Abstract
Over the past 30 years, many patients have benefited from arthroscopically assisted meniscus repair surgery and its ability to preserve a healthy knee. Although techniques have evolved, the basic premise of central-to-peripheral needle penetration across the tear with fixation into the capsular region immediately peripheral to the meniscus has remained. Suture repair techniques that involve encircling the tear have been discussed but have remained largely impractical because of the anatomic constraints of the arthroscopic knee. A suture-passing technology designed to function within these constraints was recently made available from Ceterix Orthopaedics (Menlo Park, CA). It allows surgeons to arthroscopically place circumferential sutures around meniscus tears to provide uniform, anatomic compression of the tear edges through an all-inside technique. This stitch is likely to improve healing rates and safety, as well as to enable repair of tears that were previously considered difficult or impossible to sew. The purposes of this note and accompanying video are to show the feasibility of placing all-inside circumferential compression stitches to treat tears of the knee meniscus and to discuss the potential benefits of such techniques.
It is well established in the orthopaedic literature that meniscus repair should be performed whenever possible to prevent long-term degenerative changes in the knee.1-10 The amount of meniscus tissue removed at the time of partial meniscectomy has been shown to be directly proportional to the extent of knee degeneration.3,11 At the same time, meta-analyses and systematic reviews of meniscus repair outcomes show high failure rates compared with other orthopaedic procedures, in the range of 19% to 29% and many tear patterns remain difficult to easily and effectively repair.12-18 There is also an inherent risk of neurovascular injury.19-23 Thus there is room for innovation to improve healing rates, enable repair of nonvertical tear patterns, and decrease or eliminate risk to neurovascular structures.
Circumferential stitching for meniscus repair has been shown in the laboratory to have the highest load to failure of all repair patterns.24 It is likely to improve healing rates and safety by uniformly compressing the superior, central, and inferior tear surfaces without penetrating toward neurovascular structures (Fig 1). Until recently, however, this pattern has been considered impractical because of the impossibility to atraumatically sew in vivo. This technical note and accompanying video discuss and show the feasibility of arthroscopic all-inside circumferential suture repair for vertical, oblique, horizontal, radial, and root tears, as well as those adjacent to the popliteal hiatus.
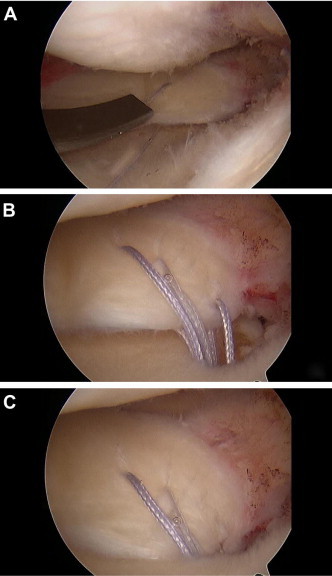
Fig 1.
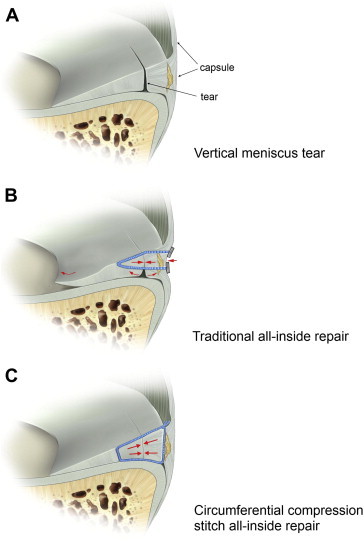
Peripheral vertical tear before repair (A), after traditional all-inside repair (B), and after circumferential compression stitch all-inside repair (C). Note that with the circumferential compression stitch, the entire tear surface is uniformly compressed from top to bottom and that the capsule remains untethered.
Surgical Technique
The patient is placed in any typical knee arthroscopy position per surgeon preference, and portals are established. The anterolateral portal is typically created by use of the inferior pole of the patella and the lateral border of the patellar tendon as anatomic landmarks, and the anteromedial portal is created under direct arthroscopic visualization of the desired repair compartment to ensure that the angle of approach is optimal for access to the torn meniscus. A spinal needle is helpful for establishing the best approach angle before one incises the working portal, and a hemostat can be used to open and optimize the portal. The camera can be moved into the anteromedial portal if the anterolateral portal gives a better approach vector to the torn region. This switch is typically useful when one is repairing the body of the medial meniscus or the posterior horn of the lateral meniscus. In some instances the best approach angle for these regions requires the anterolateral working portal to be somewhat proximal to the initially created viewing portal.
The meniscus suture-passing device from Ceterix Orthopaedics (Menlo Park, CA) enables placement of the circumferential compression stitch by use of a low-profile curved upper jaw, as well as a protractible-retractable lower jaw, to allow reversible encasement of the meniscus without injury to surrounding structures. The lower jaw of the device is loaded with any No. 2-0 braided composite suture. To load the suture, the lower jaw is protracted into view by squeezing the black handle trigger (Fig 2). One end of the suture can then be loaded into the lower jaw by pulling it into the slot located at the distal aspect of the jaw, as shown in Video 1. The lower jaw is then retracted back into the shaft by a thumb trigger so that the device can be easily and atraumatically inserted into the depths of the desired compartment through the working portal. The upper jaw can be flexed forward by the orange trigger so that it is rigidly in line with the shaft of the device to allow streamlined insertion, and it can be gradually extended to follow the contour of the femoral condyle as the device is inserted into the depths of the compartment, as shown best in Video 1. Once beyond the condyle, the upper jaw rests safely below the femoral condyle and above the superior surface of the meniscus. The lower jaw can then be protracted forward until it is underneath the meniscus to effectively encase the superior and inferior surfaces of the meniscus between the jaws at the repair region (Fig 3A-3C).
Fig 2.

Profile view of Ceterix meniscus suture passer. The orange trigger controls the upper jaw; when compressed, the upper jaw flexes forward so that it can be brought in line with the shaft during insertion into the knee. The black trigger has dual functionality: lower jaw protraction and needle drive. When compressed the first time, the lower jaw protracts forward, and when compressed a second time, the needle passes the suture from the lower jaw to the upper jaw, where it is self retained. The lower jaw can then be retracted back into the shaft by use of downward pressure on the thumb trigger so that the device can be atraumatically removed. The device is designed for use with 1 hand. The surgeon can place multiple stitches with 1 disposable device.
Fig 3.
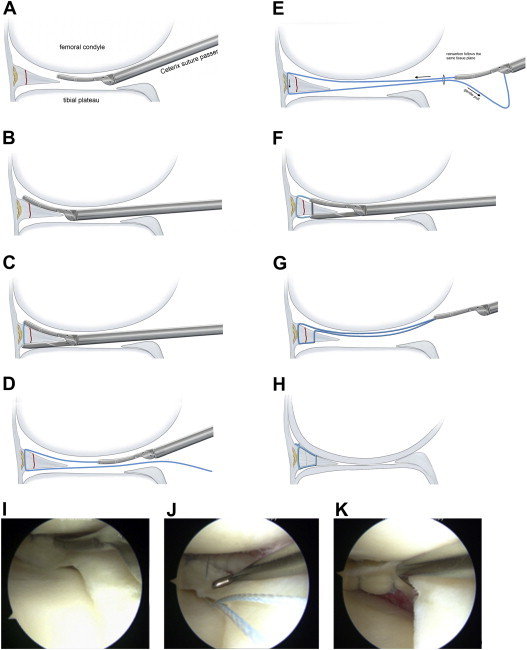
(A, B) The Ceterix suture passer is inserted through the working portal and advanced until the upper jaw is between the superior surface of the meniscus and the articular surface of the femoral condyle. (C) The lower jaw is then protracted forward so that it moves under the meniscus and the needle trigger is actuated to complete the peripheral pass of the suture from the lower jaw to the upper jaw, where it is atraumatically self retained. (D) The lower jaw is retracted and the device removed. (E) The lower jaw is then loaded with the opposite end of the suture while leaving the first end retained within the upper jaw. A gentle pull on the trailing suture during re-insertion ensures that there is not a tissue bridge. (F, G) The suture is passed evenly spaced on the other side of the tear, and then the lower jaw is again retracted and the device removed. (H) The knot is tied at the peripheral femorosynovial junction. Also shown are arthroscopic photos of the Ceterix Novostitch device passing suture to repair a vertical tear of the medial meniscus (I) in a 37-year-old woman. Note that in this case the 2 suture strands were shuttled to the tibial side (J) so that the knot could be placed within the tibial gutter (K) and that uniform tear compression was obtained. Video 1 shows this repair.
A minimally traumatic nitinol needle is deployed by squeezing the orange and black triggers in concert, which transfers the suture from the lower jaw, behind or through the meniscus, and into the upper jaw, where it is atraumatically self captured. The lower jaw is then retracted before device removal by depressing the lower jaw retract lever with the thumb (Fig 3D). Depending on the type of tear being repaired, the suture can then be tied and cut (as for horizontal cleavage tears) or brought down into a trough (as for root tears) or the second end of the suture can be loaded into the device and the device reinserted to complete the desired stitch pattern (as for vertical, oblique, and radial tears).
When repairing vertical, oblique and radial tears, reinsertion of the device along the same tissue plane can be guaranteed by leaving the first passed suture limb retained within the upper jaw. The lower jaw can then be loaded with the second suture end and retracted into the shaft as before, however on this insertion the passed suture strand can guide the upper jaw to the meniscus through the same tissue plane by gently pulling the second limb. In this way, the upper jaw is led into the joint along the identical tissue plane as the first passed limb so that there is no tissue bridging and so that knot tying can be performed without need for a cannula or sled (Figure 3E).
Once the desired suture pattern is achieved, a surgeon's square knot can be slid down to the peripheral femoral-meniscocapsular interface. If not cinched tightly on initial tying, this knot can be easily slid down the post and positioned in the optimally desired position.25 Applying 2 additional alternating half-hitches secures the knot. If the surgeon prefers the knot be placed within the peripheral tibial-sided gutter, the suture ends can be shuttled down to the tibial side before tying. The initially passed suture can also be used to shuttle polydioxanone suture before knot tying according to surgeon preference (Video 1). Use of 1 disposable passer allows placement of multiple circumferential compression stitches so that the tear can be anatomically compressed without concern for added procedure cost. Additional technique is shown in Video 1, and a summary of technique tips and pearls is listed in Table 1.
Table 1.
Technique Tips
| Use a spinal needle to optimize the approach angle prior to creating the working portal. |
| Switch camera portals to optimize the approach angle as necessary. This may sometimes be enhanced by an additional portal superior to the original camera portal. |
Avoid tissue bridging by following these steps:
|
| When necessary, enhance visibility in a tight or curved medial compartment by pie crusting the MCL. |
Discussion
Vertical Peripheral Tears
Vertical peripheral meniscus tears are among the most commonly repaired tear patterns because of the presence of a good peripheral blood supply and the robust central meniscal fragment that is typically available. Studies have shown that these tears, left untreated, increase contact pressure and decrease contact area at the tibiofemoral articular surfaces, making them important to repair.26
The gold standard for repair of peripheral vertical meniscus tears is inside-out, above-and-below repair because of its atraumatic needle diameter and its ability to uniformly compress the femoral and tibial sides of the tear.27-31 Consistent with this standard, studies have suggested that meniscus healing may be isolated to regions where the repair compresses the tear edges.18,32 Circumferential compression stitches provide uniform compression of the tear edges at the femoral, central, and tibial tear surfaces, without need for open exposure. In addition, the peripheral capsule is not directly incorporated into the repair, a feature that may avoid iatrogenic meniscal extrusion and intra-articular shrinkage of the functional meniscal surface area that can occur with other techniques.18 There is also likely to be little inherent risk to neurovascular structures because there is no posteriorly directed capsular penetration.
Lateral Meniscus Popliteal Hiatus Region Repair
The posterior horn of the lateral meniscus has traditionally been considered a region particularly difficult to repair because of the presence of the popliteal hiatus and the proximity of major neurovascular structures.20-24 The presented technique enables suture to be placed around the posterior aspect of the lateral meniscus without entrapment of the popliteal hiatus or tendon and without penetration toward neurovascular structures (Fig 4).
Fig 4.

Suture repair of a bucket-handle lateral meniscus tear in a 16-year-old boy with a small intact peripheral rim. This tear would be difficult to treat with traditional inside-out or all-inside techniques because of the presence of the popliteal hiatus and the proximity of neurovascular structures. (A) The first of multiple peripheral stitches is placed around the remnant at the region of the popliteal hiatus. (B) The Ceterix device is re-inserted to pass the central limb of the second stitch. (C) The first 2 stitches have been placed and tied at the region of the popliteal hiatus. At 6 months' follow-up, clinical healing had been obtained.
Radial and Oblique Tears
Radial meniscus tears have been shown to significantly increase contact pressure at the tibiofemoral articulation.33-37 Although successful repair of such tears has been reported, it has not been universally adopted because such repairs are difficult to perform in a manner that inspires confidence that the tear will heal.38-41 We have had success in placing simple and complex suture patterns within the meniscus to repair radial tears (Fig 5). The peripheral aspect of the tear can be sewn together, whereas the central edge can be removed without compromising the function of the meniscus.42
Fig 5.
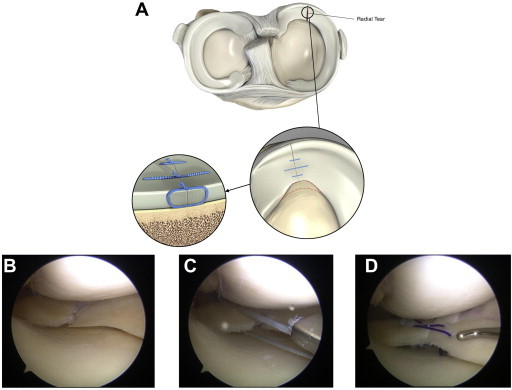
Radial meniscus tears can be repaired with the Ceterix device by placing circumferential stitches in any combination that best reduces and compresses the tear. (A) The central third of the meniscus can be excised, and the central and peripheral thirds can be repaired with side-to-side or figure-of-8 sutures. The photographs show a radial tear of the posterior horn of the medial meniscus (B) in a 55-year-old man with completely healthy tricompartmental articular surfaces. (C) Photograph taken after passage of the first stitch, showing the device being removed with the suture after it has been self retained in the upper jaw. (D) In this case the central 2 sutures were used to shuttle polydioxanone, and a third stitch was placed more peripherally and left as No. 2-0 nonabsorbable suture to back up the repair. Polydioxanone is sometimes used in radial tear repairs because the more central knots cannot be peripheralized like they can with circumferential compression stitches that are placed in the central to peripheral vector. Video 1 includes excerpts from this repair.
Horizontal Cleavage Tears
Horizontal cleavage tears have been shown to successfully heal after repair, but extensive open techniques have traditionally been required.43-46 Circumferential repair of these tears allows the superior and inferior lamina to be anatomically compressed along optimal vectors and is greatly simplified, requiring only 1 peripheral pass of suture in each repair location. The central white-white third of the meniscus is typically removed, allowing the stitch to surround the horizontal tear, as shown in Fig 6. The knots can be tied on the peripheral femoral or tibial side according to surgeon preference.
Fig 6.
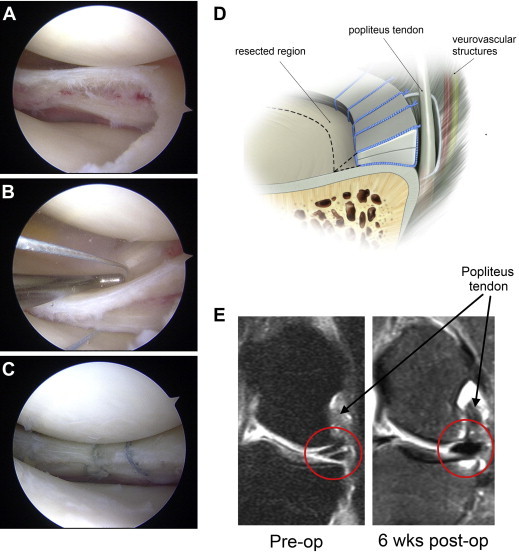
Horizontal cleavage tear of lateral meniscus in a 28-year-old woman before repair (A), after passage of the first stitch around the back of the meniscus at the level of the popliteal hiatus (B), and after repair (C). (D) Drawing showing resected and repaired regions relative to popliteal hiatus. (E) Coronal magnetic resonance images of lateral compartment at level of popliteal hiatus obtained preoperatively (Pre-op) and 6 weeks postoperatively (6 wks post-op), showing excellent early healing of the lateral meniscus horizontal cleavage tear. The postoperative magnetic resonance image was obtained to guide rehabilitation. The preoperative and postoperative MRI scans were obtained from different facilities with slightly different protocols explaining the difference in contrast within the bone.
Root Tears
Medial meniscus posterior root tears encompass 10% of all meniscus tears and render the meniscus nonfunctional.47-49 With the Ceterix technology, the surgeon can choose any number of suture patterns to secure the posterior horn meniscal tissue. Figure 7 shows a medially located simple vertical bight of tissue passed from the tibial to the femoral surface, followed by an inverted mattress stitch and an apical stitch to hold and align the tissue, respectively.
Fig 7.
Medial meniscus root tear repair in a 50-year-old woman. Four passes through the meniscus were made, including an inverted mattress stitch, and the sutures were brought through a bone tunnel and tied over a tibial washer. The bone tunnel was created with a FlipCutter device (Arthrex, Naples, FL), as shown in Video 1. Pictured is (A) Ceterix device removal after passage of the first stitch, (B) the meniscal root after passage of the above mentioned suture patterns, and (C) following reduction of the root into the prepared trough.
In summary, meniscus surgery has evolved from open total meniscectomy to all-arthroscopic suture repair. New technologies may enable surgeons to freely sew in the tight arthroscopic environment of the knee and allow placement of suture patterns previously considered difficult, if not impossible, to achieve. Surgeons may similarly be empowered to effectively repair several tear patterns that were previously considered difficult to sew. The potential advantages and limitations of the circumferential compression stitch are summarized in Table 2. Although additional studies will be required to fully define the long-term clinical benefits of such techniques, the historic body of orthopaedic literature supports the circumferential compression stitch and its ability to deliver strong, anatomic repairs.
Table 2.
Potential Advantages and Limitations of Circumferential Stitching With Ceterix Suture-Passing Device
| Potential Advantages | Potential Limitations |
|---|---|
| Improved healing | |
Tibial, femoral and intrasubstance regions of tear uniformly compressed
|
May be suboptimal for repair of meniscocapsular separations in large patients |
| Highest load to failure of all techniques25 | |
| Enables repair of complex patterns | |
| Improved safety | |
| Elimination of neurovascular risk | |
| Improved function | |
Capsule not entrapped in repair
|
Footnotes
The author reports the following potential conflict of interest or source of funding in relation to this article: Founder Ceterix Orthopaedics, Inc.
Supplementary data
Circumferential compression stitch for repair of a vertical medial meniscus tear, a horizontal cleavage tear, a vertical tibial-sided lateral meniscus tear at the level of the popliteal hiatus, a medial meniscus root tear, and a radial tear of the posterior horn of the medial meniscus. The steps for successful repair are shown, and magnetic resonance imaging views are reviewed when useful for preoperative planning.
References
- 1.Bolano L.E., Grana W.A. Isolated arthroscopic partial meniscectomy. Functional radiographic evaluation at five years. Am J Sports Med. 1993;21:432–437. doi: 10.1177/036354659302100318. [DOI] [PubMed] [Google Scholar]
- 2.Chatain F., Robinson A.H., Adeleine P., Chambat P., Neyret P. The natural history of the knee following arthroscopic medial meniscectomy. Knee Surg Sports Traumatol Arthrosc. 2001;9:15–18. doi: 10.1007/s001670000146. [DOI] [PubMed] [Google Scholar]
- 3.Hede A., Larsen E., Sandberg H. The long term outcome of open total and partial meniscectomy related to the quantity and site of the meniscus removed. Int Orthop. 1992;16:122–125. doi: 10.1007/BF00180200. [DOI] [PubMed] [Google Scholar]
- 4.Covall D.J., Wasilewski S.A. Roentgenographic changes after arthroscopic meniscectomy: Five-year follow-up in patients more than 45 years old. Arthroscopy. 1992;8:242–246. doi: 10.1016/0749-8063(92)90044-c. [DOI] [PubMed] [Google Scholar]
- 5.Faunø P., Nielsen A.B. Arthroscopic partial meniscectomy: A long-term follow-up. Arthroscopy. 1992;8:345–349. doi: 10.1016/0749-8063(92)90066-k. [DOI] [PubMed] [Google Scholar]
- 6.Scheller G., Sobau C., Bülow J.U. Arthroscopic partial lateral meniscectomy in an otherwise normal knee: Clinical, functional, and radiographic results of a long-term follow-up study. Arthroscopy. 2001;17:946–952. doi: 10.1053/jars.2001.28952. [DOI] [PubMed] [Google Scholar]
- 7.Hoser C., Fink C., Brown C., Reichkendler M., Hackl W., Bartlett J. Long-term results of arthroscopic partial lateral meniscectomy in knees without associated damage. J Bone Joint Surg Br. 2001;83:513–516. doi: 10.1302/0301-620x.83b4.11364. [DOI] [PubMed] [Google Scholar]
- 8.Cicuttini F.M., Forbes A., Yuanyuan W., Rush G., Stuckey S.L. Rate of knee cartilage loss after partial meniscectomy. J Rheumatol. 2002;29:1954–1956. [PubMed] [Google Scholar]
- 9.Little C., Smith S., Ghosh P., Bellenger C. Histomorphological and immunohistochemical evaluation of joint changes in a model of osteoarthritis induced by lateral meniscectomy in sheep. J Rheumatol. 1997;24:2199–2209. [PubMed] [Google Scholar]
- 10.Baratz M.E., Fu F.H., Mengato R. Meniscal tears: The effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14:270–275. doi: 10.1177/036354658601400405. [DOI] [PubMed] [Google Scholar]
- 11.Englund M., Lohmander L.S. Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum. 2004;50:2811–2819. doi: 10.1002/art.20489. [DOI] [PubMed] [Google Scholar]
- 12.Nepple J., Dunn W., Wright R. Meniscal repair outcomes at greater than five years: A systematic literature review and meta-analysis. J Bone Joint Surg Am. 2012;94:2222–2227. doi: 10.2106/JBJS.K.01584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eggli S., Wegmuller H., Kosina J. Long-term results of arthroscopic meniscal repair. An analysis of isolated tears. Am J Sports Med. 1995;23:715–720. doi: 10.1177/036354659502300614. [DOI] [PubMed] [Google Scholar]
- 14.Gillquist R.P. Results of open meniscus repair. Long-term follow-up study with a matched uninjured control group. J Bone Joint Surg Br. 2000;82:494–498. doi: 10.1302/0301-620x.82b4.9942. [DOI] [PubMed] [Google Scholar]
- 15.Lozano J., Ma B., Cannon W.D. All-inside meniscus repair. Clin Orthop Relat Res. 2006;455:134–141. doi: 10.1097/BLO.0b013e31802ff806. [DOI] [PubMed] [Google Scholar]
- 16.Paxton E.S., Stock M.V., Brophy R.H. Meniscal repair versus partial meniscectomy: A systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27:1275–1288. doi: 10.1016/j.arthro.2011.03.088. [DOI] [PubMed] [Google Scholar]
- 17.Grant J.A., Wilde J., Miller B.S., Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears. Am J Sports Med. 2011;20:1–10. doi: 10.1177/0363546511411701. [DOI] [PubMed] [Google Scholar]
- 18.Pujol N., Panarella L., Selmi T. Meniscal healing after meniscal repair: A CT arthrography assessment. Am J Sports Med. 2008;36:1489–1495. doi: 10.1177/0363546508316771. [DOI] [PubMed] [Google Scholar]
- 19.Klecker R.J., Winalski C.S., Aliabadi P., Minas T. The aberrant anterior tibial artery. Am J Sports Med. 2008;36:720–727. doi: 10.1177/0363546507311595. [DOI] [PubMed] [Google Scholar]
- 20.Baena A.E., Castilla B.M., Fernandez J.S., de Rota Conde A.F., Reina A.E., Rubio F.E. Inside-out medial meniscus suture: An analysis of the risk of injury to the popliteal neurovascular bundle. Arthroscopy. 2011;27:516–521. doi: 10.1016/j.arthro.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 21.Cohen S.B., Boyd L., Miller M.D. Vascular risk associated with meniscal repair using RapidLoc versus Fast-Fix—Comparison of two all-inside meniscal devices. J Knee Surg. 2007;20:235–240. doi: 10.1055/s-0030-1248049. [DOI] [PubMed] [Google Scholar]
- 22.Small N.C., Farless B.L. Avoiding complications in meniscal repair. Tech Orthop. 1993;8:70–75. [Google Scholar]
- 23.Stärke C., Kopf S., Petersen W., Becker R. Meniscal repair. Arthroscopy. 2009;25:1033–1044. doi: 10.1016/j.arthro.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 24.Asık M., Sener N. Failure strength of repair devices versus meniscus suturing techniques. Knee Surg Sports Traumatol Arthrosc. 2002;10:25–29. doi: 10.1007/s001670100247. [DOI] [PubMed] [Google Scholar]
- 25.Nottage W.M., Lieurance R.K. Arthroscopic knot tying techniques. Arthroscopy. 1999;15:515–521. doi: 10.1053/ar.1999.v15.015051. [DOI] [PubMed] [Google Scholar]
- 26.Muriuki M.G., Tuason M.D., Tucker B.G., Harner C.D. Changes in tibiofemoral contact mechanics following radial split and vertical tears of the medial meniscus. J Bone Joint Surg Am. 2011;93:1089–1095. doi: 10.2106/JBJS.I.01241. [DOI] [PubMed] [Google Scholar]
- 27.Post W.R., Akers S.R., Kish V. Load to failure of common meniscal repair techniques: Effects of suture technique and suture material. Arthroscopy. 1997;13:731–736. doi: 10.1016/s0749-8063(97)90008-6. [DOI] [PubMed] [Google Scholar]
- 28.Rimmer M.G., Nawana N.S., Keene G.C., Pearcy M.J. Failure strengths of different meniscal suturing techniques. Arthroscopy. 1995;11:146–150. doi: 10.1016/0749-8063(95)90059-4. [DOI] [PubMed] [Google Scholar]
- 29.DeHaven K.E. Meniscus repair. Am J Sports Med. 1999;27:242–250. doi: 10.1177/03635465990270022301. [DOI] [PubMed] [Google Scholar]
- 30.Noyes F.R., Barber-Westin S.D. Repair of complex and avascular meniscal tears and meniscal transplantation. J Bone Joint Surg Am. 2010;92:1012–1029. [PubMed] [Google Scholar]
- 31.Noyes F.R., Barber-Westin S.D. Management of meniscus tears that extend into the avascular region. Clin Sports Med. 2012;31:65–90. doi: 10.1016/j.csm.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 32.Van Trommel M.F., Simonian P.T., Potter H.G., Wickiewicz T.L. Different regional healing rates with the outside-in technique for meniscal repair. Am J Sports Med. 1998;26:446–452. doi: 10.1177/03635465980260031901. [DOI] [PubMed] [Google Scholar]
- 33.Ode G.E., Van Thiel G.S., McArthur S.A. Effects of serial sectioning and repair of radial tears in the lateral meniscus. Am J Sports Med. 2012;40:1863–1870. doi: 10.1177/0363546512453291. [DOI] [PubMed] [Google Scholar]
- 34.Kan A., Oshida M., Oshida S., Imada M., Nakagawa T., Okinaga S. Anatomical significance of a posterior horn of medial meniscus: The relationship between its radial tear and cartilage degradation of joint surface. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:1. doi: 10.1186/1758-2555-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harper K.W., Helms C.A., Lambert H.S., III, Higgins L.D. Radial meniscal tears: Significance, incidence, and MR appearance. AJR Am J Roentgenol. 2005;185:1429–1434. doi: 10.2214/AJR.04.1024. [DOI] [PubMed] [Google Scholar]
- 36.Kidron A., Thein R. Radial tears associated with cleavage tears of the medial meniscus in athletes. Arthroscopy. 2002;18:254–256. doi: 10.1053/jars.2002.30650. [DOI] [PubMed] [Google Scholar]
- 37.Smith J.P., III, Barrett G.R. Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees. A prospective analysis of 575 tears. Am J Sports Med. 2001;29:415–419. doi: 10.1177/03635465010290040501. [DOI] [PubMed] [Google Scholar]
- 38.Haklar U., Kocaoglu B., Nalbantoglu U., Tuzuner T., Guven O. Arthroscopic repair of radial lateral meniscus [corrected] tear by double horizontal sutures with inside-outside technique. Knee. 2008;15:355–359. doi: 10.1016/j.knee.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 39.van Trommel M.F., Simonian P.T., Potter H.G., Wickiewicz T.L. Arthroscopic meniscal repair with fibrin clot of complete radial tears of the lateral meniscus in the avascular zone. Arthroscopy. 1998;14:360–365. doi: 10.1016/s0749-8063(98)70002-7. [DOI] [PubMed] [Google Scholar]
- 40.Tao S.S., Beach W.R. Use of a Caspari suture punch to repair a radial tear of the lateral meniscus. Arthroscopy. 2002;18:206–210. doi: 10.1053/jars.2002.26858. [DOI] [PubMed] [Google Scholar]
- 41.Matsubara H., Okazaki K., Izawa T. New suture method for radial tears of the meniscus: Biomechanical analysis of cross-suture and double horizontal suture techniques using cyclic load testing. Am J Sports Med. 2012;40:414–418. doi: 10.1177/0363546511424395. [DOI] [PubMed] [Google Scholar]
- 42.Bedi A., Kelly N.H., Baad M. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am. 2010;92:1398–1408. doi: 10.2106/JBJS.I.00539. [DOI] [PubMed] [Google Scholar]
- 43.Pujol N, Bohu Y, Boisrenoult P, Macdes A, Beaufils P. Clinical outcomes of open meniscal repair of horizontal meniscal tears in young patients. Knee Surg Sports Traumatol Arthrosc. 14 June, 2012 [Epub ahead of print]. [DOI] [PubMed]
- 44.Kamimura T., Kimura M. Repair of horizontal meniscal cleavage tears with exogenous fibrin clots. Knee Surg Sports Traumatol Arthrosc. 2011;19:1154–1157. doi: 10.1007/s00167-011-1404-5. [DOI] [PubMed] [Google Scholar]
- 45.Biedert R.M. Treatment of intrasubstance meniscal lesions: A randomized prospective study of four different methods. Knee Surg Sports Traumatol Arthrosc. 2000;8:104–108. doi: 10.1007/s001670050195. [DOI] [PubMed] [Google Scholar]
- 46.Rubman M.H., Noyes F.R., Barber-Westin S.D. Arthroscopic repair of meniscal tears that extend into the avascular zone. Am J Sports Med. 1998;26:87–95. doi: 10.1177/03635465980260013301. [DOI] [PubMed] [Google Scholar]
- 47.Seedhom B.B., Dowson D., Wright V. Proceedings: Functions of the menisci: A preliminary study. Ann Rheum Dis. 1974;33:111. doi: 10.1136/ard.33.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ozkoc G., Circi E., Gonc U., Irgit K., Pourbagher A., Tandogan R.N. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16:849–854. doi: 10.1007/s00167-008-0569-z. [DOI] [PubMed] [Google Scholar]
- 49.Bin S.I., Kim J.M., Shin S.J. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20:373–378. doi: 10.1016/j.arthro.2004.01.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Circumferential compression stitch for repair of a vertical medial meniscus tear, a horizontal cleavage tear, a vertical tibial-sided lateral meniscus tear at the level of the popliteal hiatus, a medial meniscus root tear, and a radial tear of the posterior horn of the medial meniscus. The steps for successful repair are shown, and magnetic resonance imaging views are reviewed when useful for preoperative planning.


