Abstract
The treatment of chronic shoulder instability with poor quality of the anterior capsulolabral tissue is still controversial. In these cases the Latarjet procedure is certainly more effective in preventing recurrence than an arthroscopic capsular repair. However, several studies have reported a variety of severe complications related to the Latarjet procedure because of the use of bone augmentation and hardware implantation; moreover, the arthroscopic version of the Latarjet procedure is technically difficult and potentially dangerous because of the proximity of neurovascular structures. The aim of this report is to describe an innovative arthroscopic technique consisting of an augmentation of the anterior capsulolabral tissue using the articular portion of the subscapularis tendon and knotless suture anchors paired with high-strength tape for its fixation to the anterior glenoid edge. In the absence of severe bone deficiency of the anterior glenoid edge, this procedure can minimize arthroscopic technique failures, restoring the anterior capsulolabral wall without any significant reduction of shoulder functionality.
Arthroscopic capsulolabral complex repair has become extremely popular as a method for treatment of shoulder instability, although its failure rate has been relatively high.1-4 Several authors have suggested that the ideal candidate for an arthroscopic repair is a patient with a Bankart lesion and no capsular laxity or glenohumeral bone defects.5-10
Open surgical procedures have been successful in preventing recurrent instability; however, complications related to the use of hardware and late degenerative joint changes have been widely reported in the literature.11-15
The absence or deficiency of the ligament-labrum complex is a common arthroscopic finding in patients with recurrent shoulder dislocation, and the indication for arthroscopic repair in case of capsular deficiency, even if not associated with severe glenohumeral bone defects, is still debated.14-19
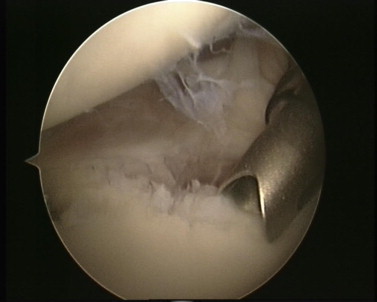
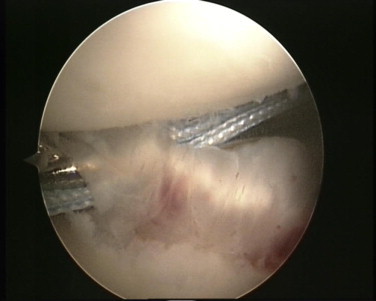
Mead et al.20 were the first authors to point out that the effectiveness of the Bristow procedure was due to the conjoined tendon preventing the subscapularis muscle from displacing upward in the elevation of the arm. In patients with capsular deficiency, the position of abduction and external rotation of the shoulder and the concomitant subscapularis tendon displacing upward allow anterior dislocation of the humeral head just below it.21-23 In 1972, furthermore, Symeonides24 showed, in a human cadaveric study, a significant elongation of the subscapularis tendon related to shoulder instability (Fig 1) and showed that a simple capsular repair is not strong enough to prevent recurrent dislocation (Fig 2). More recently, Boileau et al.25,26 described the “sling effect” concept of the conjoined tendon on the subscapularis tendon and developed an arthroscopic technique combining the arthroscopic Bankart repair with tenodesis of the coraco-biceps tendon to treat shoulder instability in patients with a deficient or stretched anteroinferior capsule.
Fig 1.
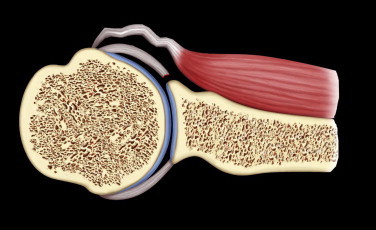
Subscapularis tendon elongation in chronic anterior shoulder instability.
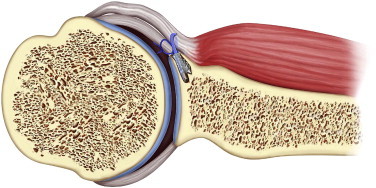
Fig 2.
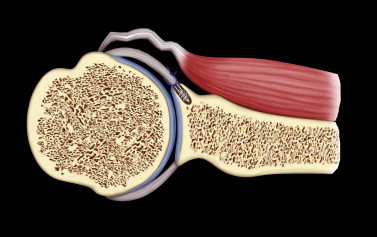
Subscapularis tendon elongation is not corrected by capsulolabral repair.
Nourissat et al.27 and Lafosse et al.28,29 described a mini-open arthroscopically assisted procedure and the arthroscopic Latarjet procedure, respectively. Both procedures are indicated in cases of bony insufficiency and recurrence. The bone block is effective in both procedures, although shoulder stabilization is mainly due to the effect of coraco-biceps transfer. Moreover, the authors emphasized that both procedures are technically difficult and potentially dangerous because of the proximity of the musculocutaneous nerve and axillary vessels.
In 1986 Johnson30 proposed an arthroscopic technique to address chronic recurrent shoulder dislocations with “virtually nonexistent gleno-humeral ligaments” that involved the articular portion of the subscapularis tendon. Despite the numerous advantages of the arthroscopic approach, Johnson's technique was criticized because of potential complications related to the placement of a metal staple for tendon fixation adjacent to the level of the shoulder joint.
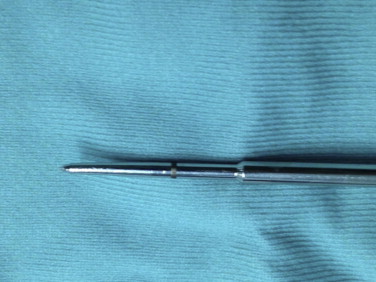
According to the technique proposed by Johnson,30 we considered using an assembling kit consisting of a tape commonly used for cuff repair and a 3.5-mm knotless polyetheretherketone (PEEK) anchor (Fig 3) to perform a capsulolabral complex augmentation in the absence of the ligament-labrum complex or in cases in which the ligament-labrum complex is deficient using the articular portion of the subscapularis tendon (Fig 4).
Fig 3.

A 3.5-mm nonabsorbable knotless PEEK suture anchor loaded with multi-strand tape.
Fig 4.
Capsulolabral complex augmentation in the absence of the ligament-labrum complex or with deficiency of the ligament-labrum complex using the articular portion of the subscapularis tendon.
Technique
Preoperative Planning
A preoperative assessment of bone loss was obtained on a 3-dimensional computed tomography scan with multiplanar reconstructions of the glenoid neck and a digital subtraction of the humeral head. The Pico surface area method31 was used to quantify the percentage of inferior glenoid deficiency compared with the contralateral shoulder.
We consider glenoid bone loss exceeding 25% of the inferior glenoid diameter a contraindication to the current procedure.
Surgical Technique
The procedure is performed with the patient under interscalene block in a lateral decubitus position; the arm is kept in 40° of abduction and 15° of forward flexion with a balanced suspension of 5 to 10 lb (Star Sleeve Traction System; Arthrex, Naples, FL). Arthroscopy is performed with a 30° arthroscope and an arthroscopic pump maintaining pressure at 60 mm Hg.
Standard anterior and posterior portals are used. An accessory anterior portal is first localized with a spinal needle and then set up into the glenohumeral joint just over the superior border of the subscapularis tendon to obtain a 45° angle of approach and easily use suture-passing devices through the tendon tissue.
Large 6-mm and 4.5-mm threaded cannulas are used for inferior and superior anterior portals. The anterior and posterior glenohumeral joint structures are inspected to assess any anteroinferior labral detachment, SLAP lesions, capsular deficiency (Fig 5), and anterior glenoid defects; to assess for the presence of Hill-Sachs lesions; and to verify the anterior displacement of the humeral head with respect to the glenoid cavity. Arthroscopic tools from both anterior portals are used alternatively to prepare the glenoid neck, repair the labral tear, and augment the capsular deficiency with subscapularis tendon.
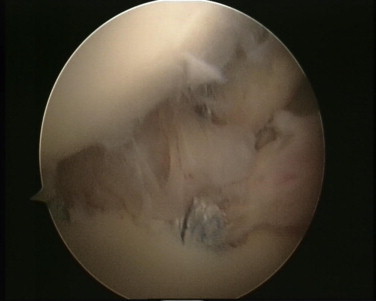
Fig 5.
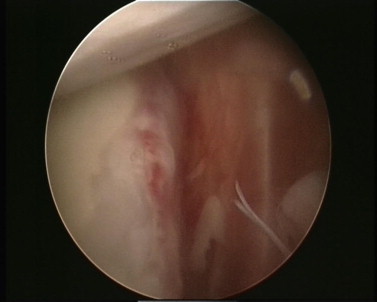
Large anterior pouch with poor capsulolabral tissue quality and absence of the labrum.
Suture anchor bone holes are placed on the anterior glenoid edge at the 3- or 5-o'clock position in a right shoulder or the 7- or 9-o'clock position in a left shoulder, by first localizing the proper angle directly with a drill guide (Fig 6). An additional anchor bone hole is placed at the 1-o'clock position in a right shoulder or the 11-o'clock position in a left shoulder to repair a coexisting detachment of the biceps long head origin.
Fig 6.
Bone hole drilling at the 9-o'clock position for subscapularis tendon fixation (left shoulder).
A lower capsular repair (Fig 7) is performed with 3.5-mm nonabsorbable knotless PEEK suture anchors (PushLock; Arthrex) loaded with multi-strand sutures (FiberWire; Arthrex). The middle portion of the subscapularis tendon, which is necessary to augment the capsulolabral deficiency, is penetrated with a suture-passing device (Fig 8) loaded with an Ultrabraid suture tape (FiberTape; Arthrex).
Fig 7.
Anteroinferior capsulorrhaphy (left shoulder).
Fig 8.

A suture-passing device loaded with multi-strand tape is used to perforate the articular portion of the subscapularis tendon from the lower cannula.
The articular portion of the subscapularis tendon and, if present, the glenoid labrum are perforated from the lower cannula with a penetrator punch so that the free ends of the tape remain accessible through the same lower cannula. Then, 1 of the free ends is carried out from the upper cannula with a suture retriever (Fig 9). In the next step the same suture tape end is passed again in the lower cannula so that the 2 ends are astride the perforated tissues and come out again from the same lower cannula. A punch device is extremely useful to assess the anchor bone hole direction and depth (Fig 10).
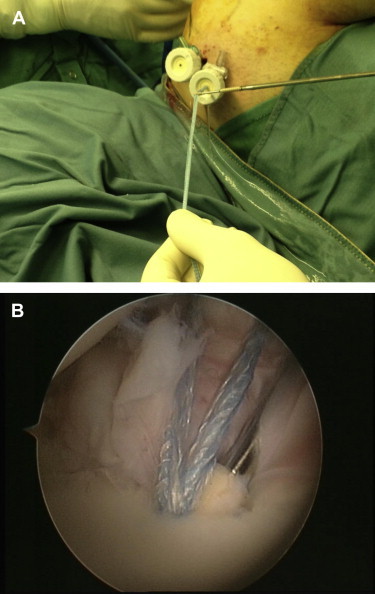
Fig 9.
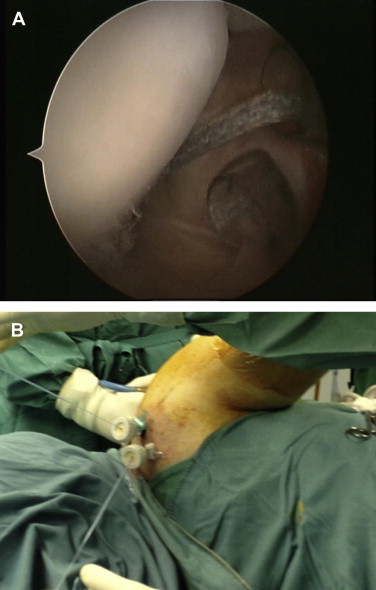
(A) One of the free ends of the tape is carried out from the upper cannula with a suture retriever. (B) External point of view of procedure.
Fig 10.
The anchor bone hole direction and depth are assessed with a punch device.
At this point, both free ends of the tape are passed through the anchor's eyelet and the anchor is pushed along the tape toward the bone hole (Fig 11). While one is inserting the anchor into the bone, tape sutures are kept in traction in parallel position and care is taken to keep the patient's arm in neutral rotation to avoid excessive tensioning on the labrum repair when the anchor is placed and the tape is locked (Fig 12).
Fig 11.
(A) A suture anchor is pushed along the tape through the lower cannula (external point of view). (B) Insertion of suture anchor's eyelet into bone hole.
Fig 12.
Advancement of the subscapularis tendon to the glenoid neck with restoration of the anterior wall.
The repair, including complete closure of the anterior pouch and centering of the humeral head in the glenoid cavity, is assessed by arthroscopic examination from the anterosuperior portal (Fig 13, Tables 1 and 2, Video 1).
Fig 13.
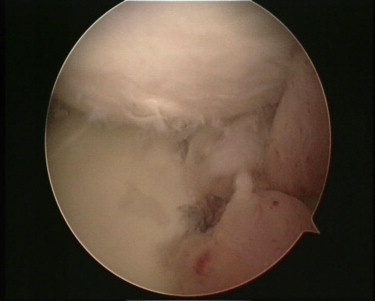
Anterosuperior view: complete closure of anterior pouch and centering of humeral head in glenoid cavity.
Table 1.
Steps of Surgical Procedure
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Table 2.
Augmentation of Anterior Capsulolabral Complex With Subscapularis Tendon
Indications
|
Contraindications
|
Tips
|
Pearls
|
Pitfalls
|
Key points
|
Postoperative Protocol
After surgical repair, the shoulder is immobilized in a sling with the arm in adduction for 4 weeks. In the fourth week, the sling is removed and pendulum exercises and active-assisted range of motion are instituted. At 7 weeks, resistive band strengthening activity for the shoulder is allowed. Return to contact sports is allowed at 5 months.
Discussion
Arthroscopic capsulolabral complex repair is generally considered the standard of excellence in the treatment of anterior shoulder instability.1-3 This is mainly because of the extremely advantageous cosmetic result of arthroscopic treatment and because it is more appreciated by patients compared with open surgery.1,9
The main criticism of arthroscopic capsulolabral complex repair concerns the significant recurrence rate of shoulder dislocation compared with open techniques.2-4 Furthermore, bone defects and poor soft-tissue quality have been clearly identified as important factors associated with recurrence after simple arthroscopic repair.6,18
Traditional open surgical procedures are commonly considered effective to provide the opportunity to manage shoulder instability in patients with either bone defects or capsular deficiency, yielding a long-term low recurrence rate.5 On the contrary, a variety of complications related to open repair procedures have been reported, including nerve injuries, vascular injuries, soft-tissue injuries, and fixation failures.11-15 As is well known, screws and staples can produce complications that require reoperation and can cause a permanent loss of joint motion and degenerative changes on the articular surface of both the humeral head and the glenoid.11
Despite a relatively high number of anatomic and biomechanical studies to assess the subscapularis tendon function in balancing force couples in the glenohumeral joint, its important role in preventing anterior shoulder dislocation has received poor attention.21-23
Symeonides24 emphasized that subscapularis tendon laxity is a determinant factor, like detachment of the labrum or bone defects, in shoulder dislocation recurrence. Moreover, the author has clarified that a simple capsular repair is not effective to address subscapularis tendon laxity.
Boileau et al.25,26 highlighted that abduction and external rotation movements of the shoulder cause a physiological upward displacement of the subscapularis tendon. Such movements have no effect under normal conditions, but when a lesion of the capsulolabral complex occurs, these movements promote an anterior dislocation of the humeral head just below the lower edge of the subscapularis tendon.
Mead et al.20 pointed out that the effectiveness of the traditional Bristow-Latarjet procedure is because of the transfer of the conjoined tendon preventing the subscapularis muscle from displacing upward in elevation of the arm. As further evidence of the conjoined tendon's action in the Latarjet procedure, some studies have reported progressive resorption of the bone plug and, consequently, a lack of bone block action.32,33 This was confirmed in a recent study by Griesser et al.,14 who reported, in a series of 262 complications related to the coracoid, that the majority of them did not require reoperation.
In 1986 Johnson30 proposed a technique to perform an arthroscopic stabilization by using the subscapularis tendon to augment a poor-quality anterior capsulolabral complex. This technique, in our opinion, addresses all the factors related to recurrent shoulder instability. It allows the surgeon to overcome problems related both to poor-quality capsulolabral tissue and to the laxity of the subscapularis tendon. In reality, criticism of the procedure proposed by Johnson was mainly dictated by the articular use of metal staples, but his second-look arthroscopies have shown restoration of the anterior capsulolabral wall.
On the basis of such evidence, we considered performing the capsulolabral complex augmentation using a new assembling kit made of a 3.5-mm knotless PEEK anchor and a tape that keeps the subscapularis tendon, without damaging it, bonded to the edge of the glenoid neck while improving the soft-tissue healing process. In our opinion, such a procedure minimizes arthroscopic failures related to degenerative changes of the capsulolabral complex that always occur after the third or fourth episode of shoulder dislocation.18
Basically, the subscapularis tendon advancement to the anterior glenoid edge leads to an effective tensioning of the tendon and reduces its slipping upward; thus it can act as an anterior stabilizer of the humeral head and prevent recurrence. Furthermore, the subscapularis tendon advancement is extremely useful to augment the anterior capsulolabral complex even in the presence of mild anterior glenoid bone deficiency. In our experience this step is best achieved by using an assembling kit consisting of a tape and a knotless anchor basically for 2 reasons: first, it can be extremely difficult to tie a knot with a regular anchor to re-tension the subscapularis tendon, and second, a wire-shaped suture, currently used for capsular repair, can damage the tendon.
We always recommend controlling the direction of the bone hole with a punch to avoid anchor divergence; moreover, it should be ensured that the eyelet has entered the hole in the correct direction before impacting. To our knowledge, there are no previous studies that describe the use of the subscapularis tendon paired with devices designed for cuff repair in the treatment of chronic shoulder instability.
Although long-term follow-up clinical trials are needed, we believe that the described arthroscopic procedure is safe, is easily reproducible, does not require a long learning curve, and allows restoration of joint stability. We therefore recommend its use in all cases of chronic shoulder instability without severe glenoid bone loss in which the Latarjet procedure or its arthroscopic version is currently indicated.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Subscapularis tendon elongation after anterior shoulder recurrent dislocation. Surgical steps of the arthroscopic subscapularis tendon augmentation that can restore the anterior wall of the shoulder in patients with capsulolabral deficiency.
References
- 1.Cole J.B., L'Insalata J., Irrgang J., Warner J.P. Comparison of arthroscopic and open anterior shoulder stabilization. J Bone Joint Surg Am. 2000;82:1108–1114. doi: 10.2106/00004623-200008000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Arciero R.A., Taylor D.C., Snyder R.J., Uhorchak J.M. Arthroscopic bioabsorbable tack stabilization of initial anterior shoulder dislocations: A preliminary report. Arthroscopy. 1995;11:410–417. doi: 10.1016/0749-8063(95)90192-2. [DOI] [PubMed] [Google Scholar]
- 3.Bacilla P., Field L.D., Savoie F.H., III Arthroscopic Bankart repair in a high demand patient population. Arthroscopy. 1997;13:51–60. doi: 10.1016/s0749-8063(97)90209-7. [DOI] [PubMed] [Google Scholar]
- 4.Burger R.S., Shengel D., Bonatus T., Lewis J. Arthroscopic staple capsulorrhaphy for recurrent shoulder instability. Orthop Trans. 1990;14:596–597. [Google Scholar]
- 5.Sisto D.J., Cook D.L. Intraoperative decision making in the treatment of shoulder instability. Arthroscopy. 1998;14:389–394. doi: 10.1016/s0749-8063(98)70006-4. [DOI] [PubMed] [Google Scholar]
- 6.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs-lesion. Arthroscopy. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 7.Piasecki D.P., Verma N.N., Romeo A.A., Levine W.N., Bach B.R., Provencher M.T. Glenoid bone deficiency in recurrent anterior shoulder instability: Diagnosis and management. J Am Acad Orthop Surg. 2009;17:482–493. doi: 10.5435/00124635-200908000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Hawkins R.B. Arthroscopic stapling repair for shoulder instability: A retrospective study of 50 cases. Arthroscopy. 1989;5:122–128. doi: 10.1016/0749-8063(89)90007-8. [DOI] [PubMed] [Google Scholar]
- 9.Benedetto K.P., Glozer W. Arthroscopic Bankart procedure by suture technique: Indications, technique, and results. Arthroscopy. 1992;8:111–115. doi: 10.1016/0749-8063(92)90144-z. [DOI] [PubMed] [Google Scholar]
- 10.Coughlin L., Rubinovich M., Johansson J., White R., Greenspoon J. Arthroscopic staple capsulorrhaphy for anterior shoulder instability. Am J Sport Med. 1992;20:253–256. doi: 10.1177/036354659202000303. [DOI] [PubMed] [Google Scholar]
- 11.Hawkins R.J., Angelo R.L. Glenohumeral osteoarthrosis. A late complication of the Putti-Platt repair. J Bone Joint Surg Am. 1990;72:1193–1197. [PubMed] [Google Scholar]
- 12.Zuckerman J.D., Matsen F.A. Complications about the glenohumeral joint related to the use of screws and staples. J Bone Joint Surg Am. 1984;66:175–180. [PubMed] [Google Scholar]
- 13.Shah A.A., Butler R.B., Romanowski J., Karadagli D., Warner J.J. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am. 2012;94:495–501. doi: 10.2106/JBJS.J.01830. [DOI] [PubMed] [Google Scholar]
- 14.Griesser M.J., Harris J.D., McCoy B.W. Complications and re-operations after Bristow-Latarjet shoulder stabilization: A systematic review. J Shoulder Elbow Surg. 2013;22:286–292. doi: 10.1016/j.jse.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 15.Griesser M.J., Harris J.D., McCoy B.W. Glenoid fracture after Bristow-Latarjet shoulder stabilization: A case report and review of the literature. J Shoulder Elbow Surg. 2013;22:e17–e20. doi: 10.1016/j.jse.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Denard P.J., Narbona P., Lädermann A., Burkhart S.S. Augmentation for capsulolabral deficiency using a split subscapularis tendon flap. Arthroscopy. 2011;27:1135–1141. doi: 10.1016/j.arthro.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 17.Hayashida K., Yoneda M., Nakagawa S., Okamura K., Fukushima S. Arthroscopic Bankart suture repair for traumatic anterior shoulder instability: Analysis of the causes of a recurrence. Arthroscopy. 1998;14:295–301. doi: 10.1016/s0749-8063(98)70146-x. [DOI] [PubMed] [Google Scholar]
- 18.Habermeyer P., Gleyze P., Rickert M. Evolution of lesions of the labrum-ligament complex in posttraumatic anterior shoulder instability: A prospective study. J Shoulder Elbow Surg. 1999;8:66–74. doi: 10.1016/s1058-2746(99)90058-7. [DOI] [PubMed] [Google Scholar]
- 19.Burkhart S.S., De Beer J.F., Barth J.R. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy. 2007;23:1033–1041. doi: 10.1016/j.arthro.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 20.Mead NC, Sweeney HJ. Bristow procedure. Spectator letter. Spectator Society. July 9, 1964. In: Rowe CR, ed. The Shoulder. Chapter 7. Philadelphia: Churchill Livingstone;1998:222-223.
- 21.Itoi E., Newman S.R., Kuechle D.K., Morrey B.F., An K.N. Dynamic anterior stabilisers of the shoulder with the arm in abduction. J Bone Joint Surg Br. 1994;76:834–836. [PubMed] [Google Scholar]
- 22.Otis J.C., Jang C.C., Wickiewicz T.L., Peterson M.G., Warren R.F., Santner T.J. Changes in the moment arms of the rotator cuff and deltoid muscles with abduction and rotation. J Bone Joint Surg Am. 1994;76:667–676. doi: 10.2106/00004623-199405000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Perry J. In: Rowe CR, ed. The shoulder. Chapter 2. Philadelphia: Churchill Livingstone;1988:23-27.
- 24.Symeonides P.P. The subscapularis muscle in the pathogenesis of recurrent anterior dislocation of the shoulder. J Bone Joint Surg Br. 1972;54:476–483. [PubMed] [Google Scholar]
- 25.Boileau P., Bicknell R.T., El Fegoun A.B., Chuinard C. Arthroscopic Bristow procedure for anterior instability in shoulder with a stretched or deficient capsule: The “belt-and suspenders” operative technique and preliminary results. Arthroscopy. 2007;23:593–601. doi: 10.1016/j.arthro.2007.03.096. [DOI] [PubMed] [Google Scholar]
- 26.Boileau P., Mercier N., Roussanne Y., Thelù C.E., Old J. Arthroscopic Bankart-Bristow-Latarjet procedure: The development and early results of a safe and reproducible technique. Arthroscopy. 2010;26:1434–1450. doi: 10.1016/j.arthro.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 27.Nourissat G., Nedellec G., O'Sullivan N.A. Mini-open arthroscopically assisted Bristow-Latarjet procedure for the treatment of patients with anterior shoulder instability: A cadaver study. Arthroscopy. 2006;22:1113–1118. doi: 10.1016/j.arthro.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 28.Lafosse L, Lejeune E, Bouchard A, Kakuda C, Gobezie R, Kochhar T. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy 2007;23:1242.e1-1242.e5. Available online at www.arthroscopyjournal.org. [DOI] [PubMed]
- 29.Lafosse L., Boyle S. Arthroscopic Latarjet procedure. J Shoulder Elbow Surg. 2010;19:2–12. doi: 10.1016/j.jse.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 30.Johnson LL. Arthroscopic surgery: Principle and practice. Chapter 15. St. Louis: Mosby; 1986:1420-1424.
- 31.Baudi P., Righi P., Bolognesi D. How to identify and calculate glenoid bone deficit. Chir Organi Mov. 2005;90:145–152. [PubMed] [Google Scholar]
- 32.Hovelius L., Sandström B., Olofsson A., Svensson O., Rahme H. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): Long-term follow-up in 319 shoulder. J Shoulder Elbow Surg. 2012;21:647–660. doi: 10.1016/j.jse.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 33.Di Giacomo G., Costantini A., De Gasperis N. Coracoid graft osteolysis after the Latarjet procedure for anteroinferior shoulder instability: A computed tomography scan study of twenty-six patients. J Shoulder Elbow Surg. 2011;20:989–995. doi: 10.1016/j.jse.2010.11.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Subscapularis tendon elongation after anterior shoulder recurrent dislocation. Surgical steps of the arthroscopic subscapularis tendon augmentation that can restore the anterior wall of the shoulder in patients with capsulolabral deficiency.


