Abstract
BACKGROUND
The purpose of this study was to compare rates of screening mammography among immigrant women in five Asian American ethnic groups in California, and ascertain the extent to which differences in mammography rates among these groups are attributable to differences in known correlates of cancer screening.
METHODS
Using 2009 data from the California Health Interview Survey, we compared the rates of mammography among Chinese, Filipino, Japanese, Korean, and Vietnamese immigrants 40 years and older. To assess the impact of Asian ethnicity on participation in screening, we performed multiple logistic regression analysis with models that progressively adjusted for acculturation, socio-demographic characteristics, access to health care and breast cancer risk factors, and examined the predicted probabilities of screening after adjusting for these factors.
FINDINGS
Participation in screening mammography differed according to ethnicity, with Filipina and Vietnamese Americans having the highest rates and Korean Americans having the lowest rates of lifetime and recent (past two years) screening. These differences decreased substantially after adjusting for acculturation, socio-demographic factors and risk factors of breast cancer but differences still remained, most notably for Korean Americans, who continued to have the lowest predicted probability of screening even after adjustment for these factors.
CONCLUSIONS
This analysis draws attention to low mammography screening rates among Asian American immigrants, especially recent immigrants who lack health insurance. Given that their breast cancer incidence is rising with length of stay in the United States, it is very important to increase regular mammography screening in these groups.
Introduction
The Asian population in the United States has been rapidly increasing from less than 0.5 million in 1965 to 18.2 million in 2011, with most of the growth attributable to high immigration rates from Asia. In 2009, Asians overtook Hispanics as the largest group of new immigrants to the United States (Pew Research Center, 2012). Of the states, California has the nation’s largest Asian American population, with 5.6 million, which is 15% of the total state population (Hoeffel, Rastogi, Kim & Shahid, 2010).
In California, breast cancer is the most commonly diagnosed cancer and the second leading cause of cancer death among women (American Cancer Society, California Department of Public Health, & California Cancer Registry, 2011). Although the incidence of breast cancer among Asian Americans overall is lower than among non-Hispanic whites in the US, the rates are substantially higher than the rates among women in their countries of origin (Jemal, Center, DeSantis & Ward, 2010). A number of studies have found that cancer incidence patterns among Asian American immigrants evolve over time to resemble those found in the US and this has been attributed to increasing exposure to Western lifestyles (Henderson et al, 1985; Le, Gomez, Clarke, Glaser, & West, 2002; Kolonel, Hinds, & Hankin, 1980; Ziegler et al, 1993;). Increases in breast cancer risk have been reported for US born as compared to foreign born women as well as for immigrants with longer residence in the US; for example, a study of women of Chinese, Japanese and Filipino ethnicities found that migrants who had lived in the West for a decade or longer had a breast cancer risk 80% higher than more recent migrants (Ziegler et al, 1993).
Considerable heterogeneity in breast cancer incidence and trends in incidence have been found among women of different Asian American ethnicities. In particular, several studies have found that the incidence among Japanese and Filipina American women is much higher and has increased more rapidly than among Chinese and Korean American women (Keegan, Gomez, Clarke, Chan, & Glaser, 2007; Kwong, Chen, Snipes, Bal, & Wright, 2005; Liu, Zhang, Wu, Pike, & Deapen, 2012; McCracken et al., 2007). Overall, we may expect breast cancer incidence to continue to increase among Asian American women as the large cohort of recent immigrants increasingly adopts a Western lifestyle and the population of second- and later-generations continues to grow.
Despite the evidence that mammography screening reduces breast cancer mortality (de Koning, 2003; Humphrey, Helfand, Chan, & Woolf, 2002) and despite guidelines from various organizations to obtain a mammogram every 1 to 2 years, immigrant women are less likely than non-immigrant women to report receipt of a mammogram in the past two years (Swan, Breen, Coates, Rimer, & Lee, 2003), or to be diagnosed at an early stage of disease (Hedeen, White, & Taylor, 1999; Hedeen & White, 2001). In general, multiple factors influence the utilization of breast cancer screening services by individuals and population subgroups. Socio-demographic characteristics such as lower income or educational level, and health care access factors such as lack of health insurance or lack of usual source of health care have been identified as barriers to cancer screening (Consedine, 2012; Juon, Kim, Shankar, & Han, 2004; Rakowski et al, 2004; Rakowski et al, 2006; Rosenberg, Wise, Plamar, Horton,& Adams-Campbell,2005). These factors may be more prevalent among immigrant groups. Several studies have reported that cultural background influences utilization of health care services including cancer screening among some immigrant ethnic groups in US (Courtright, 2004; Ma & Fleisher, 2003). Cultural incongruities between immigrant populations and the health system in their new country may influence the extent to which immigrant people access health care services (Ma & Fleisher, 2003). Another important barrier for immigrants may be low English language proficiency, which is associated with lower likelihood of screening (Juon, Kim, Shankar, & Han, 2004; Todd, Harvey, & Hoffman-Goetz, 2011). Breast cancer risk factors, in particular having a first-degree relative diagnosed with breast cancer, have been reported to be associated with increased likelihood of breast cancer screening among Chinese immigrant women (Lee-Lin et al, 2007).
To reduce the burden of breast cancer, it is important to identify groups with low rates of breast cancer screening (Rakowski, Wyn, Breen, Meissner, & Clark, 2010). Although Asian Americans are often examined as a single group, it is important to disaggregate Asian American subgroups to avoid masking differences among them (Gomez, Tan, Keegan, & Clarke, 2007; Kagawa-Singer et al, 2007). However, it is also important to examine the extent to which differences among immigrant groups may be attributable to differences in recognized barriers to cancer screening such as lower education and lack of health insurance. Some of these differences may be due to differences in immigration status and length of US residency among these groups.
Therefore, the objectives of this study were to (1) compare rates of screening mammography among immigrant women aged 40 years and older in five Asian American ethnic groups in California -- Chinese, Filipino, Japanese, Korean, and Vietnamese, and (2) ascertain the extent to which differences in mammography rates among these groups are attributable to differences in known correlates of cancer screening including acculturation, socio-demographic characteristics, access to health care and breast cancer risk factors, and what differences may remain after controlling for these factors.
Methods
Data source and study population
We used data from the 2009 California Health Interview Survey (CHIS) (http://healthpolicy.ucla.edu/chis/Pages/default.aspx). The CHIS is a population-based random digit dial telephone survey conducted biannually since 2001 to provide population-based estimates of health indicators for all major racial/ethnic groups and several Asian racial/ethnic subgroups in California. CHIS collects extensive information on health status, health conditions, health-related behaviors, health insurance coverage, access to health care services, and other health and health related issues. The 2009 CHIS employed a multi-stage sample design. Within geographic stratum, households were selected by random digit dial sampling, and within each household, one adult (age 18 and over) was randomly selected for a telephone interview. Koreans and Vietnamese were oversampled to increase the precision of estimates for these groups. Interviews were conducted in English, Spanish, Cantonese, Mandarin, Vietnamese and Korean. The 2009 CHIS interviewed a total of 47,614 adults (CHIS, 2009).
Immigrants were defined as persons who reported they were born outside the US. Asian ethnicity was defined using the University of California Los Angeles Center for Health Policy Research classification codes for Asian subtypes. We examined five Asian ethnic groups, Chinese, Filipino, Japanese, Korean and Vietnamese, and restricted the sample to women aged 40 years and older. From the total of 1848 Asian women aged 40 years and older in the 2009 CHIS (448 Chinese, 218 Filipino, 202 Japanese, 482 Korean and 498 Vietnamese), 1596 (86%) were immigrants (369 Chinese, 201 Filipino, 57 Japanese, 472 Korean and 497 Vietnamese) and were included in this analysis.
Variables
The dependent variables in this study were receiving a mammogram in the past 2 years (recent screening) and ever received a mammogram (lifetime screening). The main independent variable of interest was Asian ethnicity. Independent variables examined as potential confounders included acculturation (citizenship status, English proficiency, percent life in US), socio-demographic characteristics (age, educational attainment, income, marital status, current health insurance), and risk factors for breast cancer (regular physical activity and overweight/obesity). Sample sizes for other risk factors such as current smoking, binge drinking and family history of breast cancer were too small for stable estimates.
Age was classified as 40-49, 50-59, 60-69 or ≥70 years. Educational attainment was classified as high school graduate or less, or at least some college. Income was categorized according to the federal poverty level (FPL): 0-199% FPL or ≥200 % FPL. Marital status was classified as married or not. Citizenship status was coded as citizen or non-citizen, and English proficiency was categorized as only English/very well/well, or not well/not at all. Percent life in US was categorized as 0-40% or ≥41%. Current health insurance was classified as yes or no. Regular physical activity was coded as yes if the participant reported 20 minutes of vigorous leisure-time physical activity 3 days or more in the past week, or 30 minutes of moderate physical activity 5 days or more in the past week) and no otherwise. Overweight/obesity (self-reported height and weight corresponding to body mass index ≥ 25 kg/m2) was coded as yes or no.
Statistical Analysis
We used SAS v9.2 (SAS Institute, Cary, NC) to perform all analyses. CHIS-provided sample weights were used to account for the complex sampling design and obtain population estimates in all analyses. We first assessed the association between acculturation, socio-demographic characteristics and breast cancer risk factors and Asian ethnicity, and between mammography screening and Asian ethnicity, using Wald chi-square design-adjusted tests of independence.
We next examined differences in mammography rates among the five Asian ethnic groups when progressively adjusting for acculturation, socio-demographic characteristics, and breast cancer risk factors, using multiple logistic regression. Four models were fit for each of the outcomes, recent screening and lifetime screening. Model 1 included only Asian ethnicity. Model 2 added acculturation factors (citizenship status, English proficiency, percent life in US) to Model 1. Model 3 added socio-demographic factors (age, marital status, educational attainment, income) and access to health care services (current health insurance) to Model 2. Model 4 added risk factors for breast cancer (physical activity and overweight/obesity). Filipino Americans were used as the reference group because they had high rates of both lifetime and recent screening. In addition to examining adjusted odds ratios (ORs) and 95% confidence intervals (CIs), we conducted Wald tests to jointly test the significance of groups of covariates – ethnicity indicators, acculturation variables, socio-demographic characteristics/access to care, and breast cancer risk factors. These tests tested the null hypothesis that all coefficients for the variables were equal to zero simultaneously.
We further calculated the predicted probabilities of screening for each Asian immigrant group under each model. A predicted probability is the estimated probability of screening given a set of covariate values and is calculated by inverting the logistic link function, which yields , where is the predicted probability, x is a vector of covariate values, and is a vector of estimated regression coefficients. Means for the overall sample were used for the covariate values; thus the predicted probabilities may be interpreted as adjusted probabilities of screening for each ethnic group, when covariates are held constant at their means. Confidences intervals for predicted probabilities were obtained by applying the inverse link transformation to the confidence limits for the estimate.
P values < .05 were considered statistically significant.
Results
There was considerable heterogeneity in socio-demographic characteristics, acculturation and breast cancer risk factors among the five different ethnicities of Asian immigrant women in California (Table 1). Filipina women were older and had higher levels of income and education; Chinese, Korean and Vietnamese women were younger and had lower levels of income and education. Lack of current health insurance was most prevalent among Korean women, followed by Vietnamese and Chinese women. Filipina women had high rates of English proficiency, whereas most Chinese, Korean and Vietnamese women spoke English not well or not at all. Most Chinese and Korean women had lived 40% or less of their lifetime in the US, whereas most Filipina, Japanese and Vietnamese women had lived in the US over 40% of their lifetimes. Rates of overweight/obesity differed significantly among groups. Filipina women had the highest rates of overweight/obesity (46.7%).
Table 1.
Sample characteristics of Asian immigrant women in California by Asian ethnicity, 2009 California Health Interview Survey
| Chinese (N=−369) |
Filipino (N=201) |
Japanese (N=57) |
Korean (N=472) |
Vietnamese (N=497) |
||
|---|---|---|---|---|---|---|
| Pct (SE) | Pct (SE) | Pct (SE) | Pct (SE) | Pct (SE) | p-value | |
| Age | ||||||
| 40-49 | 45.0 (5.1) | 14.5 (3.0) | 40.0 (9.4) | 46.1 (5.1) | 37.7 (7.8) | <0.0001 |
| 50-59 | 22.0 (4.1) | 33.1 (4.6) | 26.9 (7.5) | 19.3 (4.0) | 34.0 (7.0) | |
| 60-69 | 13.8 (2.4) | 36.1 (5.0) | 10.8 (5.0) | 20.4 (3.4) | 21.5 (4.5) | |
| 70+ | 19.2 (2.7) | 16.2 (3.4) | 22.3 (7.1) | 14.2 (3.4) | 6.8 (6.0) | |
| Marital status | ||||||
| Married/live with partner |
77.3 (3.4) | 69.1 (5.0) | 71.5 (7.1) | 82.0 (3.4) | 79.4 (3.4) | 0.17 |
| Not married | 22.7 (3.4) | 30.9 (5.0) | 28.5 (7.1) | 18.0 (3.4) | 20.6 (3.4) | |
| Poverty level | ||||||
| 0-199% FPL | 40.9 (4.6) | 20.8 (3.5) | 13.6 (4.9) | 40.0 (4.7) | 52.3 (7.1) | <.0001 |
| 200% FPL & above | 59.1 (4.6) | 79.2 (3.5) | 86.4 (4.9) | 60.0 (4.7) | 41.7 (7.1) | |
| Education | ||||||
| ≤ High school | 47.5 (5.1) | 30.1 (4.6) | 39.6 (8.5) | 44.8 (5.2) | 67.0 (7.3) | <.0001 |
| College and over | 52.5 (5.1) | 69.9 (4.6) | 60.4 (8.5) | 55.2 (5.2) | 33.0 (7.3) | |
| Health insurance | ||||||
| Yes | 91.9 (1.6) | 95.6 (1.9) | 98.9 (1.1) | 67.2 (4.5) | 88.5 (4.4) | <.0001 |
| Citizenship | ||||||
| Citizen | 80.0 (5.2) | 86.0 (3.2) | 61.7 (8.7) | 70.4 (4.1) | 87.3 (5.1) | 0.02 |
| Non-citizen | 20.0 (5.2) | 14.0 (3.2) | 38.3 (8.7) | 29.6 (4.1) | 12.7 (5.1) | |
| English proficiency | ||||||
| Only/very well/ well | 48.5 (4.4) | 95.9 (1.3) | 78.8 (8.3) | 32.5 (4.7) | 39.6 (7.2) | <.0001 |
| Not well/not at all | 51.5 (4.4) | 4.1 (1.3) | 21.2 (8.3) | 67.5 (4.7) | 60.4 (7.2) | |
| Percent life in US | ||||||
| 0-40% | 51.0 (5.3) | 33.4 (4.2) | 31.9 (7.8) | 50.1 (4.7) | 35.7 (6.0) | 0.006 |
| 41% + | 49.0 (5.3) | 66.6 (4.2) | 69.1 (7.8) | 49.9 (4.7) | 64.3 (6.0) | |
| Regular physical activity |
||||||
| Yes | 53.8 (4.1) | 49.6 (4.9) | 58.0 (9.3) | 52.0 (4.3) | 57.0 (6.5) | 0.82 |
| Overweight/obesity | ||||||
| Yes | 19.1 (3.7) | 46.7 (5.2) | 22.8 (7.3) | 20.0 (3.5) | 17.4 (4.8) | <0.0001 |
Percent (pct) and standard errors (SE) calculated using CHIS sampling weights.
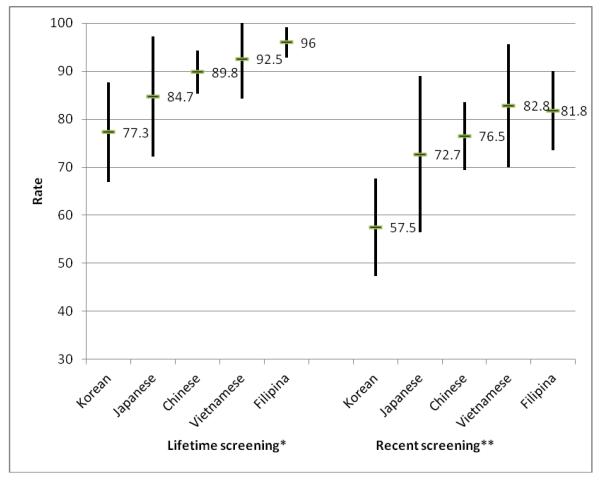
Figure 1 shows participation rates in lifetime and recent (past two years) mammography screening. Filipina and Vietnamese women had the highest rates of lifetime and recent screening; Korean women had the lowest rates (77.3%, 95% CI 66.9%-87.7% with lifetime screening, 57.5%, 95% CI 47.3%-67.7% with recent screening).
Table 2 shows results of multiple logistic regression models for the outcome lifetime mammography screening in Chinese, Japanese, Korean and Vietnamese women compared to Filipina women. In Model 1, which included only ethnicity, ethnicity was significant associated with lifetime screening (p=.006). Chinese, Japanese and Korean women had lower odds of lifetime screening (OR 0.36, 95% CI 0.14-0.93; OR 0.23, 95% CI 0.06-0.85; OR 0.14, 95% CI 0.05-0.39, respectively) compared to Filipina women. In Model 2, which added acculturation factors to Model 1, and Model 3, which added socio-demographic characteristics and current health insurance, only Korean women had lower odds of lifetime screening (Model 2: OR 0.16, 95% CI 0.05-0.52; Model 3: OR 0.21 95% CI 0.05-0.86). In Model 4, which included all variables including acculturation, socio-demographic factors, health insurance and risk factors of breast cancer, there was no significant association between ethnicity and lifetime screening; the acculturation variables and socio-demographic variables as groups were significantly associated with lifetime screening (p=.004 and p=.01, respectively). Among the individual variables, only citizenship status was associated with lifetime screening at the p<.05 level (OR 3.26, 95% CI 1.34-7.89).
Table 2.
Results of multiple logistic regression models for the outcome lifetime mammography screening among Asian immigrant women in California
| Variables | Model 1 OR (95% CI) |
Model 2 OR (95% CI) |
Model 3 OR (95% CI) |
Model 4 OR (95% CI) |
|---|---|---|---|---|
| ETHNICITY (Ref: Filipino) | ||||
| Chinese | 0.36 (0.14-0.93) | 0.38 (0.14-1.02) | 0.42 (0.13-1.38) | 0.53 (0.17-1.66) |
| Japanese | 0.23 (0.06-0.85) | 0.32 (0.08-1.20) | 0.28 (0.08-1.09) | 0.36 (0.10-1.37) |
| Korean | 0.14 (0.05-0.39) | 0.16 (0.05-0.52) | 0.21 (0.05-0.86) | 0.26 (0.06-1.05) |
| Vietnamese | 0.51 (0.08-3.13) | 0.43 (0.08-2.45) | 0.59 (0.10-3.30) | 0.63 (0.13-2.94) |
| ACCULTURATION | ||||
| Citizenship (Ref: Non-citizen) | ||||
| Citizen | - | 3.88 (1.82-8.29) | 3.25 (1.32-7.99) | 3.26 (1.34-7.89) |
| English proficiency (Ref: Not well/not at all) |
||||
| Only/very well/ well | - | 0.81 (0.41-1.58) | 0.63 (0.30-1.33) | 0.60 (0.29-1.25) |
| Percent life in US (Ref: 0-40%) | ||||
| 41%+ | - | 1.59 (0.84-3.03) | 1.50 (0.76-2.95) | 1.44 (0.72-2.85) |
| Age (Ref: 40-49) | ||||
| 50-59 | - | - | 1.76 (0.81-3.82) | 1.79 (0.85-3.80) |
| 60-69 | - | - | 2.32 (0.79-6.76) | 2.23 (0.79-6.32) |
| 70+ | - | - | 0.75 (0.22-2.53) | 0.84 (0.26-2.75) |
| SOCIODEMOGRAPHIC CHARACTERISTICS |
||||
| Marital status (Ref: Not married) | ||||
| Married/live with partner | - | - | 0.85 (0.33-2.15) | 0.88 (0.33-2.34) |
| Educational attainment (Ref: ≤ High school degree) |
||||
| College and over | - | - | 1.29 (0.61-2.76) | 1.28 (0.61-2.67) |
| Poverty level (Ref: 0-199% FPL) | ||||
| 200% FPL & above | - | - | 1.20 (0.50-2.87) | 1.20 (0.49-2.94) |
| Current health insurance (Ref: No) |
||||
| Yes | - | - | 2.69 (0.91-7.90) | 2.42 (0.88-6.64) |
| BREAST CANCER RISK FACTORS |
||||
| Regular physical activity (Ref: No) |
||||
| Yes | - | - | - | 1.76 (0.83-3.72) |
| Overweight/obesity (Ref: No) | ||||
| Yes | - | - | - | 1.35 (0.57-3.18) |
| P-value for ethnicity | 0.006 | 0.05 | 0.33 | 0.34 |
| P-value for acculturation | 0.0007 | 0.005 | 0.004 | |
| P-value for socidemographic characteristics |
0.007 | 0.01 | ||
| P-value for breast cancer risk factors |
0.31 |
Each model included the variables with listed odds ratios.
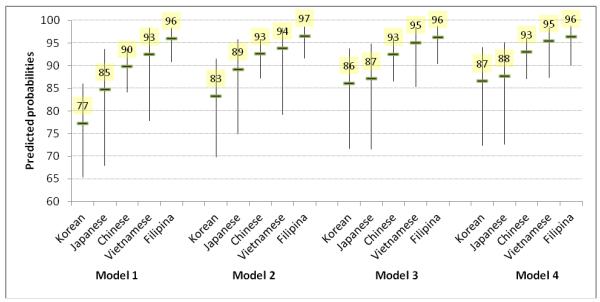
Figure 2 shows that as variables were added to the model, the predicted probabilities of lifetime screening among the five groups became more similar, although confidence intervals overlapped and some were wide. In Model 1, the gap between the lowest predicted screening rate (0.77 in Koreans) and highest (0.96 in Filipinas) was 0.19; in Model 4, the gap between the lowest (0.87 in Koreans) and highest (0.96 in Filipinas) was 0.09.
Table 3 shows results of multiple logistic regression models for the outcome recent mammography screening. Ethnicity was significant associated with recent screening only in Model 1 (p=.008); in this model, Korean women had a lower odds of recent screening compared to Filipina women (OR 0.30, 95% CI 0.15-0.61). In Model 4, which included all variables including acculturation, socio-demographic factors, health insurance and risk factors of breast cancer, socio-demographic characteristics as a group were highly significant (P<.0001); married status (OR 2.59 95% CI 1.36-4.95), educational attainment of college or higher (OR 2.02 95% CI 1.20-3.40) and current health insurance (OR 4.11 95% CI 1.97-8.58) were associated with recent screening at p<.05. Breast cancer risk factors were also significant associated with recent screening as a group (p=.0009); overweight/obesity was significant individually (OR 1.95, 95% CI 1.11-3.43).
Table 3.
Results of multiple logistic regression models for the outcome of recent mammography screening among Asian immigrant women in California
| Variables | Model 1 OR (95% CI) |
Model 2 OR (95% CI) |
Model 3 OR (95% CI) |
Model 4 OR (95% CI) |
|---|---|---|---|---|
| ETHNICITY (Ref: Filipino) | ||||
| Chinese | 0.73 (0.39-1.34) | 1.10 (0.59-2.05) | 1.08 (0.56-2.07) | 1.30 (0.66-2.57) |
| Japanese | 0.59 (0.24-1.49) | 0.76 (0.30-1.92) | 0.67 (0.28-1.61) | 0.78 (0.32-1.91) |
| Korean | 0.30 (0.15-0.61) | 0.50 (0.22-1.13) | 0.57 (0.25-1.31) | 0.68 (0.28-1.64) |
| Vietnamese | 1.07 (0.36-3.16) | 1.57 (0.55-4.44) | 2.08 (0.67-6.45) | 2.30 (0.75-7.09) |
| ACCULTURATION | ||||
| Citizenship (Ref: Non-citizen) | ||||
| Citizen | - | 1.73 (0.80-3.74) | 1.61 (0.65-3.97) | 1.65 (0.69-3.93) |
| English proficiency (Ref: Not well/not at all) |
||||
| Only/very well/well | - | 1.80 (1.02-3.20) | 1.34 (0.72-2.50) | 1.27 (0.67-2.39) |
| Percent life in US (Ref: 0-40%) | ||||
| 41% + | - | 1.48 (0.77-2.84) | 1.18 (0.63-2.21) | 1.08 (0.60-1.96) |
| SOCIODEMOGRAPHIC CHARACTERISTICS |
||||
| Age (Ref: 40-49) | ||||
| 50-59 | - | - | 2.15 (1.04-4.44) | 2.07 (0.99-4.31) |
| 60-69 | - | - | 1.74 (0.80-3.80) | 1.61 (0.74-3.49) |
| 70+ | - | - | 1.73 (0.59-5.08) | 1.76 (0.63-4.91) |
| Marital status (Ref: Not married) | ||||
| Married/live with partner | - | - | 2.50 (1.31-4.77) | 2.59 (1.36-4.95) |
| Educational attainment (Ref: ≤ High school degree) |
||||
| College and over | - | - | 2.22 (1.27-3.87) | 2.02 (1.20-3.40) |
| Poverty level (Ref: 0-199% FPL) | ||||
| 200% FPL & above | - | - | 1.11 (0.59-2.09) | 1.17 (0.61-2.24) |
| Current health insurance (Ref: No) |
||||
| Yes | - | - | 4.07 (1.85-8.95) | 4.11 (1.97-8.58) |
| BREAST CANCER RISK FACTORS |
||||
| Regular physical activity (Ref: No) |
||||
| Yes | - | - | - | 1.74 (0.96-3.16) |
| Overweight/obesity (Ref: No) | ||||
| Yes | - | - | - | 1.95 (1.11-3.43) |
| P-value for ethnicity | 0.008 | 0.13 | 0.10 | 0.09 |
| P-value for acculturation | - | 0.007 | 0.34 | 0.44 |
| P-value for sociodemographic characteristics |
- | - | <0.0001 | <0.0001 |
| P-value for breast cancer risk factors |
- | - | - | 0.009 |
Each model included the variables with listed odds ratios.
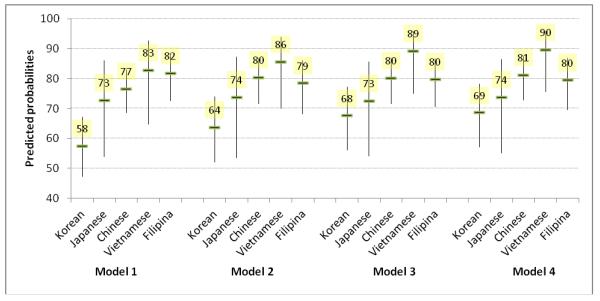
Figure 3 shows the predicted probabilities of recent mammography screening for each of the five ethnicities under each model. In Model 1, the gap between the lowest predicted screening rate (0.58 in Koreans) and the highest (0.83 in Vietnamese) was 0.25. In Model 4, the gap between the lowest (0.69 in Koreans) and the highest (0.90 in Vietnamese) was 0.21
Discussion
Our analysis of 2009 survey responses from a large population-based sample of the most populous Asian American immigrant groups in California showed that Chinese, Filipino, Japanese, Korean and Vietnamese American women differed substantially with respect to demographic characteristics, acculturation and health insurance coverage and regarding breast cancer risk factors. Large proportions of women in each ethnic group had ever had a mammogram, ranging from 77.3% among Korean American to 96.0% among Filipino American immigrants. Rates of recent mammography screening within the past 2 years were more unequal than lifetime rates, ranging from 57.5% among Korean American to 82.8% among Vietnamese American immigrants, and were less well explained by potential confounders. This is a concern since the effectiveness of mammography screening in reducing breast cancer mortality is based on annual or biannual screening (de Koning, 2003; Humphrey, Helfand, Chan, & Woolf, 2002). Korean American immigrants were the only subgroup in the study sample that did not meet the Healthy People 2010 objectives of 70% of women having a mammogram in the past 2 years (US Department of Health and Human Services, 2011).
Much of the observed differences in screening rates were attributable to differences in socio-demographic characteristics among the groups, but even after controlling for these differences, Korean American immigrants stood out as the group with the lowest odds of obtaining mammography screening. Other analyses of CHIS data that were collected between 2001 and 2005 have found similar disparities among Asian American women residing in California with respect to breast, colorectal and cervical cancer screening (Lee, Ju, Vang, & Lundquist, 2010; Lee, Lundquist, Ju, Luo, & Townsend, 2011; Maxwell, Crespi, Antonio, & Peiyun, 2010; Wong, Gildengorin, Nguyen, & Mock, 2005). All of these studies report that the lowest screening rates were among Korean American women. In addition to ethnic subgroup, low screening rates were found among women with low level of acculturation, lack of health insurance and low level of education.
Implications for practice and health policy
Based on these findings, we make the following recommendations:
Because many Korean American immigrants are seeking health care in clinics located in “Korea-towns” and/or in clinics that offer services in Korean language, providers in these clinics should comprehensively assess cancer screening history for breast, cervix and colon/rectum and perform or recommend tests that are needed.
Providers in all health care settings should be aware that Korean American women and other Asian American women who are recent immigrants and lack health insurance have a high risk of being overdue for cancer screening tests. They should utilize any visit as an opportunity to stress the importance of screening and to perform/recommend appropriate screening tests.
Programs that provide free or low-cost screening to uninsured women, such as the Centers for Disease Control and Prevention funded programs for breast, cervical and colorectal cancer screening, should make special efforts to reach out to Asian American immigrants and especially to Korean American women.
Providers should stress the importance of repeat screening every 1-2 years among Asian American patients. A one-time test is insufficient for early cancer detection.
The strength of this study is that data come from a large population-based survey that was conducted in several languages, allowing less acculturated and/or more recently immigrated Asian Americans to be included in the analysis. There are also several limitations to this study. First, although large proportions of Asian American immigrants live in California, our findings may not generalize to Asian American immigrants in other regions of the United States. In addition, we did not include other Asian American groups such as South Asians or Asian Pacific Islanders due to insufficient sample sizes for these groups. Second, CHIS data are based on self-report, and the accuracy of self-reported cancer screening rates may vary by nativity, language proficiency, and race/ethnicity (Kandula, Wen, Jacobs, & Lauderdale, 2006). Third, we could not exclude women with history of breast cancer (who may be more likely to obtain regular mammograms) because CHIS 2009 did not collect that information. Finally, we did not distinguish between routine and diagnostic mammograms for most recent and lifetime screening, which is consistent with CHIS analyses reported by others (e.g., Lee, Ju, Vang, & Lundquist, 2010).
Conclusions
This analysis draws attention to low breast cancer screening rates among Asian American immigrants, especially recent immigrants who lack health insurance. The lowest rates were found among Korean American women. Given that the Asian American population is rapidly increasing, largely through immigration, and that breast cancer incidence rises with length of stay in the United States, it is very important to increase regular mammography screening in these groups in order to decrease breast cancer disparities.
Figure 1.
Participation rates (with 95% confidence intervals) in mammography screening by ethnicity among Asian immigrant women in California, 2009 California Health Interview Survey *p=0.0009, **p=0.01
Figure 2.
Predicted probabilities (with 95% confidence intervals) of lifetime mammography screening from each model by ethnicity
Figure 3.
Predicted probabilities (with 95% confidence intervals) of recent mammography screening from each model by ethnicity
Acknowledgments
S.Y.R. was supported by research funds of Chosun University, 2012. C.M.C. was supported by National Institutes of Health grant CA16042. A.E.M. was supported by the UCLA Cancer Prevention and Control Research Network (U48DP001934), the Charles Drew University/UCLA Cancer Center Partnership to Eliminate Cancer Health Disparities (NIH U54 CA143931), and the UCLA Kaiser Permanente Center for Health Equity.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Cancer Society, California Department of Public Health, & California Cancer Registry . California Cancer Facts and Figures 2012. American Cancer Society, California Division; Oakland, CA: 2011. [Google Scholar]
- California Health Interview Survey (CHIS) CHIS 2009 Data Dictionary, Public Use File, Adult Survey. 2009 Available from: http://www.chis.ucla.edu/main/PUF/puf09_adult_datadic.pdf.
- Consedine NS. The demographic, system, and psychosocial origins of mammographic screening disparities: Prediction of initiation versus maintenance screening among immigrant and non-immigrant women. Journal of Immigrant & Minority Health. 2012;14:570–582. doi: 10.1007/s10903-011-9524-z. [DOI] [PubMed] [Google Scholar]
- Courtright C. Health information-seeking among Latino newcomers: An explanatory study. Information Research. 2004;10 paper 224. Available from: http://InformationR.net/ir/210-222/paper224.html. [Google Scholar]
- de Koning HJ. Mammographic screening; evidence from randomized controlled trials. Annals of Oncology. 2003;14:1185–1189. doi: 10.1093/annonc/mdg319. [DOI] [PubMed] [Google Scholar]
- Gomez SL, Tan S, Keegan THM, Clarke CA. Disparities in mammographic screening for Asian women in California: a cross-sectional analysis to identify meaningful groups for targeted intervention. BMC Cancer. 2007 doi: 10.1186/1471-2407-7-201. Doi:10.1186/1471-2407-7-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeden AN, White E, Taylor V. Ethnicity and birthplace in relation to tumor size and stage in Asian American women with breast cancer. American Journal of Public Health. 1999;89:1248–1252. doi: 10.2105/ajph.89.8.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeden AN, White E. Breast cancer size and stage in Hispanic American women, by birthplace: 1992-1995. American Journal of Public Health. 2001;91:122–125. doi: 10.2105/ajph.91.1.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson BE, Kolonel LN, Dworsky R, Kerford D, Mori E, Singh K, et al. Cancer incidence in islands of the Pacific. Journal of the National Cancer Institute. 1985;69:73–81. [PubMed] [Google Scholar]
- Hoeffel EM, Rastogi S, Kim MO, Shahid H. Census Briefs; The Asian population: 2010. 2010 Available from: http://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf.
- Humphrey LL, Helfand M, Chan BK, Woolf SH. Breast cancer screening: a summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2002;137:347–360. doi: 10.7326/0003-4819-137-5_part_1-200209030-00012. [DOI] [PubMed] [Google Scholar]
- Jemal A, Center MM, DeSantis C, Ward EM. Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiology Biomarkers & Prevention. 2010;19:1893–1907. doi: 10.1158/1055-9965.EPI-10-0437. [DOI] [PubMed] [Google Scholar]
- Juon HS, Kim M, Shankar S, Han W. Predictors of adherence to screening mammography among Korean American women. Preventive Medicine. 2004;39:474–481. doi: 10.1016/j.ypmed.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Kagawa-Singer M, Pourat N, Breen N, Coughlin S, Abend Mclean T, McNeel TS, et al. Breast and cervical cancer screening rates of subgroups of Asian American women in California. Medical Care Research & Review. 2007;64:706–730. doi: 10.1177/1077558707304638. [DOI] [PubMed] [Google Scholar]
- Kandula NR, Wen M, Jacobs EA, Lauderdale DS. Low rates of colorectal, cervical, and breast cancer screening in Asian Americans compared with Non-Hispanic whites; Cultural influences or access to care? Cancer. 2006;107:184–192. doi: 10.1002/cncr.21968. [DOI] [PubMed] [Google Scholar]
- Keegan THM, Gomez SL, Clarke CA, Chan JK, Glaser SL. Recent trends in breast cancer incidence among 6 Asian groups in the Greater Bay Area of Northern California. International Journal of Cancer. 2007;120:1324–1329. doi: 10.1002/ijc.22432. [DOI] [PubMed] [Google Scholar]
- Kolonel LN, Hinds MW, Hankin JH. Cancer patterns among migrant and native-born Japanese in Hawaii in relation to smoking, drinking, and dietary habits. In: Gelboin HV, et al., editors. Genetic and environmental factors in experimental and human cancer. Japan Science Society Press; Tokyo: 1980. pp. 327–340. [Google Scholar]
- Kwong SL, Chen MS, Jr, Snipes KP, Bal DG, Wright WE. Asian subgroups and cancer incidence and mortality rates in California. Cancer. 2005;104:2975–2981. doi: 10.1002/cncr.21511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le GM, Gomez SL, Clarke CA, Glaser SL, West DW. Cancer incidence patterns among Vietnamese in the United States and Ha Noi, Vietnam. International Journal of Cancer. 2002;102:412–427. doi: 10.1002/ijc.10725. [DOI] [PubMed] [Google Scholar]
- Lee HY, Ju E, Vand PD, Lundquist M. Breast and cervical cancer screening disparity among Asian American women: Does race/ethnicity matter? Journal of Women’s Health. 2010;10:1877–1884. doi: 10.1089/jwh.2009.1783. [DOI] [PubMed] [Google Scholar]
- Lee HY, Lundquist M, Ju E, Luo X, Townsend A. Colorectal cancer screening disparities in Asian Americans and Pacific Islanders: which groups are most vulnerable? Ethnicity & Health. 2011;16:501–518. doi: 10.1080/13557858.2011.575219. [DOI] [PubMed] [Google Scholar]
- Lee-Lin F, Menon U, Pett M, Nail L, Lee S, Mooney K. Breast cancer beliefs and mammography screening practices among Chinese American immigrants. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2007;36:212–221. doi: 10.1111/j.1552-6909.2007.00141.x. [DOI] [PubMed] [Google Scholar]
- Liu L, Zhang J, Wu AH, Pike M, Deapen D. Invasive breast cancer incidence trends by detailed race/ethnicity and age. International Journal of Cancer. 2012;130:395–404. doi: 10.1002/ijc.26004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma GX, Fleisher L. Awareness of cancer information among Asian Americans. Journal of Community Health. 2003;28:115–130. doi: 10.1023/a:1022695313702. [DOI] [PubMed] [Google Scholar]
- Maxwell AE, Crespi CM, Antonio CM, Lu P. Explaining disparities in colorectal screening among five Asian ethnic groups: A population-based study in California. BMC Cancer. 2010;10:214. doi: 10.1186/1471-2407-10-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken M, Olsen M, Chen MS, Jr, Jemal A, Thun M, Cokkinides V, et al. Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA: a Cancer Journal for Clinicians. 2007;57:190–205. doi: 10.3322/canjclin.57.4.190. [DOI] [PubMed] [Google Scholar]
- Pew Research Center Pew Social & Demographic Trends; The Rise of Asian Americans. 2012 Available from: http://www.pewsocialtrends.org/files/2012/06/SDT-The-Rise-of-Asian-Americans-Full-Report.pdf.
- Rakowski W, Breen N, Meissner H, Rimer BK, Vernon SW, Clark MA, et al. Prevalence and correlates of repeat mammography among women aged 55-79 in the Year 2000 National Health Interview Survey. Preventive Medicine. 2004;39:1–10. doi: 10.1016/j.ypmed.2003.12.032. [DOI] [PubMed] [Google Scholar]
- Rakowski W, Meissner H, Vernon SW, Breen N, Rimer B, Clark MA. Correlates of repeat and recent mammography for women ages 45 to 75 in the 2002 to 2003 Health Information National Rends Survey (HINTS 2003) Cancer Epidemiology Biomarkers & Prevention. 2006;15:2093–2101. doi: 10.1158/1055-9965.EPI-06-0301. [DOI] [PubMed] [Google Scholar]
- Rakowski W, Wyn R, Breen N, Meissner H, Clark MA. Prevalence and correlates of recent and repeat mammography among California women ages 55-79. Cancer Epidemiology. 2010;34:168–177. doi: 10.1016/j.canep.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg L, Wise LA, Plamer JR, Horton NJ, Adams-Campbell LL. A multilevel study of socio-economic predictors of regular mammography use among African-American women. Cancer Epidemiology Biomarkers & Prevention. 2005;14:2628–2633. doi: 10.1158/1055-9965.EPI-05-0441. [DOI] [PubMed] [Google Scholar]
- Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97:1528–1540. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- Todd L, Harvey E, Hoffman-Goetz L. Predicting breast and colon cancer screening among English-as-a-second-language older Chinese immigrant women to Canada. Journal of Cancer Education. 2011;26:161–169. doi: 10.1007/s13187-010-0141-7. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (DHHS) Healthy People 2010 midcourse review. 2011 Available from: http://www.healthypeople.gov/2010/data/midcourse/pdf/fa03.pdf.
- Wong ST, Gildengorin G, Nguyen T, Mock J. Disparities in colorectal cancer screening rates among Asian Americans and Non-Latino whites. Cancer. 2005;104:2940–2947. doi: 10.1002/cncr.21521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziegler RG, Hoover RN, Pike MC, Hildesheim A, Nomura AM, West DW, et al. Migration patterns and breast cancer risk in Asian-American women. Journal of the National Cancer Institute. 1993;85:1819–1827. doi: 10.1093/jnci/85.22.1819. [DOI] [PubMed] [Google Scholar]