Abstract
Aims
We examined two questions about the relationship between conduct disorder (CD), depression, and anxiety symptoms and substance use onset: (1) what is the relative influence of recent and more chronic psychiatric symptoms on alcohol and marijuana use initiation and (2) are there sensitive developmental periods when psychiatric symptoms have a stronger influence on substance use initiation?
Design
Secondary analysis of longitudinal data from the Pittsburgh Youth Study, a cohort study of boys followed annually from 7–19 years of age.
Setting
Recruitment occurred in public schools in Pittsburgh, Pennsylvania, USA.
Participants
Five hundred and three boys.
Measurements
The primary outcomes were age of alcohol and marijuana use onset. Discrete-time hazard models were used to determine whether (a) recent (prior year); and (b) cumulative (from age 7 until 2 years prior to substance use onset) psychiatric symptoms were associated with substance use onset.
Findings
Recent anxiety symptoms (HR= 1.10, 95% CI=1.03–1.17), recent (HR=1.59, 95% CI=1.35–1.87), cumulative (HR=1.45, 95% CI=1.03–2.03) CD symptoms, and cumulative depression symptoms (HR= 1.04, 95% CI=1.01–1.08) were associated with earlier alcohol use onset. Recent (HR=1.39, 95% CI=1.22–1.58) and cumulative CD symptoms (HR=1.38, 95% CI=1.02–1.85) were associated with marijuana use onset. Recent anxiety symptoms were only associated with alcohol use onset among black participants.
Conclusions
Timing matters in the relationship between psychiatric symptoms and substance use onset in childhood and adolescence, and the psychiatric predictors of onset are substance-specific. There is no single sensitive developmental period for the influence of psychiatric symptoms on alcohol and marijuana use initiation.
Keywords: comorbidity, substance use onset, depression, anxiety, conduct disorder
Introduction
The patterns of alcohol and drug use that emerge during childhood and adolescence are increasingly recognized as important predictors of pathological substance use behaviors and associated disorders in adulthood.1–6 Given that substance use becomes increasingly common during adolescence, the identification of factors associated with the onset of substance use needs to begin in childhood.
Psychiatric symptoms may offer important targets for early intervention designed to prevent the development of substance use problems. Common psychiatric symptom domains, including conduct disorder (CD), depression and anxiety, often start earlier than substance use and have been repeatedly correlated with substance use across development7–14. However, critical questions about the timing of the relationship between psychiatric symptoms and substance use initiation in childhood and adolescence remain. For example, we do not know whether the risk of child and adolescent substance use initiation is best predicted by recent psychiatric symptoms or by a history of cumulative psychiatric symptoms. The former may suggest that substance use onset can occur as a short-term response to a transient set of psychiatric symptoms, while the latter might reflect that early substance use onset is concentrated among individuals with a longer, potentially more severe, history of psychiatric symptoms. Recent versus cumulative effects also suggest different avenues for intervention. If substance use initiation is facilitated primarily by recent psychiatric symptoms, then substance use prevention programs should target all children who are exhibiting psychiatric symptoms. In contrast, if a cumulative history of mental health problems represents the primary risk factor for substance use initiation, prevention efforts should focus on youth with a prolonged history of psychiatric symptoms, even if they do not exhibit current psychiatric symptoms.
We also do not know whether there are sensitive developmental periods when psychiatric symptoms have a particularly strong influence on substance use initiation. By identifying the etiologic period of influence, we can gain insight into the developmentally-specific mechanisms through which psychiatric symptoms may lead to substance use initiation. For example, we can determine whether symptoms of CD, characterized by serious violations of rules and social norms, influence initiation at a different developmental stage than symptoms of depression and anxiety, which are characterized by negative emotionality. Given that early onset of substance use is a robust predictor of future substance use disorders,1 it is especially important to understand which psychiatric symptom domains are most robustly associated with substance use onset prior to adolescence. If certain domains of psychiatric symptoms are stronger predictors of risk for early rather than late substance use onset, preventing onset and reducing duration of such symptoms may also reduce risk of early onset substance use and the associated adverse long-term consequences.
While prior studies have documented an association between psychiatric symptoms and substance use initiation, most have examined the psychiatric symptoms at a single point in time8,12,15–21. This assumes a constant effect of psychiatric symptoms on onset across developmental stages. To address this limitation, the current study examined the timing of the association between symptoms of CD, depression and anxiety, and alcohol and marijuana use onset from childhood through late adolescence in a longitudinal sample of boys. In particular, this investigation examined whether a long-term accumulation of psychiatric symptoms and/or short-term fluctuations in psychiatric symptoms predicted subsequent alcohol or marijuana use initiation, and whether these associations varied by age of substance use onset. Since there are robust race/ethnic differences in substance use initiation, we also stratified by race/ethnicity.
METHOD
Study sample
We used data from the youngest cohort of the Pittsburgh Youth Study (PYS)22,23,24,25 Participants were originally selected from boys enrolled in 1st grade at 31 public schools in Pittsburgh (PA) in 1987–1988. A random sample of boys was invited for an initial screening of antisocial behavior (e.g., fighting, stealing, defiant) based on parent, teacher and youth report measures, with 85% of the families contacted agreeing to participate in the screening24. Boys ranking in the top 30% of antisocial behavior, together with an approximately equal number of participants randomly chosen from the remaining 70% of the distribution were included in the study (total N=503). Boys selected for follow-up were not different from the screening sample in terms of race, reading achievement, or parental education.25 More than half of the sample was Black (56%), the remainder was White (41%), or Asian, Mexican and Mixed-race (3%). Additional information on sampling is available elsewhere24,25.
The participants, mean age 6.7 years at baseline, were assessed annually or semi-annually, depending on the measure, for thirteen years. The analysis included all boys who had not initiated alcohol or marijuana use by age 9 and were followed until age 19 (n=470 for alcohol use and 499 for marijuana use initiation). We excluded boys who onset earlier than age 9 because data on the psychiatric predictors at age 6 was incomplete and data was not available for earlier ages. Caretakers provided informed consent and children provided assent until age 17 and consent thereafter. Study procedures were approved by the Institutional Review Boards of the University of Pittsburgh School of Medicine and the Columbia University Mailman School of Public Health.
Measures
Outcome: Drug use onset
Alcohol and marijuana use were assessed semi-annually by the Self-Reported Antisocial Behavior scale (SRA)25,26 until age 10 and by a 16-item Substance Use Scale,26,27 based on the National Youth Survey at age 10 and thereafter. The 30-item SRA scale includes many behaviors from the Self-Reported Delinquency (SRD) scale that have been modified to be more age-appropriate and understandable to young children.26 Children were queried about timing, quantity, and frequency of alcohol (beer, wine, and liquor) and marijuana use. We defined age at onset of alcohol use as the age when consumption of at least a half a drink was first reported. Age at onset of marijuana was defined as the age when any use of marijuana was first reported.
Exposure: Psychiatric disorder symptom domains
Depression symptoms were measured using the 13-item Recent Mood and Feelings Questionnaire (RMFQ) that was administered to boys annually28. RMFQ has previously demonstrated adequate reliability (alpha coefficient= 0.87)29 and a strong association with a diagnosis of depression.30
Anxiety was measured at each assessment wave using multiple informants. Items from the Achenbach scales that were rated as consistent with anxiety disorders by a group of mental health professionals were administered to caregivers (Child Behavior Checklist -CBCL) and teachers (Teacher report form -TRF) from age 7 to 16, and the youth from age 10 to 19 (Youth Self Report -YSR - until age 17, and the Young Adult Self-report -YASR - thereafter).31–33 The highest rating across the three informants was selected for each item and the items were summed to form a total anxiety score. Internal consistency coefficients of the three informant-specific anxiety scales varied from 0.67–0.73. The scale has been shown to discriminate between clinic-referred children with anxiety disorders and non-referred children34,35.
A count of CD symptoms were measured semi-annually through self-report using items from the SRA26,27 until age 9.5, items from the SRD27 from age 10 onwards, and items from the Child report of the Achenbach scales (i.e. YSR and YASR)31–33 from age 10.5 onwards. All the scales used have previously shown acceptable concurrent and predictive validity in ROC analyses comparing the scales with official records of offense and delinquency or by assessing discrimination between children referred to psychiatric clinics and non-referred children.34,36 Internal consistency was high (Cronbach’s alpha coefficients were 0.92, and 0.83 for the SRD37 and YSR34 respectively). The items included in the depression, anxiety and CD measures are listed in Tables S1–S3, available online.
Age-specific variables were created for alcohol and marijuana use and the psychiatric symptoms domain variables by combining semi-annual assessments when appropriate. For the semi-annual assessments, substance use onset was considered present if the child reported use at either assessment at a given age. The mean of the two semi-annual anxiety and CD scores were used. Because depression was measured annually across the entire duration of the study, it was not necessary to combine semi-annual assessments for this scale.
We created recent and cumulative measures for each of the three psychiatric disorder symptom domains. Recent measures reflected the level (score) of the psychiatric domains the year prior to the measurement of substance use. The cumulative measures indicated the mean level of the psychiatric domain symptoms from age 7 to two years prior to the measurement of substance use. Recent and cumulative measures of the each domain were temporally separated to enable us to examine the independent contribution that each made to alcohol and marijuana use initiation. Recent and cumulative measures of the three domains were moderately correlated at each age (Table S4, available online).
Covariates
Race/ethnicity of the child was reported by the parent at the initial screening assessment. The variable race/ethnicity was dichotomized as Black or Other. Family socioeconomic status (SES) was assessed at baseline by applying the Hollingshead Index of Social Status to data provided by the primary caretaker38. Lifetime parental history of problems with alcohol and drugs was assessed at baseline for each biological parent using the Family Substance Use Questionnaire.24,24,25. Lifetime parental history of internalizing and antisocial problems was also assessed at baseline for each biological parent with the Georgia Child Center questionnaire.
Data Analysis
Analyses were conducted is SAS 9.2.39 Missing data was treated using the listwise approach (see Table 1 for information on the amount of missing data in baseline covariates and see Tables S5–6 for the same information for each psychiatric symptom domain at each age). To examine the role of each psychiatric domain symptom on age at initiation of use of alcohol or marijuana we conducted discrete-time survival analysis (DTSA) using age-specific measures of substance use and the psychiatric symptoms. DTSA estimated the hazard of initiation of substance use at a particular age (given that initiation had not previously occurred), as a function of prior, time-varying levels of depression, anxiety and CD.40 Psychiatric symptoms that occurred following onset were not used to predict hazard of initiation. To allow for variation in the level of the psychiatric symptoms over time, we arranged the data for DTSA using the counting-process format whereby multiple records are generated per subject, each to reflect a single 1-year measurement interval over which covariates are invariant. Robust sandwich estimators were used for statistical inference, to account for clustering of responses within subjects and within schools from which respondents were recruited.41
TABLE 1.
Baseline characteristics of the participants in the samples for follow-up of alcohol and marijuana use initiation
|
|
||
|---|---|---|
| Alcohol follow-up sample N= 460 | Marijuana follow-up sample N= 488 | |
|
| ||
| Variables | N (%) or Mean (SD) | N (%) or Mean (SD) |
| Participants who initiated use during follow up | 382(83 %) | 303 (62 %) |
| Race/ethnicity | ||
| Black | 260 (55 %) | 276 (55 %) |
| Other | 210 (45 %) | 223 (45 %) |
| Missing | 0 | 0 |
| SES (Hollingshead scale score) | ||
| High (49.5–66) | 39 (8.3) | 41 (8.2) |
| Mid (33–49.5) | 165 (35) | 175 (35) |
| Low (16.5–33) | 212 (45) | 228 (46) |
| Very low (<16.5) | 54 (12) | 55 (11) |
| Missing | 0 | 0 |
| Biological parents’ problems with alcohol, score | 1.34 (2.0) | 1.35 (2.0) |
| Missing | 30 (6.6) | 31 (6.4) |
| Biological parents’ problems with drugs | ||
| 0 parent | 333 (71 %) | 414 (7.2 %) |
| 1 parent | 40 (8.5 %) | 42 (8.4 %) |
| 2 parents | 7 (1.5 %) | 7 (1.4 %) |
| Missing | 90 (19 %) | 35 (7.2 %) |
| Biological parents’ internalizing disorders, score | 0.38 (0.63) | 0.37 (0.62) |
| Missing | 64 (14) | 68 (14) |
| Biological parents’ antisocial problems, score | 0.69 (1.08) | 0.69 (1.09) |
| Missing | 60 (13) | 63 (13) |
We tested two types of models: (1) models including both recent and cumulative measures of the same psychiatric domain; and (2) models including all measures of the three psychiatric domains. All models were initially adjusted for demographic variables (race, family SES) and family history of problem substance use, internalizing, and antisocial problems. In subsequent models, we only retained covariates that were significantly associated with the outcome. We next tested whether the relationship between each of the psychiatric predictors and alcohol and marijuana use onset varied by age and race/ethnicity. Moderation by age of substance use onset was tested by including an interaction term between the psychiatric predictors and the age at which substance use onset was measured. Interactions by race/ethnicity were tested similarly.
RESULTS
The analytic sample included 460 respondents to examine alcohol use onset and 488 respondents to examine marijuana use onset. Exclusion criteria for the alcohol analysis included alcohol use prior to age 9 (n=33) and missing response to the questions on alcohol use on all measurement occasions (n=10). For the marijuana analysis, four children were excluded because of marijuana initiation before age 9 and 11 children were excluded because of missing responses to questions on marijuana use across all measurements occasions. As our final models retained only race/ethnicity and SES, which were complete for the entire sample, no respondents were excluded due to missing baseline covariates.
Table 1 shows characteristics of participants included in the current study, separately for analyses involving alcohol and marijuana use initiation. 83% of the boys initiated alcohol and 62% initiated marijuana use by the last assessment: 25% initiated alcohol only, 2.2% initiated marijuana only, and 59.5% initiated use of both substances.
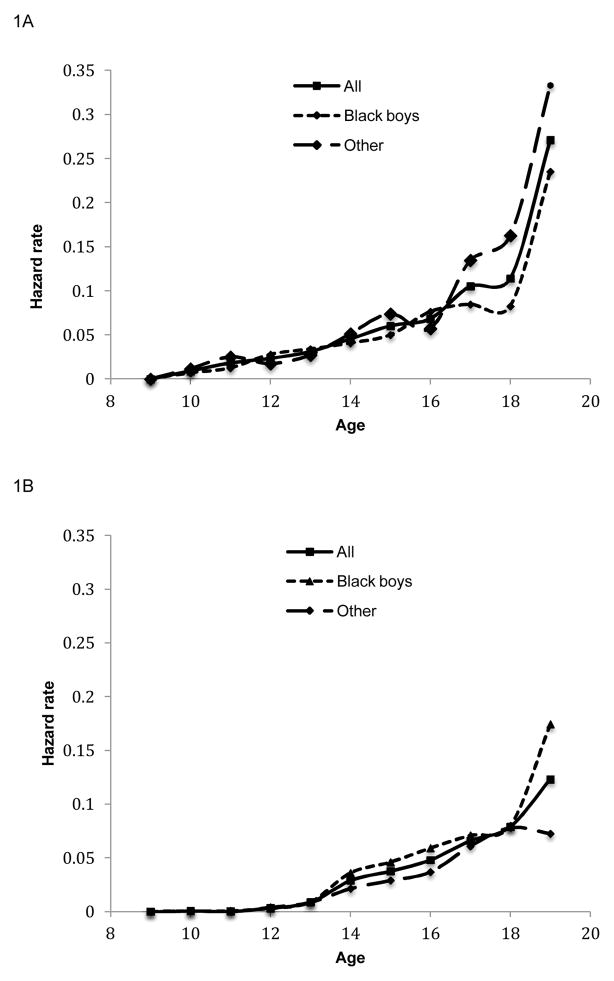
Figure 1 shows the age-specific hazard rates of alcohol and marijuana use onset for the overall sample and by race/ethnicity. While age-specific hazard rates increased between ages 9 –19 for both alcohol and marijuana, the hazard of initiating alcohol was over twice as large as the hazard of initiating marijuana, regardless of race/ethnicity. The figure suggests differences between the racial/ethnic groups in the specific hazard rates: at age 17 and after, the hazard rates for alcohol initiation were consistently higher for Other adolescents, and at age 14 and after, the hazard rates of marijuana initiation were higher in Black adolescents. The median age at alcohol initiation was 14 for Black and Other adolescents, and the median age at marijuana initiation was 16 and 17 for Black and Other adolescents respectively.
FIGURE 1.
Hazard rates of substance use initiation by age, and by race/ethnicity. Note: Fig 1A represents hazard rates of alcohol initiation, Fig 1B represents hazard rates of marijuana initiation
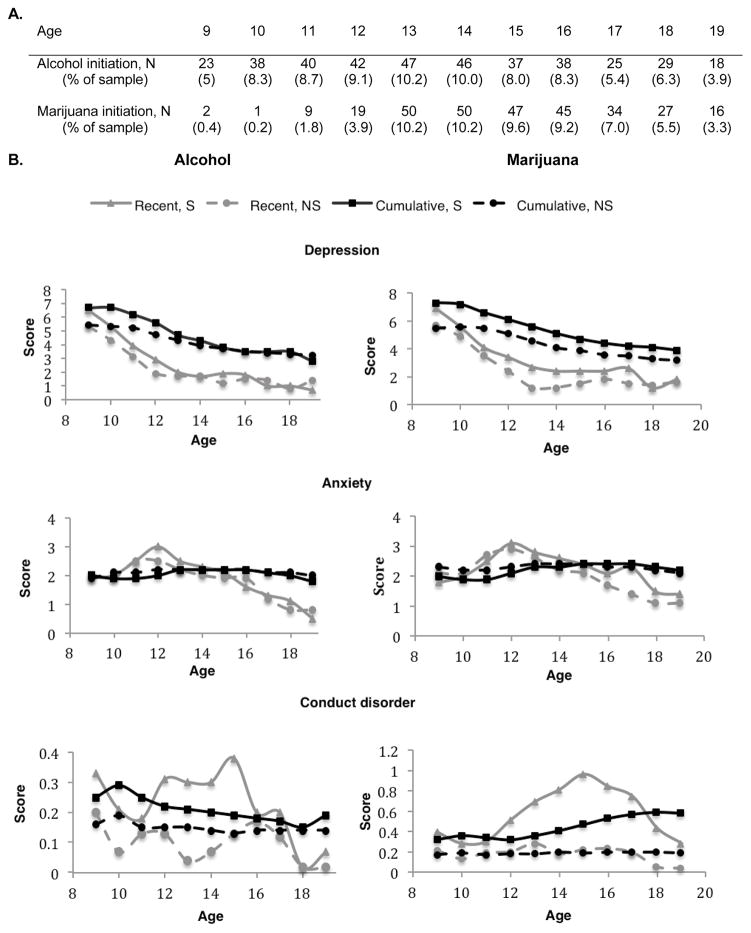
Figure 2 shows psychiatric symptom levels of participants who were at risk of initiating alcohol or marijuana use, separating those who ever initiated use from those who did not. Recent and cumulative psychiatric domain symptoms were higher in participants who eventually initiated use than in participants who never initiated use. This difference in the levels of psychiatric domain symptoms between ever and never starters was most dramatic for CD symptoms.
FIGURE 2.
A. Number of participants (and sample proportion) initiating use of alcohol and marijuana by age; B. The levels of recent and cumulative psychiatric symptoms are shown by age for participants at risk of alcohol or marijuana initiation. Starters (S) –participants who eventually started using the substance- and Never-starters (NS)–participants who never initiated use- are shown separately.
The influence of depression, anxiety, and CD on initiation of alcohol or marijuana use is depicted in Table 2. In single-domain analyses (models 1–3), cumulative depression, recent anxiety, and recent and cumulative CD symptoms were associated with earlier onset of alcohol use. In a full model (model 4) that included all three psychiatric domain symptoms, cumulative depression, recent anxiety, and recent and cumulative CD remained independently predictive of earlier alcohol initiation (Table 2). Cumulative anxiety was marginally related to alcohol use onset, with higher levels of cumulative anxiety associated with a reduced likelihood of initiating alcohol use.
TABLE 2.
| a. Alcohol use initiation | b. Marijuana use initiation | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Models | Psychiatric symptoms | HR | 95% CI | Models | Psychiatric symptoms | HR | 95% CI | ||
|
| |||||||||
| Single psychiatric domain symptoms models | Single psychiatric domain symptoms models | ||||||||
| 1 | Depression | Recent | 1.02 | 0.99–1.05 | 1 | Depression | Recent | 1.00 | 0.97–1.04 |
| Cumulative | 1.06 | 1.03–1.09 | Cumulative | 1.06 | 1.02–1.10 | ||||
| 2 | Anxiety | Recent | 1.14 | 1.07–1.21 | 2 | Anxiety | Recent | 1.05 | 0.99–1.12 |
| Cumulative | 0.93 | 0.84–1.04 | Cumulative | 0.97 | 0.88–1.07 | ||||
| 3 | Conduct disorder | Recent | 1.61 | 1.37–2.90 | 3 | Conduct disorder | Recent | 1.37 | 1.22–1.54 |
| Cumulative | 1.65 | 1.23–2.20 | Cumulative | 1.33 | 1.02–1.74 | ||||
|
| |||||||||
| All three psychiatric domain symptoms model | All three psychiatric domain symptoms model | ||||||||
|
| |||||||||
| 4 | Depression | Recent | 1.00 | 0.97–1.03 | 4 | Depression | Recent | 0.99 | 0.95–1.03 |
| Cumulative | 1.04 | 1.01–1.08 | Cumulative | 1.00 | 0.95–1.05 | ||||
| Anxiety | Recent | 1.10 | 1.03–1.17 | Anxiety | Recent | 1.02 | 0.95–1.09 | ||
| Cumulative | 0.89 | 0.80–1.00 | Cumulative | 0.91 | 0.81–1.02 | ||||
| Conduct disorder | Recent | 1.59 | 1.35–1.87 | Conduct disorder | Recent | 1.39 | 1.22–1.58 | ||
| Cumulative | 1.45 | 1.03–2.03 | Cumulative | 1.38 | 1.02–1.85 | ||||
All models are adjusted for race/ethnicity and socioeconomic status. Model 2 is also adjusted for parental history of drug problems.
Recent measures are the participant’s scores in the assessment of depression, anxiety, and conduct disorder on the year prior to the assessment of alcohol or marijuana use.
Cumulative measures represent the participant’s mean score over the period beginning at age 7 to the second year prior to the assessment of alcohol or marijuana use.
All models are adjusted for clustering of responses within subjects and within schools from which subjects were recruited
For models predicting marijuana use onset, initial single-domain analyses (models 1–3) indicated that cumulative depression and recent and cumulative CD predicted earlier initiation of marijuana. The full model containing measures for all three psychiatric symptom domains showed that only recent and cumulative CD were associated with marijuana use initiation (Table 2).
The associations of all psychiatric domains with alcohol or marijuana use initiation were constant across age: estimating interactions between each psychiatric domains and age did not improve model fit. The association of recent anxiety symptoms with alcohol use initiation differed by race/ethnicity (X2 for likelihood ratio test comparing models with and without interaction term = 7.2; p<0.01). Recent anxiety symptoms predicted initiation of alcohol use only among Black participants (HR = 1.19; 95% CI = 1.10–1.29).
DISCUSSION
Our study shows that timing matters in the relationship between psychiatric symptoms and substance use onset in childhood and adolescence, and that the psychiatric predictors of onset are substance-specific. We found, first, that cumulative depressive symptoms were more important for predicting risk for earlier alcohol use onset than recent symptoms, with the latter providing no incremental predictive utility. In contrast, recent, rather than cumulative, anxiety symptoms posed a risk for earlier alcohol use onset among Black respondents. Both recent and cumulative CD symptoms made independent contributions to the risk of alcohol and marijuana use onset. Further, there was no single sensitive developmental period for the influence of psychiatric symptoms on alcohol and marijuana use initiation.
Initiation of alcohol use arises after a cumulative, rather than recent, experience of depressive symptoms. From an etiologic perspective, this finding suggests a more nuanced perspective on the self-medication hypothesis.42 Initiation of alcohol use may not be a short-term strategy to manage current symptoms of depression associated with daily stressful life events. Instead, it points to a potential threshold effect, whereby depression symptoms needs to accumulate to a “tipping point” over time before they may lead youth to decide to experiment with alcohol to relieve symptoms of distress. Such cumulative depression may reflect distress associated with the occurrence of major traumatic events, rather than daily life events.43 Individuals with cumulative depression may also have limited capacity for self-regulation of negative affect, and may be unable to react in a constructive manner to external sources of stress.44 Alcohol use may then emerge as a maladaptive means of alleviating these persistent feelings of sadness. Overall, these findings indicate that initiatives oriented towards the prevention of alcohol use in childhood and adolescence should focus on identifying and preventing cases with a cumulative history of depression, regardless of their current status.
Recent forms of anxiety were associated with a higher risk of alcohol use initiation, while cumulative forms of anxiety were marginally associated with a lower risk of alcohol use onset across childhood and adolescence. Earlier studies in this cohort found a positive association between recent anxiety symptoms and alcohol use onset;45 we extend this work by finding that recent and cumulative forms of anxiety may actually have opposite effects on alcohol use onset. The positive relationship between recent anxiety and alcohol use initiation is consistent with laboratory studies that found stress-response dampening effects associated with acute alcohol intoxication, as well as prior prospective studies of adolescents that found a positive association between past 12-month anxiety symptoms and alcohol use problems.46 The marginally negative association between cumulative anxiety and alcohol use onset, in contrast, may reflect certain types of stable anxiety problems such as social phobia and separation anxiety or a fearful temperament. These types of problems may inhibit children and adolescents from detaching from their caregiver and establishing relationships with deviant peers, thus reducing the opportunities to access and experiment with alcohol earlier in life18,47,48. High temperamental fear in children is associated with a reduced likelihood of alcohol use onset, and adolescents who exhibit shy/withdrawn behaviors are less likely to develop alcohol dependence in adulthood.49,50
The association of recent anxiety symptoms with alcohol use onset was specific to Black respondents, suggesting that the social context around which psychiatric symptoms emerge is an important modifier of the relation between these symptoms and alcohol use onset. Black respondents face greater adversity than their peers in a number of domains, including on average lower socio-economic status, experiences of discrimination and social adversity, and higher likelihood of exposure to violence and other stressful experiences.51,52 All of these experiences may engender greater levels of anxiety and stress, which may be mitigated by engagement with substance use at an early age. Black adolescents and adults who report higher levels of discrimination due to race/ethnicity are more likely to engage in problematic drinking patterns.53,54 The present study is the first, to our knowledge, that reports on a differential pattern of the association between recent anxiety symptoms and alcohol use onset, and suggests that the social context may be a critical part of assessing psychiatric symptoms and substance use in childhood and adolescence.
The impact of depression and anxiety on substance use onset were specific to alcohol, not marijuana.8,13 This is consistent with prior studies that examined either alcohol or marijuana use, and found a robust relationship between symptoms of affective disorders and alcohol use,46,55 but conflicting findings on the relationship between symptoms of affective disorders and marijuana use.19,45,56–58 By separately examining the relationship among depression and anxiety and alcohol and marijuana in the same population, we were able to differentiate the particular impact that depression and anxiety had on the two types of substances.
There was consistent evidence across substances that both cumulative and recent CD symptoms increase the risk for early initiation of substance use.7,9,10,16,59 A life-course pattern of persistent antisocial problems, associated with a series of long-term risk behaviors, increases risk for alcohol and marijuana use initiation, even among individuals who do not exhibit any current symptoms of CD.60–62 In addition, temporally-proximate elevations in CD, which may reflect more prevalent antisocial problems in adolescence, also predict risk for alcohol and marijuana use initiation, regardless of any prior history of CD.63,64 Such findings are consistent with developmental theories of antisocial behavior, that propose that both childhood and adolescent-onset forms of antisocial behavior are linked to problematic substance use.60–62
This study was subject to several limitations. First, we did not attempt to disentangle the factors that explain the association of depression, anxiety and CD with substance use initiation. The observed links could be due to common genetic and social factors that lead to the onset of both psychiatric symptoms and substance use, or they could be causally connected through social and behavioral pathways. Second, because all participants in the Pittsburgh Youth Study are male, it was not possible to examine the relationship between psychopathology and substance use onset among girls. Third, all participants were selected from Pittsburgh public schools, which limits our ability to generalize findings beyond this area. Fourth, half of the sample consisted of high-risk boys, limiting our ability to infer to the general population, but also providing us with greater power to detect an association between psychiatric symptoms and substance use. Fifth, while we examined measures of psychiatric symptoms that are generally consistent with DSM diagnoses, these measures did not explicitly measure diagnostic criteria for DSM disorders. However, it is increasingly recognized that psychiatric symptoms are best conceptualized as falling on a continuum of severity rather than representing a discrete taxon. Sixth, a low base rate prevented us from examining the predictors of initiation of other illicit drugs. Finally, informants on anxiety varied across time: while teachers and parents reported in childhood, boys themselves reported in late childhood through adolescence. However, a sensitivity analysis found that the type of informant had no effect on the relationship between anxiety and substance use onset.
Our findings suggest that substance use prevention efforts should target youth based on the type and chronicity of their psychiatric symptoms. While youth with a cumulative history of depressive symptoms appear at increased risk for alcohol use initiation, recent and cumulative experience of CD symptoms across childhood and adolescence produce a generalized vulnerability to alcohol and marijuana use. Recent anxiety symptoms pose an increased risk for alcohol use initiation among Black boys. The impact of psychiatric symptoms on substance use initiation is constant from childhood to late adolescence: no sensitive period of influence was identified.
Supplementary Material
Acknowledgments
We would like to thank Ms. Rebecca Stallings for her assistance with the data. This study was supported by National Institutes of Health Grants DA030449 (to M.C.), MH 082729 (to S.G), MH093612 (to K.K.); and MH078039 (to D.P.). Data collection for the Pittsburgh Youth Study was supported by grants awarded to Dr. Rolf Loeber from the National Institutes of Health (DA411018, MH 48890, MH 50778) and the Office of Juvenile Justice and Delinquency Prevention (96-MU-FX-0012).
Contributor Information
Dr. Magdalena Cerdá, Department of Epidemiology, Mailman School of Public Health, Columbia University.
Ms. Paula M. Bordelois, Department of Epidemiology, Mailman School of Public Health, Columbia University.
Dr. Katherine M. Keyes, Department of Epidemiology, Mailman School of Public Health, Columbia University.
Dr. Sandro Galea, Department of Epidemiology, Mailman School of Public Health, Columbia University.
Dr. Karestan C. Koenen, Department of Epidemiology, Mailman School of Public Health, Columbia University.
Dr. Dustin Pardini, University of Pittsburgh School of Medicine and Western Psychiatric Institute.
References
- 1.Grant BF, Dawson DA. Age of onset of drug use and its association with DSM-IV drug abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. J Subst Abuse. 1998;10(2):163–173. doi: 10.1016/s0899-3289(99)80131-x. [DOI] [PubMed] [Google Scholar]
- 2.Grant BF, Stinson FS, Harford TC. Age at onset of alcohol use and DSM-IV alcohol abuse and dependence: A 12-year follow-up. J Subst Abuse. 2001;13(4):493–504. doi: 10.1016/s0899-3289(01)00096-7. [DOI] [PubMed] [Google Scholar]
- 3.Gruber E, DiClemente RJ, Anderson MM, Lodico M. Early drinking onset and its association with alcohol use and problem behavior in late adolescence. Prev Med. 1996 May-Jun;25(3):293–300. doi: 10.1006/pmed.1996.0059. [DOI] [PubMed] [Google Scholar]
- 4.Guttmannova K, Bailey JA, Hill KG, et al. Sensitive Periods for Adolescent Alcohol Use Initiation: Predicting the Lifetime Occurrence and Chronicity of Alcohol Problems in Adulthood. J Stud Alcohol Drugs. 2011 Mar;72(2):221–231. doi: 10.15288/jsad.2011.72.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hawkins JD, Catalano RF, Kosterman R, Abbott R, Hill KG. Preventing adolescent health-risk behaviors by strengthening protection during childhood. Arch Pediatr Adolesc Med. 1999 Mar;153(3):226–234. doi: 10.1001/archpedi.153.3.226. [DOI] [PubMed] [Google Scholar]
- 6.Lynskey MT, Heath AC, Bucholz KK, et al. Escalation of drug use in early-onset cannabis users vs co-twin controls. Jama-J Am Med Assoc. 2003 Jan 22;289(4):427–433. doi: 10.1001/jama.289.4.427. [DOI] [PubMed] [Google Scholar]
- 7.Galéra C, Bouvard M-P, Melchior M, et al. Disruptive symptoms in childhood and adolescence and early initiation of tobacco and cannabis use: The Gazel Youth Study. European Psychiatry. 2010;25:402–408. doi: 10.1016/j.eurpsy.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 8.King S, Iacono W, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99(1):1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- 9.Jester J, Nigg J, Buu A, et al. Trajectories of Childhood Aggression and Inattention/Hyperactivity: Differential Effects on Substance Abuse in Adolescence. J Am Acad Child Adolesc Psychiatry. 2008;47(10):1158–1165. doi: 10.1097/CHI.0b013e3181825a4e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brook JS, Whiteman M, Finch S, Cohen P. Young adult drug use and delinquency: childhood antecedents and adolescent mediators. J Am Acad Child Adolesc Psychiatry. 1996;35:1584–1592. doi: 10.1097/00004583-199612000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Lynskey MT, Fergusson DM. Childhood conduct problems, attention deficit behaviors, and adolescent alcohol, tobacco, and illicit drug use. J Abnorm Child Psychol. 1995 Jun;23(3):281–302. doi: 10.1007/BF01447558. [DOI] [PubMed] [Google Scholar]
- 12.Sartor CE, Lynskey MT, Heath AC, Jacob T, True W. The role of childhood risk factors in initiation of alcohol use and progression to alcohol dependence. Addiction. 2007 Feb;102(2):216–225. doi: 10.1111/j.1360-0443.2006.01661.x. [DOI] [PubMed] [Google Scholar]
- 13.Marmorstein N. Longitudinal associations between depressive symptoms and alcohol problems: The influence of comorbid delinquent behavior. Addict Behav. 2010;35(6):564–571. doi: 10.1016/j.addbeh.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zimmermann P, Wittchen HU, Hofler M, Pfister H, Kessler RC, Lieb R. Primary anxiety disorders and the development of subsequent alcohol use disorders: a 4-year community study of adolescents and young adults. Psychological Medicine. 2003 Oct;33(7):1211–1222. doi: 10.1017/s0033291703008158. [DOI] [PubMed] [Google Scholar]
- 15.Anderson KG, Tomlinson K, Robinson JM, Brown SA. Friends or foes: social anxiety, peer affiliation, and drinking in middle school. J Stud Alcohol Drugs. 2011 Jan;72(1):61–69. doi: 10.15288/jsad.2011.72.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flory K, Lynam D, Milich R, Leukefeld C, Clayton R. Early adolescent through young adult alcohol and marijuana use trajectories: early predictors, young adult outcomes, and predictive utility. Dev Psychopathol. 2004 Winter;16(1):193–213. doi: 10.1017/s0954579404044475. [DOI] [PubMed] [Google Scholar]
- 17.Kandel DB, Johnson JG, Bird HR, et al. Psychiatric disorders associated with substance use among children and adolescents: findings from the Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) Study. J Abnorm Child Psychol. 1997 Apr;25(2):121–132. doi: 10.1023/a:1025779412167. [DOI] [PubMed] [Google Scholar]
- 18.Kaplow JB, Curran PJ, Angold A, Costello EJ. The prospective relation between dimensions of anxiety and the initiation of adolescent alcohol use. Journal of Clinical Child Psychology. 2001 Sep;30(3):316–326. doi: 10.1207/S15374424JCCP3003_4. [DOI] [PubMed] [Google Scholar]
- 19.Ohannessian CM, Hesselbrock VM. A Finer Examination of the Role That Negative Affect Plays in the Relationship Between Paternal Alcoholism and the Onset of Alcohol and Marijuana Use. J Stud Alcohol Drugs. 2009 May;70(3):400–408. doi: 10.15288/jsad.2009.70.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tomlinson KL, Brown SA. Self-medication or social learning? A comparison of models to predict early adolescent drinking. Addict Behav. 2012 Feb;37(2):179–186. doi: 10.1016/j.addbeh.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 21.Wu P, Bird HR, Liu XH, et al. Childhood depressive symptoms and early onset of alcohol use. Pediatrics. 2006 Nov;118(5):1907–1915. doi: 10.1542/peds.2006-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pardini DA, Loeber R, Farrington DP, Stouthamer-Loeber M. Identifying direct protective factors for nonviolence. Am J Prev Med. 2012 Aug;43(2 Suppl 1):S28–40. doi: 10.1016/j.amepre.2012.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Loeber R, Menting B, Lynam DR, et al. Findings from the Pittsburgh Youth Study: cognitive impulsivity and intelligence as predictors of the age-crime curve. J Am Acad Child Adolesc Psychiatry. 2012 Nov;51(11):1136–1149. doi: 10.1016/j.jaac.2012.08.019. [DOI] [PubMed] [Google Scholar]
- 24.Loeber R, Farrington D, Stouthamer-Loeber M, Raskin White H, Wei E. Violence and Serious Theft: Development and Prediction from Childhood to Adulthood. New York, NY: Taylor & Francis Group, LLC; 2008. [Google Scholar]
- 25.Loeber R, Farrington DP, Stouthamer-Loeber M, Van Kammen WB. Antisocial behavior and mental health problems: Explanatory factors in childhood and adolescence. New York, NY: Routledge; 1998. [Google Scholar]
- 26.Elliott DS, Huizinga D, Ageton . Explaining delinquency and drug use. Beverly Hills, CA: Sage; 1985. [Google Scholar]
- 27.Loeber R, Stouthamer-Loeber M, White HR. Developmental aspects of delinquency and internalizing problems and their association with persistent juvenile substance use between ages 7 and 18. Journal of Clinical Child Psychology. 1999 Sep;28(3):322–332. doi: 10.1207/S15374424jccp280304. [DOI] [PubMed] [Google Scholar]
- 28.Costello AJ, Angold A. Scales to assess child and adolescent depression: checklists, screens, and nets. Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27:726–737. doi: 10.1097/00004583-198811000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Kuo ES, Stoep AV, Stewart DG. Using the short mood and feelings questionnaire to detect depression in detained adolescents. Assessment. 2005 Dec;12(4):374–383. doi: 10.1177/1073191105279984. [DOI] [PubMed] [Google Scholar]
- 30.Rhew IC, Simpson K, Tracy M, et al. Criterion validity of the Short Mood and Feelings Questionnaire and one- and two-item depression screens in young adolescents. Child Adolesc Psychiatry Ment Health. 2010;4(1):8. doi: 10.1186/1753-2000-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Achenbach T. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 32.Achenbach T. Manual for the Youth Self Report and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 33.Achenbach T. Young Adult Self Report. Burlington, VT: University of Vermont Department of Psychiatry; 1997. [Google Scholar]
- 34.Achenbach T. Integrative Guide to the 1991 CBCL/4–18, YSR, and TRF Profiles. Burlington, VT: University of Vermont; 1991. [Google Scholar]
- 35.Ferdinand RF. Validity of the CBCL/YSR DSM-IV scales Anxiety Problems and Affective Problems. J Anxiety Disord. 2008;22(1):126–134. doi: 10.1016/j.janxdis.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 36.Farrington DP. Explaining the link between problem drinking and delinquency. Addiction. 1996 Apr;91(4):498–500. doi: 10.1111/j.1360-0443.1996.tb02304.x. [DOI] [PubMed] [Google Scholar]
- 37.Allwood M, Bell D. A preliminary examination of emotional and cognitive mediators in the relationship between violence exposure and violent behaviors in youth. Journal of Community Psychology. 2008;36(8):989–1007. [Google Scholar]
- 38.Miller DS, Miller TQ. A test of socioeconomic status as a predictor of initial marijuana use. Addict Behav. 1997 Jul-Aug;22(4):479–489. doi: 10.1016/s0306-4603(96)00059-7. [DOI] [PubMed] [Google Scholar]
- 39.SAS 9.2 [computer program] 2002–2008. [Google Scholar]
- 40.Singer J, Willett J. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- 41.Wei L, Lin D, Weissfeld L. Regression analysis of multivariate incomplete failure time data by using the marginal distributions. Journal of American Statistical Association. 1989;84:1065–1073. [Google Scholar]
- 42.Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry. 1997 Jan-Feb;4(5):231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- 43.Turner R, Wheaton B, Lloyd D. The Epidemiology of Social Stress. American Sociological Review. 1995;60(1):104–125. [Google Scholar]
- 44.Shoal GD, Giancola PR. Cognition, negative affectivity and substance use in adolescent boys with and without a family history of a substance use disorder. J Stud Alcohol. 2001 Sep;62(5):675–686. doi: 10.15288/jsa.2001.62.675. [DOI] [PubMed] [Google Scholar]
- 45.Marmorstein NR, White HR, Loeber R, Stouthamer-Loeber M. Anxiety as a predictor of age at first use of substances and progression to substance use problems among boys. J Abnorm Child Psychol. 2010 Feb;38(2):211–224. doi: 10.1007/s10802-009-9360-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kushner MG, Abrams K, Borchardt C. The relationship between anxiety disorders and alcohol use disorders: A review of major perspectives and findings. Clinical Psychology Review. 2000 Mar;20(2):149–171. doi: 10.1016/s0272-7358(99)00027-6. [DOI] [PubMed] [Google Scholar]
- 47.Clark DB, Smith MG, Neighbors BD, Skerlec LM, Randall J. Anxiety Disorders in Adolescence - Characteristics, Prevalence and Comorbidities. Clin Psychol Rev. 1994;14(2):113–137. [Google Scholar]
- 48.Fergusson DM, Horwood LJ. Prospective childhood predictors of deviant peer affiliations in adolescence. J Child Psychol Psyc. 1999 May;40(4):581–592. [PubMed] [Google Scholar]
- 49.Pardini D, Lochman J, Wells K. Negative emotions and alcohol use initiation in high-risk boys: the moderating effect of good inhibitory control. Journal of abnormal child psychology. 2004 Oct;32(5):505–518. doi: 10.1023/b:jacp.0000037780.22849.23. [DOI] [PubMed] [Google Scholar]
- 50.Pardini D, White HR, Stouthamer-Loeber M. Early adolescent psychopathology as a predictor of alcohol use disorders by young adulthood. Drug and alcohol dependence. 2007 Apr;88:S38–S49. doi: 10.1016/j.drugalcdep.2006.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Williams DR, Jackson PB. Social sources of racial disparities in health - Policies in societal domains, far removed from traditional health policy, can have decisive consequences for health. Health Affairs. 2005 Mar-Apr;24(2):325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- 52.Williams DR, Williams-Morris R. Racism and mental health: the African American experience. Ethnicity & health. 2000 Aug-Nov;5(3–4):243–268. doi: 10.1080/713667453. [DOI] [PubMed] [Google Scholar]
- 53.Yen IH, Ragland DR, Greiner BA, Fisher JM. Racial discrimination and alcohol-related behavior in urban transit operators: findings from the San Francisco Muni Health and Safety Study. Public health reports. 1999 Sep-Oct;114(5):448–458. doi: 10.1093/phr/114.5.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Terrell F, Miller AR, Foster K, Watkins CE., Jr Racial discrimination-induced anger and alcohol use among black adolescents. Adolescence. 2006 Fall;41(163):485–492. [PubMed] [Google Scholar]
- 55.Conner KR, Pinquart M, Gamble SA. Meta-analysis of depression and substance use among individuals with alcohol use disorders. J Subst Abuse Treat. 2009 Sep;37(2):127–137. doi: 10.1016/j.jsat.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Degenhardt L, Hall W, Lynskey M. Exploring the association between cannabis use and depression. Addiction. 2003 Nov;98(11):1493–1504. doi: 10.1046/j.1360-0443.2003.00437.x. [DOI] [PubMed] [Google Scholar]
- 57.Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J Consult Clin Psych. 2002 Dec;70(6):1224–1239. doi: 10.1037//0022-006x.70.6.1224. [DOI] [PubMed] [Google Scholar]
- 58.Clark DB, Parker AM, Lynch KG. Psychopathology and substance-related problems during early adolescence: a survival analysis. J Clin Child Psychol. 1999 Sep;28(3):333–341. doi: 10.1207/S15374424jccp280305. [DOI] [PubMed] [Google Scholar]
- 59.Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. J Abnorm Psychol. 2002 Aug;111(3):411–424. [PubMed] [Google Scholar]
- 60.Moffitt TE, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: follow-up at age 26 years. Dev Psychopathol. 2002 Winter;14(1):179–207. doi: 10.1017/s0954579402001104. [DOI] [PubMed] [Google Scholar]
- 61.Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychol Rev. 1993 Oct;100(4):674–701. [PubMed] [Google Scholar]
- 62.Wiesner M, Kim HK, Capaldi DM. Developmental trajectories of offending: Validation and prediction to young adult alcohol use, drug use, and depressive symptoms. Development and Psychopathology. 2005;17:251–270. doi: 10.1017/s0954579405050133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fite PJ, Colder CR, Lochman JE, Wells KC. Pathways from proactive and reactive aggression to substance use. Psychol Addict Behav. 2007 Sep;21(3):355–364. doi: 10.1037/0893-164X.21.3.355. [DOI] [PubMed] [Google Scholar]
- 64.Dishion TJ, Tipsord JM. Peer contagion in child and adolescent social and emotional development. Annu Rev Psychol. 2011;62:189–214. doi: 10.1146/annurev.psych.093008.100412. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.