not shown). Two-thirds of female youth surveyed at the RH clinic had ever been pregnant; the proportion ever pregnant was significantly smaller in the PLACE and VCT sites. Among female youth that had ever been pregnant, those in the PLACE study were more likely to report multiple pregnancies. Responses to pregnancy desirability varied considerably across the data collection approaches. Only 18 percent of ever pregnant female youth in the VCT clinic and 30 percent in the RH clinic reported wanting their last pregnancy. While 51 percent of female youth in the PLACE study said they wanted their last pregnancy, they were also more likely to report ever having an abortion (58 percent).
Male respondents in the PLACE study also reported significantly higher levels of family planning use at first sex (47 percent) and last sex (79 percent) (Table 5). Similar levels of male youth reported ever impregnating a woman in the PLACE and facility-based studies (ranging from 23 to 26 percent). Among male youth who reported ever fathering a child, a greater proportion in the PLACE study reported multiple pregnancies, with 33 percent reporting three or more. This difference was not significant in comparing the PLACE and facility-based studies. Desirability of the last pregnancy was generally low, particularly at the condom distribution program, where 89 percent of men said their partner’s last pregnancy was not wanted. Males who had ever impregnated a woman also reported high levels of abortion in the PLACE (76 percent), VCT (75 percent) and condom distribution (65 percent) sites.
Access to Reproductive Health Services in the PLACE Study
An advantage of the PLACE approach is that because it is not based in a facility, it is possible to assess youth’s interest and access to RH services. This is particularly interesting given that the PLACE identifies youth at high-risk of STIs, HIV, and unwanted pregnancies. In Figure 1, use of VCT and interest in using VCT in the next 12 months is presented for sexually experienced female and male youth interviewed in the PLACE study. Nearly a third of sexually experienced females reported having had an HIV test in the past 12 months while about a quarter of sexually experienced male youth reported recent testing. The majority of respondents were interested in being tested in the next 12 months. In another question, sixty-three percent of sexually experienced female youth reported ever using clinical services (not shown); the comparable proportion among their male counterparts was 59 percent. Notably, when asked the reason for their last clinical visit, most youth reported that the most recent visit was for services other than RH or VCT (not shown). In the PLACE study, there was a high percentage of female and male youth who reported having had symptoms of STIs and that had never been tested for HIV but was interested in VCT. This could mean that the youth surveyed have more access to general clinical services than to RH and STI services, including VCT.
Figure 1.
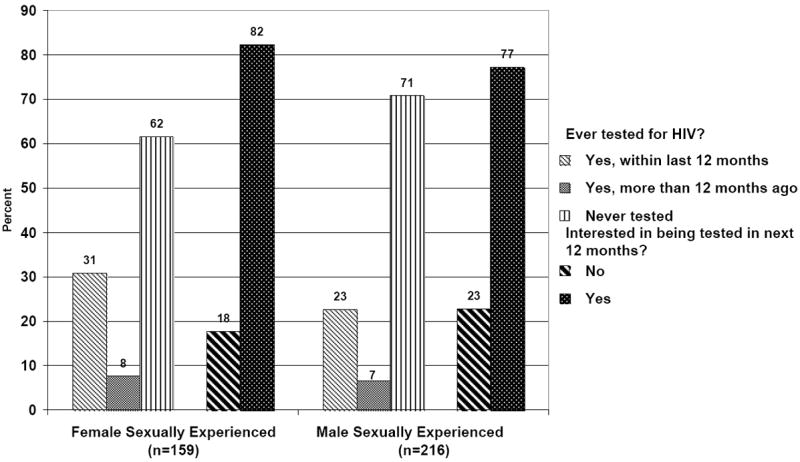
HIV testing experience and interest among sexually experienced youth in place study, 2006/7, by gender
Discussion
This study examines three approaches to studying youth sexual risk taking to inform future RH programming. The conventional approaches, such as undertaking a population-based study and obtaining exit interviews with youth visiting RH facilities, each have limitations for informing programmatic approaches. In particular, population-based studies, such as the Demographic and Health Surveys, often include large proportions of youth who are sexually inexperienced or in union, and thus not at high risk of HIV and unintended pregnancies. Furthermore, population-based approaches are often costly to implement. Facility-based studies, while less-expensive and more likely to include sexually experienced youth, are limited because they focus on youth who already have access to RH and VCT services; responses from these youth cannot be used to identify strategies to target youth who do not visit the facilities. The PLACE methodology, which is also a rapid and low-cost approach, provides an alternative method to examine sexual risk-taking among youth to inform future programming that can take place at the identified venues and in communities. In addition, because the PLACE approach identifies youth at non-clinical locations, it is possible to determine youths’ RH service needs.
This study demonstrates that youth identified in the PLACE and facility-based studies are different in terms of their demographic characteristics than youth included in a population-based sample. In particular, the PLACE and facility-based studies generally included a larger proportion of youth who were not in union, have secondary or higher education and know someone with HIV/AIDS than the HDHS.
In the comparison of the facility-based and PLACE methodologies, we find that female youth in the PLACE study reported higher levels of protective behaviors such as condom use at last sex and family planning use at first and last sex, compared with female youth in the facility-based study. This is likely related to the fact that female youth visiting the RH clinic were significantly more likely to have ever been married and to have ever been pregnant than all others. This is to be expected, given that some of the young women interviewed for the study were visiting the RH clinics for pregnancy testing and prenatal care. Conversely, the sexually experienced female youth in the PLACE study were more likely to be single, have had multiple sexual partnerships in the last year and have participated in transactional sex than their counterparts surveyed in RH and VCT sites, putting the PLACE youth at risk of HIV and other STIs.
The comparison of the facility-based and PLACE data indicated that male youth in the two studies were similar for most risk-taking behaviors. Male youth who received free condoms at participating youth centers were similar to male youth surveyed in high-risk venues. Among both males and females in the PLACE study, most had never been tested for HIV, though many were interested in being tested in the next 12 months.
A number of gender differences are also apparent within and across the data sources. In particular, across all of the data sources, a smaller percentage of males are in union and a greater percentage has ever had sex. Males also report a much earlier age at sexual debut than females. Whether this indicates that males initiate sex with older females or females under-report their sexual activity is not possible to determine with the available data. Across each data source, a similar percentage of female and male youth report experience with a pregnancy. Conversely, a smaller percentage of males report that the last pregnancy was wanted and a greater percentage of males report that they have ever had a partner that aborted a pregnancy. This suggests that males are highly motivated to avoid an unwanted pregnancy; programs that target males for HIV prevention may want to use this motivation to help support condom use for HIV and pregnancy prevention.
This study provides a portrait of youth risk-taking from three different study approaches of PAP youth. We were unable to locate any previous studies comparing different approaches aimed at capturing characteristics and sexual behaviors of youth. Most studies that do compare clinic- and population-based approaches focus on differences in HIV seroprevalence between sentinel surveillance and community-based samples of adults (Changalucha et al. 2002; Dandona et al. 2006; Fylkesnes et al. 1998), and very few compare sexual behaviors (Tate et al. 2007). The present study demonstrates that household surveys may not reach youth at greatest risk of contracting HIV and experiencing unintended pregnancies, and that alternative approaches are needed for the development of targeted prevention programs for these youth.
Facility-based and PLACE studies can be used to make programmatic recommendations for youth HIV and unintended pregnancy prevention programming. For example, a large proportion of youth in the PLACE study reported interest in being tested for HIV, though most had not been recently tested, and few had accessed RH services. This suggests that sending outreach workers to the PLACE sites may be a viable approach to attract high-risk youth to the youth centers for VCT and other RH clinical services.
The facility-based data showed high levels of pregnancy experience, with many pregnancies reported as unwanted and one-fifth of women ever having had an abortion. Reports of unwanted pregnancies and abortions are indicative of unintended pregnancies (mistimed and unwanted) in this population. Indeed, some of the pregnancies reported as unwanted are likely to be considered mistimed (i.e., a desire to delay the birth by two or more years) rather than not wanted at all, but this distinction was not obtained in the study. The data from the RH clinic indicate the need for pregnancy prevention programs targeting sexually active women before they become pregnant and are identified in a RH clinic, and for the prevention of subsequent unintended pregnancies. The VCT data from female and male youth and the condom distribution data from male youth indicate that youth using these services are at high-risk of STIs and HIV. Strengthening and intensifying prevention programs within the youth centers could help these youth to avoid future risks of negative outcomes. These programs should also target unintended pregnancy risks, given that we found that about a quarter of female and male youth identified in facility-based sites had ever experienced (or had a partner who experienced) a pregnancy and nearly three-quarters reported that the last pregnancy was unwanted, with particularly high levels of abortions reported among male youth.
The PLACE data also can be used to make programmatic recommendations. These data provide rich information on: 1) the types of locations where young people meet new sexual partners; 2) the potential to implement STI and HIV prevention programs in these sites; and 3) site patron sexual risk-taking. This paper did not highlight the data from step 3 of the PLACE methodology; however, in this step, information is obtained on the types of sites, the hours when the sites are most frequently visited, the types of people visiting the sites (e.g., estimates of age and gender distributions), activities at the sites (e.g., drinking, socializing, sports, etc.), and physical locations of sites (by recording GPS data). This information could be used by RH program managers seeking to target high-risk sites with outreach workers who provide information on HIV risk-taking and who can refer patrons for RH services at local facilities. Outreach workers could also sell or refer patrons for condoms and other contraceptives. Specific high-risk behaviors may also be targeted in the venues. For example, in the present study, we found that youth in the PLACE study reported higher levels of multiple partnerships and transactional sex than those visiting facilities. Programs that promote alternative income generating activities or target reduction of multiple and concurrent partnerships are important for these high-risk youth. Moreover, if it is found that all sites are clustered in a particular area or along a main road, the program can undertake community-wide events and one-on-one activities in these specific neighborhoods and locations.
To date, there is a lack of epidemiological evidence linking interventions in PLACE sites with reduced HIV-risk-taking behaviors; this may be a consequence of a lack of or poor intervention development, failure to evaluate programs in these sites or the possibility that some of the highest-risk sites (and, ultimately, highest-risk individuals) are not identified using the PLACE method (Weir et al. 2004). A randomized controlled trial is currently underway in Jamaica to test this methodology of targeting sites based on PLACE findings (Weir et al. 2008).
An additional way that the PLACE methodology can be used is for program conceptualization, modification and evaluation. In particular, collecting PLACE data (with or without facility-based data) provides an indication of gaps in existing programs in terms of outreach in the community and patron (youth) sexual risk-taking behaviors and needs. While a limitation of our PLACE data is that the survey did not include specific enough questions about accessing FOSREF clinics, programs can collect such data and identify gaps in their interventions. Programs can use this information to target new locations, revise program messages and approaches and increase access to VCT and other RH services. Moreover, if the PLACE data are collected at the beginning of the program to inform program strategies, they also can be collected again at follow-up to determine if patron sexual risk-taking has changed once the program has been fully implemented in the sites.
Some of the limitations of the PLACE approach have been mentioned above. This includes possibly missing some of the highest risk groups if they visit hidden or dangerous locations that are not included in the study sites, and persons interviewed in identified sites may be inebriated or under the influence of drugs and thus may not accurately report their sexual and RH behaviors. In the Haiti application of the PLACE methodology, every effort was made to include even some of the highest-risk sites identified. This was done by having interviewers who would be working late at night in the high-risk sites stay at hotels in the area, to avoid having study drivers in the neighborhoods in the middle of the night. While not all of the study sites had alcohol (e.g., taxi stands and other outdoor public venues), those that did may have under-represented the individuals who had consumed large amounts of alcohol, since these individuals were less likely to be approached by study interviewers. With the data available, it is not possible to determine the extent of bias introduced by not interviewing inebriated youth. An additional limitation of the PLACE approach is that when questions are asked about facility use, respondents may not know the name of the facility nor be able to give a specific address or location. This limits the possibility of examining access to RH services at specific facilities.
Beyond the limitations of each study approach, there are also a number of limitations of this comparative study that are worth noting. In particular, there is a lack of significance testing across the three datasets on demographic characteristics due to the different study designs and weights. Additionally, while most of the variables were similarly measured across the studies, the STI variable did vary, making interpretations more difficult. Moreover, other variables that are risk factors for contracting HIV and experiencing an unintended pregnancy, such as partner violence, history of child abuse and cross-generational sex, were not included in this comparison because of a lack of common survey items across the studies. For example, in a separate analysis, we found that sexual violence was a risk factor for condom non-use, pregnancy experience and recent STI symptoms among PLACE youth but were not able to explore differences in violence experiences here because of a lack of violence measures in the facility-based data (Gómez et al. in press). Finally, while the HDHS youth represent the entire PAP metropolitan area, the PLACE study occurred in an area targeted specifically because of occurrence of high-risk behaviors in the vicinity. The facility-based study was conducted at FOSREF youth centers in four areas of PAP, as well as a RH clinic just on the outskirts of Cité Soleil, a densely populated slum. Therefore, the study areas are not entirely comparable.
To conclude, identifying and characterizing high-risk youth is an important first step in improving HIV and unintended pregnancy prevention programs targeting youth. Population-based surveys provide important indicators of prevalence but are less useful for determining appropriate programmatic approaches. Facility-based studies are useful for identifying youth who initiated sex at an early age, have ever been pregnant, have ever experienced an unintended pregnancy and use or do not use condoms to protect against STIs. Facility-based approaches, however, are limited only to those youth who have access to the clinics and often do not include male youth. The PLACE approach is a newer methodology that identifies individuals (youth, in this case) who socialize in high-risk sites that can be targeted for prevention programming. Future studies will need to determine whether interventions that take place in these high-risk sites lead to changes in behaviors and subsequent reductions in HIV transmission and unintended pregnancies. Additionally, data are lacking to determine how well the PLACE method characterizes high-risk sites and if certain types of sites (for example, outdoor or public sites or sites where drug use or other higher risk behaviors take place) are less likely to be mentioned by knowledgeable community informants and thus may be missed in the survey. This will require not only interviewing key informants but also undertaking participatory methods that engage various community members to learn about places where sexual partnerships are formed by youth. As these questions are answered, greater depth on the utility of each approach for studying youth will be gained. Using these methodologies for program design, program improvements, and evaluation will provide insights into how best to prevent HIV transmission and unintended pregnancy and lead to improved health outcomes for youth.
Acknowledgments
This study was supported by the U.S. Agency for International Development (USAID) under cooperative agreement GPO-A-00-03-00003-00 with the MEASURE Evaluation project. The views expressed here are those of the authors and not necessarily those of USAID or the United States government. The authors thank Dr. Kavita Singh and two anonymous reviewers for their helpful insights into the paper. The authors also acknowledge Dr. Heidi Reynolds and Dr. Nancy Murray for their leadership in the design and development of the FOSREF facility-based study, on which Dr. Speizer was a collaborator.
Contributor Information
Ilene S. Speizer, Research Associate Professor in the Department of Maternal and Child Health at the University of North Carolina at Chapel Hill Gillings School of Global Public Health, 206 W. Franklin St., CB 8120, Chapel Hill, NC 27516
Harry Beauvais, Director of Monitoring, Evaluation, and Research at the Fondation pour la Santé Reproductrice et l’Education Familiale (FOSREF), Port-au-Prince, Haiti.
Anu Manchikanti Gómez, Doctoral Candidate in the Department of Maternal and Child Health at the University of North Carolina at Chapel Hill Gillings School of Global Public Health.
Theresa Finn Outlaw, Research Associate at the MEASURE Evaluation project, Carolina Population Center, Chapel Hill, NC.
Barbara Roussel, technical researcher at FOSREF.
References
- Adih William K, Alexander Cheryl S. Determinants of condom use to prevent HIV infection among youth in Ghana. Journal of Adolescent Health. 1999;24(1):63–72. doi: 10.1016/s1054-139x(98)00062-7. [DOI] [PubMed] [Google Scholar]
- Anderson Roy M. Transmission dynamics of sexually transmitted infections. In: Holmes King K, Sparling Frederick P, Mardh Per-Anders, Lemon Stanley M, Stamm Walter E, Piot Peter, Wasserheit Judith N., editors. Sexually transmitted diseases. 3. New York: McGraw Hill; 1999. pp. 25–37. [Google Scholar]
- Bailey Patricia E, Bruno Zenilda V, Bezerra Maria F, Queiros Ivany, Oliveira Cristiana M. Adolescents’ decision-making and attitudes towards abortion in north-east Brazil. Journal of Biosocial Science. 2003;35(1):71–82. doi: 10.1017/s0021932003000713. [DOI] [PubMed] [Google Scholar]
- Boer Henk, Mashamba M Tshilidzi. Gender power imbalance and differential psychosocial correlates of intended condom use among male and female adolescents from Venda, South Africa. British Journal of Health Psychology. 2007;12(1):51–63. doi: 10.1348/135910706X102104. [DOI] [PubMed] [Google Scholar]
- Cayemittes Michel, Placide Marie Florence, Mariko Soumaïla, Barrère Bernard, Sévère Blaise, Alexandre Canez. Enquête mortalité, morbidité et utilisation des services, Haïti, 2005-2006. Calverton, Maryland: Ministère de la Santé Publique et de la Population, Institut Haïtien de l’Enfance and ORC Macro; 2007. [Google Scholar]
- Changalucha John, Grosskurth Heiner, Mwita Wambura, Todd James, Ross David, Mayaud Phillippe, Mahamoud Abdul, Klokke Arnoud, Mosha Frank, Hayes Richard, Mabey David. Comparison of HIV prevalences in community-based and antenatal clinic surveys in rural Mwanza, Tanzania. AIDS. 2002;16(4):661–665. doi: 10.1097/00002030-200203080-00019. [DOI] [PubMed] [Google Scholar]
- Dandona Lalit, Lakshmi Vemu, Sudha Talasila, Kumar G Anil, Dandona Rakhi. A population-based study of human immunodeficiency virus in south India reveals major differences from sentinel surveillance-based estimates. BMC Medicine. 2006 doi: 10.1186/1741-7015-4-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggleston Elizabeth. Use of family planning at first sexual intercourse among young adults in Ecuador. Journal of Biosocial Science. 1998;30(4):501–510. doi: 10.1017/s002193209800501x. [DOI] [PubMed] [Google Scholar]
- Fylkesnes Knut, Ndhlovu Zacchaeus, Kasumba Kelvin, Mubanga Musonda Rosemary, Sichone Moses. Studying dynamics of the HIV epidemic: Population-based data compared with sentinel surveillance in Zambia. Aids. 1998;12(10):1227–1234. doi: 10.1097/00002030-199810000-00015. [DOI] [PubMed] [Google Scholar]
- Geary Cynthia Waszak, Wedderburn Maxine, Mccarraher Donna, Cuthbertson Carmen, Pottinger Audrey. Sexual violence and reproductive health among young people in three communities in Jamaica. Journal of Interpersonal Violence. 2006;21(11):1512–1533. doi: 10.1177/0895904805293487. [DOI] [PubMed] [Google Scholar]
- Gómez Anu M, Speizer Ilene S, Beauvais Harry. Sexual violence and reproductive health among youth in Port-au-Prince, Haiti. Journal of Adolescent Health. doi: 10.1016/j.jadohealth.2008.09.012. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horizons Program, Kenya Project Partners & Uganda Project Partners. HIV voluntary counseling and testing among youth: Results from an exploratory study in Nairobi, Kenya and Kampala and Masaka, Uganda. New York, NY: Population Council; 2001. [Google Scholar]
- Koenig Michael A, Zablotska Iryna, Lutalo Tom, Nalugoda Fred, Wagman Jennifer, Gray Ron. Coerced first intercourse and reproductive health among adolescent women in Rakai, Uganda. International Family Planning Perspectives. 2004;30(4):156–163. doi: 10.1363/3015604. [DOI] [PubMed] [Google Scholar]
- Maharaj Pranitha, Munthree Chantal. Coerced first sexual intercourse and selected reproductive health outcomes among young women in Kwazulu-Natal, South Africa. Journal of Biosocial Science. 2006;39(2):1–14. doi: 10.1017/S0021932006001325. [DOI] [PubMed] [Google Scholar]
- MEASURE Evaluation Project. Priorities for local AIDS control efforts. A manual for implementing the PLACE method. Chapel Hill, NC: MEASURE Evaluation Project, University of North Carolina at Chapel Hill; 2005. [Google Scholar]
- Meyer-Weitz Anna, Reddy Priscilla, Van Den Borne HW, Kok Gerjo, Pietersen Jacques. The determinants of health care seeking behaviour of adolescents attending STD clinics in South Africa. Journal of Adolescence. 2000;23(6):741–752. doi: 10.1006/jado.2000.0356. [DOI] [PubMed] [Google Scholar]
- Murray Nancy, Buek Kathy, Dougherty Leanne, Speizer Ilene, Rosen James, Beauvais Harry, Viala Tania. Insights into young people: Findings from a survey of youth clients of VCT and other reproductive health services at FOSREF clinics in Haiti. Washington, DC: Futures Group; 2005. [Google Scholar]
- Newmann Sarah J, Goldberg Alisa B, Aviles Rodolfo, Molina De Perez Olga, Foster-Rosales Anne F. Predictors of contraception knowledge and use among postpartum adolescents in El Salvador. American Journal of Obstetrics and Gynecology. 2005;192(5):1391–1394. doi: 10.1016/j.ajog.2004.12.077. [DOI] [PubMed] [Google Scholar]
- ORC Macro. n.d. [Feb. 20, 2008];Demographic and Health Survey Statcompiler. [Online]. Available from: http://www.statcompiler.com.
- Prata Ndola, Morris Leo, Mazive Elizio, Vahidnia Farnaz, Stehr Mark. Relationship between HIV risk perception and condom use: Evidence from a population-based survey in Mozambique. International Family Planning Perspectives. 2006;32(4):192–200. doi: 10.1363/3219206. [DOI] [PubMed] [Google Scholar]
- Reynolds Heidi W, Kimani Joshua. Services for prevention of mother-to-child transmission (PMTCT). YouthNet Brief No 12. Arlington, VA: Family Health International; 2006. [Google Scholar]
- Speizer Ilene, Finn Theresa, Manchikanti Anu, Beauvais Harry, Roussel Barbara. Risk-taking behaviors among youth socializing in target venues of Carrefour, Haiti: Adaptation of the priorities for local AIDS control efforts (PLACE) methodology. Chapel Hill, NC: MEASURE Evaluation, Carolina Population Center, University of North Carolina at Chapel Hill; 2007. [Google Scholar]
- Tate Jackie, Singh Kavita, Ndubani Phillimon, Kamwanga Jolly, Buckner Bates. A comparison of the PLACE method and a household survey in Zambia. Chapel Hill, NC: MEASURE Evaluation, Carolina Population Center, University of North Carolina at Chapel Hill; 2007. [Google Scholar]
- Thurman Tonya, Brown Lisanne, Richter Linda, Maharaj Pranitha, Magnani Robert. Sexual risk behavior among South African adolescents: Is orphan status a factor? Aids and Behavior. 2006;10(6):627–635. doi: 10.1007/s10461-006-9104-8. [DOI] [PubMed] [Google Scholar]
- Varga CA. Sexual decision-making and negotiation in the midst of AIDS: Youth in Kwazulu-Natal, South Africa. Health Transition Review. 1997;7(S3):45–67. [Google Scholar]
- Voeten Hélène ACM, Egesah Omar B, Habbema J Dik F. Sexual behavior is more risky in rural than in urban areas among young women in Nyanza province, Kenya. Sexually Transmitted Diseases. 2004;31(8):481–487. doi: 10.1097/01.olq.0000135989.14131.9d. [DOI] [PubMed] [Google Scholar]
- Weir SS, Figueroa JP, Byfield L, Hall A, Cummings S, Suchindran C. Randomized controlled trial to investigate impact of site-based safer sex programmes in Kingston, Jamaica: Trial design, methods and baseline findings. Trop Med Int Health. 2008;13(6):801–813. doi: 10.1111/j.1365-3156.2008.02057.x. [DOI] [PubMed] [Google Scholar]
- Weir SS, Tate JE, Zhusupov B, Boerma JT. Where the action is: Monitoring local trends in sexual behaviour. Sexually Transmitted Infections. 2004;80(Suppl 2):ii63–68. doi: 10.1136/sti.2004.012336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir Sharon S, Pailman Charmaine, Mahlalela Xoli, Coetzee Nicol, Meidany Farshid, Boerma J Ties. From people to places: Focusing AIDS prevention efforts where it matters most. AIDS. 2003;17(6):895–903. doi: 10.1097/01.aids.0000050809.06065.e0. [DOI] [PubMed] [Google Scholar]


