Abstract
Introduction and Hypothesis:
Patient preparedness for stress urinary incontinence (SUI) surgery is associated with improvements in post-operative satisfaction, symptoms and quality of life (QoL). This planned secondary analysis examined the association of patient preparedness with surgical outcomes, treatment satisfaction and quality of life.
Methods:
The ValUE trial compared the effect of pre-operative urodynamic studies to a standardized office evaluation on outcomes of SUI surgery at one year. In addition to primary and secondary outcome measures, patient satisfaction with treatment was measured with a 5-point Likert scale (very dissatisfied to very satisfied) that queried subjects to rate the treatment’s effect on overall incontinence, urge incontinence, SUI, and frequency. Preparedness for surgery was assessed using an 11-question Patient Preparedness Questionnaire (PPQ).
Results:
Based on PPQ Question 11, 4 out of 5 (81%) of women reported they “agreed” or “strongly agreed” that they were prepared for surgery. Selected demographic and clinical characteristics were similar in unprepared and prepared women. Among SUI severity baseline measures, total UDI score was significantly but weakly associated with preparedness (question 11 of the PPQ) (Spearman r = 0.13, p = 0.001). Although preparedness for surgery was not associated with successful outcomes, it was associated with satisfaction (rs=0.11, p = 0.02) and larger PGI-S improvement (increase) (p=0.008).
Conclusions:
Approximately half (48%) of women “strongly agreed” that they felt prepared for SUI. Women with higher pre-operative preparedness scores were more satisfied although surgical outcomes did not differ.
Keywords: Stress Incontinence, Mid-urethral Sling, Randomized Trial, Urodynamics, Satisfaction, Surgical Outcomes
Introduction
Patient reported outcomes (PROs) have gained increasing attention since traditional measures of objective cure and patient satisfaction frequently differ. Patient satisfaction is often strongly influenced by pre-treatment expectations. This is especially evident in reconstructive pelvic surgery where there is increasing interest in the importance of patient expectations and goal achievement when assessing surgical outcomes. Among women undergoing surgery for pelvic organ prolapse, goal achievement was significantly associated with improvement in condition specific QOL measures and maintained 1-3 years post-operatively [1]. Others have shown that patients who reported they were prepared for prolapse and/or continence surgery were more likely to be satisfied with surgery and show improvement in pre-surgical symptoms and QOL [2]. Conversely, short- and long-term dissatisfaction with surgery was associated with being “unprepared” for surgery [3, 4].
In this planned subanalysis of data from participants in the ValUE study, we examined whether preoperative preparedness was associated with surgical treatment outcomes, satisfaction and quality of life in women with uncomplicated stress urinary incontinence.
Materials and Methods
The design and primary results of the ValUE trial have been published [5, 6]. Briefly, women 21 years of age or older with predominant stress urinary incontinence (SUI) for at least 3 months without prior incontinence surgery were recruited from 11 clinical sites in the United States. Women who met inclusion criteria and desired surgery for SUI were offered participation after undergoing a provocative stress test confirming uncomplicated, demonstrable SUI. Peri-operative counseling, including plans for catheter management, were not standardized and left to the discretion of the local surgical team. After completing all baseline questionnaires and demonstrating a positive cough stress test on basic office evaluation, subjects were randomized to undergo either urodynamics (UDS group) or no UDS (Office Evaluation Only group) before surgery. Prior to randomization, the participant’s surgeon outlined the diagnosis and treatment plan based on the results of this evaluation. The institutional review boards at each site approved the study and all participants provided written informed consent for research.
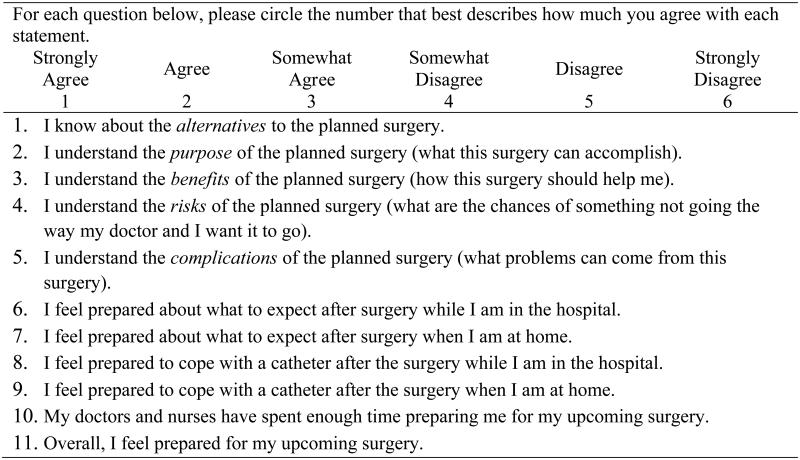
The primary outcome of the ValUE study, measured 12 months after surgery, included the Urogenital Distress Inventory (UDI) [3], a validated patient-reported measure of urinary incontinence, irritative and obstructive symptoms, and the Patient Global Impression – Improvement (PGI-I),[4] a validated patient-reported measure of perceived improvement after treatment of stress and urge incontinence. We defined primary outcome success as a reduction in the UDI score from baseline to 12 months of 70% or more and a PGI-I response of “very much better” or “much better” at 12 months. Secondary outcomes measured at 12 months were based on questionnaires which assessed incontinence severity (Incontinence Severity Index (ISI) [5] and Patient Global Impression of Severity (PGI-S))[7], self-reported incontinence symptoms (Medical, Epidemiologic, and Social Aspects of Aging Project (MESA))[6], and condition-specific quality of life (Incontinence Impact Questionnaire (IIQ-7))[3]. Patient satisfaction with treatment outcome was measured with a 5-point Likert scale (the range of responses were from “very dissatisfied” to “very satisfied”) that queried subjects to rate the treatment’s effect on overall incontinence, urge incontinence, stress incontinence, and urinary frequency. Subjects’ perception of preparedness for surgery was assessed prior to randomization using an 11-question Patient Preparedness Questionnaire (Figure 1) [2]. Women were categorized as “prepared” (those answering “strongly agree”) and “unprepared” (all other responses) based on their response to question 11 of the PPQ “Overall, I feel prepared for my upcoming surgery”. Although there are no fully validated patient preparedness scales, this scale has been previously reported in a population of women undergoing SUI and/or pelvic organ prolapse surgery. The original 11 question scale had responses ranging from 1=strongly agreed to 6=strongly disagreed; these were re-coded so that 0=strongly disagreed and 5=strongly agreed. Then, we calculated the mean of that scale, divided by the 5 point scale and multiplied by 100 and the resulting scale ranged from 0-100, with higher values indicating greater perceived preparedness.
Figure 1.
Patient Preparedness Questionnaire
Statistical analysis
Descriptive statistics were calculated to assess the level of pre-operative patient preparedness according to each preparedness question and by PPQ question 11 (percentage in each category). Spearman correlation coefficients (r2) were calculated to assess the magnitude of the relationship PPQ question 11 and other continuous measures including incontinence severity, satisfaction, and changes in PGI-S and IIQ scores from baseline;chi-squared tests were used to assess relationships with categorical variables (e.g. pre-operative urodynamic testing, primary outcome).
The mean (standard deviation) of the overall continuous preparedness scale was also presented; if a woman was missing a response to a particular preparedness question, then the scale was computed for only the preparedness questions that were non-missing. Pearson correlation coefficients (r) were calculated to assess the magnitude of the relationship between the continuous summary preparedness measure and continuously measured variables (e.g. baseline UDI, ISI, MESA stress, IIQ, PGI-S, satisfaction, changes in PGI-S and IIQ scores from baseline). A 5% two-sided significance level was used for all statistical testing. All statistical analysis was performed using SAS version 9.2.
Results
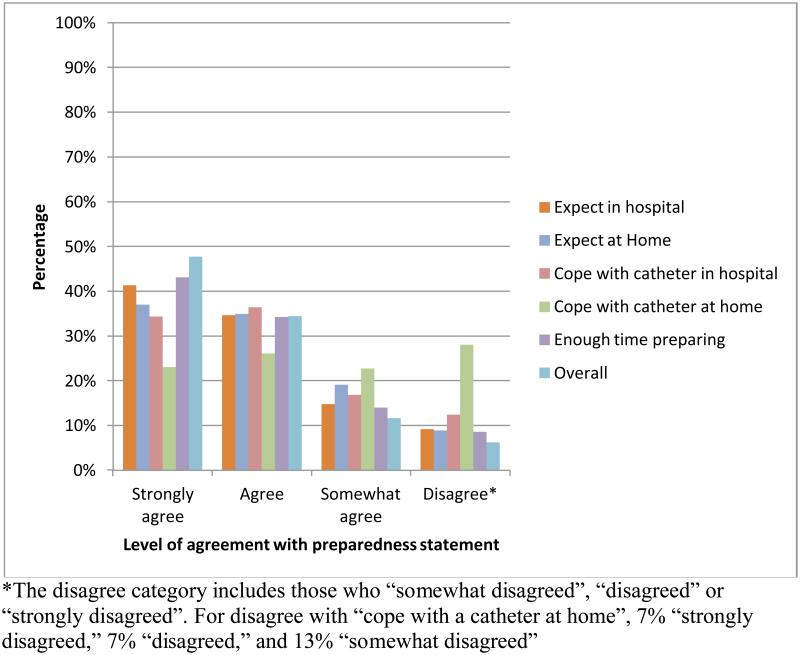
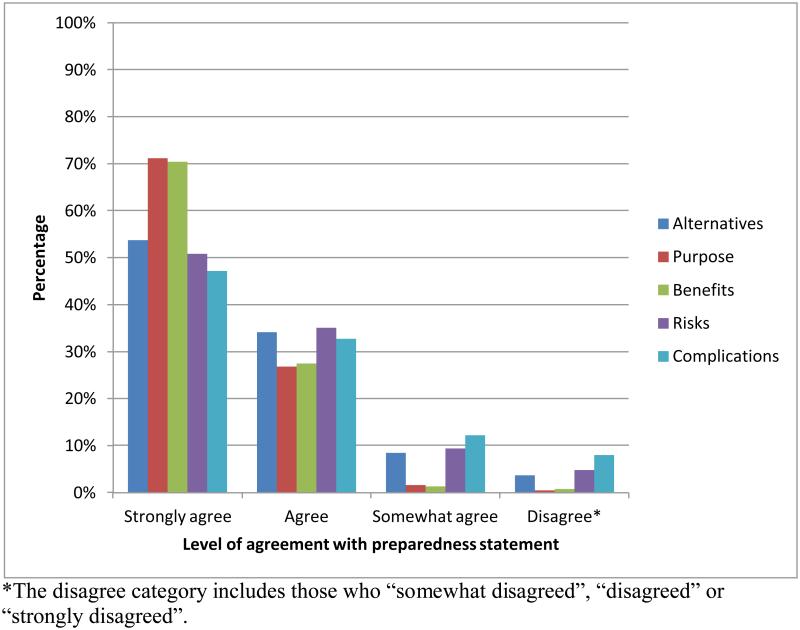
According to the preparedness question 11 of the PPQ, 300 (48%) answered that they “strongly agreed” that they felt prepared for their surgery; about 4 of 5 (81%) women reported that they “agreed” or “strongly agreed” that they felt prepared for their surgery. The question regarding feeling prepared to cope with a catheter after the surgery at home elicited the highest proportion of women not prepared (Figure 2; 7% “strongly disagreed,” 7% “disagreed,” and 13% “somewhat disagreed”). The patient-preparedness responses for the purpose, risks, benefits, complications and alternatives for surgery are shown in Figure 3. The majority of women “agreed” or “strongly agreed” that they were prepared and understood the purposes, risk, benefits, complications, and alternatives for the planned surgery (Figure 3).
Figure 2.
Patients’ preparedness for the planned surgery (responses from questions 6-11 listed in Figure 1)
Figure 3.
Patients’ understanding of the planned surgery (responses from questions 1-5 listed in Figure 1)
Selected clinical and demographic characteristics were not significantly different in women who reported they were not prepared compared to those who reported they were prepared (Table 1). Among the measures of baseline urinary incontinence symptoms we examined, total UDI score and PGI-S were associated with question 11 PPQ (Table 2), (p = 0.001 and p<0.001, respectively).
Table 1.
Patient Characteristics at Baseline By Preparedness Status.
| Prepared (n=300) |
Not Prepared (n=329) |
|||
|---|---|---|---|---|
| Characteristic | Mean (SD) or n (%) |
Mean (SD) or n (%) |
p-value | |
| Age (years) | 51.4 (10.2) | 51.4 (10.5) | 0.99 | |
| BMI (kg/m2)* | 29.7 (6.1) | 28.8 (6.0) | 0.08 | |
| Duration of incontinence (mos) |
92.4 (92.0) | 102.9 (86.2) | 0.14 | |
| Race/ethnicity | 0.51 | |||
| Hispanic | 50 (16.7) | 15 (4.6) | ||
| Non-Hispanic White | 216 (72.0) | 251 (76.3) | ||
| Non-Hispanic Black | 14 (4.7) | 22 (6.7) | ||
| Other | 20 (6.7) | 41 (12.5) | ||
| Number of pregnancies |
0.72 | |||
| 0 | 16 (5.3) | 12 (3.7) | ||
| 1 | 111 (37.0) | 127 (38.6) | ||
| 2 | 133 (44.3) | 142 (43.2) | ||
| 3+ | 40 (13.3) | 48 (14.6) | ||
| Menopausal status/HRT |
0.31 | |||
| Pre-menopausal | 116 (38.8) | 140 (42.7) | ||
| Peri or post- menopausal with HRT use |
52 (17.4) | 64 (19.5) | ||
| Peri or post- menopausal with no HRT use |
131 (43.8) | 124 (37.8) | ||
| Pelvic surgery | 0.47 | |||
| Yes | 214 (71.3) | 226 (68.7) | ||
| Urethral mobility | ||||
| Yes | 275 (91.7) | 296 (90.2) | 0.54 |
n=293 in the prepared group, n=319 in the unprepared group
Table 2.
Correlation between PPQ question 11 (single, dichotomous response) and measures of severity of urinary incontinence at baseline
| Measure | N | Spearman correlation coefficient, r2 |
p-value (for test of whether correlation differs from 0) |
|---|---|---|---|
| Total baseline UDI score |
629 | 0.13 | 0.001 |
| ISI scale | 623 | 0.07 | 0.10 |
| Baseline MESA stress score |
629 | 0.03 | 0.44 |
| Baseline total IIQ score |
629 | 0.06 | 0.11 |
| PGI-S | 626 | 0.15 | <0.001 |
There was no difference in the proportion of women who responded by the single question (PPQ, question 11) that they were prepared among those who achieved surgical treatment success compared to women who did not (48.1% and 46.8%, respectively, p=0.80). Also, when the secondary outcome of global improvement was used (“very much” better or “much” better on the PGI-I at 12 months), we saw no differences in the proportion of those considering themselves prepared between those with improvement and those without improvement (p=0.77). However, question 11 PPQ was associated with larger changes in patient-reported severity on the PGI-S from baseline to 12 months after treatment (p = 0.008). In addition, patients who reported higher levels of preparedness were more satisfied at 12 months (rs = 0.11, p = 0.02). Although participants did not complete another preparedness questionnaire after undergoing urodynamic testing, we also compared preparedness in the proportion of women randomized to subsequent preoperative UDS testing. The proportion of women who reported they were prepared (44.9%, PPQ question 11) was similar to that in women who were randomized to standardized office evaluation alone (50.5%, p=0.16).
After an exploratory factor analysis revealed that a factor involving all preparedness questions accounted for nearly 60% of the total correlation in the preparedness variables, we scored the measure as a continuous summary score of preparedness using all the questions. The PPQ was completed by all but one participant (n=629/630, 99.8%); most [622/630 (98.7%)] completed all 11 questions. Correlation coefficients between the individual questions of the PPQ varied from 0.22 – 0.91 with a Cronbach alpha value of 0.899, indicating a high level of internal consistency. The mean (± standard deviation) PPQ score was 82.7 (± 14.9). As when considering PPQ question 11, total baseline UDI score was positively associated with total PPQ score (Table 3). However, contrary to PPQ question 11, the PGI-S score was not positively associated with total PPQ score (p=0.13).
Table 3.
Association between total PPQ score and measures of incontinence severity at baseline
| Measure | N | Pearson correlation coefficient, r |
p-value (for test of whether correlation differs from 0) |
|---|---|---|---|
| Total baseline UDI score |
630 | 0.10 | 0.01 |
| ISI scale | 624 | 0.06 | 0.13 |
| Baseline MESA stress score | 630 | −0.01 | 0.81 |
| Baseline total IIQ score | 630 | 0.05 | 0.23 |
| PGI-S* | 627 | 0.06 | 0.13 |
Spearman correlation coefficient, r2, used here since PGI-S is not a continuous variable.
Total PPQ score was statistically significantly greater in women who achieved surgical treatment success compared to those who did not (83.6 ± 13.7 and 79.7 ± 18.7, respectively, p=0.03); this was in contrast to the result found when considering PPQ Question 11. Similar to Question 11 PPQ, changes in PGI-I and IIQ score were not correlated with total PPQ score (p= 0.35and p=0.23, respectively). Total PPQ score was also associated with larger changes in patient-reported severity on the PGI-S from baseline to 12 months after treatment (r2 = -0.09, p = 0.046) and patients who reported higher levels of preparedness were more satisfied at 12 months (r2= 0.09, p = 0.03). In addition, no significant difference on the continuous PPQ scale between the women randomized to subsequent UDS (81.7 ± 15.5) and those who had basic office evaluation alone (83.8 ± 14.2) (p = 0.09).
Discussion
Four out of five women who underwent anti-incontinence surgery as part of the ValUE study reported high levels of pre-operative preparedness. Studies of incontinence treatments have traditionally focused on objective outcomes such as information obtained from urodynamic studies and number of reported urinary incontinence episodes to define success. However, it has become increasingly apparent that patient perceived success and satisfaction are important measures to include when considering the broader impact of surgery on daily function, de novo pelvic floor symptoms [7], and postoperative healing [3]. Goal achievement, expectations, and preparedness for the surgical experience have also been shown to influence patient perception of surgical success [2-4, 8]. Such factors may be especially important in surgery for symptom driven conditions such as pelvic floor disorders including urinary incontinence and pelvic organ prolapse. Patient centered outcomes for pelvic floor disorders will take on greater importance as there is increasing emphasis on comparative efficacy trials [9]. Therefore, it is important that we understand peri-operative events that impact patient satisfaction, including pre-operative counseling and post-operative recovery course.
Although 4 of 5 women enrolled in ValUE study reported they were prepared for surgery, about one in four (27%) did not feel prepared to cope with a catheter at home. This is about twice the frequency previously reported among women (14%) undergoing reconstructive pelvic surgery [2]. Interestingly, “going home with a catheter,” which is not an uncommon event after pelvic floor surgery, was reported as a post-operative complication by 6% of the subjects in that study despite extensive counseling efforts. This is important when one considers the influence of patient perceived “complications” such as requiring a catheter, constipation, and urine leakage [2] on satisfaction, despite the fact that these events would not typically be classified as complications by a surgeon.
We found that urinary incontinence severity as measured by the UDI and PGI-S was correlated to preparedness level at baseline. It is possible that feeling prepared is related less to pre-operative counseling and more to patient comfort level with the decision to move forward with surgery due to more severe symptoms. However, our observation in this larger patient population contrasts with Kenton’s smaller study, which did not observe differences in symptom severity between women prepared and not prepared for pelvic surgery [2]. Finally, although preparedness was not significantly associated with treatment success after MUS surgery, preparedness scores were correlated with satisfaction at 12 months and also with greater improvement in PGI-S scores from baseline to 12 months.
Preparedness for anti-incontinence surgery appears related to a patient’s understanding of the purpose, risks, benefits, and complications [2]. It is also known that new pelvic symptoms are common after reconstructive surgery, and these symptoms (incontinence, urgency, difficult defecation, and voiding difficulty) are associated with decreased post-operative satisfaction [10-12]. Setting realistic patient expectations for improvement in their initial condition as well as the possibility of developing new symptoms may represent an opportunity to intervene and improve patient satisfaction. More focused education regarding post-operative recovery course may also influence patient confidence and overall perception of their surgical experience. Pre-operative patient education tools that describe what to expect both during and after surgery have been developed and tested in other specialties [13, 14] and demonstrated greater patient satisfaction and less anxiety compared to controls that received “routine” counseling.
A limitation of our study is the use of non-validated questionnaires to assess preparedness and surgical satisfaction. In addition, our study did not provide information on the effect of urodynamics on patient preparedness, as the preparedness questionnaire was not repeated after urodynamic testing. Given the main findings of the ValUE study and the costs of urodynamic testing in this population, it would seem reasonable to seek more cost-effective mechanisms of improving patient preparedness. Another limitation is that weak correlations seen may be secondary to the multiple comparisons done.
The strengths of our study include the randomized multi-center design, the large, well-defined surgical cohort, and the use of novel measures of patient preparedness and patient satisfaction. We showed that women with higher pre-operative preparedness scores were more satisfied with their incontinence surgery. Future studies are needed to identify approaches to enhance patient preparedness for surgery, to define the optimal pre-operative interventions, and their impact on patient readiness for surgery and to understand how these may influence surgical outcome.
Brief Summary (21/25): Approximately 4 in 5 (81%) of participants reported they were prepared for SUI surgery. Preparedness was positively associated with surgical satisfaction.
Acknowledgments
Supported by cooperative agreements from the National Institute of Diabetes and Digestive and Kidney Diseases, U01 DK58225, U01 DK58229, U01 DK58234, U01 DK58231, U01 DK60379, U01 DK60380, U01 DK60393, U01 DK60395, U01 DK60397, and U01 DK60401. Support was also provided by the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Following is a list of disclosures from the authors:
The following author is sponsored by the Department of Veterans Affairs and has a VA sponsored grant: Markland
The following authors do not have any disclosures to report: Drs. Brubaker, Casiano, Ghetti, Kusek, Litman, Paraiso, Dyer, Rahn
The following author is sponsored by Johnson & Johnson: Sirls
The following author is sponsored by Pfizer: Rickey
References
- 1.Hullfish KL, Bovbjerg VE, Steers WD. Patient-centered goals for pelvic floor dysfunction surgery: long-term follow-up. American Journal of Obstetrics & Gynecology. 2004;191:201–5. doi: 10.1016/j.ajog.2004.03.086. [DOI] [PubMed] [Google Scholar]
- 2.Kenton K, Pham T, Mueller E, Brubaker L. Patient preparedness: an important predictor of surgical outcome. American Journal of Obstetrics & Gynecology. 2007;197:654.e1–654.e6. doi: 10.1016/j.ajog.2007.08.059. [DOI] [PubMed] [Google Scholar]
- 3.Elkadry EA, Kenton KS, FitzGerald MP, Shott S, Brubaker L. Patient-selected goals: A new perspective on surgical outcome. Obstet Gynecol. 2003;189:1551–1557. doi: 10.1016/s0002-9378(03)00932-3. [DOI] [PubMed] [Google Scholar]
- 4.Mahajan ST, Elkadry EA, Kenton KS, Shott S, Brubaker L. Patient-centered surgical outcomes: The impact of goal achievement and urge incontinence on patient satisfaction one year after surgery. Amer J Obstet Gynecol. 2006;194:722–728. doi: 10.1016/j.ajog.2005.08.043. [DOI] [PubMed] [Google Scholar]
- 5.Nager CW, Brubaker L, Daneshgari F, Litman HJ, Dandreo KJ, Sirls L, et al. Design of the Value of Urodynamic Evaluation (ValUE) trial: A non-inferiority randomized trial of preoperative urodynamic investigations. Contemporary Clinical Trials. 2009;30:531–539. doi: 10.1016/j.cct.2009.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nager CW, Brubaker L, Litman HJ, Zyczynski HM, Varner RE, Amundsen C, et al. A Randomized Trial of Urodynamic Testing before Stress-Incontinence Surgery. N Engl J Med. 2012;366:1987–1997. doi: 10.1056/NEJMoa1113595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trabuco EC, Klingele CJ, Weaver AL, McGree ME, Lightner DJ, Gebhart JB. Preoperative and postoperative predictors of satisfaction after surgical treatment of stress urinary incontinence. Obstet Gynecol. 2011;204:444.e1–444.e6. doi: 10.1016/j.ajog.2010.12.037. [DOI] [PubMed] [Google Scholar]
- 8.Srikrishna S, Robinson D, Cardozo L. A longitudinal study of patient and surgeon goal achievement 2 years after surgery following pelvic floor dysfunction surgery. BJOG: An International Journal of Obstetrics & Gynaecology. 2010;117:1504–1511. doi: 10.1111/j.1471-0528.2010.02705.x. [DOI] [PubMed] [Google Scholar]
- 9.Fleurence R, Selby JV, Odom-Walker K, Hunt G, Meltzer D, Slutsky JR, et al. How The Patient-Centered Outcomes Research Institute Is Engaging Patients And Others In Shaping Its Research Agenda. Health Affairs. 2013;32:393–400. doi: 10.1377/hlthaff.2012.1176. [DOI] [PubMed] [Google Scholar]
- 10.Pham T, Kenton K, Mueller E, Brubaker L. New pelvic symptoms are common after reconstructive pelvic surgery. American Journal of Obstetrics & Gynecology. 2009;200:88.e1–88.e5. doi: 10.1016/j.ajog.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 11.Elkadry EA, Kenton KS, FitzGerald MP, Shott S, Brubaker L. Patient-selected goals: a new perspective on surgical outcome. American Journal of Obstetrics & Gynecology. 2003;189:1551–7. doi: 10.1016/s0002-9378(03)00932-3. discussion 1557-8. [DOI] [PubMed] [Google Scholar]
- 12.Richter HE, Diokno A, Kenton K, Norton P, Albo M, Kraus S, et al. Predictors of treatment failure 24 months after surgery for stress urinary incontinence. J Urol. 2008;179:1024–30. doi: 10.1016/j.juro.2007.10.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crabtree TD, Puri V, Bell JM, Bontumasi N, Patterson GA, Kreisel D, et al. Outcomes and Perception of Lung Surgery with Implementation of a Patient Video Education Module: A Prospective Cohort Study. J Am Coll Surg. 2012;214:816–821.e2. doi: 10.1016/j.jamcollsurg.2012.01.047. [DOI] [PubMed] [Google Scholar]
- 14.Pager C. Randomised controlled trial of preoperative information satisfaction with cataract surgery. BJOG: an International Journal of Obstetrics & Gynaecology. 2005;89:10–13. doi: 10.1136/bjo.2004.048637. [DOI] [PMC free article] [PubMed] [Google Scholar]