Abstract
Prophylactic extraction of unerupted asymptomatic third molars is the most common oral surgery procedure in the United States. However, limited evidence exists to justify its costs and associated morbidity. We analyzed data collected over 25 years from 416 adult men enrolled in the Veterans Affairs Dental Longitudinal Study to evaluate the association of retained asymptomatic third molars with risk of adjacent second molar pathology (caries and/or periodontitis), based on third molar status (i.e., absent, erupted, or unerupted). Unerupted molars were further categorized as either “soft tissue” or “bony” impacted. We found that the lowest prevalence and incidence of second molar pathology occurred when the adjacent third molar was absent. The presence of a third molar that was soft tissue impacted increased the risk of incident second molar pathology 4.88-fold (95% confidence interval: 2.62, 9.08). Having an erupted or “bony” impacted third molar increased the risk of incident second molar pathology by 1.74 (95% confidence interval: 1.34, 2.25) and 2.16 (95% confidence interval: 1.56, 2.99), respectively. The retention of third molars is associated with increased risk of second molar pathology in middle-aged and older adult men.
Keywords: caries, periodontal disease, cohort study, alveolar bone loss, longitudinal study
Introduction
Prophylactic extraction of unerupted asymptomatic third molars is the most common oral surgery procedure in the United States. One rationale given for extracting teeth that are disease-free is to prevent future disease in adjacent teeth. However, there is limited evidence available regarding risk of caries and periodontitis in second molars adjacent to retained third molars.
We have used available longitudinal data from an observational cohort study of adult U.S. men to examine the association of third molar status with prevalent and incident caries and periodontal outcomes in adjacent second molars.
Materials & Methods
We used data from the U.S. Department of Veterans Affairs Dental Longitudinal Study, a subset of the closed-panel longitudinal Veterans Affairs Normative Aging Study, based in Boston, Massachusetts. Beginning in 1961, the Normative Aging Study enrolled 2,280 medically healthy male volunteers, aged 25 to 84 yrs, from the Greater Boston area. A subset of 1,231 volunteers enrolled in the Dental Longitudinal Study beginning in 1969 (Kapur et al., 1972). Men were not Veterans Affairs patients and have gotten their medical and dental care in the private sector. Subjects received comprehensive oral examinations approximately every 3 years by a trained, calibrated periodontist. Panoramic and intraoral full-mouth radiographs were also taken. Interproximal alveolar bone loss was measured from full mouth radiographs with a Schei ruler (Schei et al., 1959). Over 25 years of data were available for analyses.
We identified 416 subjects who had both first and second molars present in at least 1 quadrant at baseline and had at least 1 follow-up examination. Third molar status was assessed from radiographs by a board-certified oral and maxillofacial surgeon (RF) and a board-certified oral and maxillofacial radiologist (AG). Third molars were categorized for analyses as absent, erupted, or unerupted, with the last subcategorized as either “soft tissue” or “bony” impacted, based on the extent that the radiographic coronal aspect was covered by bone. Bony impacted third molars include those with at least two-thirds impacted in bone. Soft tissue impacted third molars include all soft tissue impactions and partial bony impactions with less than two-thirds impacted in bone.
The association of third molar status to second molar outcomes was examined both cross-sectionally and longitudinally, using generalized estimating equation logistic regression models and multivariate survival analysis. The reference group for all analyses was second molars adjacent to absent third molars. For cross-sectional analysis, second molar outcomes included distal caries experience (either primary or secondary caries), distal alveolar bone loss ≥ 20%, and distal probing depth > 4 mm. For the longitudinal analyses, incidence of these outcomes was used. All analyses were adjusted for baseline age, smoking status, and education. Longitudinal analyses were also adjusted for corresponding baseline second molar measures. Marginal survival analysis was utilized to account for multiple outcomes within subjects. The proportional hazards assumption was verified graphically and by testing inclusion of interaction terms with log of time.
In addition to analysis of the complete data set, a subset was constructed of subjects with an absent third molar on one side and an unerupted or erupted third molar on the opposite side; 54 subjects were found to have an absent third molar on one side and either unerupted or erupted third molars on the opposite side. Survival analysis was conducted to examine the association of third molar status to development of any pathology on adjacent second molars in this subset. A subset of subjects with an absent third molar on one side and an unerupted third molar on the opposite side was also constructed, but the sample included only 13 subjects, so formal analysis was not possible. The eventual loss of adjacent second molars was also explored. Unfortunately, the small subsample size also precluded a formal analysis, as only 29 second molars were lost over time. However, a survival plot was constructed for loss of second molars by third molar status.
The protocol was approved by the Veterans Affairs Subcommittee on Human Studies, VA Boston Healthcare System, and the Boston University Medical Campus Institutional Review Board. All procedures were in accordance with institutional guidelines. All subjects provided written informed consent. This study conforms to the STROBE guidelines.
Results
Table 1 shows subjects’ baseline characteristics and distribution of third molar status for all quadrants included in the study. Appendix Table 1 shows the distribution of distal caries experience, distal bone loss, and periodontal pockets of second molars, by adjacent third molar status.
Table 1.
Baseline Characteristics of Subjects (N = 416) and Distribution of Third Molars (N = 804)
| Characteristics | % (n) |
|---|---|
| Age, y | |
| Mean ± SD | 45.8 ± 7.4 |
| Range | 28.1-76.2 |
| Smoking status | |
| Nonsmokers | 67.8 (282) |
| Smokers | 32.2 (134) |
| Educational status | |
| High school or less | 22.1 (92) |
| Some college | 37.5 (156) |
| College graduate | 40.4 (168) |
| Third Molar Status | |
| Absent | |
| Mandibular | 25.7 (207) |
| Maxillary | 31.5 (253) |
| Erupted | |
| Mandibular | 12.9 (104) |
| Maxillary | 15.7 (126) |
| Unerupteda | |
| Soft tissue impaction | |
| Mandibular | 1.0 (8) |
| Maxillary | 2.1 (17) |
| Bony impaction | |
| Mandibular | 6.6 (53) |
| Maxillary | 4.5 (36) |
Total percentage unerupted, 14.2%.
Cross-sectional Analysis
Appendix Table 2 shows odds ratios (ORs) from generalized estimating equation logistic regression modeling for distal caries experience, distal bone loss ≥ 20%, and distal probing depth > 4 mm of adjacent second molars. ORs were adjusted for baseline age, smoking status and education. Prevalent second molar disease differed significantly according to third molar status. Second molars adjacent to erupted third molars were more likely to have distal caries than second molars adjacent to absent third molars (OR = 1.73). Second molars adjacent to soft tissue impacted third molars were more likely to have distal bone loss ≥ 20% (OR = 4.93) and distal probing depth > 4 mm (OR = 3.98). Second molars adjacent to bony impacted third molars were more likely to have distal bone loss ≥ 20% (OR = 2.64).
Longitudinal Analysis
Tables 2 and 3 show relative risks (RR) from multivariate survival regression modeling for incidence of distal caries, distal bone loss ≥ 20%, distal probing depth > 4 mm, and any one or more of these disease outcomes on second molars. RRs were adjusted for baseline age, smoking status, education, and corresponding baseline second molar measures. Results had similar trends to cross-sectional analyses with the exception of caries experience with results for soft tissue impactions and bony impactions reversed, although neither were statistically significant.
Table 2.
Survival Analysis for Incident Pathologies of Adjacent Second Molar
| Third Molar Status | Relative Risk | 95% Confidence Interval | pa |
|---|---|---|---|
| Caries experience | |||
| Absent | Reference | — | .003 |
| Erupted | 2.53 | 1.55, 4.14 | |
| Soft tissue impaction | 0.83 | 0.11, 6.04 | |
| Bony impaction | 1.44 | 0.55, 3.72 | |
| Distal bone loss, ≥ 20% | |||
| Absent | Reference | — | < .001 |
| Erupted | 1.49 | 0.96, 2.31 | |
| Soft tissue impaction | 9.15 | 4.63, 18.1 | |
| Bony impaction | 3.09 | 1.83, 5.22 | |
| Distal probing depth, > 4 mm | |||
| Absent | Reference | — | < .001 |
| Erupted | 1.87 | 1.25, 2.79 | |
| Soft tissue impaction | 6.41 | 2.92, 14.1 | |
| Bony impaction | 1.60 | 0.96, 2.67 |
Values are based on marginal multivariate survival regression models comparing third molar status while adjusting for age, smoking status, and educational status.
Table 3.
Survival Analysis for Any Incident Pathology on Distal of Adjacent Second Molar
| Third Molar Statusa | Relative Risk | 95% Confidence Interval | pa |
|---|---|---|---|
| Absent | Reference | — | < .0001 |
| Erupted | 1.74 | 1.34, 2.25 | |
| Soft tissue impaction | 4.88 | 2.62, 9.08 | |
| Bony impaction | 2.16 | 1.56, 2.99 |
Value is based on marginal multivariate survival regression models comparing third molar status impact on incident pathology of distal of adjacent second molars while adjusting for age, smoking status, and educational status.
Second molars adjacent to erupted third molars were at greater risk of incident distal caries (RR = 2.53) and incident distal probing depth > 4 mm (RR = 1.87) than were second molars adjacent to absent third molars, the reference group (Table 2). Second molars adjacent to soft tissue impacted third molars were at greater risk of incident distal bone loss ≥ 20% (RR = 9.15) and incident distal probing depth > 4 mm when compared to the reference group (RR = 6.41). Second molars adjacent to bony impacted third molars were at greater risk of incident distal bone loss ≥ 20% versus the reference group (RR = 3.09), although the risk was a third of that for soft tissue impactions.
An analysis was conducted using incidence of any 1 of the 3 disease outcomes (i.e., caries, bone loss ≥ 20%, probing depth > 4 mm) in adjacent second molars (Table 3). Compared to second molars adjacent to absent third molars, those adjacent to soft tissue impacted third molars were at highest risk for developing any one of these disease outcomes, followed by those adjacent to bony impacted or erupted third molars. The survival plot (Fig.) shows relative incidence of any second molar outcome according to status of adjacent third molars. Second molars adjacent to absent third molars were at lowest risk, while second molars adjacent to soft tissue impacted third molars were at greatest risk. Second molars adjacent to erupted third molars or bony impacted third molars were at an equivalent, intermediate risk over the 20+ years of follow-up.
Figure.
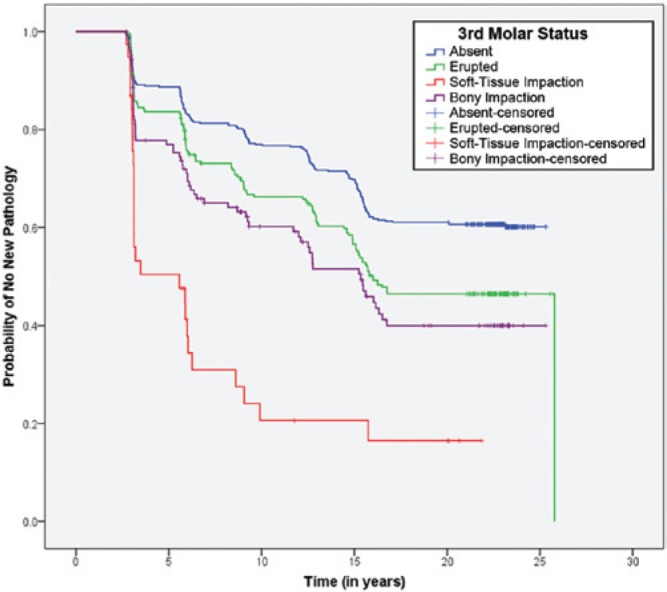
Survival plot for any incident pathology on distal of second molar by status of adjacent third molar
Survival analysis was also conducted of a subset of subjects with an absent third molar on one side and either an erupted or unerupted third molar on the opposite side. Results (see Appendix Table 3) were remarkably similar to the overall dataset. The survival plot for this subset is also presented (see Appendix Fig. 1).
A survival plot for loss of adjacent second molars by third molar status is shown in Appendix Figure 2. Again, second molars adjacent to soft tissue impacted third molars had the greatest risk of eventual tooth loss, while second molars adjacent to bony impacted third molars appeared to have a slightly greater risk of eventual tooth loss than that of second molars adjacent to erupted third molars. No second molars adjacent to absent third molars were lost.
Discussion
Data remain limited regarding the longer term effects of unerupted third molars on adjacent teeth. However, the existing evidence indicates that retention of third molars is associated with increased risk of second molar disease. Marciani (2012) recently reviewed published prospective studies with samples of at least 50 subjects and a follow-up longer than 1 year. He found that retained asymptomatic third molars posed a risk for second molar incident pathology. Elter et al. (2004), using data from 5,831 young adults (18-34 years old) in the U.S. Third National Health and Nutrition Examination Survey, found that presence of a visible third molar was associated with twice the odds of periodontal probing depth of 5 mm or more on the adjacent second molar. Similarly, in 52- to 74-year-olds in the Dental Atherosclerosis Risk in Communities Study, the presence of third molars was associated with a 50% increased odds of periodontal probing depth of 5 mm or more on adjacent second molars (Elter et al., 2005). These data on periodontal pathology related to retained third molars are the most extensive to date. Interestingly, these findings are also congruent with the classic observations of Ash et al. (1962).
Our study provides additional evidence for the association while also providing novel longitudinal data, with over 20+ years of follow-up, comparing second molar risk to situations where third molars are absent or unerupted. We found that both the prevalence and the incidence of periodontal pathology of second molars varied significantly depending on whether adjacent third molars were absent, erupted, soft tissue impacted, or bony impacted. Unlike many previous studies, ours had radiographs available on all subjects with which to categorize third molar status and measure second molar alveolar bone loss. We found that the prevalence of periodontal pathology of the distal of second molars adjacent to soft tissue impacted third molars was significantly greater than that for second molars adjacent to any other category of third molars, whether periodontal pathology was defined as distal probing depth > 4 mm or distal bone loss ≥ 20%. In addition, risks over time of incident probing depth > 4 mm and incident distal bone loss ≥ 20% on second molars adjacent to soft tissue impacted third molars were significantly greater than they were for second molars adjacent to absent third molars. However, in regard to caries risk, we found that only second molars adjacent to erupted third molars were at significantly increased risk of distal caries. Second molars adjacent to unerupted third molars did not differ significantly from those adjacent to absent third molars in regard to caries risk.
To our knowledge, this is the first study to apply a multivariate approach with generalized estimating equations and survival analysis to model risk of second molar pathology based on the status of adjacent third molars, including their absence. The availability of comprehensive radiographs on all subjects, both for assessment of third molar status and for determination of second molar outcomes, is another advantage. Furthermore, the length of our observation period surpasses that of most previous studies. However, our work has several important limitations. All subjects are male and drawn from a single geographic area, and almost all are white. These factors greatly limited the generalizability of the findings. All subjects were also self-selected volunteers in a long-term study of aging and health. That they enrolled in the study and returned for follow-ups likely makes them more health aware than their age-matched peers in the community and likely to practice better health behaviors. However, if that were true, then any bias in our results would be toward underestimating the prevalence and incidence of second molar pathology as compared to that of other community-dwelling adult men, all else being equal. Last, the subjects’ third molar status at baseline was not randomized. That is, the men entered the study in adulthood, with many already having had one or more third molars removed at an earlier point in their lives. We were not able to determine whether, nor why, subjects may have had any third molars removed before their study entry.
Despite our accumulating knowledge regarding clinical outcomes of retained third molars, there remains a need for additional evidence to better inform clinical decision making regarding management of unerupted third molars. For example, if optimizing second molar health is a primary desired outcome, then our data suggest that absence of adjacent third molars is the best option. However, the prophylactic removal of asymptomatic third molars is neither cost-free nor risk-free. Earlier, Flick (1999) had estimated that over $2 billion per year is spent on removal of unerupted teeth in the United States, with the majority involving third molars. Song et al. (1997) conducted a systematic review and concluded that insufficient evidence existed supporting removal of asymptomatic impacted third molars. In 2000, the U.K. National Institute for Health and Care Excellence (2000) reviewed the evidence and recommended that the “practice of prophylactic removal of pathology-free impacted third molars should be discontinued” by the National Health Service due to lack of reliable evidence of a health benefit. A Cochrane systematic review (Mettes et al., 2005) assessed prophylactic removal of unerupted third molars and similarly concluded that there was insufficient evidence to support removal of asymptomatic unerupted third molars. In 2008, the American Public Health Association (2008) issued an evidence-based policy statement opposing prophylactic removal of asymptomatic third molars. While the comprehensiveness of the evidence-based review underlying the association’s policy has been questioned by some (Dodson, 2010), it should be noted that leading proponents of the policy have also emphasized the need for further research to establish an evidence-based approach to clinical decision making regarding asymptomatic third molars (Friedman, 2007; Friedman and Presson, 2010).
In contrast, the American Association of Oral and Maxillofacial Surgeons (2013) has published indications for removal of asymptomatic third molars, based in part on clinical studies supported by the association that found localized progression of periodontal probing depth, among other findings (Blakey et al., 2006; Blakey et al., 2007; Blakey et al., 2009; Garaas et al., 2012). The association has also recommended that long-term studies be conducted with well-defined inclusion and exclusion criteria and clear endpoints. To this end, it has sponsored a series of longitudinal studies known as the Third Molar Clinical Trials to better define prevalence and incidence of third molar and adjacent second molar pathology (White, 2007). The 2010 Third Molar Multidisciplinary Conference convened by the association (Dodson et al., 2012) is another example of the continuing interest in building the necessary evidence base to guide clinical decision making.
Supplementary Material
Footnotes
The Veterans Affairs Dental Longitudinal Study and Normative Aging Study are components of the Massachusetts Veterans Epidemiology Research and Information Center, supported by the U.S. Department of Veterans Affairs Cooperative Studies Program. Dr. Garcia was a recipient of a Veterans Affairs Career Development Award in Health Services Research from the Veterans Affairs Health Services Research and Development Service. This work was also supported by the National Institute of Dental and Craniofacial Research (K24 DE000419 and R01 DE019656). Views expressed in this article are solely those of the authors and do not necessarily represent the views of the U.S. Department of Veterans Affairs.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
A supplemental appendix to this article is published electronically only at http://jdr.sagepub.com/supplemental.
References
- American Association of Oral and Maxillofacial Surgeons (2013). The Management of Impacted Third Molar Teeth. URL accessed on 9/25/2013 at: http://www.aaoms.org/docs/practice_mgmt/condition_statements/impacted_third_molars.pdf.
- American Public Health Association (2008). Policy Statement No. 20085: Opposition to Prophylactic Removal of Third Molars (Wisdom Teeth). URL accessed on 9/25/2013 at: http://www.apha.org/advocacy/policy/policysearch/default.htm?id=1371.
- Ash MM, Costich ER, Hayward JR. (1962). A study of periodontal hazards of third molars. J Periodontal 33:209-219. [Google Scholar]
- Blakey GH, Jacks MT, Offenbacher S, Nance PE, Phillips C, Haug RH, et al. (2006). Progression of periodontal disease in the second/third molar region in subjects with asymptomatic third molars. J Oral Maxillofac Surg 64:189-193. [DOI] [PubMed] [Google Scholar]
- Blakey GH, Hull DJ, Haug RH, Offenbacher S, Phillips C, White RP., Jr (2007). Changes in third molar and nonthird molar periodontal pathology over time. J Oral Maxillofac Surg 65:1577-1583. [DOI] [PubMed] [Google Scholar]
- Blakey GH, Golden BA, White RP, Jr, Offenbacher S, Phillips C, Haug RH. (2009). Changes over time in the periodontal status of young adults with no third molar periodontal pathology at enrollment. J Oral Maxillofac Surg 67:2425-2430. [DOI] [PubMed] [Google Scholar]
- Dodson TB. (2010). Wisdom tooth extraction: Goals gone wild. Dental Abstracts 55:4-5. [Google Scholar]
- Dodson TB, Rafetto LK, Nelson WJ. (2012). Introduction to Proceedings of the Third Molar Multidisciplinary Conference Washington, DC, October 19, 2010. J Oral Maxillofac Surg 70(9):S2-S3. [DOI] [PubMed] [Google Scholar]
- Elter JR, Cuomo CH, Offenbacher S, White RP., Jr (2004). Third molars associated with periodontal pathology in the Third National Health and Nutrition Examination Survey. J Oral Maxillofac Surg 62:440-445. [DOI] [PubMed] [Google Scholar]
- Elter JR, Offenbacher S, White RP, Beck JD. (2005). Third molars associated with periodontal pathology in older Americans. J Oral Maxillofac Surg 63:179-184. [DOI] [PubMed] [Google Scholar]
- Flick WG. (1999). The third molar controversy: framing the controversy as a public health policy issue. J Oral Maxillofac Surg 57:438-444. [DOI] [PubMed] [Google Scholar]
- Friedman JW. (2007). The prophylactic extraction of third molars: a public health hazard. Am J Public Health 97:1554-1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman JW, Presson SM. (2010). Wisdom tooth extraction in perspective. Dental Abstracts 55:228-229. [Google Scholar]
- Garaas RN, Fisher EL, Wilson GH, Phillips C, Shugars DA, Blakey GH, et al. (2012). Prevalence of third molars with caries experience or periodontal pathology in young adults. J Oral Maxillofac Surg 70:507-513. [DOI] [PubMed] [Google Scholar]
- Kapur KK, Glass RL, Loftus ER, Alman JE, Feller RP. (1972). The Veterans Administration longitudinal study of oral health and disease. Int J Aging Human Develop 3:125-137. [Google Scholar]
- Marciani RD. (2012). Is there pathology associated with asymptomatic third molars? J Oral Maxillofac Surg 70(suppl 1):15-19. [DOI] [PubMed] [Google Scholar]
- Mettes TG, Nienhuijs ME, van der Sanden WJ, Verdonschot EH, Plasschaert AJ. (2005). Interventions for treating asymptomatic impacted wisdom teeth in adolescents and adults. Cochrane Database Syst Rev 2:CD003879. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (2000). Guidance on the Extraction of Wisdom Teeth: Technology Appraisals Guidance No 1. URL accessed on 9/25/2013 at: http://publications.nice.org.uk/guidance-on-the-extraction-of-wisdom-teeth-ta1
- Schei O, Waerhaug J, Lovdal A, Arno A. (1959). Alveolar bone loss as related to oral hygiene and age. J Periodontol 30:7-16 [Google Scholar]
- Song F, Landes DP, Glenny AM, Sheldon TA. (1997). Prophylactic removal of impacted third molars: an assessment of published reviews. Br Dent J 182:339-346. [DOI] [PubMed] [Google Scholar]
- White RP., Jr (2007). Progress report on Third Molar Clinical Trials. J Oral Maxillofac Surg 65:377-383. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


