Abstract
Various surgical treatment procedures for plantar fasciitis, such as open surgery, percutaneous release, and endoscopic surgery, exist. Skin trouble, nerve disturbance, infection, and persistent pain associated with prolonged recovery time are complications of open surgery. Endoscopic partial plantar fascia release offers the surgeon clear visualization of the anatomy at the surgical site. However, the primary medial portal and portal tract used for this technique have been shown to be in close proximity to the posterior tibial nerves and their branches, and there is always the risk of nerve damage by introducing the endoscope deep to the plantar fascia. By performing endoscopic partial plantar fascia release under ultrasound assistance, we could dynamically visualize the direction of the endoscope and instrument introduction, thus preventing nerve damage from inadvertent insertion deep to the fascia. Full-thickness release of the plantar fascia at the ideal position could also be confirmed under ultrasound imaging. We discuss the technique for this new procedure.
Plantar fasciitis is a common cause of chronic heel pain.1 The primary method of care is conservative therapy, such as oral intake of nonsteroidal anti-inflammatory drugs, physiotherapy including stretching of the plantar fascia, activity modification, use of shoe insoles, injection of corticosteroids, and extracorporeal shock wave therapy.1-4 Although most cases respond well to such conservative therapy, some patients do not respond to this type of treatment or have recurrence of symptoms and may progress to surgical release.5,6
Various surgical procedures for plantar fasciitis release exist, such as open surgery,7-10 percutaneous release, and endoscopic surgery.11-14 Skin trouble, nerve disturbance, infection, and persistent pain associated with prolonged recovery time are complications of open surgery.8,15 Percutaneous release is not a reliable method because of its inability to allow visualization of the plantar fascia. Endoscopic partial plantar fascia release (EPFR) offers the surgeon clear visualization of the anatomy at the surgical site and was developed recently to decrease the occurrence of surgical complications and shorten the duration to return to the initial level of activities. However, the primary medial portal and portal tract used for this technique have been shown to be in close proximity to the posterior tibial nerve and its branches (Fig 1), and there is always the risk of nerve damage by introducing the arthroscopic cannula deep to the plantar fascia.16 To prevent this risk, we have been performing EPFR under ultrasound assistance (Video 1). Tips for ultrasound use during EPFR are presented in Table 1. The purpose of this report is to discuss our technique of ultrasound-assisted EPFR.
Fig 1.
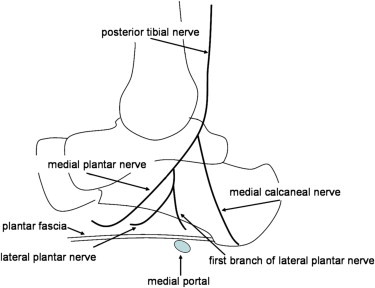
The medial portal and portal tract are in close proximity to the posterior tibial nerve and its branches, running distal and deep to the proximal calcaneal attachment of the plantar fascia. Ultrasound assistance prevents inadvertent insertion deep to the fascia, causing nerve damage.
Table 1.
Tips for Ultrasound Use During EPFR
| Tips | Reasons |
|---|---|
| Prevent wrinkling of probe cover | Prevent ultrasound artifact |
| Use sterile gel inside cover and between skin | Obtain better ultrasound conduction |
| Hold probe perpendicular to anatomy | Obtain clearer contour of structure |
| Adjust focus to intended depth | Obtain clear image |
| Hold skin with probe during study | Prevent slipping of probe |
| Visualize fascia in 2 planes | Obtain 3-dimensional orientation |
Surgical Technique
Under general anesthesia, the patient is placed in the supine position with the ankle off the edge of the table. A tourniquet is used. The ultrasound machine (LOGIC E9; GE Healthcare Japan, Tokyo, Japan) and high-frequency linear probe (ML6-15-D; GE Healthcare Japan) are prepared with a sterile ultrasound probe cover and sterile gel. We use the ECTRA II Carpal Ligament System (Smith & Nephew KK, Tokyo, Japan) to perform this surgical technique.
The medial portal is located at the point of intersection between 2 lines: a longitudinal line at the posterior border of the medial malleolus and a transverse line perpendicular to the first line, dividing the plantar and dorsal skin of the foot (Fig 2). A skin incision of approximately 5 mm is made with a No. 11 knife blade, followed by dissection of subcutaneous fat with a small mosquito forceps. A blunt dissector is used to gently clear the plantar surface of the fascia from the heel fat pad under ultrasound assistance. The fascia can be palpated and the route cleared for passage of the slotted cannula. It is important that the cannula contacts the fascia as closely as possible, superficial to it, to minimize trauma to the fat pad to avoid postoperative hematoma and also to avoid any risk of nerve damage. This can be easily performed under ultrasound assistance. A slotted metal cannula and obturator are then passed from medial to lateral until the lateral border of the foot is reached, at the junction between the plantar skin and the dorsal skin. Great care is taken to make sure that the cannula is inserted perpendicular to the long axis of the foot. When the tip of the obturator is felt subcutaneously, the skin is incised approximately 5 mm to make the lateral portal, and the cannula is advanced to come out of the portal. Thus the cannula is placed across the plantar fascia from medial to lateral and should lie just plantar to, and in contact with, the fascia. The obturator is then removed, and the cannula is rotated so that the slot faces the fascia.
Fig 2.
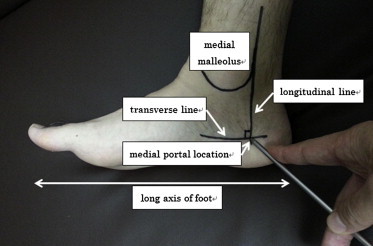
Medial view of right foot. The medial portal is located at the intersection between a longitudinal line at the posterior border of the medial malleolus and a transverse line dividing the plantar and dorsal skin. Insertion of the endoscope and instruments from this portal and perpendicular to the long axis of the foot is essential for release of the plantar fascia at its proximal calcaneal attachment.
The endoscope is then introduced from the medial portal. Sometimes there may be fat overlying the fascia. In this case we use initial irrigation and sterile swabs or a hooked probe to scrape away the fat to clearly visualize the shiny fibers of the fascia. Usually no irrigation is necessary during the release because the tourniquet ensures a bloodless field. The hooked probe is passed medially and used to evaluate the medial and lateral borders of the plantar fascia.
A small triangular knife is passed medially from the lateral portal, and under direct vision, it is used to completely divide the fibers of the plantar fascia at the lateral one-third position. The division is complete when the underlying muscle is visualized. Next, an antegrade knife is used by pushing medially from the lateral portal to release the medial two-thirds of the fascia. The hooked probe is used to ensure completion of the release endoscopically. Ultrasound evaluation of the plantar fascia is also performed at this time, and a full-thickness release at the ideal position is confirmed.
After thorough irrigation of the operative field, the cannula is removed and the portals are closed with No. 3-0 nylon. Bulky dressing with a tensor bandage is applied, and the foot is elevated.
Postoperative Care and Rehabilitation
Patients are allowed to start partial weight bearing 1 day after surgery. Stretching of the plantar fascia is started as tolerated. Sutures are removed in 1 week, and full weight bearing is started on the following day. We prescribe nonsteroidal anti-inflammatory medicine for 2 weeks if the patients have postoperative pain. Usually the patients are symptom free by 1 month after surgery, and at this time, long-distance walking is allowed. We do not allow the patients to perform high-impact activities such as running for at least 2 months, and athletes participate in a sports-specific training program before returning to sports.
Discussion
Complication rates after EPFR have been reported to range from 3% to 10%.1,16,17 Although neurologic complication rates are not very high, there is the risk of nerve damage by introducing the arthroscopic cannula deep to the plantar fascia and it has been reported previously by various authors.16,18,19 Barrett et al.18 reported on numbness around the fifth metatarsal due to lateral plantar nerve injury, and Komatsu et al.19 reported on plantar paresthesia after the deep fascia approach.
Various methods for preventing such complications during cannula placement have been reported, from simple palpation of bony landmarks1,16,18 to the use of lateral radiographs20 and image intensifiers.19 However, the thick fat pad surrounding the calcaneus prevents accurate palpation, and radiation exposure is an issue when one is using radiographs and image intensifiers. On the other hand, ultrasound imaging allows multi-planar and real-time imaging without radiation exposure. Although ultrasound imaging has been previously considered to be operator dependent with poor repeatability, recent studies have established moderate to good interobserver reliability.21,22
All the advantages and disadvantages of ultrasound-assisted EPFR are presented in Table 2. Disadvantages exist, such as requiring a high-frequency ultrasound device and increasing the operative time especially during the learning curve, which is steep. However, the advantages outnumber the disadvantages, and the greatest advantage of this technique is that it enables us to dynamically visualize the plantar fascia as well as the direction of the endoscope and instrument introduction, thus preventing nerve damage from inadvertent insertion deep to the fascia.
Table 2.
Advantages and Disadvantages of Ultrasound-Assisted EPFR
| Advantages | Disadvantages |
|---|---|
| No radiation exposure | Requires high-frequency ultrasound device |
| Allows multiplanar and real-time imaging | Operator dependent |
| Allows visualization of plantar fascia and superficial fat pad (minimizing trauma to fat pad and postoperative hematoma) | Increased operative time |
| Steep learning curve | |
| Allows visualization of endoscope and instrument introduction (prevent nerve damage from inadvertent introduction deep to fascia) | |
| Confirmation of full-thickness release at ideal position |
In summary, we have described the technique of ultrasound-assisted EPFR. Precise release of the plantar fascia with lower complication rates results in quicker recovery time, and we believe that this new technique has all the potential advantages of minimally invasive surgery.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary data
Key principles and technical pearls of ultrasound-assisted endoscopic plantar fascia release.
References
- 1.Shazly O.E., El Hilaly R.A., Maged M. Endoscopic plantar fascia release by hooked soft-tissue electrode after failed shock wave therapy. Arthroscopy. 2010;26:1241–1245. doi: 10.1016/j.arthro.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 2.Bordelon R.L. Heel pain. In: Mann R.A., editor. Surgery of the foot and ankle. CV Mosby; St. Louis: 1993. pp. 837–847. [Google Scholar]
- 3.Landorf K.B., Keenan A.M., Herbert R.D. Effectiveness of different types of foot orthoses for the treatment of plantar fasciitis. J Am Podiatr Med Assoc. 2004;94:542–549. doi: 10.7547/0940542. [DOI] [PubMed] [Google Scholar]
- 4.Martin J.E., Hosch J.C., Goforth W.P. Mechanical treatment of plantar fasciitis. A prospective study. J Am Podiatr Med Assoc. 2001;91:55–62. doi: 10.7547/87507315-91-2-55. [DOI] [PubMed] [Google Scholar]
- 5.Rompe J.D., Schoellner C., Nafe B. Evaluation of low-energy extracorporeal shock-wave application for treatment of chronic plantar fasciitis. J Bone Joint Surg Am. 2002;84:335–341. doi: 10.2106/00004623-200203000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Chuckpaiwong B., Berkson E.M., Theodore G.H. Extracorporeal shock wave for chronic proximal plantar fasciitis: 225 patients with results and outcome predictors. J Foot Ankle Surg. 2009;48:148–155. doi: 10.1053/j.jfas.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Daly P.J., Kitaoka H.B., Chao E.Y. Plantar fasciotomy for intractable plantar fasciitis: Clinical results and biomechanical evaluation. Foot Ankle. 1992;13:188–195. doi: 10.1177/107110079201300404. [DOI] [PubMed] [Google Scholar]
- 8.Tomczak R.L., Haverstock B.D., II A retrospective comparison of endoscopic plantar fasciotomy to open plantar fasciotomy with heel spur resection for chronic plantar fasciitis/heel spur syndrome. J Foot Ankle Surg. 1995;34:305–311. doi: 10.1016/S1067-2516(09)80065-3. [DOI] [PubMed] [Google Scholar]
- 9.Davies M.S., Weiss G.A., Saxby T.S. Plantar fasciitis: How successful is surgical intervention? Foot Ankle Int. 1999;20:803–807. doi: 10.1177/107110079902001209. [DOI] [PubMed] [Google Scholar]
- 10.Woelffer K.E., Figura M.A., Sandberg N.S., Snyder N.S. Five-year follow-up results of instep plantar fasciotomy for chronic heel pain. J Foot Ankle Surg. 2000;39:218–223. doi: 10.1016/s1067-2516(00)80003-4. [DOI] [PubMed] [Google Scholar]
- 11.Lundeen R.O., Aziz S., Burks J.B., Rose J.M. Endoscopic plantar fasciotomy: A retrospective analysis of results in 53 patients. J Foot Ankle Surg. 2000;39:208–217. doi: 10.1016/s1067-2516(00)80002-2. [DOI] [PubMed] [Google Scholar]
- 12.Blanco C.E., Leon H.O., Guthrie T.B. Endoscopic treatment of calcaneal spur syndrome: A comprehensive technique. Arthroscopy. 2001;17:517–522. doi: 10.1053/jars.2001.24065. [DOI] [PubMed] [Google Scholar]
- 13.Boyle R.A., Slater G.L. Endoscopic plantar fascia release: A case series. Foot Ankle Int. 2003;24:176–179. doi: 10.1177/107110070302400213. [DOI] [PubMed] [Google Scholar]
- 14.Hogan K.A., Webb D., Shereff M. Endoscopic plantar fascia release. Foot Ankle Int. 2004;25:875–881. doi: 10.1177/107110070402501206. [DOI] [PubMed] [Google Scholar]
- 15.Kinley S., Frascone S., Calderone D. Endoscopic plantar fasciotomy versus traditional heel spur surgery: A prospective study. J Foot Ankle Surg. 1993;32:595–603. [PubMed] [Google Scholar]
- 16.Ogilvie-Harris D.J., Lobo J. Endoscopic plantar fascia release. Arthroscopy. 2000;16:290–298. doi: 10.1016/s0749-8063(00)90053-7. [DOI] [PubMed] [Google Scholar]
- 17.Urovitz E.P., Birk-Urovitz A., Birk-Urovitz E. Endoscopic plantar fasciotomy in the treatment of chronic heel pain. Can J Surg. 2008;51:281–283. [PMC free article] [PubMed] [Google Scholar]
- 18.Barrett S.L., Day S.V., Pignetti T.T., Robinson L.B. Endoscopic plantar fasciotomy: A multi-surgeon prospective analysis of 652 cases. J Foot Ankle Surg. 1995;34:400–406. doi: 10.1016/S1067-2516(09)80011-2. [DOI] [PubMed] [Google Scholar]
- 19.Komatsu F., Takao M., Innami K., Miyamoto W., Matsushita T. Endoscopic surgery for plantar fasciitis: Application of a deep-fascial approach. Arthroscopy. 2011;27:1105–1109. doi: 10.1016/j.arthro.2011.02.037. [DOI] [PubMed] [Google Scholar]
- 20.Hake D.H. Endoscopic plantar fasciotomy: A minimally traumatic procedure for chronic plantar fasciitis. Ochsner J. 2000;2:175–178. [PMC free article] [PubMed] [Google Scholar]
- 21.Iagnocco A., Perricone C., Scirocco C. The interobserver reliability of ultrasound in knee osteoarthritis. Rheumatology. 2012;51:2013–2019. doi: 10.1093/rheumatology/kes161. [DOI] [PubMed] [Google Scholar]
- 22.Naredo E., Moller I., Moragues C. Interobserver reliability in musculoskeletal ultrasonography: Results from a “teach the teachers” rheumatologist course. Ann Rheum Dis. 2006;65:14–19. doi: 10.1136/ard.2005.037382. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Key principles and technical pearls of ultrasound-assisted endoscopic plantar fascia release.


