Abstract
Purpose
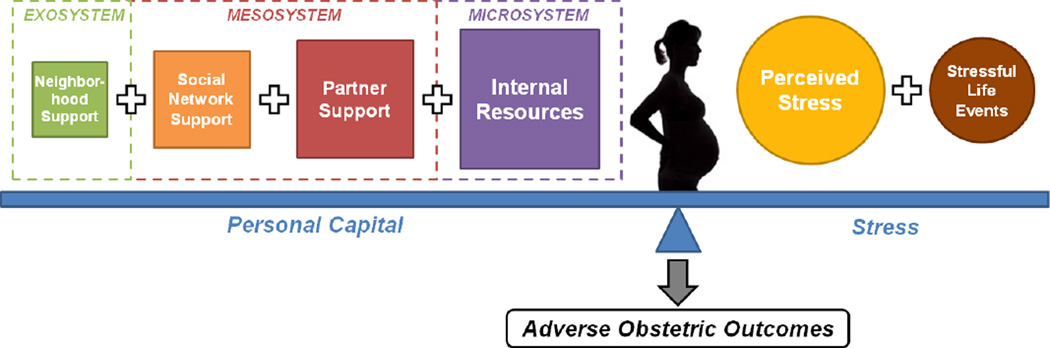
Stress during pregnancy is a salient risk factor for adverse obstetric outcomes. Personal capital during pregnancy, defined as internal and social resources that help women cope with or decrease their exposure to stress, may reduce the risk of poor obstetric outcomes.
Methods
Using data from the 2007 Los Angeles Mommy and Baby (LAMB) survey (N=3,353), we examined the relationships between the balance of stress and personal capital during pregnancy, or the Stress-to-Capital Ratio (SCR), and adverse obstetric outcomes ((i.e., pregnancy complications, preterm birth (PTB), low birthweight (LBW), and small-for-gestational-age (SGA)).
Results
Women with a higher SCR (i.e. greater stress relative to personal capital during pregnancy) were significantly more likely to experience at least one pregnancy complication, PTB, and lower gestational age, but not LBW or SGA. Accounting for pregnancy complications completely mediated the association between the SCR and PTB.
Conclusions
Our findings indicate that experiencing greater stress relative to personal capital during pregnancy is associated with an increased risk for pregnancy complications, PTB, and lower gestational age and that pregnancy complications may be a mechanism by which the SCR is related to adverse obstetric outcomes.
Keywords: Personal capital, maternal stress, obstetric outcomes, preterm birth, pregnancy complications
Introduction
In the United States, adverse obstetric outcomes, including pregnancy complications, preterm birth (PTB), low birthweight (LBW), and small-for-gestational-age (SGA), account for over 40 percent of all neonatal deaths (Heron 2012) and have contributed to significant increases in childhood morbidity in recent decades (Hack et al. 1995; Kramer 2003; McCormick 1985). Mounting evidence suggests that stress during pregnancy is a salient risk factor for poor obstetric outcomes (Dole et al. 2003; Rondo et al. 2003). However, studies have largely employed uni-dimensional stress measures, such as perceived stress or stressful life events (Sable & Wilkinson 2000; Zhu et al. 1999). Furthermore, very few studies have examined the components of personal capital during pregnancy, or the resources that may help women cope with or decrease their exposure to stress during pregnancy (Wakeel et al. 2013), and none have explored personal capital as a composite construct that is related to obstetric outcomes. Importantly, no study has examined the relationship between stress, personal capital and obstetric outcomes. Therefore, we created and employed a conceptually-based ratio of stress and personal capital, or the Stress-to-Capital Ratio (SCR), to determine if and how the balance between these two factors during pregnancy was associated with obstetric outcomes.
Theory suggests that stress is a process by which environmental stimuli (e.g. stressful life events) may overwhelm an individual’s coping resources (Cohen & Williamson 1987), leading to the perception of stress and subsequent physiological responses that attempt to gain homeostasis (McEwen 1998). Physiological responses to stress that have been shown to directly impact obstetric outcomes primarily entail the neuroendocrine and immune/inflammatory processes (Coussons-Read et al. 2005, 2007; Dunkel-Schetter 2011; Gennaro & Hennessy 2003; Steer 2005; Wadhwa et al 1998, 2001, 2004). Additionally, the two pathways most likely interact with each other in that the combination of chronic stress and infectious pathogens has an additive impact, resulting in shortened gestational length (Wadhwa et al. 2001).
Personal capital is a multidimensional set of resources that may help women cope with or reduce their exposure to stress during pregnancy (Wakeel et al. 2013), yet as defined, it has been under-explored in the literature and has not been tied to obstetric outcomes. We posit that personal capital may operate on multiple levels (Bronfenbrenner 1977, 1979) to increase the likelihood of favorable obstetric outcomes. At the individual level, internal resources (i.e., self-esteem and mastery) have been associated with higher infant birthweight (Rini et al. 1999) and decreased risk of intrauterine growth retardation (IUGR) (Goldenberg et al. 1991). At the interpersonal level, social resources, including partner support and social network support, have been linked to increased fetal growth, better labor progress, higher birthweight, and higher infant APGAR scores (Collins et al. 1993; Feldman et al. 2000). At the community level, neighborhood support may play an indirect role in lowering women’s risk of adverse obstetric outcomes (Bell et al. 2006). As previous studies have provided evidence of the independent effects of personal capital components on obstetric outcomes, we expand this work by incorporating these critical resources into a unified construct to comprehensively capture the available resources that women may garner during pregnancy.
Although stress and components of personal capital have been shown to be associated with obstetric outcomes, there is a paucity of research examining the relationships among stress, personal capital, and outcomes. To our knowledge, our study is the first to examine the balance of stress and personal capital during pregnancy in relation to subsequent obstetric outcomes. Our research draws upon Misra et al.’s (2003) framework of perinatal health, which integrates the life-course model (Halfon & Hochstein 2002) with the multiple determinants of health theory (Evans & Stoddard 1990), as well as stress theory (House 1974). The life-course model posits that perinatal health is influenced by cumulative effects of events across the lifespan as well as intergenerational effects, while the multiple determinants of heath theory proposes that a combination of interrelated biological, psychological, behavioral, social and environmental factors contributes to health outcomes. Additionally, stress theory (Lazarus & Folkman 1984) contends that both maternal risks (e.g. stress) and resources (e.g. personal capital) likely influence obstetric outcomes and that greater risks relative to resources may lead to deleterious obstetric outcomes. Overall, we posit that stress and personal capital likely accumulate over the life-course from multiple sources and modify each other in impacting obstetric outcomes. Consequently, we operationalized the relationship between stress and personal capital as a ratio that captures the continuum of the relative levels of these two factors during pregnancy, rather than examining the interaction between stress and personal capital, which ignores stress relative to personal capital and instead only captures concurrent increases or decreases in these two constructs. Therefore, the aims of this paper were to: 1) create a Stress-to-Capital Ratio (SCR) which empirically represents the level of balance between stress and personal capital during pregnancy; and 2) examine the relationships between the SCR and the risk of adverse obstetric outcomes, specifically pregnancy complications, PTB, LBW, and SGA.
Materials and Methods
Sample
Data are from 3,353 women who participated in the 2007 LAMB study, a cross-sectional, population-based study that examined preconception, prenatal, and postpartum correlates of adverse MCH outcomes. Eligible mothers were Los Angeles County residents who had given birth to a live-born infant in Los Angeles County in 2007.
The 2007 LAMB Study was a collaboration between the University of California, Los Angeles (UCLA) and the Los Angeles County Department of Maternal, Child and Adolescent Health. They employed a stratified random sample, selected by sampling neighborhoods based on census tracts and then sampling births within the neighborhoods, resulting in a sample of 4,518 women. The response rate for the Los Angeles County sample was 56%, after adjusting for faulty addresses, language issues, maternal deaths, and loss to follow-up due to inability to locate the respondent.
Respondents with missing values for personal capital (n=762), stress (n=467), and prenatal depressive symptoms (n=113) variables were removed by listwise deletion, resulting in a sample size of 3,411 women. Furthermore, as 99 of these mothers had gestational age data that was either missing (n=90) or deemed illogical (n=9) (i.e., values <100 days or >365 days), we imputed for this variable based on estimated dates of conception and infant birth data. We used only estimated gestational age values that were logical (100–365 days), resulting in a final sample size of 3,353 women for the present analyses.
We compared the sociodemographic characteristics and obstetric outcomes of women with missing data (n=985) and women with complete data (n=3,353). Women with missing data were significantly more likely to be Hispanic, unmarried, low-income, less educated; there were no significant differences in obstetric outcomes among the two groups.
Procedures
In 2007, over 10,000 surveys were mailed to eligible women within six months after delivery. The recruitment process entailed a(n): 1) mailed preletter four months after childbirth; 2) initial mailed questionnaire one week later; 3) mailed reminder one week later; 4) second mailed questionnaire two weeks later (if needed); and 4) telephone follow-up two weeks later (if needed). Finally, the data from the completed surveys were linked to corresponding California birth certificates prior to analyses.
The survey was approved in 2007 by both the Los Angeles County Department of Public Health and UCLA Institutional Review Boards and therefore has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Measures
Outcome variables
Poor obstetric outcomes included pregnancy complications, PTB, LBW, and SGA. Pregnancy complications, which included pregnancy-induced hypertension, gestational diabetes, premature labor (i.e., labor that began <37 weeks gestation), premature rupture of membranes (i.e., membrane rupture occurring <37 weeks gestation), bacterial vaginosis, and kidney or bladder infection during pregnancy, were dichotomized as either experiencing any versus no complication. Three gestational age categories were used, including PTB (i.e., delivery occurring before 259 days of gestation), early-term birth (i.e., delivery occurring between 259 and 272 days), and late-term birth (i.e., delivery occurring at or after 273 days). Preterm and early-term births were compared with late-term births. Infants weighing less than 2,500 grams at birth were considered to be LBW and were compared with normal-weight infants (i.e., weighing 2,500–4,000 grams). Using Olsen et al.’s (2010) gender-specific growth curves, we defined SGA infants as those weighing less than 10% of the birthweight of infants of their gender and gestational age and compared them with appropriate-for-age infants (i.e., weighing above the 10th percentile for their age and gender). Infant birthweight, gestational age, and gender were obtained from birth records; pregnancy complications were self-reported in the LAMB survey.
Stress and personal capital measures
Stress was operationalized as perceived stress and severe stressful life events during pregnancy (Appendix A). Perceived stress items (e.g. feeling sad) assessed psychological stress during pregnancy and inquired about the degree to which the respondent appraised her life as stressful (Cohen et al. 1983). Severe stressful life events measured environmental stress and included events (e.g. death of a loved one) that have been shown to impact obstetric outcomes (Newton and Hunt 1984).
Appendix A.
Stress and Personal Capital Items Included in the Stress-to-Capital Ratio (SCR)
| Measure | Origin of Scale | Items in Measure | Possible Responses | |
|---|---|---|---|---|
| Stress Index | ||||
| Perceived Stress |
LAMB 9-item version of Cohen’s Perceived Stress Scale (PSS)1 |
Never; Occasionally; Fairly often; Always |
||
| How much of the time, during your most recent pregnancy, had you: |
||||
| Been a very nervous person; felt calm and peaceful*; felt sad; been a happy person*; been upset because of something that happened unexpectedly; felt that you were unable to control the important things in your life; felt that things were going your way*; felt difficulties were piling up |
||||
| so high that you could not overcome them; felt so down in the dumps that nothing could cheer you up? |
||||
| Severe Life Events |
Subset of LAMB 14-item stressful life events list, adapted from modified life event inventory in Pregnancy Risk Assessment Monitoring System (PRAMS)2 |
During pregnancy, did these events happen to you? |
Yes; No | |
| You got separated or divorced from your husband or partner; were homeless; lost your job even though you wanted to go on working; were in a physical fight; your husband or partner lost his job; you or your husband or partner went to jail; someone close and important to you died. |
||||
| Personal Capital Index | ||||
| Internal Resources |
Here is a list of statements dealing with your feelings about yourself during your last pregnancy |
Strongly disagree; Disagree; Neither disagree nor agree; Agree; Strongly agree |
||
| Selfesteem | 3-item Rosenberg Self-Esteem Scale Short Form3 |
On the whole, I am satisfied with myself; feel that I’m a person of worth, at least on an equal plane with others; am able to do things as well as most other people. |
||
| Mastery | 4-item Pearlin Mastery Scale Short Form3 |
I have little control over the things that happen to me*; there is really no way I can solve some of the problems I have*; sometimes I feel that I am being pushed around in life*; I can do just about anything I really set my mind to do. |
||
| Partner Support |
Fragile Families Study4 | Yes; No | ||
| During your last pregnancy, did the baby’s father do any of the following? |
||||
| Gave you money or brought things for you; helped you in other ways, such as taking you to the doctor or helping with chores; gave you emotional support in labor; visited you and the baby at the hospital after the delivery; wanted to put his name on the baby’s birth certificate as the father; said he wanted to help you raise your child in the coming years. |
||||
| Social network Support |
PRAMS5 | During your last pregnancy, how often would you get these kinds of supports, if you needed them? |
Never; Rarely; Sometimes; Most of the time; All the time |
|
| Someone to loan me $50; help me if I were sick and needed to be in bed; take me to the clinic or doctor if I needed a ride; give me a place to live; help me with babysitting or child care; help me with household chores; talk to about my problems. |
||||
| Neighborho od Support |
Project on Human Development in Chicago Neighborhoods (PHDCN)6 |
|||
| Social Cohesion |
Do you agree that people in your neighborhood… |
Strongly disagree; Disagree; Neutral; Agree; Strongly agree |
||
| Are willing to help their neighbors; this is a close-knit (tight) neighborhood; can be trusted; generally, don’t get along with each other*; do not share the same values*. |
||||
| Reciprocal Exchange |
And how often do your neighbors… |
Never; Almost never; Sometimes; Fairly often; Very often |
||
| Do favors for each other; ask each other advice about personal things such as child rearing or job openings; have parties or other get-togethers where other people in the neighborhood are invited; visit in each other’s homes or on the street; watch over each other’s property? |
||||
Reverse-coded items
Cohen et al., 1983;
Personal capital was operationalized as internal resources, partner support, social network support and neighborhood support during pregnancy (Appendix A). Internal resources included self-esteem and mastery. Self-esteem (e.g. overall satisfaction with self) was defined as a “positive or negative orientation toward oneself or an overall evaluation of one’s worth or value.” (Jesse et al. 2006: 70). Mastery (e.g. being able to do anything she sets her mind to do) embodied the belief that one has control over her life (Rini et al. 1999). Partner support encompassed instrumental (e.g. financial support) and emotional support from the baby’s father (Fragile Families Study 2003). Social network support included support (e.g. having someone help with childcare) from kin and close friends (Adams et al. 1991). The neighborhood support items concerned neighborhood social cohesion (e.g. being a close-knit neighborhood) and reciprocal exchange (e.g. neighbors visiting each other’s homes) (Buka et al. 2003).
Stress-to-Capital Ratio (SCR)
The relationship between stress and personal capital was operationalized as a ratio in order to capture the continuum of women’s relative levels of stress and personal capital. Testing the interaction between stress and personal capital was not performed as an interaction term ignores stress relative to personal capital and instead only captures concurrent increases or decreases in these two constructs. Therefore, we argue that an interaction between these constructs is neither practically relevant nor a sufficient answer to our research question; as such, only the method of the SCR was employed in this study.
Prior to the creation of the SCR, items within the stress and personal capital measures were summed to create raw overall scores for each measure, with higher scores reflecting greater levels of that measure. Based on theory (Figure 1), weighting schemes were applied to the variables that contributed to the composite measures of stress and personal capital. For the composite stress measure, perceived stress was weighted twice as heavily (67%) as severe life events (33%) because while life events may not render the same impact on all individuals, the subjective appraisal of stress arguably has a more direct effect on mental health during pregnancy as well as the behavioral and biological pathways leading to adverse obstetric outcomes (Ayers 2001; Dole et al. 2003; Hedegaard et al. 1996; Lazarus & Folkman 1984, Lobel et al. 1992). Additionally, severe life events are rare shocks, whereas perceived stress is likely to be persistent and chronic (Lobel & Dunkel-Schetter 1990). Furthermore, for the composite personal capital measure, proximal (i.e., internal) resources were weighed more heavily than distal (i.e., social) resources, as they were posited to have a more direct impact on the individual (Cohen & Wills 1985; Hobfoll et al. 1987; Hobfoll 2002). As such, internal resources, partner support, social network support, and neighborhood support comprised 32.5%, 27.5%, 22.5%, and 17.5%, respectively, of the overall personal capital score. The weighted composite measures for stress and personal capital were constructed such that the scores ranged from 1 to 100.
Figure 1. A Conceptual Framework for the Relationship between the Balance of Personal Capital and Stress during Pregnancy and Adverse Obstetric Outcomes.
The figure illustrates the balance between personal capital and stress during pregnancy. The personal capital score was created using a weighting scheme based on Bronfenbrenner’s ecological model and comprised internal resources, partner support, social network support, and neighborhood support. Proximal resources were weighed more heavily than distal resources as they were posited to have a larger and more direct impact on the individual. As such, internal resources, partner support, social network support, and neighborhood support comprised 32.5%, 27.5%, 22.5%, and 17.5%, respectively, of the overall score. Further, for the composite stress measure, perceived stress was weighted twice as heavily (67%) as severe life events (33%) because while life events may not render the same impact on all individuals, the subjective appraisal of stress arguably has a more direct effect on mental health during pregnancy as well as the behavioral and biological pathways leading to adverse obstetric outcomes. Additionally, severe life events are rare shocks, whereas perceived stress is more likely to be persistent and chronic. Therefore, the figure graphically depicts how each component was weighted and then summed to create the composite measures of personal capital and stress. Finally, the balance between personal capital and stress (empirically captured by the Stress-to-Capital Ratio) is hypothesized to lead to adverse obstetric outcomes.
Two sensitivity analyses were performed to examine the assumptions used in the weighting schemes for personal capital and stress. First, twenty weighting schemes (based on five schemes for stress and four schemes for personal capital) were empirically tested by evaluating the predictive ability of each scheme for the outcomes under investigation. This analysis showed that the results did not substantially vary across these weighting schemes. Second, we conducted confirmatory factor analysis (CFA) using Mplus 7 (Muthen and Muthen, Los Angeles, CA). The standardized factor loadings from our CFA, which included personal capital and stress as two latent factors with their respective components, confirmed our chosen weighting schemes for personal capital and stress (data available upon request). Based on the results from these analyses, the weighting scheme with the best predictive ability was chosen as the final scheme.
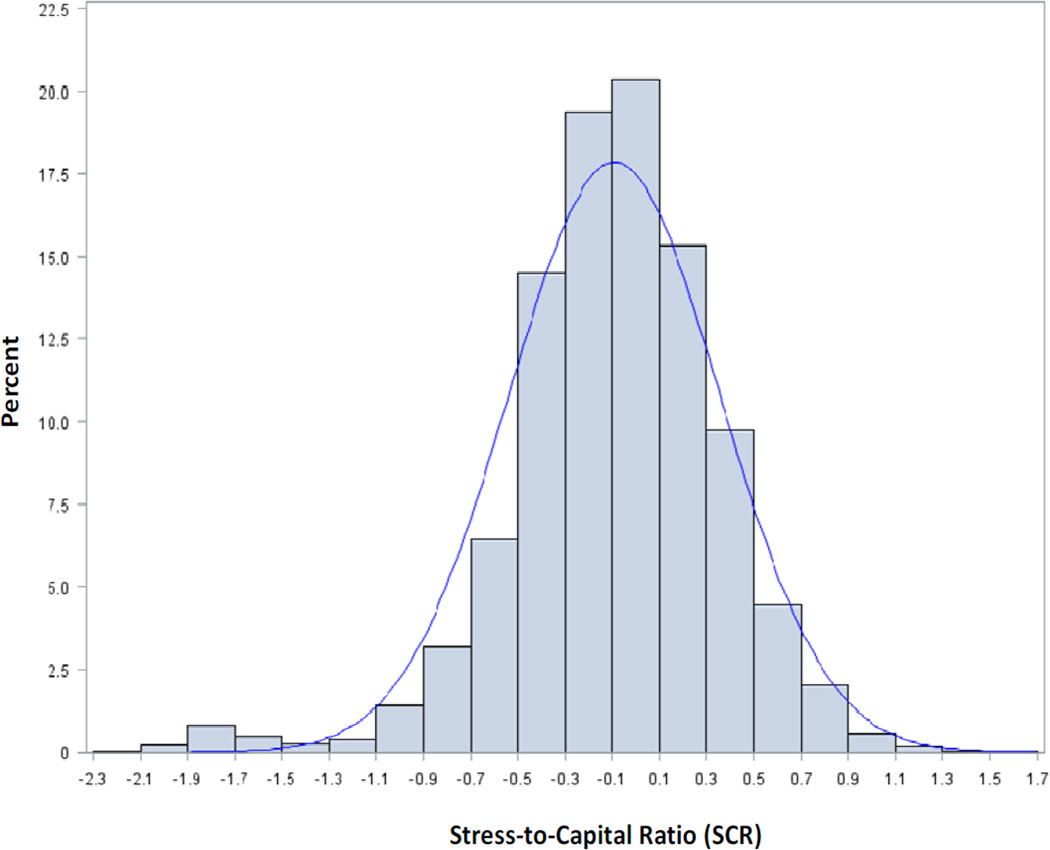
In order to create the SCR, the finalized weighted composite measures of stress and personal capital were standardized. First, various cumulative distribution functions for the stress and personal capital measures were examined for the best possible fit. The weighted composite score for stress followed a Gamma distribution, and the weighted composite score for personal capital followed a Beta distribution. The probability of each weighted score was calculated based on the appropriate distribution, and this probability was applied to a Normal/Gaussian distribution (mean of 50, standard deviation of 10) to determine the standardized score. The standardized stress score was then divided by the standardized personal capital score to derive the raw SCR. Finally, the raw SCR was natural log transformed in order to ensure a symmetric distribution for the final SCR (Figure 2). An SCR greater than zero indicated greater stress relative to personal capital during pregnancy.
Figure 2. Distribution of the Stress-to-Capital Ratio (SCR) for 2007 LAMB Study Respondents.
Legend: The histogram illustrates the distribution of the Stress-to-Capital Ratio (SCR) scores for the 2007 LAMB study respondents. The blue curve represents a normal distribution fit to the mean and standard deviation of the SCR. The mean SCR for the sample was −0.09, with a standard deviation of 0.45.
Control variables
The multivariate analyses controlled for maternal race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Asian/Pacific Islander, Native American), age (continuous), education (≥12 versus <12 years of schooling), annual household income (≤$19,000, $20,000-$39,000, $40,000-$59,000, $60,000-$99,000, ≥$100,000), marital status (married, single/never married, separated/divorced/widowed, cohabiting), prenatal depressive symptoms (yes versus no), the number of prior children ≤5 years old (continuous), parity (primaparous versus multiparous), and pre-pregnancy health conditions (i.e., hypertension and diabetes) (yes versus no) and depression (yes versus no). Further, to capture contextual neighborhood effects, we adjusted for geographic region of residence within Los Angeles County, or service planning area (SPA; Antelope Valley, San Fernando Valley, San Gabriel Valley, Metro Los Angeles, West, South, East, and South Bay). Data for race/ethnicity, age, education, and SPA were obtained from birth certificates, whereas data for the other control variables were self-reported in the survey.
Analytic Approach
Analyses were conducted using SAS 9.3 (SAS Institute Inc, Cary, NC) and were weighted to account for sampling design and survey non-response. First, in order to determine the levels of stress and personal capital within the sample, the means of the raw, weighted, and standardized scores for each stress and personal capital measure as well as the raw and log-transformed final SCR’s were calculated; reliability statistics (i.e., Cronbach’s alphas) were also computed for the overall measures and components of stress and personal capital. Second, bivariate comparisons were made between sociodemographic, health, and obstetric characteristics and the SCR; Table 1 shows comparisons of the mean SCR by the independent and dependent variables, while Tables 3 and 4 include comparisons of the mean SCR and covariates by obstetric outcomes. Third, multivariable logistic regression models were developed to examine the relationships between the SCR and pregnancy complications, LBW, and SGA. Multinomial logistic regression models were employed to investigate the relationship between the SCR and the gestational age categories (i.e., PTB versus late-term birth; early-term birth versus late-term birth). Additionally, Sobel tests (Baron & Kenny 1986) were performed to test for the potential mediating role of pregnancy complications in the associations between the SCR and PTB, LBW, and SGA. Finally, we conducted multivariable linear regression to examine the relationships between the SCR and gestational age and birthweight as continuous outcomes.
Table 1.
Weighted Means of Stress-to-Capital Ratio Scores by Selected Maternal Sociodemographic and Health Characteristics, 2007 LAMB Study
| Stress-to-Capital Ratio | ||||
|---|---|---|---|---|
| Total | Mean/% | Mean | SD | p-value |
| Unweighted n=3,353 |
−0.09 | 0.45 | ||
| Weighted n=246,286 |
−0.07 | 0.46 | ||
| Sociodemographic factors | ||||
| Age | 27.9 | |||
| ≤18 | 7.4% | 0.07 | 0.34 | *** |
| 19–34 | 75.8% | −0.07 | 0.46 | Ref |
| ≥35 | 16.8% | −0.16 | 0.49 | *** |
| Race/ethnicity | ||||
| Non-Hispanic White | 13.1% | −0.18 | 0.49 | Ref |
| Non-Hispanic Black | 4.7% | 0.02 | 0.54 | *** |
| Hispanic | 71.9% | −0.06 | 0.44 | *** |
| Asian/Pacific Islander | 9.6% | −0.10 | 0.44 | * |
| Native American | 0.7% | −0.04 | 0.52 | NS |
| Annual household income | ||||
| <$20,000 | 42.8% | 0.05 | 0.42 | *** |
| $20,000-$39,000 | 23.0% | −0.12 | 0.45 | ** |
| $40,000-$59,000 | 9.3% | −0.12 | 0.42 | * |
| $60,000-$99,000 | 10.4% | −0.21 | 0.44 | Ref |
| >$ 100,000 | 9.4% | −0.30 | 0.48 | ** |
| Unknown | 5.1% | −0.06 | 0.51 | *** |
| Education | ||||
| ≤12 years (no HS diploma/GED) | 33.0% | −0.04 | 0.42 | * |
| ≥HS diploma/GED | 65.0% | −0.09 | 0.47 | Ref |
| Unknown | 2.0% | −0.06 | 0.42 | NS |
| Marital status | ||||
| Married | 54.5% | −0.19 | 0.47 | Ref |
| Separated/Divorced/Widowed | 2.9% | 0.37 | 0.40 | *** |
| Single/never married | 11.2% | 0.23 | 0.43 | *** |
| Cohabiting | 30.6% | −0.01 | 0.38 | *** |
| Unknown | 0.8% | 0.05 | 0.47 | ** |
| Service Planning Area (SPA) | ||||
| 1 (Antelope Valley) | 2.5% | 0.08 | 0.56 | *** |
| 2 (San Fernando Valley) | 21.0% | −0.13 | 0.47 | NS |
| 3 (San Gabriel Valley) | 18.8% | −0.07 | 0.44 | NS |
| 4 (Metro Los Angeles) | 9.9% | −0.07 | 0.46 | NS |
| 5 (West) | 2.5% | −0.16 | 0.58 | Ref |
| 6 (South) | 15.0% | −0.02 | 0.42 | ** |
| 7 (East) | 14.0% | −0.05 | 0.43 | * |
| 8 (South Bay) | 16.3% | −0.09 | 0.48 | NS |
| Health factors | ||||
| Pre-pregnancy depression | *** | |||
| Yes | 14.9% | 0.26 | 0.39 | |
| No | 85.1% | −0.13 | 0.45 | |
|
Pre-pregnancy health conditions (hypertension or diabetes) | ||||
| Yes | 5.1% | 0.05 | 0.40 | |
| No | 94.9% | −0.08 | 0.47 | |
| Prenatal depressive symptoms | *** | |||
| Yes | 20.0% | 0.30 | 0.34 | |
| No | 80.0% | −0.17 | 0.44 | |
| Other control variables | ||||
| Parity | NS | |||
| Primaparous (no prior births) | 37.7% | −0.08 | 0.45 | |
| Multiparous (≥1 prior birth) | 62.3% | −0.07 | 0.47 | |
| Number of prior children under age 5 | ||||
| 0 | 58.8% | −0.08 | 0.46 | Ref |
| 1 | 35.1% | −0.08 | 0.47 | NS |
| ≥2 | 6.1% | 0.04 | 0.47 | *** |
| Obstetric outcomes | ||||
| Pregnancy complications | *** | |||
| Any (≥1) | 44.3% | −0.02 | 0.45 | |
| None (0) | 55.7% | −0.12 | 0.47 | |
| Gestational age | 272.8 days | |||
| Preterm (<259 days) | 12.7% | 0.00 | 0.48 | *** |
| Early-term (259–272 days) | 29.4% | −0.07 | 0.45 | NS |
| Late-term (>273 days) | 57.9% | −0.09 | 0.47 | Ref |
| Birthweight | 3,284.9 grams | |||
| Low (<2,500 grams) | 7.5% | −0.05 | 0.51 | NS |
| Normal (2,500–4,000 grams) | 84.1% | −0.08 | 0.46 | Ref |
| High (<4,000 grams) | 8.3% | −0.06 | 0.41 | NS |
| Small-for-gestational age | NS | |||
| Yes | 10.5% | −0.07 | 0.48 | |
| No | 89.5% | −0.07 | 0.46 | |
Note: Weighted means and percentages accounted for sampling design and survey non-response. Ref - reference category; NS –not significant; p≥0.05;
p<0.05;
p<0.01;
p<0.001
Table 3.
Characteristics of 2007 LAMB Study Respondents by Pregnancy Complications and Multivariate Analysis of the Odds of Any Complications
| Any complication (vs. None) | |||||
|---|---|---|---|---|---|
| Total | Any complications | No complications |
|||
| Mean/% | Mean/% | AOR | 95% CI | ||
| TOTAL: | |||||
| Weighted | 246,286 | 109,218 | 137,068 | ||
| Weighted % | 100% | 44.3% | 55.7% | ||
| TOTAL: | |||||
| Unweighted | 3,353 | 1,497 34 | 1,856 | ||
| Unweighted % | 100% | 44.6% | 55.4% | ||
| Stress-to-Capital Ratioc | −0.02 | −0.12 | 1.35 | 1.10, 1.65 | |
| Sociodemographic characteristics | |||||
| Age | 27.9 | 27.9 | 1.0 1 | 0.99, 1.03 | |
| Race/ethnicityc | |||||
| Non-Hispanic Whiteb | 11.3% | 14.5% | 1.0 0 | Refer ence | |
| Non-Hispanic Blackb | 5.8% | 3.8% | 1.79 | 1.24, 2.58 | |
| Hispanic | 73.3% | 70.8% | 1.22 | 0.97, 1.53 | |
| Asian/Pacific Islander | 8.8% | 10.3% | 1.05 | 0.80, 1.39 | |
| Native American | 0.8% | 0.6% | 1.01 | 0.45, 2.25 | |
| Annual household incomea | |||||
| <$20,000 | 44.5% | 41.5% | 1.2 3 | 0.93, 1.63 | |
| $20,000-$39,000 | 23.4% | 22.7% | 1.28 | 0.97, 1.68 | |
| $40,000-$59,000 | 9.5% | 9.2% | 1.28 | 0.94, 1.73 | |
| $60,000-$99,000a | 9.1% | 11.4% | 1.00 | Reference | |
| >$100,000b | 8.0% | 10.6% | 0.99 | 0.74, 1.33 | |
| Unknown | 5.5% | 4.6% | 1.45 | 0.92, 2.26 | |
| Educationa | |||||
| ≤12 years (no HS diploma/GED) | 33.0% | 33.0% | 0.93 | 0.76, 1.14 | |
| ≥HS diploma/GED | 64.1% | 65.7% | 1.00 | Reference | |
| Unknownb | 2.9% | 1.3% | 2.19 | 1.21, 3.95 | |
| Marital statusa | |||||
| Marrieda | 52.2% | 56.4% | 1.00 | Reference | |
| Separated/Divorced/Widowed | 3.4% | 2.5% | 1.09 | 0.64, 1.85 | |
| Single/never marrieda | 12.9% | 9.9% | 1.06 | 0.80, 1.41 | |
| Cohabiting | 30.8% | 30.4% | 0.96 | 0.78, 1.17 | |
| Unknown | 0.7% | 0.9% | 0.76 | 0.30, 1.93 | |
| Service PlanninR Area (SPA) | |||||
| 1 (Antelope Valley) | 3.0% | 2.2% | 1.39 | 0.83, 2.35 | |
| 2 (San Fernando Valley) | 21.6% | 20.5% | 1.29 | 0.88, 1.90 | |
| 3 (San Gabriel Valley) | 18.0% | 19.4% | 1.10 | 0.74, 1.64 | |
| 4 (Metro Los Angeles) | 9.3% | 10.3% | 1.04 | 0.68, 1.61 | |
| 5 (West) | 2.1% | 2.8% | 1.00 | Reference | |
| 6 (South) | 14.8% | 15.2% | 1.04 | 0.68, 1.60 | |
| 7 (East) | 13.5% | 14.4% | 1.10 | 0.73, 1.66 | |
| 8 (South Bay) | 17.7% | 15.2% | 1.31 | 0.88, 1.94 | |
| Other control variables | |||||
| Pre-pregnancy depressionc | |||||
| Yes | 18.0% | 12.5% | 1.1 9 | 0.94, 1.52 | |
| No | 82.0% | 87.5% | 1.00 | Reference | |
|
Pre-pregnancy health conditions (hypertension or diabetes)c | |||||
| Yes | 9.3% | 1.9% | 4.7 6 | 3.13, 7.30 | |
| No | 90.7% | 98.2% | 1.00 | Reference | |
| Prenatal depressive symptomsc | |||||
| Yes | 24.1% | 16.8% | 1.23 | 0.98, 1.5\4 | |
| No | 75.9% | 83.2% | 1.00 | Reference | |
| Parity | |||||
| Primaparous (no prior births) | 37.5% | 37.9% | 0.9 6 | 0.77, 1.20 | |
| Multiparous (≥1 prior birth) | 62.5% | 62.1% | 1.00 | Reference | |
| Number of prior children under age 5 | 0.46 | 0.49 | 0.90 | 0.76, 1.06 | |
For univariate analysis,
p<0.05;
p<0.01;
p<0.001
Data are weighted to account for sampling design and survey non-respon se.
Note: The multivariate model included all variables listed in the table.
Table 4.
Characteristics of 2007 LAMB Study Respondents by Infant Gestational Age and Multinomial Logistic Regression Analysis of the Odds of Preterm Birth and Early-term Birth
| Preterm birth (vs. Late-term birth) |
Early-term birth (vs. Late-term birth) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Total | Preterm birth |
Early-term birth |
Late-term birth |
Model 1 | Model 2 | Model 1 | Model 2 | |
| Mean/% | Mean/% | Mean/% | AOR (95% CI) |
AOR (95% CI) |
AOR (95% CI) |
AOR (95% CI) |
||
| TOTAL: | ||||||||
| Weighted | 246,286 | 31,229 | 72,394 | 142,663 | ||||
| Weighted % | 100% | 12.7% | 29.4% | 57.9% | ||||
| TOTAL: | ||||||||
| Unweighted | 3,353 | 499 | 956 | 1,898 | ||||
| Unweighted % | 100% | 14.9% | 28.5% | 56.6% | ||||
|
Stress-to-Capital Ratio |
0.00c | −0.07 | −0.09 | 1.44 (1.07, 1.93) |
1.33 (0.98, 1.80) |
1.18 (0.94, 1.47) |
1.15 (0.92, 1.44) |
|
| Sociodemographic characteristics | ||||||||
| Age | 27.9 | 28.4b | 27.6 | 1.02 (1.00, 1.04) |
1.02 (1.00, 1.04) |
1.01 (1.00, 1.03) |
1.01 (1.00, 1.03) |
|
| Race/ethnicity | ||||||||
| Non-Hispanic White |
9.5% | 12.2% | 14.4% | 1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
|
| Non-Hispanic Black |
4.5% | 5.1% | 4.5% | 1.26 (0.72, 2.18) |
1.07 (0.61, 1.88) |
1.43 (0.96, 2.13) |
1.36 (0.91, 2.04) |
|
| Hispanic | 76.9%b | 72.1% | 70.7% | 1.41 (0.97, 2.03) |
1.35 (0.93, 1.95) |
1.23 (0.96, 1.58) |
1.22 (0.95, 1.56) |
|
| Asian/Pacific Islander |
8.1% | 10.0% | 9.7% | 1.19 (0.78, 1.81) |
1.20 (0.78, 1.83) |
1.18 (0.88, 1.58) |
1.17 (0.87, 1.58) |
|
| Native American | 1.0% | 0.6% | 0.7% | 1.44 (0.52, 3.94) |
1.48 (0.53, 4.15) |
1.17 (0.46, 2.97) |
1.18 (0.47, 2.97) |
|
| Annual household income | ||||||||
| <$20,000 | 45.3%a | 42.1% | 42.6% | 1.33 (0.89, 2.00) |
1.26 (0.83, 1.90) |
0.91 (0.67, 1.25) |
0.90 (0.66, 1.23) |
|
| $20,000-$39,000 | 26.0%b | 23.8% | 22.0% | 1.55 (1.05, 2.30) |
1.46 (0.97, 2.18) |
1.00 (0.74, 1.35) |
0.99 (0.73, 1.33) |
|
| $40,000-$59,000 | 8.3% | 9.1% | 9.7% | 1.16 (0.73, 1.84) |
1.06 (0.66, 1.70) |
0.88 (0.63, 1.24) |
0.87 (0.62, 1.22) |
|
| $60,000-$99,000 | 7.5% | 11.1% | 10.7% | 1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
|
| >$ 100,000 | 6.5% | 9.5% | 10.0% | 1.00 (0.63, 1.60) |
1.00 (0.63, 1.59) |
0.94 (0.69, 1.29) |
0.94 (0.69, 1.29) |
|
| Unknown | 6.4%a | 4.5% | 4.9% | 1.83 (1.01, 3.34) |
1.65 (0.89, 3.09) |
0.88 (0.53, 1.46) |
0.86 (0.52, 1.42) |
|
| Education | ||||||||
| ≤12 years (no HS diploma/GED) | 33.7% | 33.6% | 32.5% | 0.88 (0.66, 116) |
0.89 (0.67, 1.19) |
1.03 (0.82, 1.30) |
1.04 (0.83, 1.30) |
|
| ≥HS diploma/GED |
62.9% | 64.7% | 65.6% | 1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
|
| Unknown | 3.4% | 1.6% | 1.9% | 1.70 (0.82, 3.55) |
1.37 (0.65, 2.90) |
0.81 (0.39, 1.69) |
0.77 (0.37, 1.59) |
|
| Marital status | ||||||||
| Married | 49.1% | 56.0% | 55.0% (ref) |
1.00 | 1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
|
| Separated/ Divorced/ Widowed |
3.4% | 3.0% | 2.7% | 1.15 (0.59, 2.24) |
1.16 (0.58, 2.32) |
1.19 (0.68, 2.08) |
1.18 (0.68, 2.08) |
|
| Single/never Married |
12.6% | 9.7% | 11.7% | 1.04 (0.70, 1.55) |
1.04 (0.69, 1.56) |
0.85 (0.61, 1.18) |
0.84 (0.61, 1.18) |
|
| Cohabiting | 34.7%a | 29.8% | 30.1% | 1.18 (0.90, 1.56) |
1.22 (0.92, 1.61) |
1.02 (0.81, 1.27) |
1.02 (0.81, 1.28) |
|
| Unknown | 0.2% | 1.5%a | 0.6% | 0.37 (0.05, 2.82) |
0.40 (0.06, 2.95) |
2.62 (1.09, 6.31) |
2.67 (1.13, 6.29) |
|
| Service Planning Area (SPA) | ||||||||
| 1 (Antelope Valley) | 2.8% | 2.7% | 2.4% | 1.36 (0.62, 2.97) |
1.23 (0.55, 2.76) |
1.33 (0.75, 2.36) |
1.30 (0.73, 2.31) |
|
| 2 (San Fernando Valley) | 19.0% | 21.5% | 21.2% | 1.23 (0.67, 2.27) |
1.14 (0.61, 2.12) |
1.28 (0.84, 1.97) |
1.26 (0.82, 1.93) |
|
| 3 (San Gabriel Valley) | 17.6% | 20.7% | 18.1% | 1.31 (0.70, 2.43) |
1.26 (0.67, 2.38) |
1.43 (0.93, 2.21) |
1.42 (0.92, 2.20) |
|
| 4 (Metro Los Angeles) | 10.3% | 9.2% | 10.2% | 1.33 (0.68, 2.58) |
1.30 (0.66, 2.58) |
1.12 (0.70, 1.81) |
1.12 (0.69, 1.81) |
|
| 5 (West) | 1.8% | 2.1% | 2.8% | 1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
|
| 6 (South) | 15.7% | 14.7% | 15.0% | 1.25 (0.65, 2.41) |
1.22 (0.62, 2.39) |
1.15 (0.72, 1.85) |
1.15 (0.71, 1.85) |
|
| 7 (East) | 15.0% | 11.7% | 15.0% | 1.26 (0.67, 2.38) |
1.21 (0.64, 2.32) |
0.94 (0.59, 1.49) |
0.93 (0.59, 1.48) |
|
| 8 (South Bay) | 17.8% | 17.3% | 15.5% | 1.49 (0.81, 2.78) |
1.37 (0.73, 2.58) | 1.35 (0.87, 2.10) | 1.33 (0.86, 2.07) | |
| Other control variables | ||||||||
| Pre-pregnancy depression | ||||||||
| Yes | 18.3%a | 14.7% | 14.3% | 1.11 (0.80, 1.55) |
1.06 (0.75, 1.49) |
1.02 (0.78, 1.34) |
1.01 (0.77, 1.32) |
|
| No | 81.7% | 85.3% | 85.7% | 1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
|
|
Pre-pregnancy health conditions (hypertension or diabetes) | ||||||||
| Yes | 7.1%a | 5.4% | 4.6% | 1.35 (0.87, 2.11) |
0.93 (0.60, 1.44) |
1.13 (0.76, 1.67) |
1.00 (0.68, 1.49) |
|
| No | 92.9% | 94.6% | 95.4% | 1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
|
| Prenatal depressive symptoms | ||||||||
| Yes | 24.2%a | 20.1% | 19.1% | 1.02 (0.75, 1.40) |
0.95 (0.68, 1.33) |
0.98 (0.76, 1.26) |
0.96 (0.74, 1.24) |
|
| No | 75.8% | 79.9% | 80.9% | 1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
|
| Parity | ||||||||
| Primaparous (no prior births) | 34.3%b | 32.3%c | 41.2% | 0.87 (0.64, 1.19) |
0.87 (0.64, 1.19) |
0.71 (0.56, 0.90) |
0.71 (0.56, 0.90) |
|
| Multiparous (≥1 prior birth) | 65.7% | 67.7% | 58.8% | 1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
1.00 (ref) |
|
|
Number of prior children under age 5 |
0.52 | 0.50 | 0.46 | 1.08 (0.86, 1.35) |
1.12 (0.89, 1.40) |
0.95 (0.80, 1.13) |
0.96 (0.81, 1.15) |
|
| Obstetric outcomes | ||||||||
| Pregnancy complications | ||||||||
| Any | 70.4%c | 46.2%c | 37.7% | 3.77 (2.96, 4.80) |
1.40 (1.18, 1.67) |
|||
| None | 29.6% | 53.8% | 62.3% | 1.00 (ref) | 1.00 (ref) | |||
For univariate analysis,
p<0.05;
p<0.01;
p<0.001
Data are weighted to account for sampling design and survey non-re sponse.
Note: Model 1 included all variables listed in the table except pregnancy complications. Model 2 included all variables in the table.
Results
Descriptive Comparison of Maternal Characteristics by Stress-to-Capital Ratio (SCR) Scores
The majority of respondents were 19–34 years old, Hispanic, multiparous, or had incomes ≤$39,000 or ≥12 years of schooling (Table 1). Over half of the women were married or had no prior children ≤5 years old. Approximately 15% of women reported pre-pregnancy depression, 20% of women reported prenatal depressive symptoms, and 5% of women reported having a pre-pregnancy health condition. Additionally, 44%, 13%, 8%, and 11% of women experienced pregnancy complications, PTB, LBW, and SGA, respectively.
Overall, respondents who were ≤18 years old, non-White, unmarried, or low-income had, on average, higher SCR (i.e. greater stress relative to personal capital) scores (Table 1). Women who lived in SPA 1 had at least two prior children ≤5 years old, had lower education or had experienced pre-pregnancy health conditions or depression, prenatal depressive symptoms, pregnancy complications or PTB also had higher SCR scores.
Distribution of Stress, Personal Capital, and Stress-to-Capital Ratio (SCR) Scores
Overall, the composite stress and personal capital measures and the stressful life events measure had low reliability, whereas all of the personal capital components and the perceived stress measure had high reliability (Cronbach’s alphas ≥0.80) (Table 2). Respondents, on average, had relatively low weighted stress scores (mean=24) and high weighted personal capital scores (mean=72) (Table 2). The final SCR ranged from −2.1 to 1.6, with a mean of −0.09 (Figure 2, Table 2).
Table 2.
Distribution of Stress, Personal Capital, and the Stress-to-Capital Ratio (SCR) Scores, 2007 LAMB Study
| Weighted Score | Cronbach's alpha | ||||||
|---|---|---|---|---|---|---|---|
| Raw (Unweighted) Score | Standardized Score | ||||||
| Mean (SD) |
Range | Mean (SD) |
Range | Mean (SD) |
Range | ||
| Stress Score | 8.87 (5.29) |
0.0–31.0 | 23.91 (14.03) |
1.0–85.9 | 46.64 (11.81) |
9.8–78.8 | 0.523 |
| Perceived Stress | 8.33 (4.91) |
0.0–27.0 | 0.849 | ||||
| Severe Stressful Life Events | 0.54 (0.89) |
0.0–7.0 | 0.472 | ||||
| Personal Capital Score | 63.01 (14.46) |
19.0–98.0 | 71.85 (13.87) |
12.1–98.3 | 50.00 (10.00) |
14.3–81.6 | 0.477 |
| Internal Resources | 20.88 (4.67) |
0.0–28.0 | 0.795 | ||||
| Partner Support | 5.35 (1.35) |
0.0–6.0 | 0.831 | ||||
| Social Network Support | 18.35 (8.86) |
0.0–28.0 | 0.919 | ||||
| Neighborhood Support | 18.42 (6.82) |
0.0–40.0 | 0.813 | ||||
| Stress-to-Capital Ratio | Raw (Untransformed) | Log Transformed | |||||
| Absolute Difference | |||||||
|
Mean (SD) |
Range |
Mean (SD) |
Range |
Mean (SD) |
Range | ||
| 1.00 (0.43) |
0.1–4.9 | −0.09 (0.45) |
−2.1–1.6 | −3.36 (18.69) |
−71.8–56.1 | ||
Pregnancy Complications
Women who experienced at least one pregnancy complication had significantly higher mean SCR scores than women who did not experience any complications (Table 3). Black, single/never married women, as well as women with unknown educational attainment, prenatal depressive symptoms, or pre-pregnancy health conditions or depression were also significantly more likely to report at least one pregnancy complication (Table 3)
Multivariate analysis indicated that women with higher SCR’s were significantly more likely to experience at least one pregnancy complication (OR= 1.35; p=0.004) (Table 3). Additionally, a higher SCR was most significantly associated with hypertension (OR=1.54; p=0.03), diabetes (OR=1.45; p=0.02), and premature labor (OR=1.36; p=0.03) during pregnancy.
Preterm Birth and Gestational Age
Bivariate comparisons indicated that women who experienced PTB had significantly higher mean SCR scores than women who experienced a late-term birth (Table 4). Also, women who were Hispanic, multiparous, had low or unknown income, cohabited with their partners, or experienced prenatal depressive symptoms or pre-pregnancy health conditions or depression were more likely to experience PTB (Table 4). Notably, among women who experienced PTB, 70% of them also reported at least one pregnancy complication. Furthermore, women who were older, multiparous, or experienced at least one pregnancy complication were more likely to have an early-term birth, as opposed to a late-term birth (Table 4).
Further, the SCR was significantly associated with PTB (OR=1.36; p=0.03), but not early-term birth, in the multivariate analysis (Table 4 Model 1). Accounting for pregnancy complications completely mediated this association for PTB (Table 4 Model 2). Sobel test findings further confirmed that pregnancy complications mediated the association between the SCR and PTB (Z-value=−5.82, p<0.001). We then conducted supplementary logistic regression analyses to individually account for each pregnancy complication and found that premature labor appeared to be the largest contributor to the mediating effect of pregnancy complications on the risk of PTB (data not shown). Furthermore, using multivariable linear regression to examine the association between the SCR and gestational age, we found that a one unit increase in the SCR was associated with a decrease of 1.8 gestational days, even after accounting for pregnancy complications (Table 5 Model 2).
Table 5.
Multivariate Linear Regression Analysis of Infant Gestational Age among 2007 LAMB Study Respondents
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Coefficient | 95% CI | Coefficient | 95% CI | |
| Stress-to-Capital Ratio | –2.21b | −3.84, −0.59 | −1.78a | −3.37, −0.20 |
| Sociodemographic characteristics | ||||
| Age | −0.20c | −0.32, −0.08 | −0.19b | −0.31, −0.07 |
| Race/ethnicity | ||||
| Non-Hispanic White | 1.0 0 | Reference | 1.00 | Reference |
| NonHispanic Black | −0.37 | −3.36, 2.61 | 0.48 | −2.52, 3.47 |
| Hispanic | −1.48 | −3.25, 0.29 | −1.20 | −2.96, 0.57 |
| Asian/Pacific Islander | −0.52 | −2.51, 1.47 | −0.44 | −2.40, 1.51 |
| Native American | −2.22 | −7.42, 2.97 | −2.22 | −7.42, 2.99 |
| Annual household income | ||||
| <$20,000 | −1.34 | −3.26, 0.59 | −1.04 | −2.94, 0.86 |
| $20,000-$39,000 | −2.20a | −4.06, −0.35 | −1.85a | −3.67, −0.03 |
| $40,000-$59,000 | −0.37 | −2.34, 1.60 | −0.02 | −1.96, 1.93 |
| $60,000-$99,000 | 1.00 | Reference | 1.00 | Reference |
| >$ 100,000 | −0.23 | −2.11, 1.65 | −0.24 | −2.08, 1.59 |
| Unknown | −4.29a | −8.46, −0.11 | −3.75 | −7.90, 0.39 |
| Education | ||||
| ≤12 years (no HS diploma/GED) | 1.40 | −0.20, 3.00 | 1.30 | −0.30, 2.90 |
| ≥HS diploma/GED | 1.00 | Reference | 1.00 | Reference |
| Unknown | −1.14 | −4.86, 2.58 | −0.02 | −3.62, 3.59 |
| Marital status | ||||
| Married | 1.0 0 | Reference | 1.0 0 | Reference |
| Separated/ Divorced/Widowed |
−1.03 | −5.06, 2.99 | −0.91 | −4.93, 3.10 |
| Single/never married | −1.45 | −3.86, 0.96 | −1.36 | −3.74, 1.03 |
| Cohabiting | −1.39 | −2.95, 0.17 | −1.46 | −2.99, 0.08 |
| Unknown | 2.00 | −3.72, 7.71 | 1.59 | −3.56, 6.73 |
| Service Planning Area (SPA) | ||||
| 1 (Antelope Valley) | −0.51 | −4.56, 3.54 | −0.05 | −4.09, 3.99 |
| 2 (San Fernando Valley) | −0.99 | −3.63, 1.65 | −0.61 | −3.18, 1.96 |
| 3 (San Gabriel Valley) | −1.87 | −4.52, 0.79 | −1.72 | −4.32, 0.87 |
| 4 (Metro Los Angeles) | −1.13 | −4.15, 1.88 | −1.07 | −4.04, 1.90 |
| 5 (West) | 1.00 | Reference | 1.00 | Reference |
| 6 (South) | −1.21 | −4.26, 1.83 | −1.15 | −4.12, 1.81 |
| 7 (East) | −0.77 | −3.64, 2.10 | −0.64 | −3.45, 2.17 |
| 8 (South Bay) | −2.67 | −5.50, 0.16 | −2.28 | −5.03, 0.46 |
| Other control variables | ||||
| Pre-pregnancy depression | ||||
| −0.33 | −2.40, 1.75 | −0.07 | ||
| Yes | −2.12, 1.99 | |||
| No | 1.00 | Reference | 1.00 | Reference |
|
Pre-pregnancy health conditions (hypertension or diabetes) | ||||
| Yes | −2.62 | −5.45, 0.21 | −0.54 | −3.33, 2.25 |
| No | 1.00 | Reference | 1.00 | Reference |
| Prenatal depressive symptoms | ||||
| Yes | 0.22 | −1.74, 2.19 | 0.53 | −1.42, 2.48 |
| No | 1.00 | Reference | 1.00 | Reference |
| Parity | ||||
| Primaparous (no prior births) | 1.02 | −0.71, 2.76 | 0.97 | −0.74, 2.68 |
| Multiparous (≥1 prior birth) | 1.00 | Reference | 1.00 | Reference |
|
Number of prior children under age 5 |
−0.66 | −2.11, 0.79 | −0.82 | −2.26, 0.63 |
| Obstetric outcomes | ||||
| Pregnancy complications | ||||
| Any | −6.22c | −7.43, −5.01 | ||
| None | 1.0 0 | Reference | 1.00 | Reference |
p<0.05;
p<0.01;
p<0.001
Data are weighted to account for s ampling design and survey non-resp onse.
Note: Model 1 included all variables listed in the table except pregnancy complications . Model 2 included all variables listed in the table.
Infant Birthweight and Small for Gestational Age
Overall, the mean SCR scores did not significantly differ by LBW or SGA statuses (data available upon request). Further, there were no significant associations between the SCR and LBW, SGA, or continuous infant birthweight, even in the unadjusted models (data available upon request).
Supplementary Analyses of Relationships between the Individual Personal Capital and Stress Measures and Obstetric Outcomes
In order to compare the individual associations between the SCR, standardized personal capital and standardized stress measures with obstetric outcomes, multivariable logistic regression analyses were conducted. In the final models, none of the personal capital or stress components or composite scores were independently associated with adverse obstetric outcomes (data available upon request).
Discussion
Our study contributes to the literature in three important ways. First, our findings provide evidence that experiencing greater stress relative to personal capital during pregnancy is significantly associated with the risk of pregnancy complications, PTB, and lower gestational age; further, pregnancy complications completely mediate the relationship between the SCR and PTB. Second, most studies have explored individual dimensions of stress and personal capital, whereas we developed conceptually-based, multi-dimensional stress and personal capital measures. This contribution is particularly significant in terms of personal capital as it has been previously under-explored. Third, to our knowledge, our study is the first to examine the balance between stress and personal capital during pregnancy and its relationship with adverse outcomes, as previous work has only considered the independent effects of stress and individual components of personal capital. Expanding the theoretical approach to incorporate both risks and resources during pregnancy is imperative because these factors do not exist independently of one another; rather, they coexist to determine women’s resiliency (i.e., the ability to bounce back after facing adversity due to having adequate personal capital relative to stress) and ultimately impact their risk of adverse obstetric outcomes.
Our finding regarding the significant association between the SCR and pregnancy complications is important, as there is a dearth in the literature on the relationships between stress, personal capital, and pregnancy complications. A prospective study by Roy-Matton et al. (2011), which operationalized pregnancy complications similar to our study, revealed that women who had higher perceived stress at 10–20 weeks of pregnancy were more likely than their counterparts to experience subsequent pregnancy complications. Our findings expand on this research by supporting the theoretically justified link between higher stress and lower personal capital taxing the female body to the extent that pregnancy complications may result. Although we cannot definitively establish that the pregnancy complications occurred after experiencing a high SCR, the proposed mechanism is biologically plausible. As this association has important implications for reducing the risk of pregnancy complications, future prospective work should focus on this pathway.
We also found that experiencing pregnancy complications, especially premature labor, mediated the risk of PTB for women with higher SCR’s. This finding is unsurprising, as spontaneous premature labor is a primary symptom of PTB (Steer 2005). This finding is also important, as it indicates that targeting efforts to decrease women’s risk of pregnancy complications, especially premature labor, may help prevent PTB. Additionally, our finding regarding the significant negative linear relationship between the SCR and gestational age, even after accounting for pregnancy complications, underscores the critical role that the SCR plays in determining infant gestational age, which may not be best captured by the use of cut-points (i.e., PTB vs. not PTB). Each day in the womb has critical long-term medical and social implications for child health (Moster et al 2008), and if higher stress relative to personal capital can decrease gestation by several days, then reducing women’s stress and increasing their resources will play an important role in improving birth outcomes and subsequent child health.
Furthermore, we found that the SCR was not significantly associated with LBW, continuous birthweight, or SGA in our study. Theory and empirical evidence suggest that the biological pathways to LBW and SGA can differ from the pathways to PTB (Coussons-Read et al. 2005, 2007; Dunkel-Schetter 2011; Gennaro & Hennessy 2003; Steer 2005; Wadhwa et al. 1998, 2001, 2004). The mechanisms contributing to LBW and/or SGA may involve more prolonged exposures or exposures that occur further upstream, such as the preconception period (Precht et al. 2007); therefore, future research should investigate the SCR both during and before pregnancy in relation to infant growth and birthweight.
Our findings have important implications for clinical and public health interventions to reduce women’s risk for experiencing adverse obstetric outcomes. In clinical settings, routinely assessing the life stressors, psychological stress, and available internal and social resources among women who are pregnant or planning pregnancy would enable healthcare providers to offer the most appropriate support (e.g. referrals to community resources) to women with high levels of stress or low personal capital. Moreover, though life stressors may be unavoidable, there are multiple public health opportunities at the individual, interpersonal, and community levels to increase personal capital and potentially counteract perceived stress for pregnant and preconception women. We posit that programs that offer comprehensive resources (e.g. individual, group, and couples counseling, individual and group prenatal care) would be more likely to increase personal capital relative to stress, and subsequently, resiliency, among pregnant women.
Several potential limitations should be considered when interpreting the findings of this study. First, as the survey was administered postpartum, and many of the variables in this study were self-reported, responses may be vulnerable to bias. Second, women with missing data for the stress, personal capital, and prenatal depressive symptoms variables were removed from the analyses; nonetheless, as these women were likely to have the lowest personal capital and highest stress, our findings were likely conservative estimates of the examined associations. Third, the weighting schemes for the stress and personal capital measures, though conceptually based, may not have accurately captured the relative importance of the individual components and may not be applicable to all populations. However, our sensitivity analysis found very similar associations among the different SCRs and obstetric outcomes. Fourth, the measurement of stress and personal capital was limited to the available variables in the LAMB survey; therefore, we were unable to incorporate pregnancy-specific measures of stress or other potential components of personal capital (e.g. spirituality).
The LAMB study had some potential limitations as well. Its cross-sectional nature precluded the assumption of causality between predictors and outcomes. Also, it had a relatively low response rate, though we argue that non-respondents were at higher risk for having low personal capital and greater stress and that our findings were thus conservative estimates of the associations examined. Finally, though the study sample was diverse and representative of the LA population, the findings may not be generalizable to other populations.
Based on the findings and potential limitations, this study highlights the need for further areas of research. First, future studies need to assess the reliability and validity of the SCR in relation to obstetric outcomes to test the generalizability of our measure and our findings in other populations. Second, in order to inform effective clinical and public health interventions, further longitudinal research is warranted to examine the potential causal mechanisms in which the SCR may be associated with pregnancy complications. Third, we recommend that longitudinal studies incorporate life-course measures of stress (e.g. early childhood trauma, pregnancy-specific stress) and personal capital (e.g. childhood family stability) in order to identify effective points of intervention throughout the life-course and ultimately improve maternal and child health outcomes.
Conclusion
Our study examined the relationship between the balance of personal capital and stress during pregnancy, operationalized as the SCR, and adverse obstetric outcomes, including pregnancy complications, PTB, LBW, and SGA. Our findings indicate that women’s relative level of personal capital and stress during pregnancy is significantly associated with the risk of experiencing at least one pregnancy complication, PTB, and lower gestational age; further, pregnancy complications mediated the associated between the SCR and PTB, thereby suggesting that pregnancy complications may be a mechanism linking the SCR to adverse obstetric outcomes. Most importantly, our work underscores the importance of recognizing that risks and resources coexist in women’s lives and likely impact each other; therefore, we need to address both women’s stress and personal capital during pregnancy in order to improve obstetric outcomes and long-term maternal and child health outcomes.
Acknowledgements
This project was made possible by the Health Resources and Services Administration (HRSA) grant # R40MC06635, the Los Angeles County Productivity and Investment fund, and the Los Angeles County Department of Maternal, Child and Adolescent Health (MCAH) Programs general grants and was completed in collaboration with 2007 LAMB Principal Investigator M.C. Lu. FW was supported by a grant from the Health Disparities Research Training Program (T32 HD049302; Principal Investigator G. Sarto). LW was supported by a grant from the Agency for Healthcare Research and Quality (AHRQ) (T32 HS000083; Principal Investigator M. Smith). We would like to thank the Los Angeles Mommy and Baby (LAMB) study team (Chandra Higgins, Diana Liu, Marian Eldahaby, Carmen Gutierrez, Yvornia Horton, and Martha Martinez) for their dedicated work in the design and implementation of the 2007 LAMB project. We would also like to thank the Lifecourse Epidemiology and Family Health (LEAF) team for their incredible support with the editing of the manuscript.
References
- Adams MM, Shulman HB, Bruce C, Hogue C, Brogan D. The Pregnancy Risk Assessment Monitoring System: design, questionnaire, data collection and response rates. PRAMS Working Group. Paediatr Perinat Epidemiol. 1991;5:333–346. doi: 10.1111/j.1365-3016.1991.tb00718.x. 1991. [DOI] [PubMed] [Google Scholar]
- Ayers S. Assessing stress and coping in pregnancy and postpartum. J Psychosom Obstet Gynaecol. 2001;22:13–27. doi: 10.3109/01674820109049947. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bell JF, Zimmerman FJ, Almgren GR, Mayer JD, Huebner CE. Birth outcomes among urban African-American women: a multilevel analysis of the role of racial residential segregation. Soc Sci Med. 2006;63:3030–3045. doi: 10.1016/j.socscimed.2006.08.011. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. Toward an experimental ecology of human development. American Psychologist. 1977;32:513–531. [Google Scholar]
- Bronfenbrenner U. The ecology of human development Cambridge. MA: Harvard University Press; 1979. [Google Scholar]
- Buka SL, Brennan RT, Rich-Edwards JW, Raudenbush SW, Earls F. Neighborhood support and the birth weight of urban infants. Am J Epidemiol. 2003;157:1–8. doi: 10.1093/aje/kwf170. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310–357. [PubMed] [Google Scholar]
- Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacaman S, Oskamp S, editors. The social psychology of health. Newbury Park, CA: Sage Publications; 1987. pp. 31–49. [Google Scholar]
- Collin NL, Dunkel-Schetter C, Lobel M, Scrimshaw SC. Social support in pregnancy: psychosocial correlates of birth outcomes and postpartum depression. J Pers Soc Psychol. 1993;65:1243–1258. doi: 10.1037//0022-3514.65.6.1243. [DOI] [PubMed] [Google Scholar]
- Coussons-Read ME, Okun ML, Schmitt MP, Giese S. Prenatal stress alters cytokine levels in a manner that may endanger human pregnancy. Psychosom Med. 2005;67:625–631. doi: 10.1097/01.psy.0000170331.74960.ad. [DOI] [PubMed] [Google Scholar]
- Coussons-Read ME, Okun ML, Nettles CD. Psychosocial stress increases inflammatory markers and alters cytokine production across pregnancy. Brain Behav Immun. 2007;21:343–350. doi: 10.1016/j.bbi.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz A, McMahon MJ, Buekens P. Maternal stress and preterm birth. Am J Epidemiol. 2003;151:14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- Evans RG, Stoddart GL. Consuming research, producing policy? Am J Public Health. 2003;93:371–379. doi: 10.2105/ajph.93.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman PJ, Dunkel-Schetter C, Sandman CA, Wadhwa PD. Maternal social support predicts birth weight and fetal growth in human pregnancy. Psychosom Med. 2000;62:715–725. doi: 10.1097/00006842-200009000-00016. [DOI] [PubMed] [Google Scholar]
- Fragile Families and Child Wellbeing Study. “Mother’s baseline questionnaire.”. 2003 http://www.fragilefamilies.princeton.edu/documentation.asp.
- Gennaro S, Hennessy MD. Psychological and physiological stress: impact on preterm birth. J Obstet Gynecol Neonatal Nurs. 2003;32:668–675. doi: 10.1177/0884217503257484. [DOI] [PubMed] [Google Scholar]
- Goldenberg RL, Cliver SP, Cutter GR, Hoffman HJ, Copper RR, Gotlieb S, Davis RO. Maternal psychological characteristics and intrauterine growth retardation; Journal of Prenatal & Perinatal Psychology &. Health. 1991;6:129–134. [Google Scholar]
- Hack M, Klein NK, Taylor GH. Long-term developmental outcomes of low birthweight infants. Future Child. 1995;5:176–196. [PubMed] [Google Scholar]
- Halfon N, Hochstein M. Life course health development: an integrated framework for developing health, policy, and research. Milbank Q. 2002;80:433–479. doi: 10.1111/1468-0009.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard M, Henriksen TB, Secher NJ, Hatch MC, Sabroe S. Do stressful life events affect duration of gestation and risk of preterm delivery? Epidemiology. 1996;7:339–345. doi: 10.1097/00001648-199607000-00001. [DOI] [PubMed] [Google Scholar]
- Heron M. Deaths: leading causes for 2008. Natl Vital Stat Rep. 2012;60:1–94. [PubMed] [Google Scholar]
- Hobfoll SE, Leiberman JR. Personality and social resources in immediate and continued stress resistance among women. J Pers Soc Psychol. 1987;52:18–26. doi: 10.1037//0022-3514.52.1.18. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE. Social and Psychological Resources and Adaptation. Review of General Psychology. 2002;6:307–324. [Google Scholar]
- House JS. Occupational stress and coronary heart disease: A review and theoretical integration. J Health Soc Behav. 1974;15:12–27. [PubMed] [Google Scholar]
- Jesse DE, Graham M. Swanson Mel Psychosocial and spiritual factors associated with smoking and substance use during pregnancy in African American and White low-income women. J Obstet Gynecol Neonatal Nurs. 2006;35:68–77. doi: 10.1111/j.1552-6909.2006.00010.x. [DOI] [PubMed] [Google Scholar]
- Kramer MS. The epidemiology of adverse pregnancy outcomes: an overview. J Nutr. 2003;133:1592S–1596S. doi: 10.1093/jn/133.5.1592S. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, Appraisal and Coping. New York: Springer; 1984. [Google Scholar]
- Lobel M, Dunkel-Schetter C. Conceptualizing stress to study effects on health: Environmental, perceptual and emotional components. Anxiety Research. 1990;3:213–230. [Google Scholar]
- Lobel M, Dunkel-Schetter C, Scrimshaw SC. Prenatal maternal stress and prematurity: a prospective study of socioeconomically disadvantaged women. Health Psychol. 1992;11:32–40. doi: 10.1037//0278-6133.11.1.32. [DOI] [PubMed] [Google Scholar]
- Marks NF, Lambert JD. Transition to caregiving, gender, and psychological well-being: prospective evidence from the National Survey of Family and Households. Working paper for NSFH. 1999 [Google Scholar]
- McCormick MC. The contribution of low birth weight to infant mortality and childhood morbidity. N Engl J Med. 1985;312:82–90. doi: 10.1056/NEJM198501103120204. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci. 198;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- Misra DP, Guyer B, Allston A. Integrated perinatal health framework. A multiple determinants model with a life span approach. Am J Prev Med. 2003;25:65–75. doi: 10.1016/s0749-3797(03)00090-4. [DOI] [PubMed] [Google Scholar]
- Moster D, Lie RT, Markestad T. Long-term medical and social consequences of preterm birth. N Engl J Med. 2008;359:62–273. doi: 10.1056/NEJMoa0706475. [DOI] [PubMed] [Google Scholar]
- Newton RW, Hunt LP. Psychosocial stress in pregnancy and its relation to low birth weight. Br Med J (Clin Res Ed) 1984;288:1191–1194. doi: 10.1136/bmj.288.6425.1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS. New intrauterine growth curves based on United States data. Pediatrics. 2010;125:e214–e224. doi: 10.1542/peds.2009-0913. [DOI] [PubMed] [Google Scholar]
- Precht DH, Anderson PK, Olsen J. Severe life events and impaired fetal growth: a nation-wide study with complete follow-up. Acta Obstetricia Et Gynecologica Scandinavica. 2007;86:266–275. doi: 10.1080/00016340601088406. [DOI] [PubMed] [Google Scholar]
- Rini CK, Dunkel-Schetter C, Wadhwa PD, Sandman CA. Psychological adaptation and birth outcomes: the role of personal resources, stress, and sociocultural context in pregnancy. Health Psychol. 1999;18:333–345. doi: 10.1037//0278-6133.18.4.333. [DOI] [PubMed] [Google Scholar]
- Rondo PHC, Ferreira RF, Nogueira FC, Ribeiro MC, Lobert H, Artes R. Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardation. Eur J Clin Nutr. 2003;57:266–272. doi: 10.1038/sj.ejcn.1601526. [DOI] [PubMed] [Google Scholar]
- Roy-Matton N, Moutquin J, Brown C, Carrier N, Bell L. The impact of perceived maternal stress and other psychosocial risk factors on pregnancy complications. J Obstet Gynaecol Can. 2011;33:344–352. doi: 10.1016/s1701-2163(16)34852-6. [DOI] [PubMed] [Google Scholar]
- Sable MR, Wilkinson DS. Impact of perceived stress, major life events and pregnancy attitudes on low birth weight. Fam Plann Perspect. 2000;32:288–294. [PubMed] [Google Scholar]
- Steer P. The epidemiology of preterm labour. Bjog. 2005;112(Suppl 1):1–3. doi: 10.1111/j.1471-0528.2005.00575.x. [DOI] [PubMed] [Google Scholar]
- Wadhwa PD, Porto M, Garite T, Chicz-DeM AI, Sandman CA, et al. Maternal corticotropin-releasing hormone levels in the early third trimester predict length of gestation in human pregnancy. Am J Obstet Gynecol. 1998;179:1079–1085. doi: 10.1016/s0002-9378(98)70219-4. [DOI] [PubMed] [Google Scholar]
- Wadhwa PD, Culhane JF, Rauh V, Barve SS, Hogan V, Sandman CA, Hobel CJ, Chicz-DeMet A, Dunkel-Schetter C, Garite TJ, Glynn L. Stress, infection and preterm birth: a biobehavioural perspective. Paediatr Perinat Epidemiol. 2001;15(Suppl 2):17–29. doi: 10.1046/j.1365-3016.2001.00005.x. [DOI] [PubMed] [Google Scholar]
- Wadhwa PD, Garite TJ, Porto M, Glynn L, Chicz-DeMet A, Dunkel-Schetter C, Sandman CA. Placental corticotropin-releasing hormone (CRH), spontaneous preterm birth, and fetal growth restriction: a prospective investigation. Am J Obstet Gynecol. 2004;191:1063–1069. doi: 10.1016/j.ajog.2004.06.070. [DOI] [PubMed] [Google Scholar]
- Wakeel F, Witt WP, Wisk LE, Lu MC, Chao SM. Racial and Ethnic Disparities in Personal Capital During Pregnancy: Findings from the 2007 Los Angeles Mommy and Baby (LAMB) Study. Accepted for publication at Maternal and Child Health Journal. 2013 doi: 10.1007/s10995-013-1256-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu P, Tao F, Hao J, Sun Y, Jiang X. Prenatal life events stress: implications for preterm birth and infant birthweight. Am J Obstet Gynecol. 2010;203:34e31–34e38. doi: 10.1016/j.ajog.2010.02.023. [DOI] [PubMed] [Google Scholar]