Abstract
Purpose
Non-Hispanic Blacks in the US have lower rates of major depression than non-Hispanic Whites, in national household samples. This has been termed a “paradox,” as Blacks suffer greater exposure to social stressors, a risk factor for depression. Subgroup analyses can inform hypotheses to explain this paradox. For example, it has been suggested that selection bias in household samples undercounts depression in Blacks; if selection is driving the paradox, Black–White differences should be most pronounced among young men with low education.
Methods
We examined Black–White differences in lifetime major depression in subgroups defined simultaneously by sex, age, and education using data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) and the Collaborative Psychiatric Epidemiology Surveys (CPES).
Results
In NESARC and CPES, Blacks had lower odds than Whites of lifetime major depression in 21 and 23 subgroups, respectively, of 24. All statistically significant differences were in subgroups favoring Blacks, and lower odds in Blacks were more pronounced among those with more education.
Conclusions
These results suggest that hypotheses to explain the paradox must posit global mechanisms that pertain to all subgroups defined by sex, age, and education. Results do not lend support for the selection bias hypothesis.
Keywords: Major depressive disorder, Blacks, Whites, Socioeconomic status, United States
Introduction
Studies using nationally representative samples of noninstitutionalized adults in the US have consistently reported a lower prevalence of major depressive disorder (MDD) in non-Hispanic Blacks compared with non-Hispanic Whites [1–4]. Unadjusted odds ratios for lifetime prevalence differences range from an estimated 0.53 [4] to 0.62 [1]. For more recent diagnostic time frames (i.e., past 12 months and past month), this pattern persists, but with attenuated effect sizes. Importantly, never in these studies do Blacks have a higher prevalence than Whites.
The persistently lower risk of depression in Blacks compared to Whites in the US poses a critical challenge to our understanding of the social determinants of health. MDD is among the psychiatric disorders thought to be particularly vulnerable to stressors [5–7], and empirical evidence demonstrates that Blacks in the US are exposed to more stressors, both acute and chronic, than Whites [8–13]. All else being equal, it stands to reason that Blacks would have a higher prevalence of MDD than Whites. The failure of epidemiologic data to support this expectation has been called counterintuitive and a paradox [14–17].
Although several methodological and substantive explanations have been discussed to interpret this paradox [15, 18–20], definitive evidence for any is lacking. Tests of existing hypotheses have yielded conflicting results [21–23] or have not been borne out [14]. Given these results, additional, novel hypotheses should be pursued.
A critical step in the process of testing and refining extant hypotheses as well as developing novel explanations is to establish the full extent of the paradoxical racial patterning across sociodemographic subgroups. Stratum-specific estimates that do not parallel those found in an overall estimate suggest needed refinement of global theories and sometimes point to developing entirely new theories. Conversely, stratum-specific estimates that do parallel those found in the overall estimate indicate that explanatory theories for the paradox would have to postulate mechanisms that operate equally across subgroups.
Analyses of ethnic subgroups defined by nativity status have shown that the influence of race or ethnicity on mental health outcomes is potentially contingent on the degree of socialization in the United States [24–27]. Subgroup comparisons can also be used to advantage when interpreting the Black–White depression paradox. For example, an artifactual explanation posits that rates of depression among Blacks are underestimated in major psychiatric epidemiologic studies due to selection bias [15, 28–30]. Estimates of MDD from household samples exclude institutionalized populations (e.g., the incarcerated, the homeless, and those living on military bases), which have higher rates of depression than household samples [31–36]. As Blacks in the US are more likely to be institutionalized than Whites [37–40], household samples may disproportionately underestimate depression among Blacks [15, 28–30]. Definitive tests of this hypothesis would require extensive data on Black–White differences in depression among institutionalized populations. However, if selection processes are an important driver of the overall paradox, the underestimate in depression should be especially pronounced among the subgroups most likely to be institutionalized. Thus, younger Black men with low socioeconomic status (SES) would be more impacted by under-counting than Black women and/or older Blacks and/or higher SES Blacks, given that young Black men are disproportionately likely, for example, to be incarcerated [38, 40].
To date, the few studies that have examined subgroup differences in MDD between non-Hispanic Blacks and Whites have not reported results from statistical tests of these differences [1, 4, 41]. Other studies have compared Black and White subgroups on either disorder classes (e.g., mood disorders) rather than specific disorders [2], or have used distress or symptomatology measures as outcomes, not psychiatric disorders [42]. A fairly consistent finding across studies using either major depression or mood disorders as the outcome is that in virtually all defined subgroups, Blacks had lower levels of disorder than Whites. For example, Blazer et al. [1] found a lower prevalence of lifetime major depression in Blacks compared with Whites in all subgroups defined simultaneously by age and gender. In bivariate subgroups characterized by a wide range of sociodemographic variables, Williams et al. [4] found that African-Americans consistently had a lower prevalence of lifetime major depression than Whites. Finally, Breslau et al. [2] found that Blacks’ lower prevalence of lifetime mood disorders, compared with Whites, persisted across age-of-onset, cohort, respondent education, and parent education categories, and across subgroups cross-tabulated by age-of-onset and cohort. These studies contribute to our understanding of the extent of racial differences in mental health outcomes, but they do not sufficiently address the question of interest to us here because they lack the power to produce robust estimates across granular subgroups or they do not focus specifically on MDD, the outcome where the “paradox” has been most pronounced.
Using data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), we use the largest nationally representative data source currently available to examine racial differences in major depression simultaneously stratified on three critical axes: sex, age, and education. This large sample size allows for sufficient power in these granular subgroups to obtain robust estimates. We replicate these analyses in two data sources from the second largest psychiatric epidemiology study conducted to date in the US, the Collaborative Psychiatric Epidemiology Surveys.
Materials and methods
Study population and data
Data for our primary analysis are from the 2001–2002 NESARC study, conducted by the National Institute on Alcohol Abuse and Alcoholism (Bethesda, MD, USA). The survey used a civilian, noninstitutionalized sample of adults 18 and older living in households and group quarters, including military off-base housing, boarding houses, rooming houses, non-transient hotels and motels, shelters, facilities for housing workers, college housing, and group homes in all 50 states. The sampling frame was based on households in the Census 2000–2001 Supplementary Survey and group quarters in the Census 2000 Group Quarters Inventory. Face-to-face interviews were conducted with 43,093 respondents with a survey response rate of 81 %. Blacks, Hispanics, and young adults (ages 18–24 years) were oversampled, and data were weighted to adjust for oversampling and household- and person-level nonresponse to represent the US population not living on military bases in the 2000 census in terms of region, age, sex, race, and ethnicity. Additional information on the study can be found elsewhere [3, 43–45].
The present sample includes individuals who self-identified as being born in the US, non-Hispanic ethnicity, and White (n = 23,162) or Black (n = 7,556) race. We excluded those born outside the US because the patterns of depression are different among foreign-born Blacks and Whites [25, 46] and, with foreign-born Blacks comprising 6 % of the US Black population [4], the paradox of interest has been documented using samples that are primarily US-born blacks or those identifying as African-Americans.
Data for our replication analysis are from the National Comorbidity Survey Replication (NCS-R, n = 9,282) and the National Survey of American Life (NSAL, n = 6,082), which are two of the three Collaborative Psychiatric Epidemiology Surveys studies conducted between 2001 and 2003. We excluded the third study because it excluded our study populations. Both the NCS-R and NSAL drew their samples from the noninstitutionalized US population, ages 18 and older, in the 48 contiguous states. The NCS-R sample was nationally representative and the response rate was 73 % [46]. The NSAL sample was nationally representative of those self-identifying as African-American and without ancestral ties to the Caribbean. A supplementary Afro-Caribbean sample of Blacks identifying a Caribbean ancestry was obtained from areas with higher Afro-Caribbean residential density. The overall response rate in the NSAL was 72 % [4]. The NCS-R and NSAL are described in greater detail elsewhere [47, 48]. Similar to our analyses of the NESARC sample, the included NCS-R and NSAL respondents were those who self-identified as US-born non-Hispanic Black (n = 4,717) and non-Hispanic White (n = 7,577).
Measures
Sex
The NESARC study included 17,671 women and 13,047 men. Sample sizes in NCS-R/NSAL were 7,147 and 5,147, respectively.
Age
We created four age groups based on self-reported age: 18–29 (NESARC n = 5,409; NCS-R/NSAL n = 2,572); 30–44 (NESARC n = 8,911; NCS-R/NSAL n = 3,924); 45–64 (NESARC n = 9,716; NCS-R/NSAL n = 3,809); >64 (NESARC n = 6,682; NCS-R/NSAL n = 1,989).
Education
In both datasets, we categorized education in the following tertiles based on self-reported highest education level achieved: less than a high school diploma (NESARC, n = 4,351; NCS-R/NSAL, n = 2,130), high school diploma (NESARC n = 9,374; NCS-R/NSAL n = 3,995), and education beyond a high school diploma (NESARC n = 16,993, NCS-R/NSAL n = 6,169).
Major depressive disorder
NESARC assessed MDD as defined by the Diagnostic and Statistical Manual IV (DSM-IV) using the Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV Version (AUDA-DIS-IV), a structured lay interview. Diagnoses were made in both lifetime and past-12 month time frames. As reported in greater detail elsewhere, test–retest reliability of the AUDADIS-IV for MDD in the NESARC sample was good (12-month MDD κ = 0.59; lifetime MDD κ = 0.65) [44] and clinical re-appraisals demonstrated fair agreement (κ = 0.64–0.68) [49] with psychiatrists’ diagnoses.
The NCS-R and NSAL assessed DSM-IV MDD using the World Mental Health Survey Initiative Version of the World Health Organization Composite Diagnostic Interview (WMH-CIDI). As with the AUDADIS-IV, the WMH-CIDI assesses MDD using trained lay interviewers conducting face-to-face structured diagnostic interviews. In the NCS-R, concordance between the WMH-CIDI and a follow-up clinician-administered Structured Clinical Interview for DSM-IV was considered good for lifetime diagnosis of Major Depressive Episode (κ = 0.59) and fair for 12-month MDE (κ = 0.40) [46]. In the NSAL, the concordance for 12-month MDE between these two diagnostic interviews was lower than in the NCS-R (κ = 0.34) [4].
Analytic strategy
In both samples, we estimated unadjusted odds ratios for the effect of race on MDD within 24 subgroups defined by sex, age, and education. In both datasets, the smallest subgroup was men aged 18–29 with less than a high school education (NESARC n = 297; NCS-R/NSAL n = 158) and the largest subgroup was women aged 30–44 with greater than a high school education (NESARC n = 3,326; NCS-R/NSAL n = 1,228). We then tested for multiplicative interactions between race and sex, age, and education in three separate models predicting lifetime MDD, adjusting for sex, age, and education in all models. Analyses were weighted to the 2000 census and we used SAS-callable SUDAAN to adjust standard errors for the complex sample design.
Results
Descriptive results of NESARC data
Blacks in the sample were on average younger, had fewer years of completed education, and the Black sample included a higher proportion of women (see Table 1). Not shown, US-born Blacks overall had lower odds of both lifetime and past-year MDD than Whites [Lifetime MDD odds ratio (OR) = 0.60, 95 % confidence interval (CI) 0.53, 0.67; past-year MDD OR = 0.82, 95 % CI 0.70, 0.97].
Table 1.
Socio-economic characteristics of US-born non-Hispanic White and non-Hispanic Black respondents of the National Epidemiologic Survey on Alcohol and Related Conditions (N = 30,718)
| n | US-born non-Hispanic White (n = 23,162) % (SE) | US-born non-Hispanic Black (n = 7,556) % (SE) | Chi-square, df, P value | |
|---|---|---|---|---|
| Age (years) | ||||
| 18–29 | 5,409 | 19.0 (0.4) | 25.6 (0.7) | 26.6, 3, P <0.001 |
| 30–44 | 8,911 | 29.1 (0.4) | 32.8 (0.7) | |
| 45–64 | 9,716 | 33.0 (0.4) | 29.1 (0.7) | |
| 65+ | 6,682 | 18.8 (0.3) | 12.5 (0.5) | |
| Education | ||||
| Less than high school | 4,351 | 11.2 (0.3) | 19.9 (0.7) | 36.5, 2, P <0.001 |
| High school | 9,374 | 30.4 (0.6) | 32.9 (1.0) | |
| More than high school | 16,993 | 58.4 (0.8) | 47.4 (1.1) | |
| Sex | ||||
| Men | 13,047 | 48.3 (0.4) | 43.6 (0.8) | 20.0, 1, P <0.001 |
| Women | 17,671 | 51.8 (0.4) | 56.5 (0.8) | |
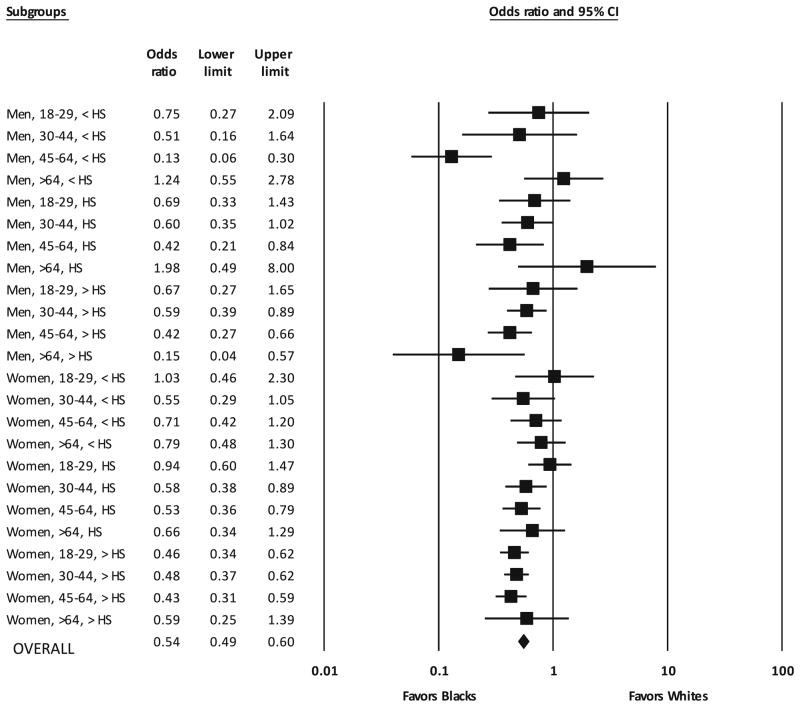
Is there subgroup variation in the Black–White odds ratios for lifetime MDD? Figure 1 shows the odds ratios for the race difference in lifetime MDD within each of the 24 strata. Blacks had lower odds compared to Whites in 21 of the 24 subgroup comparisons, ranging from 0.13 to 0.94 and 10 of these were statistically significant. None of the three comparisons in which Blacks had higher odds than Whites, which ranged from 1.03 to 1.98, was statistically significant.
Fig. 1.
Forest plot of Black–White subgroup odds ratios for lifetime major depressive disorder in National Epidemiologic Survey on Alcohol and Related Conditions data. Subgroups are defined by sex, age group, and education. HS high school
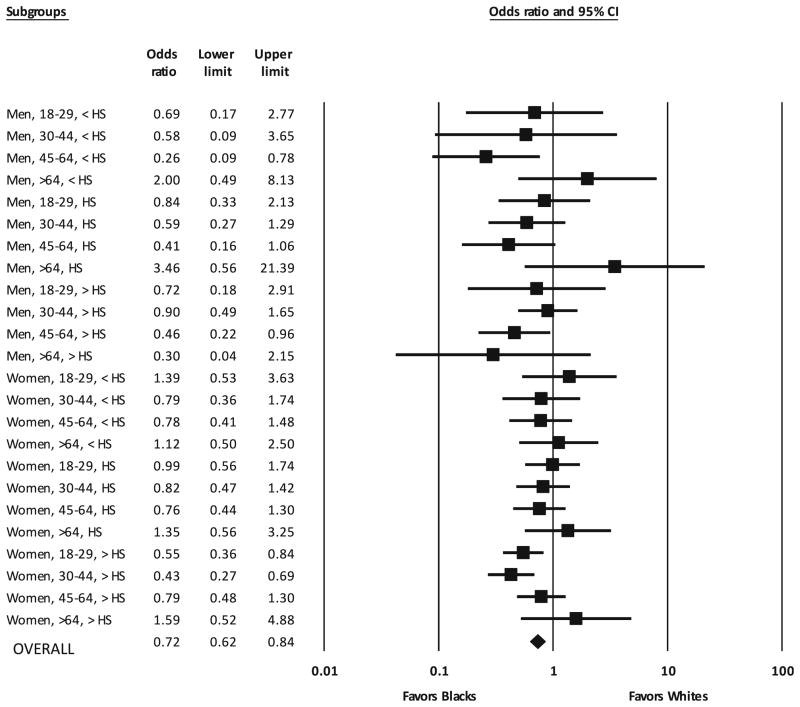
Is there subgroup variation in the Black–White odds ratios for past 12-month MDD? We conducted secondary analyses with past 12-month MDD as the outcome (Fig. 2). Blacks had lower odds than Whites in 18 of 24 subgroups, ranging from 0.26 to 0.99, and four of these were statistically significant. Of the six comparisons in which Blacks had higher odds than Whites, which ranged from 1.12 to 3.46, none was statistically significant.
Fig. 2.
Forest plot of Black–White subgroup odds ratios for 12-month major depressive disorder in the National Epidemiologic Survey on Alcohol and Related Conditions data. Subgroups are defined by sex, age group, and education. HS high school
Tests of interaction in NESARC data
Do age, education, or sex function differently between Blacks and Whites as predictors of MDD? Relationships between race and lifetime MDD varied across levels of both age and education in our data. Regarding the race and age interaction, Black–White odds ratios tended to follow a U-shaped pattern across age quartiles, with the greatest protective effects for Blacks in the two middle quartiles (ages 30–64) (Wald Fdf = 3 = 4.33, P = 0.01). With respect to race and education, Black men and women with beyond a high school diploma had statistically significantly lower odds than Whites of lifetime MDD in three of the four age groups. These robustly lower odds for Blacks were not seen in the two lower education tertiles, indicating that Blacks were most strongly protected against major depression at higher education levels (Wald Fdf=2 = 3.10, P = 0.05). The race × sex interaction term was non-significant (P = 0.89). We did not have sufficient power to test for interaction in models predicting 12-month MDD.
Descriptive results of replication analysis
We replicated theses analyses in the combined NCS-R/NSAL dataset. The relevant table and figure, which follow the same template as we use for the NESARC results reported here, can be found in the on-line version of this article (Online Table 1, Online Fig. 1). Blacks overall had lower odds of both lifetime and past-year MDD than Whites (Lifetime MDD OR = 0.55, 95 % CI 0.49, 0.62; past-year MDD OR = 0.80, 95 % CI 0.69, 0.93). For lifetime MDD, Blacks had lower odds than Whites in 23 of 24 subgroups, ranging from 0.06 to 0.91, and 11 of these comparisons were statistically significant. We had insufficient power to complete these same analyses using past 12-month MDD as the outcome.
Tests of interaction in replication analysis
As with the NESARC dataset, the relationship between race and lifetime MDD varied across age categories. However, unlike the U-shaped pattern seen in the NES-ARC data, in the replication dataset, the greatest protection for Blacks with respect to lifetime MDD appeared in the three older age groups (ages 30 and older). The test of multiplicative interaction was statistically significant (Wald Fdf=3 = 2.99, P = 0.03). No patterns in the replication results suggested interaction between race and education and race and sex, and our tests for multiplicative interaction bore this out (race × education: Wald Fdf=2 = 0.39, P = 0.68; race × sex: Wald Fdf=1 = 0.00, P = 0.99).
Discussion
We found little evidence for subgroup variation in the race difference in major depression across the critical axes of sex, age, and education. Of 24 subgroup comparisons for lifetime MDD outcomes, Blacks had lower odds than Whites in 21 and 10 of these differences were statistically significant. None of the three subgroup comparisons in which Blacks had higher odds of MDD than Whites was significant. Our 12-month MDD results were consistent with the lifetime MDD findings. The little evidence for subgroup variation that we did find indicated that Blacks’ lower odds of lifetime MDD were most pronounced in the middle two age quartiles and in the highest education tertile. Our findings for both lifetime and 12-month MDD did not change when we conducted these same analyses using risk differences and risk ratios as our measures of association (results not shown).
We replicated these analyses using pooled US-born Black and US-born White samples from the NCS-R and NSAL studies. Our replication results did not meaningfully differ; in all but one subgroup, Blacks had lower odds of MDD than Whites, and all statistically significant differences were in comparisons in which Blacks had lower odds than Whites of MDD. Thus, our combined results from the NESARC and NCS-R/NSAL studies are compelling evidence that the paradox of Blacks’ lower odds than Whites of lifetime and 30-day MDD occurs across subgroups defined by the key demographic axes of sex, age, and education.
To our knowledge, only two previous studies using national samples have examined MDD prevalence in Black–White subgroups. Blazer et al. [1] compared Blacks and Whites on lifetime and past 30-day MDD in subgroups created by cross-tabulating age and sex using data from the National Comorbidity Study. In the resulting 16 subgroup comparisons, Blacks had a lower prevalence of MDD in 14. The statistical significance of these differences was not reported. More recently, Williams et al. [4] reported lower lifetime unadjusted prevalence of MDD in African-Americans relative to Whites across a range of demographic characteristics in the NSAL. These strata were not cross-tabulated and the statistical significance of the prevalence differences was not reported. Thus, whether stratifying on one, two, or, as we have here, three key social axes, and doing so in different datasets, the lower odds of MDD in Blacks compared with Whites is remarkably stable.
These results have important implications for hypotheses to explain the Black–White depression paradox. Specifically, in light of the findings from our study, a plausible hypothesis must posit a mechanism that mitigates the effects of Blacks’ presumed greater stressor exposure for all subgroups defined by age, sex, and education. To date, a range of methodological and substantive hypotheses has been proposed to account for the Black–White depression paradox [15, 18–20]. We discuss a sample of the more prominent hypotheses.
The selection bias hypothesis posits [15, 28–30] that the noninstitutionalized household samples on which the large psychiatric epidemiology studies are based exclude segments of the population in which Blacks are overrepresented and in which psychiatric morbidity, including depression, is more prevalent. Household noninstitutionalized sampling by definition excludes the incarcerated, those living on military bases, and the homeless. On the whole, young Black men are more likely than Black women or elderly Blacks to be in these excluded groups [28, 30]. If the selection bias is operative, we should see the strongest inverse relation between race and depression comparing young Black men to young White men. In fact, in our analysis of the NESARC data, we found the strongest inverse relation between race and depression among those in middle age and those who were more educated, which is inconsistent with the selection bias hypothesis as it has been described in the literature. Therefore, we conclude that our data do not lend support to the selection bias hypothesis.
Two types of measurement bias have been offered as potential explanations for the lower prevalence of depression in Blacks. First, evidence suggests clinicians are more likely to diagnose Blacks with a psychotic spectrum disorder and Whites with a depressive disorder, when both have the same symptom profile [50, 51]. Second, diagnostic nosology might more efficiently capture symptom presentations of depression in Whites than in Blacks [19, 52–54]. Although depressed Blacks may be misdiagnosed with a psychotic spectrum disorder more frequently than depressed Whites, this measurement error is unlikely to explain a meaningful portion of the Black–White MDD prevalence difference given the rarity of psychotic spectrum disorders compared with MDD [55]. Likewise, a study of differential item functioning between Blacks and Whites in the diagnostic interview for MDD revealed differences at the item level that, as a whole, made little change in the prevalence of MDD in either group [14]. Nevertheless, measurement error can take many additional forms, and consequently, there is need for further work in this area.
Recently, Jackson et al. [21, 23, 56] have found support for their substantive hypothesis that engagement in unhealthy eating and substance use behaviors in the face of life stressors is more protective against major depression in Blacks than in Whites. This is an elegant proposal because it simultaneously attempts to account for the better stress-related mental health and worse physical health outcomes in Blacks compared with Whites in the US. Our recent [22] test of the hypothesis using NESARC data failed to support this hypothesis, however. This study found that engaging in unhealthy behaviors was not protective against MDD in either Blacks or Whites, both in general and at different levels of stressor exposure. Moreover, Jackson et al.’s hypothesis is contradicted by the reliable findings in epidemiology that high BMI and substance use disorders are comorbid with major depression in Blacks and in Whites [22, 43, 57, 58] and that Blacks are less likely than Whites to have nicotine, alcohol, or other substance use disorders [55, 59] and more likely to be lifetime abstainers [22, 60, 61].
Finally, it has been argued that religiosity, racial socialization, and high self-esteem, each of which is known to be protective against depression as well as more prevalent in Blacks than in Whites may explain the Black–White depression paradox [2, 4, 15, 62, 63]. However, to date, the extent to which these factors explain the lower prevalence of MDD in Blacks compared with Whites has not been adequately tested. We posit that formal hypotheses regarding these factors would need to indicate uniform effects across subgroups to be consistent with the findings we report here.
Notably, we found that lower odds of MDD in Blacks compared with Whites were particularly pronounced in the second and third age quartiles (ages 30 to 64), controlling for sex and education in the NESARC data. Those aged 30 to 64 at the time NESARC was conducted were born between 1937 and 1971 and one could argue that, on balance, Blacks born during these years in the US, compared with those born before and after, experienced more pronounced civil rights’ expansions and improving economic opportunities both while coming of age and during working years [64, 65]—environmental factors plausibly protective against major depression. The potential for cohort effects on depression that would have mechanisms specific to Blacks in the US is, to our knowledge, an under-examined research question; a more comprehensive understanding of cohort-level processes that might protect Blacks from depression may be a fruitful area to understand the macro-level social context and its effects on mental health [66]. A related topic also in need of greater scrutiny is age-of-onset differences in major depression between Blacks and Whites. Breslau et al. [2] showed that Black–White differences in mood disorder prevalence did not vary across early and late ages of onset, suggesting, they argue, protective factors in Blacks that start early in life. Testing for age of onset differences for MDD more specifically could likewise illuminate potential explanations for the paradox.
Limitations of these analyses should be noted. All diagnoses of major depression were based on self-reported diagnostic information and therefore lack external validation. This may have led to some misclassification of the outcome, which could be differential or non-differential with respect to race. To the extent misclassification of major depression is non-differential by race, our results would be biased to the null. In this case, the paradox would be even greater than the NESARC and replication data suggested. Potential misclassification that is differential by race should be considered in further studies. The purpose of our study was to provide a clearer roadmap for developing hypotheses to explain the paradoxical finding across psychiatric epidemiology studies that Blacks have a lower prevalence of major depression than Whites. Accordingly, by not minimizing possible biases in the NESARC or NCS-R/NSAL studies, we hope to expose pathways by which these biases may actually be operating.
In this study, we provide the foundation for future hypotheses attempting to explain the consistent finding in psychiatric epidemiology studies in the US of a lower prevalence of major depression in Blacks compared to Whites. We found across two of the largest psychiatric epidemiologic surveys conducted to date that subgroup results are mostly concordant with the overall finding and never statistically significantly discordant with it. We considered the selection bias hypothesis—that depression in Blacks is undercounted in studies using household samples—in light of our findings and ruled it out specifically because it postulates a bias far more operant in some subgroups than others. Future proposals to explicate the finding of lower levels of depression in Blacks compared to Whites need to offer global mechanisms that operate more or less consistently across the socio-economic subgroups we define in our study.
Supplementary Material
Acknowledgments
This research was supported by a fellowship from the National Institute of Mental Health (T32 MH013043, first author) and support from the other authors’ university. The funder had no role in the design and conduct of the study; in the collection, management, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s00127-013-0718-7) contains supplementary material, which is available to authorized users.
Conflict of interest None declared.
Contributor Information
David M. Barnes, Email: dmb23@columbia.edu, Department of Epidemiology, Mailman School of Public Health, Columbia University, 722 W. 168th Street, Room 720D, New York, NY 10032, USA
Katherine M. Keyes, Department of Epidemiology, Mailman School of Public Health, Columbia University, 722 W. 168th Street, Room 503, New York, NY 10032, USA
Lisa M. Bates, Department of Epidemiology, Mailman School of Public Health, Columbia University, 722 W. 168th Street, Room R808, New York, NY 10032, USA
References
- 1.Blazer DG, Kessler RC. The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry. 1994;151:979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- 2.Breslau J, Aguilar-Gaxiola S, Kendler KS, Su M, Williams D, Kessler RC. Specifying race-ethnic differences in risk for psychiatric disorder in a US national sample. Psychol Med. 2006;36:57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 4.Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, Jackson JS. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64:305. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 5.Dohrenwend BP. The role of adversity and stress in psychopathology: some evidence and its implications for theory and research. J Health Soc Behav. 2000;41:1–19. [PubMed] [Google Scholar]
- 6.Kessler RC. The effects of stressful life events on depression. Annu Rev Psychol. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- 7.Monroe SM, Slavich GM, Georgiades K. Handbook of depression. 2. The Guilford Press; New York: 2009. The social environment and life stress in depression; pp. 340–360. [Google Scholar]
- 8.Boardman JD. Health pessimism among black and white adults: the role of interpersonal and institutional maltreatment. Soc Sci Med. 2004;59:2523–2533. doi: 10.1016/j.socscimed.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 9.Boardman JD, Alexander KB. Stress trajectories, health behaviors, and the mental health of black and white young adults. Soc Sci Med. 2011;72:1659–1666. doi: 10.1016/j.socscimed.2011.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meyer IH, Schwartz S, Frost DM. Social patterning of stress and coping: does disadvantaged social statuses confer more stress and fewer coping resources? Soc Sci Med. 2008;67:368–379. doi: 10.1016/j.socscimed.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schulz A, Israel B, Williams D, Parker E, Becker A, James S. Social inequalities, stressors and self reported health status among African American and white women in the Detroit metropolitan area. Soc Sci Med. 2000;51:1639–1654. doi: 10.1016/s0277-9536(00)00084-8. [DOI] [PubMed] [Google Scholar]
- 12.Taylor J, Turner RJ. Perceived discrimination, social stress, and depression in the transition to adulthood: racial constrasts. Soc Psychol Q. 2002;65:213–225. [Google Scholar]
- 13.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health, socio-economic status, stress and discrimination. J Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 14.Breslau J, Javaras KN, Blacker D, Murphy JM, Normand SLT. Differential item functioning between ethnic groups in the epidemiological assessment of depression. J Nerv Ment Dis. 2008;196:297–306. doi: 10.1097/NMD.0b013e31816a490e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keyes CLM. The black–white paradox in health: flourishing in the face of social inequality and discrimination. J Pers. 2009;77:1677–1706. doi: 10.1111/j.1467-6494.2009.00597.x. [DOI] [PubMed] [Google Scholar]
- 16.Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annu Rev Psychol. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams DR. Racial variations in adult health status: patterns, paradoxes, and prospects. In: Smelser NJ, Wilson WJ, Mitchell F, editors. America becoming: racial trends and their consequences. National Academy Press; Washington: 2001. pp. 371–410. [Google Scholar]
- 18.Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychol Med. 2005;35:317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown TN. Critical race theory speaks to the sociology of mental health: mental health problems produced by racial stratification. J Health Soc Behav. 2003;44:292–301. [PubMed] [Google Scholar]
- 20.Neighbors HW, Williams DR. The epidemiology of mental disorder. In: Braithwaite RL, Taylor SE, editors. Health issues in the Black community. Jossey-Bass Publishers; San Francisco: 2001. pp. 99–128. [Google Scholar]
- 21.Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health. 2010;100:933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keyes KM, Barnes DM, Bates LM. Stress, coping, and depression: testing a new hypothesis in a prospectively studied general population sample of US-born whites and blacks. Soc Sci Med. 2011;72:650–659. doi: 10.1016/j.socscimed.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mezuk B, Rafferty JA, Kershaw KN, Hudson D, Abdou CM, Lee H, Eaton WW, Jackson JS. Reconsidering the role of social disadvantage in physical and mental health: stressful life events, health behaviors, race, and depression. Am J Epidemiol. 2010;172:1238–1249. doi: 10.1093/aje/kwq283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Breslau J, Chang DF. Psychiatric disorders among foreign-born and US-born Asian-Americans in a US national survey. Soc Psychiatry Psychiatr Epidemiol. 2006;41:943–950. doi: 10.1007/s00127-006-0119-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dey AN, Lucas JW. Physical and mental health characteristics of US-and foreign-born adults, United States, 1998–2003. Adv Data Vital Health Stat. 2006;369:1–20. [PubMed] [Google Scholar]
- 26.Grant BF. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic Whites in the United States: results From the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:1226. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- 27.Miranda J, Siddique J, Belin TR, Kohn-Wood LP. Depression prevalence in disadvantaged young black women. Soc Psychiatry Psychiatr Epidemiol. 2005;40:253–258. doi: 10.1007/s00127-005-0879-0. [DOI] [PubMed] [Google Scholar]
- 28.Mays VM, Cochran SD, Ponce NA. Thinking about race and ethnicity in population-based studies of health. In: Beech BM, Goodman M, editors. Race and research: perspectives on minority participation in health studies. American Public Health Association; Washington: 2004. pp. 79–100. [Google Scholar]
- 29.Schwartz S, Meyer IH. Mental health disparities research: the impact of within and between group analyses on tests of social stress hypotheses. Soc Sci Med. 2010;70:1111–1118. doi: 10.1016/j.socscimed.2009.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams DR, Harris-Reid M. Race and mental health: emerging patterns and promising approaches. In: Horwitz AV, Scheid TL, editors. A handbook for the study of mental health: social contexts, theories, and systems. Cambridge University Press; Cambridge: 1999. pp. 295–314. [Google Scholar]
- 31.Bassuk EL, Buckner JC, Perloff JN, Bassuk SS. Prevalence of mental health and substance use disorders among homeless and low-income housed mothers. Am J Psychiatry. 1998;155:1561–1564. doi: 10.1176/ajp.155.11.1561. [DOI] [PubMed] [Google Scholar]
- 32.Koegel P, Burnam AM, Farr RK. The prevalence of specific psychiatric disorders among homeless individuals in the inner city of Los Angeles. Arch Gen Psychiatry. 1988;45:1085–1092. doi: 10.1001/archpsyc.1988.01800360033005. [DOI] [PubMed] [Google Scholar]
- 33.Teplin LA. The prevalence of severe mental disorder among male urban jail detainees: comparison with the Epidemiologic Catchment Area Program. Am J Public Health. 1990;80:663–669. doi: 10.2105/ajph.80.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA. Psychiatric disorders in youth in juvenile detention. Arch Gen Psychiatry. 2002;59:1133–1143. doi: 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Trestman RL, Ford J, Zhang W, Wiesbrock V. Current and lifetime psychiatric illness among inmates not identified as acutely mentally ill at intake in Connecticut’s jails. J Am Acad Psychiatry Law. 2007;35:490–500. [PubMed] [Google Scholar]
- 36.Gadermann AM, Engel CC, Naifeh JA, Nock MK, Petukhova M, Santiago PN, Wu B, Zaslavsky AM, Kessler RC. Prevalence of DSM-IV major depression among U.S. military personnel: meta-analysis and simulation. Mil Med. 2012;177:47–59. doi: 10.7205/milmed-d-12-00103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Armor DJ, Gilroy CL. Changing minority representation in the US military. Armed Forces Soc. 2010;36:223–246. [Google Scholar]
- 38.Glaze LE. Correctional population in the United States, 2010. US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; Washington, DC: 2011. pp. 1–8. [Google Scholar]
- 39.Cortes A, Leopold J, Rothschild L, Buron L, Khadduri J, Culhane DP. The 2010 annual homeless assessment report to Congress.2011. [Google Scholar]
- 40.Pettit B, Western B. Mass imprisonment and the life course: race and class inequality in US incarceration. Am Sociol Rev. 2004;69:151–169. [Google Scholar]
- 41.Williams DR, Takeuchi DT, Adair RK. Socioeconomic status and psychiatric disorder among blacks and whites. Soc Forces. 1992;71:179–194. [PubMed] [Google Scholar]
- 42.Kessler RC, Neighbors HW. A new perspective on the relationships among race, social class, and psychological distress. J Health Soc Behav. 1986;27:107–115. [PubMed] [Google Scholar]
- 43.Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- 44.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 45.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 46.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder. JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 47.Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the collaborative psychiatric epidemiology studies (CPES) Int J Methods Psychiatr Res. 2004;13:221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pennell BE, Bowers A, Carr D, Chardoul S, Cheung G, Dinkelmann K, Gebler N, Hansen SE, Pennell S, Torres M. The development and implementation of the national comorbidity survey replication, the national survey of American life, and the national Latino and Asian American survey. Int J Methods Psychiatr Res. 2004;13:241–269. doi: 10.1002/mpr.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Canino G, Bravo M, Ramirez R, Febo VE, Rubio-Stipec M, Lewis-Fernandez R, Hasin D. The Spanish alcohol use disorder and associated disabilities interview schedule (AUDA-DIS): reliability and concordance with clinical diagnoses in a Hispanic population. J Stud Alcohol. 1999;60:790–799. doi: 10.15288/jsa.1999.60.790. [DOI] [PubMed] [Google Scholar]
- 50.Neighbors HW, Trierweiler SJ, Munday C, Thompson EE, Jackson JS, Binion VJ, Gomez J. Psychiatric diagnosis of African Americans: diagnostic divergence in clinician-structured and semi structured interviewing conditions. J Natl Med Assoc. 1999;91:601–612. [PMC free article] [PubMed] [Google Scholar]
- 51.Strakowski SM, Keck PE, Arnold LM, Collins J, Wilson RM, Fleck DE, Corey KB, Amicone J, Adebimpe VR. Ethnicity and diagnoses in patients with affective disorders. J Clin Psychiatry. 2003;64:747–754. doi: 10.4088/jcp.v64n0702. [DOI] [PubMed] [Google Scholar]
- 52.Baker FM. Diagnosing depression in African Americans. Community Ment Health J. 2001;37:31–38. doi: 10.1023/a:1026540321366. [DOI] [PubMed] [Google Scholar]
- 53.Kleinman A. Culture and depression. N Engl J Med. 2004;351:951–953. doi: 10.1056/NEJMp048078. [DOI] [PubMed] [Google Scholar]
- 54.Rogler LH. Methodological sources of cultural insensitivity in mental health research. Am Psychol. 1999;54:424–433. doi: 10.1037//0003-066x.54.6.424. [DOI] [PubMed] [Google Scholar]
- 55.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the national comorbidity survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 56.Jackson JS, Knight KM. Race and self-regulatory health behaviors: the role of the stress response and the HPA axis in physical and mental health disparities. In: Schaie KW, Carstensen LL, editors. Social structures, aging, and self-regulation in the elderly. Springer; New York: 2006. pp. 189–207. [Google Scholar]
- 57.Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000;90:251–257. doi: 10.2105/ajph.90.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Grant BF. Comorbidity between DSM-IV drug use disorders and major depression: results of a national survey of adults. J Subst Abus. 1995;7:481–497. doi: 10.1016/0899-3289(95)90017-9. [DOI] [PubMed] [Google Scholar]
- 59.Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 60.Gilman SE, Breslau J, Conron KJ, Koenen KC, Subramanian SV, Zaslavsky AM. Education and race-ethnicity differences in the lifetime risk of alcohol dependence. J Epidemiol Community Health. 2008;62:224–230. doi: 10.1136/jech.2006.059022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Grant BF. Prevalence and correlates of alcohol use and DSM-IV alcohol dependence in the United States: results of the national longitudinal alcohol epidemiologic survey. J Stud Alcohol. 1997;58:464–473. doi: 10.15288/jsa.1997.58.464. [DOI] [PubMed] [Google Scholar]
- 62.Fischer AR, Shaw CM. African Americans’ mental health and perceptions of racist discrimination: the moderating effects of racial socialization experiences and self-esteem. J Couns Psychol. 1999;46:395–407. [Google Scholar]
- 63.Williams DR, Fenton BT, Livingston IL. The Mosaic of Conditions, Issues, Policies, and Prospects. Greenwood Press; Westport, Conn: 1994. The mental health of African Americans: findings, questions, and directions; pp. 253–268. Handbook of Black American health. [Google Scholar]
- 64.Mason PL. Race, cognitive ability, and wage inequality. Challenge. 1998;41:63–84. [Google Scholar]
- 65.Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annu Rev Sociol. 1995;21:349–386. [Google Scholar]
- 66.Keyes KM, Liu X. Life course epidemiology of mental disorders. Age, period, and birth cohort effects in psychiatric disorders in the United States. (in press) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.