Short abstract
Most South Asian governments have concentrated on emulating a Western style of healthcare service, with the result that an elite few are overmedicalised whereas the majority are neglected. However, community participation in the development of local health services could provide a solution
Despite a remarkable improvement during recent decades in many countries' overall health and nutrition statistics and macro-economic indicators,1 some 10.8 million children aged under 5 years still die annually worldwide, of which 34% occur in South Asia alone.2 It is too simplistic to relate improvements in economic indicators with better health because this does not take account of inequality, change in focus of public health priorities, and, most importantly, the involvement of the community in improving health. This article discusses some of the most prominent examples in South Asia of involvement of the community in planning, managing, and evaluating health projects. However, showing a direct relation between community development and improved health remains a challenge.
Community development and health: where is the link?
Community development is becoming one of the most popular subjects in the context of public health interventions. Although an accurate definition of community development is problematic, a reasonable description would be the empowerment of a community to obtain self reliance and control over the factors that affect their health. Unfortunately, South Asia, so richly endowed with natural and human resources, has suffered for centuries from poverty and consequent ill health. It has, however, a rich heritage of community initiatives such as the establishment of education facilities, religious institutions, and orphanages and the construction of roads. It is unfortunate that health has remained the responsibility of governments, outside agencies, and, of course, the private sector (both formal and informal) and the provision of medical services has become big business.3
Most of the public and private health services in South Asia have concentrated on establishing large hospitals and organisations that have been able to cater to only a small privileged fraction of the population. In recent years, however, development organisations have taken on projects to promote community participation in rural areas to enhance health development.
Evolution of community based healthcare system
From the late 1940s, South Asia enjoyed a short spell of rapid improvement in health status (albeit from a low baseline, and mainly through reducing malaria, smallpox, cholera, and plague) and a modest improvement in the socioeconomic situation. This was due to strong political systems, which mobilised the vast latent human resource that was liberated during the struggle for independence. Unfortunately, later generations of leaders increasingly have promoted a Western style of health services based on personalised curative treatment administered by doctors and hospitals regardless of the entirely different disease pattern and socioeconomic conditions of most people.4 This has been supported and vigorously promoted by the market oriented pharmaceutical and medical instrumentation industries, together with health insurance to combat the exponential rise in cost of such medical care. As a consequence, the rich are dangerously over medicalised, the middle class are impoverished when they fall ill, while the rural and urban poor, who make up 85% of the population, are neglected.
As early as the 1970s, several doctors were disturbed by this trend, which not only distorted the values of the medical profession but was converting health into a marketable commodity in human suffering. They realised their inability to stem these forces by merely pleading the cause of the marginalised masses with government or other agencies with their narrow vertical programmes operated through the same infrastructure. This led to the emergence of many independent institutions and organisations, chiefly under the leadership of motivated doctors and even non-medical individuals, operating in both rural and urban areas.
Since then, several community based approaches to health care have been suggested and implemented. One of these has been involving the community in development, management, and ownership of community based healthcare systems. This entails training local people, building awareness, and providing health education to reduce communities' dependence on the private and public health sectors. Moreover, this follows an integrated concept of health, which goes beyond the mere curative aspect and encompasses both preventive and promotive dimensions. Different models of community based health care can be identified:
Integrated and comprehensive models—This involves combining training of local volunteers with health education and rural development health activities emphasising self help and use of local resources5-7
Training—This merely involves training of local health volunteers, who then assume responsibility for delivering certain aspects of basic health care8,9
Health education campaigns—These are usually based on single health issues and attempt to raise awareness about certain national programmes such as immunisation, AIDS, etc10
Development of community financing for local health programmes—This aims to raise financial resources from within the community to support existing healthcare activities.11,12
Community participation versus community involvement in health
Since Alma Ata has defined community participation as one of the pillars of primary health care, most governments and non-governmental organisations have included it in their primary health care programmes. However, ensuring community participation in the true sense remains a challenge, as merely inviting community members to participate in programmes introduced by outsiders does not take account of the complexity of community psychology, culture, and other social issues. In a recent global review some of the projects from South Asian countries scored highly in terms of community involvement in various phases of project evolution such as initiation, needs assessment, defining, planning and implementing actions, monitoring and evaluation, and resource mobilisation.13 Boxes 1-3 briefly describe examples from Bangladesh, India, and Pakistan, which have the major share of the population of this region.3,13,14
Bangladesh—Examples of community participation include national house to house education efforts by BRAC, one of the largest national non-governmental organisations in the country, with its unsalaried community health workers called Shastho Shebikas (25 140 covering the population of 35 million) teaching every woman how to prepare oral rehydration solution to treat diarrhoea; the efforts of World Vision/Bangladesh with community partners; the Local Initiative Programme and the Jiggasha approach, with community collaborators; and the work of the International Center for Diarrhoeal Disease Research, Bangladesh (ICDDR,B) to empower a community (Chakaria Community Health Project) to take full control of its health through the self help initiatives.13,15 Gonoshashthya Kendra is a remarkable experiment near Dhaka, where a surgeon returned from training in Britain to participate in the struggle for national independence. He started by training village health workers with a small supporting hospital in Savar but now provides employment to divorced Muslim women in the campus. Gonoshashthya Kendra has established a community based medical college in Dhaka and is extending its activities to provide health care to a population of a million in needy regions of the country.
Box 1: Chakaria Community Health Project, Bangladesh3
In 1994 the International Center for Diarrhoeal Disease Research, Bangladesh launched the Chakaria Community Health Project in Chakaria, a rural village in Cox's Bazar district. The main objective was to establish a strategy to ensure community participation in health matters and to improve health issues in the area over two years. It was also hoped that such a system would motivate the community to become self reliant. The project adopted the following strategies in implementing its activities:
Operating through local village based organisations, it promoted health issues on their agendas and encouraged preventive measures
It provided technical assistance in health matters and organisational development but encouraged the use of existing health facilities
It developed participatory methods in every aspect of project implementation so that the community took up a leadership role and remained in control.
Four years after implementation, it had achieved the following:
Health orientation sessions were launched in educational institutions, mosques, madrasas (religious schools), female gatherings, and through home visits
Male community health workers disseminated sermons on health issues during Friday prayers
Seven village health posts were established where senior house officers managed health services
33% of families had subscribed to a health card, which provided them with access to subsidised basic health care, and immunisation rates had improved by 52% (compared with 15% in comparison areas)
Box 2: Comprehensive Rural Health Project, Jamkhed, India13
The Comprehensive Rural Health Project was established in Jamkhed in 1971 by an Indian couple with a background in surgery. Their main objective was to provide health services and facilities to the poorest rural villages. Activities revolved around health and family planning and development procedures through:
Offering curative services
Mobilisation of the community by the community health volunteers
Breaking down stereotypes between in the different castes.
There was an instant response from the community, which eventually led to the establishment of the Farmers' Club and a women's organisation called the Mahila Mandal. While the community health volunteers were providing both preventive and curative services, the Farmers' Club and Mahila Mandal began to disseminate health messages as soon as they had the confidence of community. They also advocated smaller families, good hygiene, and less superstition in order to augment health development in the community.
The project's major achievements were the reduction in chronic diseases such as leprosy, tuberculosis, and malaria and a marked decline in infant mortality to less than 40/1000 live births (compared with a state average of 110). The project also improved the position of women in society, removed certain boundaries within the caste system, and helped in the establishment and organisation of village based institutions, pointing the villagers to a future of self reliance and prosperity
Box 3: HANDS-AKF project on NGO-community partnership14
Health and Nutrition Development Society (HANDS) launched a project in Talukha Hala district in Hyderabad, called “reducing maternal mortality through NGO community partnership during 1999 to 2001.” The society worked directly in 30 villages and indirectly in another 12, covering a total population of 36 000. The main objectives of the project were to mobilise and create a partnership of communication and understanding between the female and male populations of the selected communities and to recruit and train community midwives in order to reduce maternal mortality. The procedure took place through:
Training local healthcare workers and community midwives and community health attendants thorough institution based (168 days) and community based (120 days) hands-on training
Establishing community based organisations and institutions
Providing preventive and curative health services
Providing proper reproductive health care and reducing maternal and infant morbidity and mortality.
The society, with the collaboration of the Taluka Hospital, provided a team of highly trained doctors along with locally trained community health workers. The main achievements of the project were a 24% increase in the proportion of women at child bearing age who received tetanus vaccination, 21% increase in contraceptive use, 0.4% increase in deliveries managed at health facilities, a 20% increase in the number of children aged under 3 years with normal nutritional status, a reduction in child mortality from 167 per1000 live births in 1997 to 35 in 2002.
India—Since the 1960s Mabelle and Rajanikant Arole have built up a truly comprehensive development in Jamkhed, a drought prone area in western Maharashtra, that serves a population of almost 250 000 and covers many aspects of rural development.7 The emphasis is on women's empowerment together with other activities such as farmers' clubs and a health service that includes well equipped hospitals. Rani and Abhay Bang started at Gadchiroli with a government district hospital and later covered a large forested tribal area in central India.16 In 400 villages they have markedly reduced infant deaths by training illiterate women. Ragini Prem, a former professor of medicine at Osmania University, and her husband achieved remarkable social and economic transformation of a very backward and neglected community in northern India at Banwasi Sewa Ashram.17 They trained local village health workers, who now perform most of the functions of a qualified doctor and live within the communities they serve, which otherwise would have no access to medical care. The Child in Need Institution under the leadership of Dr Chowdhary has improved paediatric care over a large area of West Bengal, including a well equipped hospital in Kolkata.18
Pakistan lacks examples of operations by nongovernmental organisations at the national scale, but for almost two decades Pakistani non-government organisations such as HANDS (Health And Nutrition Development Society, Pakistan) and the Aga Khan Foundation have worked on a partnership with local communities in rural Pakistan.14 Their aim is to seek sustainable ways of financing and delivering basic health care to remote areas.
Community health workers: a bridge between community and health professionals
In most cases, projects with strong community participation have suffered from constraints of time and resources. The model that has been replicated in almost all the countries is the introduction of community health workers to provide local primary health care services. Unicef Regional Office for South Asia has recently reviewed the different models of community health workers in South Asian countries and concluded that no model is perfect.19 So, each country has adopted models based on their strength and weakness in the local context.
Bangladesh is close to achieving complete national coverage by community health workers; 21 000 health assistants and 23 500 family welfare assistants provide family planning and limited primary healthcare services to communities.20 There is no one standard model of community programme forced by the government but rather a proliferation, most with a firm base in the community.
Bhutan—The Ministry of Health initiated the village health worker programme in 1979 with the basic philosophy of establishing a link between communities and health services. The concept of primary health care is disseminated to the community through this group of volunteers; their work includes improving basic hygiene and sanitation, promotiing vaccination, and encouraging other preventive and basic aspects of health.21
India—The greatest catalyst in improving public health was the establishment and work of community health workers. The scheme was initiated in 1977, and later the workers' name changed to community health volunteers in 1980 and village health guides in 1981.19 From 2000 until April 2002, about 323 000 village health guides were working throughout India under a government sponsored scheme.22
Nepal—The government launched it's first national community health volunteer programme in 1970. During the past three decades, the volunteer programme has evolved and expanded into the current national female community health volunteer programme, with more than 48 550 trained volunteers in all 75 districts of the country.19 Community members consider traditional birth attendants, female ward members, functional users group, and committee members to be volunteers.19
Pakistan—The government (Ministry of Health) employs about 70 000 female health workers to provide family planning and primary healthcare services to Pakistani women and children, each worker covering about 150-200 households or roughly 1000 people.23
Sri Lanka—Although the history of volunteers in health goes back to 1915, the main growth of the volunteer programme was from the mid-70s. The largest trainer of volunteers within the government, however, is the Health Education Bureau, part of the Public Health Division of the Ministry of Health. From 1976 onwards, the Health Education Bureau developed its volunteers.24 Opinions differ on the current number of volunteers working regularly, with a conservative estimate being 15 000.
Effect of development on health: where is the evidence?
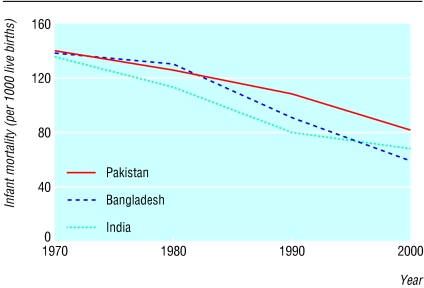
Although it is possible to show the impact of community development on health at the level of a project or intervention (as with the Chakaria Community Health Project, Comprehensive Rural Health Project, Jamkhed, etc), it is difficult to establish such an impact at the national level. Since the evolution of community development projects in South Asia, the national data show a drastic improvement not only in infant mortality (see figure) but also in other health development indicators.1 The success of public health interventions is thought to be due also to the shift in focus from a hospital based system towards a community based primary healthcare system during the past few decades. In these years, of research and project implementation, one can observe a myriad factors that may have played a role in improving health, but the challenge remains to find the definite answers regarding the share between interventions and the process of implementation (influence of community empowerment or development) in improving the health of communities and at what level and scale.
Figure 1.
Changes in infant mortality in Bangladesh, India, and Pakistan during the past 30 years
Summary points
Since the 1940s, South Asian governments have concentrated on designing Western style health services, which have benefited few people
Since the 1970s, realisation of shortcomings in the Western healthcare model has led to greater emphasis placed on primary health care, and most countries have shown improvement in health indicators
Community participation has been the pillar of primary health care since the Alma Ata declaration, but few examples of true participation by local community members can be found
Various community development models exist in different countries, but the introduction of community based health workers is common in almost all south Asian countries
Community development has coincided with improvements in health indicators in recent decades, but a causal link has been established in only a few small scale projects and remains to be shown at the national scale
We gratefully acknowledge the contribution of Farzana Bilkes of CARE Bangladesh, S M Hanifi of ICDDR,B, Bangladesh; Dr Tanveer Ahmed of HANDS, Pakistan; and N H Antia and Purva Abhyankar of the Foundation for Research on Community Health, India, for their generous support in providing useful information and documents to write this article. The opinions expressed in this article are of the authors and do not reflect the policy of their affiliated organisations.
Competing interests: None declared.
References
- 1.World Bank Group, Human Development Network. HNPStats (Health, Nutrition and Population Statistics). http://devdata.worldbank.org/hnpstats/ (accessed 17 Mar 2004).
- 2.Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet 2003;361: 2226-34. [DOI] [PubMed] [Google Scholar]
- 3.Bhuiya A, Ribaux C, Eppler P. Community-led primary health care initiatives: lessons from a project in rural Bangladesh. In: Rohde J, Wyone, J, eds. Community-based healthcare: lessons from Bangladesh to Boston. Boston, MA: Management Sciences for Health, 2002: 87-111.
- 4.Antia NH, Dutta GP, Kasbekar AB. Health and medical care: a people's movement. Bombay: Foundation for Research in Community Health, 2000.
- 5.Antia NH, Bhatia K. People's health in people's hands—a model for Panchyati Raj. Bombay: Foundation for Research in Community Health, 1993.
- 6.Antia NH. The Mandwa experiment, an alternative strategy. BMJ 1986;292: 1181-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arole R, Arol M. Jamkhed: a comprehensive rural health project. London: McMillan Press, 1994.
- 8.De la Paz T. The Katiwala approach to training community health workers. World Health Forum 1983;4: 34-7. [Google Scholar]
- 9.Chaulagai C. Urban community health volunteer. World Health Forum 1993;14: 16-9. [PubMed] [Google Scholar]
- 10.El-Katsha S, Watss S. A model for health education. World Health Forum 1994;15: 29-33. [PubMed] [Google Scholar]
- 11.Stefanini A. Sustainability—the role of NGOs. World Health Forum 1995;16: 42-6. [PubMed] [Google Scholar]
- 12.Saludung D. Community mobilization and empowerment for health. World Health Forum 1997;18: 274-7. [PubMed] [Google Scholar]
- 13.Bhuiya A, Yasmin F, Begum F, Rob U. Community participation in health, family planning and development activities: a review of international experiences. Dhaka: International Center for Diarrhoeal Research Bangladesh, Population Council, 1996
- 14.Health and Nutrition Development Society. HANDS-AKF project: reducing maternal mortality by NGO-community partnership. Close out report. Karachi: HANDS, 2003
- 15.Perry HB. Health for all in Bangladesh: lessons in primary health care for the twenty first century. Dhaka: University Press, 2000.
- 16.Bang A, Bang R, Baitule S, Reddy M, Deshmukh M. Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet 1999;354: 1955-61. [DOI] [PubMed] [Google Scholar]
- 17.Hoddy E. The Banwasi Seva Ashram. New Delhi: Gandhi Peach Foundation, 1999.
- 18.Child in Need Institution (CINI). www.cini-india.org/ (accessed 6 Mar 2004).
- 19.What works? Literature review on community health workers in South Asia. Kathmandu, Nepal: Unicef, 2004.
- 20.World Bank. The road to better health conditions in Bangladesh. Washington, DC: World Bank, South Asia Region, Health, Population, and Nutrition Unit, 1998. (Available at http://lnweb18.worldbank.org/sar/sa.nsf/0/2f8c3d033ba533098525687b0065e63d?OpenDocument, accessed 17 March 2004.)
- 21.Namgyal P. Evaluation of the village health worker programme, Bhutan. Health Division, Royal Government of Bhutan, Unicef Bhutan, 1994.
- 22.Ministry of Health and Family Welfare. Major schemes and programmes. New Delhi: Government of India, 2000:160-1. (Available at http://mohfw.nic.in/MSP-1.pdf, accessed 17 March 2004.)
- 23.Government of Pakistan, Ministry of Health. National programme for family planning and primary health care. Lady health workers. http://phc.gov.pk/template.php?id=30 (accessed 17 Mar 2004).
- 24.Walt G, Perera M, Heggenhougen K. Are large-scale volunteer community health worker programmes feasible? The case of Sri Lanka. Soc Sci Med 1989;29: 599-608. [DOI] [PubMed] [Google Scholar]