Short abstract
This article explores the burden of the major non-communicable diseases in South Asia and the extent to which obstacles hinder prevention and management of these diseases
The World Health Organization (WHO) stated in 2002 that “in many regions, some of the most formidable enemies of health are joining forces with the allies of poverty to impose a double burden of disease, disability and premature death in many millions of people.”1 This is what is happening in South Asia, which has one quarter of the global population but where about half the population lives below the poverty line and has limited access to health care. Although infectious diseases remain a formidable enemy, the population is ageing and non-communicable diseases are rising.2-4 South Asia has made fair economic progress in recent decades but is struggling to find a road towards sustainable development.
We review here the estimated burden of noncommunicable diseases in South Asia, the risk factors for these diseases, the limitations of the available data, and the attempts being made to gather evidence of better quality. We aim to provide a profile of non-communicable disease burdens in this region.
Sources and selection criteria
We conducted a systematic search on Medline; used reports from WHO and other international organisations; and communicated with experts in the field. Although non-communicable diseases have been variously defined, we propose to limit the term to four major disease categories that are linked by common risk factors: cardiovascular diseases, diabetes mellitus, cancers, and chronic obstructive pulmonary disease. Dietary consumption patterns, physical inactivity, tobacco use, and environmental pollution are among the common risk factors shared by these disorders, providing common pathways of epidemiological transition as well as public health action.
Estimating the burden of non-communicable diseases
Validated nationally representative estimates of cause specific mortality are not available for any country in South Asia. The available data are based on combinations of different datasets. In India, for example, deaths are registered as a part of “medical certification of cause of death” (registration of hospital deaths) and “survey of cause of death” (a rural based registry). Other countries in the region provide mostly hospital based mortality data for assignment of cause of death. Population based estimates of mortality from non-communicable diseases are therefore difficult to produce: the urban data are based on inadequate death certification, and the rural data are limited by the inaccuracies in record keeping and partial coverage of health information systems.
Summary points
Mortality, morbidity, and disability attributable to the major non-communicable diseases account for about 60% of all deaths and 47% of the global burden of disease; these rates are expected to rise
Almost half of the adult disease burden in South Asia is attributable to non-communicable diseases
Environmental factors are the major determinants of almost all non-communicable diseases
Obstacles to managing the non-communicable diseases epidemic in South Asia include sedentary lifestyles, extreme poverty, and inadequate health systems
Establishment of surveillance systems for noncommunicable diseases and their risk factors is essential for developing prevention strategies and monitoring the impact of control programmes. Pilot programmes are now under way in some of the countries to establish and evaluate such systems.
According to national reports gathered by WHO's South East Asia regional office, of the total deaths in South Asia, the proportion attributable to selected non-communicable diseases ranged from about 7% in Nepal to 40% in the Maldives in 1998.2 Table 1 shows data for 2000.
Table 1.
| India | Sri Lanka† | Sub-Saharan Africa | China | |
|---|---|---|---|---|
| Cardiovascular disease |
31.7 |
20.1 |
11.2 |
32.1 |
| Diabetes mellitus |
1.1 |
1.5 |
0.3 |
0.6 |
| Cancer |
7.4 |
5.6 |
6.2 |
20.5 |
| Chronic obstructive pulmonary disease and asthma | 2.5 | 1.6 | 1.9 | 17.8 |
For 1998.
Cardiovascular diseases
Cardiovascular diseases are major and growing contributors to mortality and disability in South Asia.3,5 Studies conducted in South Asian migrants show they have higher coronary mortality than the reference population of their adopted countries and an earlier onset of disease linked to abnormalities of glucose homoeostasis.6 The cardiovascular disease profile in the region shows the presence of emerging and advancing diseases (such as coronary heart disease and stroke) and established but receding diseases (such as rheumatic heart disease and hypertension (which is also a risk factor for stroke and coronary heart disease)).
Box 1: Non-communicable diseases in South Asia
India has a higher number of people with diabetes than any other country in the world
Pakistan is among the top 10 world nations for high numbers of people with diabetes
A third of Pakistanis aged more than 45 years have hypertension
In India 52% of cardiovascular deaths occur below the age of 70, compared with 23% in countries with established market economies
In the Maldives, non-communicable diseases account for 48% of all deaths and stroke accounts for 11% of non-communicable diseases deaths
Deaths from coronary heart disease in India rose from 1.17 million in 1990 to 1.59 million in 2000 and are expected to rise to 2.03 million in 2010. Prevalence varies by site, age group studied, and diagnostic criteria used, but an urban prevalence of about 10% in urban adults aged ≥ 35 years is a credible estimate based on several surveys.4 A 1994 study found that prevalence of coronary heart disease in Sri Lankan men aged 35-59 years was 1.6%—on the basis of electrocardiographic and questionnaire criteria; prevalence estimates based on history alone were 1.9% in higher and 0.6% in lower socioeconomic status groups in an urban population.7
Stroke is a major cause of mortality and also amounts to a large proportion of DALYs (disability adjusted life years) lost. Rheumatic heart disease continues to be an important problem in the region, though there are indicators of a recent decline in some of the countries.8-11
Hypertension has been widely studied in community surveys, though nationally representative estimates are available only in a few countries. The prevalence of hypertension in adults was estimated to be 23% and 18% in urban and rural areas respectively in the national health survey of Pakistan, conducted during 1990-4.12 Hypertension was positively associated with higher socioeconomic status in both urban and rural areas. In adults in Sri Lanka the prevalence of hypertension was estimated to be 17% in urban and 8% in rural areas.1 Several studies across India also report a higher prevalence in adults in urban compared with rural areas (20-40% v 12-17%).13-15
Several surveys of risk factors conducted across South Asian countries have shown high and rising rates of overweight, central obesity, diabetes, high blood pressure, and dyslipidaemia in urban populations.12,13,16 Such trends also exist in rural populations but are lower in magnitude and less steep in the slope of change. Although inflammation may play a role in accelerated atherogenesis, specific evidence linking that process to the early onset of coronary heart disease in South Asians is not yet available.
The socioeconomic gradient in cardiovascular diseases and related risk factor distributions among population groups are also changing. Tobacco consumption is now universally more common among the lower socioeconomic groups. Other risk factors are beginning to show a reversal in some populations—for example, hypertension is now more common in poorer groups in Chennai, India, and diabetes is emerging as an important disease in the urban slums of Delhi.
As the epidemics advance and mature, the risk of cardiovascular diseases will affect all sections of society, with the poor most likely to develop the diseases. Recent studies from India show that individuals with lower levels of income or education are at higher risk of coronary heart disease, suggesting that for some population groups in South Asia, prevalence is following the pattern seen with advanced epidemics in developed countries—the highest prevalence is shifting from the more affluent to the less affluent.17,18
Diabetes mellitus
The prevalence of diabetes and its adverse health effects has risen more rapidly in South Asia than in any other large region of the world. India has a higher number of people with diabetes than any other country, with estimates ranging from 19.4 million in 199519 to 32.7 million in 2000.20
In Bangladesh, the prevalence of diabetes in urban areas is double that in rural areas (8% v 4%) and rises with affluence.21 The International Diabetes Federation gives an estimate of 12% prevalence in Pakistan, with a total of 8.8 million people with diabetes in 2000.20 In Sri Lanka the 1999 census report records diabetes prevalence as 8% in rural areas and 12% in urban areas22; equivalent current rates for Nepal have been reported as 3% and 15% respectively.23
Projections for 2020, based on modelled estimates by WHO, show a marked escalation of diabetes related burden in South Asia.3 The number of people with diabetes is expected to rise by 195% in India during 1995-2025 to reach 57.2 million in 2025.19 Pakistan is expected to have about 14.5 million people with diabetes by that year (table 2).
Table 2.
Prevalence of diabetes in South Asia, 2000 and 2025 (projected in 1998).19 Values are percentages (number of people with diabetes, 000s)
| Country | 2000 | 2025 |
|---|---|---|
| Bangladesh |
2.2 (1 564) |
3.1 (4 032) |
| Bhutan |
2.1 (19) |
2.3 (39) |
| India |
4.0 (22 878) |
6.0 (57 243) |
| Maldives |
2.5 (3.2) |
3.0 (9.2) |
| Nepal |
2.2 (263) |
2.6 (638) |
| Pakistan |
7.1 (5 310) |
8.7 (14 523) |
| Sri Lanka | 2.6 (318) | 3.5 (617) |
These figures are likely to be higher if current diagnostic criteria are used for diagnosis. South Asians have been observed to have a high risk of developing diabetes at lower levels of body mass index than Western populations.24
Cancer
Cancer is regarded as one of the major noncommunicable diseases affecting South Asia, accounting for a large proportion of the DALYs lost in this area.3 Estimates of age standardised rates in this region range from 99.0 to 129.6 per 100 000 in males and 104.4 to 154.3 per 100 000 in females.25 The most common cancers in males are of lung and oropharynx and in females are of the cervix, uterus, and breast.25,26
Chronic respiratory diseases
Chronic obstructive airway diseases (emphysema and chronic bronchitis) and asthma, resulting from indoor and outdoor air pollution, account for a large proportion of the burden of chronic respiratory diseases.27,28 Morbidity from respiratory diseases accounts for 65 million cases and about 580 000 deaths in India.29
Features of non-communicable diseases in South Asia
Although the non-communicable diseases epidemic in South Asia is essentially following the course of similar epidemics in other developing countries, some features characterise non-communicable diseases in this region. Recent studies suggest that the metabolic syndrome is indeed very common in urban Indians.15,30 The high prevalence of glucose intolerance and the distinctive dyslipidaemic pattern of reduced concentrations of high density lipoprotein (HDL) cholesterol and high concentrations of triglycerides characterise the metabolic profile, and abdominal obesity characterises the phenotype of the urban adult in India. This is also likely to be the pattern in Pakistan, Bangladesh, and Sri Lanka, where more population surveys are needed to profile the South Asian propensity for the metabolic syndrome. The low levels of HDL cholesterol result in dangerously high ratios of total cholesterol to HDL cholesterol, even at concentrations of total cholesterol that would be considered acceptable in Western populations. Cross sectional studies in India show that total to HDL cholesterol ratios of > 4.5 exist in 73% of urban men and 54% of urban women and in 52% of both rural men and rural women; these men and women have total cholesterol values in the range of 4.7 mmol/l to 5.2 mmol/l (K S Reddy et al, unpublished data).
Box 2: Current research in non-communicable diseases in South Asia
Evaluation of health systems interventions for vascular risk reduction in primary healthcare settings in developing countries (conducted by the Initiative for Cardiovascular Health Research in the Developing Countries (IC-Health), New Delhi)
Lady health worker heart health project (conducted by Heartfile, a leading national non-governmental organisation in Pakistan)
Reorientation of health services to manage non-communicable diseases (conducted by Heartfile, Pakistan)
Risk factor surveillance programmes under WHO's STEPS programme (a graded approach to surveillance of non-communicable diseases, developed and implemented by WHO)
Global programme for assessing coronary risk factors (conducted in 41 countries by INTERHEART, a case-control study of risk factors for myocardial infarction)
Box 3: Additional educational resources
Articles
Jabbour S, Nishtar S, Prabhakaran D, Chockalingam A, Achutti A, Agrawal A, et al. Information and communication technology in cardiovascular disease prevention in developing countries: hype and hope.
Report of the International Collaboration on Information Use in Cardiovascular Health Promotion in Developing Countries. Int J Cardiol 2003;92: 105-1114659841
Nishtar S, Wierzbicki AS, Lumb PJ, Lambert-Hammill M, Turner CN, Crook MA, et al. Waist-hip ratio and low HDL predict the risk of coronary artery disease in Pakistanis. Curr Med Res Opin 2004;20: 55-62
Websites (research)
www.ichealth.org—Initiative for Cardiovascular Health Research in the Developing Countries (see box 2)
www.heartfile.org/nap.htm—a coalition of Pakistan's health ministry, WHO, and Heartfile to prevent and control non-communicable diseases in Pakistan
Websites (general)
www.worldheart.org—World Heart Federation
www.who.int/ncd—World Health Organization
www.ktl.fi/monica/public/mdc—MONICA study (international study to monitor trends in and determinants of cardiovascular disease)
www.health.gov/healthypeople—The healthy people 2010 (a US government initiative on health promotion and disease prevention)
Impaired fetal nutrition, resulting in low birth weight, may be another vascular risk factor relevant to South Asia 31,32 Indeed, it has been implicated in the causation of metabolic syndrome and diabetes, as well as in the mediation of vascular risk through other risk factors, such as high blood pressure.33 The association may have especially profound effects on the incidence of diabetes and cardiovascular diseases in South Asia, where maternal and fetal malnutrition are common.
With respect to cancers, the high rates of tobacco consumption as well as the diversity of tobacco products available influence the profile of common cancers. Lung cancer is common, as are oropharyngeal cancers, which are linked to tobacco chewing, a distinctive South Asian habit. Cancer of the cervix is common, especially among poorer women, and is associated with many factors.
Indoor air pollution contributes to chronic obstructive airway disease in South Asia, where poorer people burn wood fuel in their homes. It is a major contributor to the disease in regions such as Nepal and rural India and Pakistan. Burning wood fuel in the home is likely to increase the burden of this disease, especially in winter.
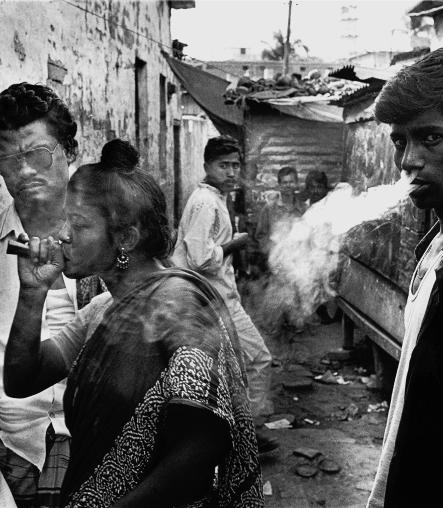
Figure 1.
Smokers in Bangladesh
Credit: SHEHZAD NOORANI/PANOS
South Asia is also experiencing urbanisation, with widening income and social inequities. The impact of non-communicable diseases on the rich and the poor are likely to be different, in terms of both the principal causes and the manifestations. The rich, for example, are likely to be more inactive, and the poor will consume fewer fruit and vegetables. As the rich are likely to recognise their risk earlier and seek medical attention, they will develop chronic but manageable disease; as the poor are likely to be less aware of their risk and less able to access medical care, they will develop rapidly progressive disease with early and sudden fatal outcomes. The challenge to public health is to anticipate and avert an epidemic of noncommunicable diseases.
Conclusions
The health burdens of non-communicable diseases are high in South Asia, though there are differences among countries and within urban and rural areas of each country, depending on the level of developmental and epidemiological transition. Many of these disease burdens occur in the productive mid-life period and will, therefore, adversely affect workforce productivity and economic development. Although the absence of well established disease surveillance mechanisms prevents precise estimation of the size of noncommunicable disease burdens, the direction of change is clear—the burden is rising. More accurate estimation of these burdens, their risk factors, and time trends would help to better inform policy and to monitor change in response to public health interventions. Even at the current state of knowledge, however, the magnitude of the problem is large enough to demand urgent attention and action.
Editorial by Basnyat and Rajapaksa
Contributors: AG and KSR conceptualised and developed the idea and wrote the article. MS carried out the literature search and reviewed the article. AG is guarantor for the article.
Funding: None.
Competing interests: None declared.
References
- 1.World Health Organization. The world health report 2002. Reducing risks, promoting healthy life. Geneva:WHO, 2002. [DOI] [PubMed]
- 2.World Health Organization. Noncommunicable diseases in South-East Asia region. A profile. New Delhi: WHO, 2002.
- 3.Murray CJL, Lopez AD, eds. Global burden of disease. Harvard, MA: Harvard School of Public Health, 1996. (Vol 1 of Global Burden of Disease and Injury series.)
- 4.World Health Organization. Health situation in the South-East Asia region 1998-2000. New Delhi: WHO, 2002.
- 5.Nishtar S. Prevention of coronary heart disease in south Asia. Lancet 2002;360: 1015-8. [DOI] [PubMed] [Google Scholar]
- 6.McKeigue PM, Ferrie JE, Pierpont T, Marmot MG. Association of early-onset coronary heart disease in South Asian men with glucose intolerance and hyperinsulinemia. Circulation 1993;87: 152-61. [DOI] [PubMed] [Google Scholar]
- 7.Mendis S, Ekanayake EM. Prevalence of coronary heart disease and cardiovascular risk factors in middle aged males in a defined population in central Sri Lanka. Int J Cardiol 1994;46: 135-42. [DOI] [PubMed] [Google Scholar]
- 8.Indian Council of Medical Research. Community control of rheumatic fever and rheumatic heart disease. Delhi: ICMR, 1994.
- 9.Jose VJ, Gomathi M. Declining prevalence of rheumatic heart disease in rural school children in India: 2001-2002. Indian Heart J 2003;55: 158-60. [PubMed] [Google Scholar]
- 10.Lalchandani A, Kumar HRP, Alam SM. Prevalence of rheumatic fever and rheumatic heart disease in rural and urban school children of district Kanpur. Indian Heart J 2000;52: 672. [Google Scholar]
- 11.Krishnaswami S, Joseph G, Richard J. Demands on tertiary care for cardiovascular diseases in India: analysis of data for 1960-89. Bull World Health Organ 1991;69: 325-30. [PMC free article] [PubMed] [Google Scholar]
- 12.Jafar TH, Levey AS, Jafary FH, White F, Gul A, Rahbar MH, et al. Ethnic subgroup differences in hypertension in Pakistan. J Hypertens 2003;21: 905-12. [DOI] [PubMed] [Google Scholar]
- 13.Singh RB, Bajaj S, Niaz MA, Rastogi SS, Moshiri M. Prevalence of type 2 diabetes mellitus and risk of hypertension and coronary artery disease in rural and urban population with low rates of obesity. Int J Cardiol 1998;66: 65-72. [DOI] [PubMed] [Google Scholar]
- 14.Reddy NK, Kumar DN, Rayudu NV, Sastry BK, Raju BS. Prevalence of risk factors for coronary atherosclerosis in a cross-sectional population of Andhra Pradesh. Indian Heart J 2002;54: 697-701. [PubMed] [Google Scholar]
- 15.Gupta R, Gupta VP, Sarna M, Bhatnagar S, Thanvi J, Sharma V, et al. Prevalence of coronary heart disease and risk factors in an urban Indian population: Jaipur Heart Watch-2. Indian Heart J 2002;54: 59-66. [PubMed] [Google Scholar]
- 16.Sayeed MA, Mahtab H, Akter Khanam P, Abdul Latif Z, Keramat Ali SM, Banu A, et al. Diabetes and impaired fasting glycemia in a rural population of Bangladesh. Diabetes Care 2003;26: 1034-9. [DOI] [PubMed] [Google Scholar]
- 17.Gupta R, Gupta VP. Meta-analysis of coronary heart disease prevalence in India. Indian Heart J 1996;48: 241-5. [PubMed] [Google Scholar]
- 18.Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al. High prevalence of diabetes and impaired glucose intolerance in India: national urban diabetes survey. Diabetologia 2001;44: 1094-101. [DOI] [PubMed] [Google Scholar]
- 19.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care 1998;21: 1414-31. [DOI] [PubMed] [Google Scholar]
- 20.International Diabetes Federation. Diabetes atlas 2000. Brussels: IDF, 2000.
- 21.Abu Sayeed M, Ali L, Hussain MZ, Rumi MA, Banu A, Azad Khan AK. Effect of socioeconomic risk factors in prevalence of diabetes between rural and urban populations in Bangladesh. Diabetes Care 1997;20: 551-5. [DOI] [PubMed] [Google Scholar]
- 22.Diabetes Association of Sri Lanka. 1999 Problem census report of Sri Lanka. (Questionnaire proforma of International Diabetes Federation's South East Asia region for the mid-term regional meeting, 26 March 1999.)
- 23.Singh DL, Bhattarai MD. High prevalence of diabetes and impaired fasting glycaemia in urban Nepal [letter]. Diabet Med 2003;20: 170-1. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363: 157-63. [DOI] [PubMed] [Google Scholar]
- 25.Ferlay J, Bray F, Pisani P, Parkin DM. GLOBOCAN 2000: Cancer incidence, mortality and prevalence worldwide. Version 1.0. Lyons: IARC Press, 2001. (IARC Cancer base No 5.)
- 26.National Cancer Registry Programme. Consolidated report of the population based cancer registries 1990-1996. Incidence and distribution of cancer. New Delhi: Indian Council of Medical Research, 2001.
- 27.Mishra V. Effects of indoor air pollution from biomass combustion on prevalence of asthma in the elderly. Environ Health Perspect 2003;111: 71-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Melsom T, Brinch L, Hessen JO, Schei MA, Kolstrup N, Jacobsen BK, et al. Asthma and indoor environment in Nepal. Thorax 2001;56: 477-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jindal SK, Aggarwal AN, Gupta D. A review of population studies from India to estimate national burden of chronic obstructive pulmonary disease and its association with smoking. Indian J Chest Dis Allied Sci 2001;43: 139-47. [PubMed] [Google Scholar]
- 30.Ramachandran A, Snehalatha C, Satyavani K, Sivasankari S, Vijay V. Metabolic syndrome in urban Asian Indian adults—a population study using modified ATP III criteria. Diabetes Res Clin Pract 2003;60: 199-204. [DOI] [PubMed] [Google Scholar]
- 31.Barker DJP. Fetal origins of coronary heart disease. BMJ 1995;311: 171-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stein CE, Fall CHD, Kumaran K, Osmond C, Cox V, Barker DJP. Fetal growth and coronary heart disease in South India. Lancet 1996;348: 1269-73. [DOI] [PubMed] [Google Scholar]
- 33.Yajnik CS. The insulin resistance epidemic in India: fetal origins, later lifestyle, or both? Nutr Rev 2001;59: 1-9. [DOI] [PubMed] [Google Scholar]