Abstract
Objective
Mindfulness-based stress reduction (MBSR) is an increasingly popular practice demonstrated to alleviate stress and treat certain health conditions. MBSR may reduce elevated blood pressure (BP). Treatment guidelines recommend lifestyle modifications for BP in the prehypertensive range (SBP 120–139 or DBP 80–89), followed by antihypertensives if BP reaches hypertensive levels. MBSR has not been thoroughly evaluated as a treatment for prehypertension. A randomized clinical trial of MBSR for high BP was conducted to determine whether BP reductions associated with MBSR exceed those observed for an active control condition consisting of progressive muscle relaxation training (PMR).
Methods
56 men (43%) and women (57%) averaging 50.3 (SD = 6.5) years of age (91% Caucasian) with unmedicated BP in the prehypertensive range were randomized to 8 weeks of MBSR or PMR delivered in a group format. Treatment sessions were administered by 1 treatment provider and lasted approximately 2.5 hours each week. Clinic BP was the primary outcome measure. Ambulatory BP was a secondary outcome measure.
Results
Analyses were based on intent-to-treat. Patients randomized to MBSR exhibited a 4.8 mm Hg reduction in clinic SBP, which was larger than the 0.7 mm Hg reduction observed for PMR, p = .016. Those randomized to MBSR exhibited a 1.9 mm Hg reduction in DBP, compared to a 1.2 mm Hg increase for PMR, p = .008. MBSR did not result in larger decreases in ambulatory BP than PMR.
Conclusions
MBSR resulted in a reduction in clinic SBP and DBP compared to PMR.
Keywords: Mindfulness, meditation, prehypertension, blood pressure, clinical trial, MBSR
Nearly 60 million adults in the United States have high blood pressure (BP) in the prehypertensive range (SBP of 120–139 or DBP of 80–89) (1, 2). Current treatment guidelines recommend health-promoting lifestyle modifications, including exercise, weight loss, and dietary changes (e.g., adopting the DASH diet) for individuals with BP in the prehypertensive range. Antihypertensive medication is not indicated but should be initiated if lifestyle changes fail to prevent BP from reaching hypertensive levels (2).
Mindfulness-based stress reduction (MBSR) is an increasingly popular practice that has been purported to alleviate stress, treat depression and anxiety, and treat certain health conditions. MBSR incorporates meditation and stress management into a structured stress management program. Meditation treatments, such as MBSR, are not substitutes for health behavior changes, but have been evaluated for their potential to lower BP. MBSR has been alleged to reduce BP, although there has been only one published controlled trial of a similar treatment, mindfulness meditation, on BP (3). In this study, 73 normotensive middle school students were randomly assigned to 10 minutes of daily meditation for 3 months or to a health education control condition. A larger reduction in resting SBP was associated with the meditation intervention, as well as larger reductions in ambulatory BP during certain time periods (e.g., SBP and DBP after school). Although these findings are encouraging, applying the data from normotensive children to the adult population with elevated BP is speculative. A recent American Heart Association (AHA) Scientific Statement (4) reviewed this literature and acknowledged that there are few trials of meditation techniques (other than transcendental meditation; see below) for BP reduction.
Other stress management therapies and meditation practices have shown some promise in reducing elevated BP (5, 5–10). For example, two meta-analyses of stress management treatments for hypertension concluded that multi-component stress management therapies can be effective in reducing BP and that single-component stress management therapies (e.g., relaxation alone) are less effective (11, 12). However, a later meta-analysis reported that stress management training was not very effective in lowering BP (13).
Relaxation therapies, such as progressive muscle relaxation (PMR), have not consistently lowered high BP. The Hypertension Intervention Pooling Project integrated data from 12 randomized controlled trials and concluded that relaxation provided a small treatment effect for DBP and no treatment effect for SBP among unmedicated patients with hypertension (14). Despite good patient acceptance of PMR, it is consequently not currently considered an effective treatment for high BP. It was thus chosen as an active control condition because PMR can appear to be a credible treatment and can be matched with the MBSR condition for therapist contact and homework.
Transcendental meditation (TM) has been the most extensively studied meditation therapy for high BP. A report commissioned by the Agency for Healthcare and Research Quality (AHRQ) concluded that TM, Qi Gong, and Zen Buddhist meditation reduced BP (15). Although not without controversy, the AHRQ report also concluded that the studies often had poor methodological quality and that the effect of TM on BP was small when compared to a health education control condition (e.g., 1.1 mm Hg SBP). A subsequent meta-analysis, which included additional studies, concluded that TM reduced SBP by 5.0 mm Hg and DBP 2.8 mm Hg compared to control conditions (13). The recent AHA statement concluded that TM produces modest reductions in BP (4).
Although both MBSR and TM can be regarded as meditation therapies, there are obvious differences in how they are taught and practiced. For example, TM consists solely of meditation, whereas MBSR includes three skills: meditation, body scan, and non-strenuous yoga. TM is taught via personal instruction and practice, whereas MBSR is a structured 8-week group stress management program. Thus, they are not necessarily equivalent treatments merely by virtue of involving meditation. There are few trials comparing TM with other meditation interventions (4). The relative effectiveness of existing meditation methods for reducing BP is not known, although there is less evidence that meditation techniques besides TM are effective for lowering BP. It remains an empirical question and one beyond the scope of this study to address whether MBSR and TM have differing effects on blood pressure.
Collectively, the widespread use of MBSR, the trial showing some BP reduction in adolescents (3), the AHRQ report (15), and the AHA statement (4) suggest the need for randomized trials of MBSR for BP reduction. When combined with lifestyle modification advice, MBSR may be an appropriate complementary treatment for prehypertension or adjunct to pharmacotherapy for hypertension. There are several potential mechanisms for how MBSR might lower BP. Meditation may affect the sympathetic nervous system, effectively reducing cardiac output, increased heart rate, and increased norepinephrine levels observed in the early stages of elevated blood pressure (16, 17). MBSR may improve subjective feelings of stress, reduce negative affect, or improve coping with negative affect. It is also possible that mindfulness training can improve adherence to lifestyle modification advice. Prehypertension was targeted because pharmacological treatments are necessary for BP above the prehypertensive range, but also because the magnitude of BP lowering obtained with MBSR may be adequate for patients who desire to avoid or delay antihypertensive medication.
This study examined the effects of MBSR on high BP using a small-scale randomized controlled design. A total of 56 patients with unmedicated elevated BP in the prehypertensive range (SBP 120–139 mm Hg or DBP 80–89 mm Hg) were randomized to MBSR or an active control condition, PMR. All patients received lifestyle modification advice in keeping with current guidelines for the treatment of prehypertension. It was hypothesized that MBSR would result in greater BP reductions than PMR.
Methods
Study Participants
Healthy individuals aged 30–60 years with unmedicated BP in the prehypertensive range (SBP 120–139 mm Hg or DBP 80–89 mm Hg) were sought for this trial. Participants could not be taking antihypertensive medication, could not be experienced with meditation practices, could not be current smokers, and could not report any disease (e.g., myocardial infarction, heart failure, chronic kidney disease, diabetes) that would mandate treatment with drugs that could substantially affect BP.
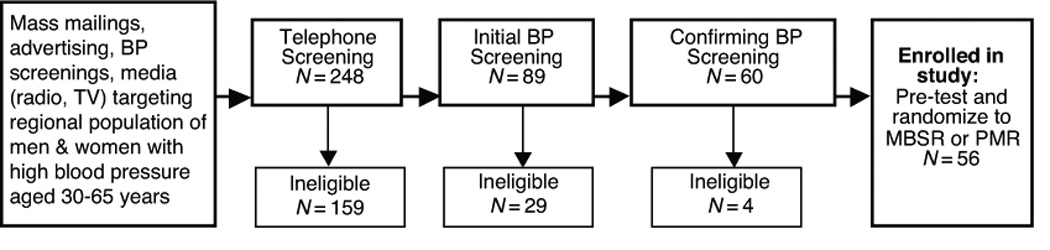
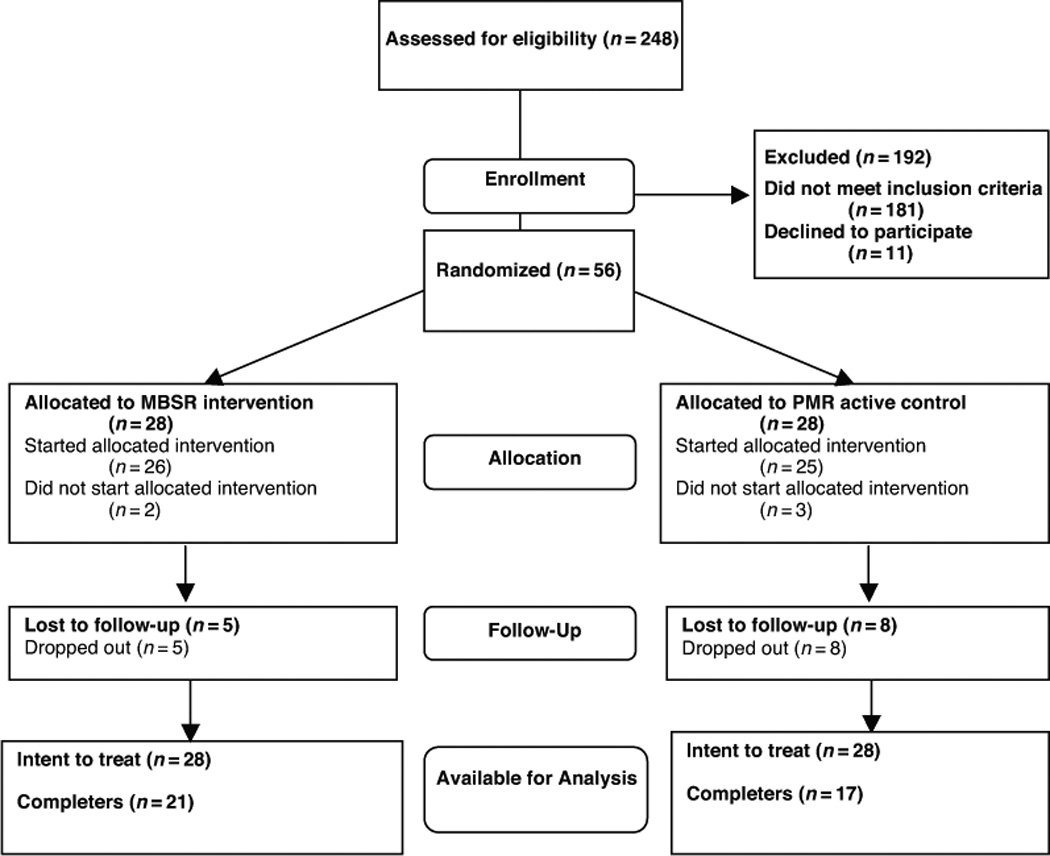
Enrollment began in January 2006. Participants were enrolled in 7 cohorts ranging in size from 3–11. MBSR and PMR treatment groups included some non-protocol patients in order to increase the group size so that a high-quality group treatment experience could be provided to every patient enrolled in the trial. That is, some individuals who were not enrolled in the trial participated in the treatment groups. The circumstances of their involvement was that they had responded to the advertisements but were not eligible for enrollment. Reasons for ineligibility included falling outside the age range, taking antihypertensive medication, previous experience with meditation, being a smoker, or not being pre-hypertensive. When patients were ineligible but remained interested in participating in treatment, they were allowed to opt to participate in one of the treatments. There were 13 non-protocol participants in each group. No baseline BP data were collected from non-protocol patients, and their presence was designed to maintain an adequate group size. The CONSORT chart in Figure 1 presents the flow of patients through the trial. Patient accrual from recruiting efforts and eligibility screening is presented in Figure 2.
Figure 1.
CONSORT Chart
Figure 2.
Patient accrual from recruiting efforts and eligibility screening
Procedure
The Institutional Review boards of Kent State University and SUMMA Health System reviewed and approved the study procedures. Prospective participants completed a telephone screening that included questions about their medical history. If there were any concerns about whether or not a patient was “healthy” for purposes of eligibility, the case was reviewed by the study physician (RAJ). Those who appeared eligible then scheduled an initial BP screening, which consisted of three separate BP readings separated by 5 minutes after 10 minutes of quiet rest (additional details in the measures below). This initial screening was followed by a second screening approximately one week later that followed the same procedures, and participants were scheduled for a pre-treatment assessment approximately one week later. When they returned, a third screening that used the same procedures was conducted. If BP remained in the pre-hypertensive range, the patient was enrolled and the pre-treatment assessment was completed at the same visit. Thus, BP had to remain in the prehypertension range on three separate determinations over a three-week period for patients to be eligible. If BP was not in the pre-hypertensive range at any of the three screenings, the patient was no longer eligible and was not enrolled. Participants who were eligible and who consented to participate in the study were enrolled in the study and completed a pre-test assessment including clinic and ambulatory BP. After the pre-test assessment, patients were randomized to eight weekly sessions of MBSR or PMR using an order of assignment generated by random number, stratified for gender and ethnicity. After the eight sessions, patients returned for reassessment of both clinic and ambulatory BP, as described below in the measurement procedures.
Blinding
Concealment of treatment allocation was maintained by having different study personnel perform recruitment and treatment assignment functions so the investigators responsible for recruiting and assessments were not aware of random assignment. The adequacy of this blinding procedure was assessed using a questionnaire asking the primary research assistants to predict group membership. No patient volunteered their treatment assignment to the research assistants, and research assistants were unable to predict group membership (Cohen’s к = .135, p = .37), confirming adequacy of blinding. Furthermore, investigators responsible for random assignment and the delivery of the treatments were not aware of assessment results (e.g., BP values) until after the study was complete. The blind was not broken until after the final assessment.
MBSR
The MBSR program consisted of eight group sessions, each 2.5 hours long, and delivered on consecutive weeks. MBSR included instruction and practice in mindfulness meditation skills along with discussion of stress, coping, and homework assignments. The MBSR therapist participated in the mindfulness exercises with group members during the weekly sessions, and group members were instructed to practice these mindfulness exercises outside group meetings for at least 45 minutes per day, 6 days per week. Homework was collected by the study therapist and consisted of weekly logs in the participant folder with spaces for each day of the week for participants to record the duration of homework completed.
Group members were taught three main varieties of mindfulness skills: the body scan exercise, sitting meditation, and yoga exercises. The body scan exercise entails lying down with one’s eyes closed and deliberately focusing one’s attention on various parts of the body with the goal of noticing nuances of sensations going on within the body. In sitting meditation, participants sit in a relaxed and wakeful posture with eyes closed and deliberately bring their attention to the sensations of breathing. Finally, group members learned a series of physically non-strenuous yoga exercises designed to bring mindful attention to bodily sensations during gentle movements and stretching. The daily homework exercises consisted of repeating body scan work, sitting meditation and yoga exercises at home to provide practice and generalization of the skills. Group members were provided audiotapes or CD’s with guided MBSR exercises to assist their homework. In addition, group members were encouraged to bring mindful attention to daily activities such as walking, standing, and eating.
Progressive Muscle Relaxation Training
The PMR treatment was based on a manual created for this study, adapted from other sources (18). PMR consisted of eight group sessions lasting 2.5 hours each delivered on consecutive weeks. PMR patients received instruction and practice in PMR skills, which involved learning to achieve a state of relaxation by alternately tensing and relaxing various muscle groups, along with homework assignments. The PMR therapist participated in the exercises with group members during the weekly sessions. Sessions progressed from 16 muscle group relaxation to 7 muscle groups, 4 muscle groups, and finally relaxation by recall. Relaxation by recall was intended to allow participants learning PMR to apply relaxation skills during their daily lives, and there was explicit instruction on generalizing the relaxation response to stressful situations. Group members were instructed to practice these exercises outside group meetings for at least 45 minutes per day, six days per week. Homework was collected by the study therapist and consisted of weekly logs in the participant folder with spaces for each day of the week for participants to record the duration of homework completed. They were provided with audio recordings of to assist their home PMR exercises.
Measures
Clinic BP
All clinic BP assessments were completed in a quiet, climate controlled room. All measures were completed in the same room, and in accordance with American Heart Association guidelines for taking BP (19). Participants were asked to refrain from consuming caffeine for at least 60 minutes prior to their appointment time. Patients had their BP assessed on their non-dominant arm while sitting in a chair with their feet flat on the floor and their arm supported at heart level. Patients rested quietly for 10 minutes, and then had 3 seated BP readings taken, each 5 minutes apart using an automated oscillometric BP device (Accutor Plus Oscillometric BP Monitor, Datascope Corp, Mahwah, NH). An automated oscillometric BP device was chosen in favor of manual sphygmomanometer for several reasons. First, mercury has been phased out (20). Second, the Accutor Plus performed well in a validation study (21). Specifically, the Datascope Accutor Plus received a grade of A (British Society of Hypertension) for both systolic and diastolic BP and met the Association for the Advancement of Medical Instrumentation guidelines (the mean difference between the BP device and the mercury standard were ≤ 5 mmHg). Finally, an automated device eliminated any potential experimenter bias. Clinic BP assessment procedures were the same at the BP screening, pre-test, and post-test assessment visits. Pre-test and post-test clinic BP are based on one visit and are not aggregated across several visits.
Ambulatory BP
Following the laboratory assessments, participants completed 24-hour ambulatory BP monitoring. Participants were instrumented with an Oscar (Suntech, Raleigh, NC) oscillometric BP monitor at the time of their assessment, and the monitor was programmed to take three BP measurements each hour between the hours of 6 AM to 11 PM and two BP measurements were taken each hour between the hours of 11 PM to 6 AM. Participants were instructed to lower their arms to their sides as soon as they sensed the cuff inflating and to keep it relaxed and still until a few seconds after the deflation had finished because of possible movement artifact. Artifactual values were deleted after inspection by an experienced examiner blind to patient condition using modified Casadei criteria (22). Participants wore the ambulatory BP device for a continuous 24-hour period. Daytime and nighttime BP values were defined by patient diary entries indicating sleep and waking times.
Data analysis
The primary outcome measures were clinic SBP and DBP, and secondary outcome variables were ambulatory SBP and DBP. Clinic BP for analyses was derived by taking the average of the three BP readings from the final pre-test visit and the three readings from the post-test assessment visit. Ambulatory SBP and DBP were derived by computing the mean of all valid readings obtained during waking hours and nighttime sleep. Hierarchical linear regression analyses using pre-intervention clinic BP levels as control variables were conducted separately for change in clinic SBP and DBP. A variable representing treatment condition was regressed on change in clinic BP score from pretest to posttest while controlling for pretest clinic BP levels in separate analyses. The same analytic strategy was used for ambulatory BP. Analyses were based on intent to treat with baseline values carried forward when post-treatment values were missing, although analyses were repeated with completers to check for consistency. That is, discrepant results for completers could reveal a bias in the intent-to-treat analyses given the higher drop out among patients randomized to PMR. Furthermore, although evaluating group effects on change scores is equivalent to the interaction term from a 2 (group; MBSR vs. PMR) by 2 (time; pretreatment vs. posttreatment) factorial design, for completeness these interaction terms were reported for clinic BP as well as mean values of posttreatment BP. All analyses were conducted at the .05 level of significance and were not corrected for multiple comparisons. Data were analyzed using IBM SPSS Version 20 (Chicago, IL) using linear regression procedures with forced entry of control variables. Means reported in the table are unadjusted means from simple descriptive statistics.
Results
Description of the sample
Participants included 56 men (24) and women (32) with a mean (SD) age of 50.3 (6.5) years of age (91% white) with unmedicated BP in the prehypertensive range. Demographic and medical characteristics (Table 1) were similar between groups. Patients were generally overweight, with a mean (SD) BMI of 30.0 (5.9). Clinic blood pressures were similar in both the MBSR and PMR groups at baseline. However, ambulatory BP’s were slightly lower among those assigned to the MBSR group as shown in Table 1.
Table 1.
Clinical and demographic characteristics of study sample.
| All Patients |
MBSR | PMR |
*p value |
|
|---|---|---|---|---|
| N** | 56 | 28 | 28 | |
| Age | 50.3 (6.5) | 51.2 (5.8) | 49.5 (7.2) | .338 |
| Gender (% female) | 57% | 61% | 54% | .589 |
| Race (% white) | 91% | 89% | 93% | .639 |
| Body mass index | 30 (5.9) | 30 (6.5) | 30 (5.2) | .964 |
| Employed | 66% | 57% | 75% | .317 |
| Education | 15.7(2.6) | 16.0 (2.7) | 15.4 (2.5) | .407 |
| Blood Pressure (mm Hg) | ||||
| Systolic | ||||
| Clinic | 129.5+(6.3) | 130.2 (6.3) | 128.8 (6.3) | .428 |
| Daytime | 137.1(10.8) | 134.4 (9.3) | 139.9 (11.6) | .055 |
| Nighttime | 117.3+(10.8) | 113.8 (8.9) | 120.6 (11.6) | .019 |
| Diastolic | ||||
| Clinic | 77.8 (5.5) | 77.3 (4.8) | 78.3 (6.1) | .484 |
| Daytime | 82.9 (7.5) | 79.9 (5.6) | 85.7 (8.1) | .033 |
| Nighttime | 67.3 (7.8) | 65.3 (6.3) | 69.3 (8.7) | .061 |
Data are shown as mean (SD) unless otherwise indicated.
group difference at baseline using t-test for independent groups for continuous variables and chi square for dichotomous variables (e.g., employment, race)
for ambulatory BP, N = 27 in the MBSR group
Treatment adherence and fidelity
Equal numbers of patients were randomized to the MBSR and PMR conditions (Figure 1). Two patients did not begin the MBSR intervention and 3 did not start the PMR intervention, due to unanticipated conflicts with the scheduled group treatment times. Five participants did not complete the MBSR intervention and 8 did not complete the PMR condition. One additional individual in the MBSR group did not have ambulatory BP data available because of equipment failure. In the MBSR group, attendance at treatment sessions was 89%, and in the PMR condition attendance was 90%. Home practice logs were submitted 74% of the time by participants in PMR groups and 74% of the time by participants in the MBSR groups.
Clients were treated by a licensed clinical psychologist (RM) with a longtime personal meditation practice, who also received formal training in MBSR by Jon Kabat-Zinn and Saki Santorelli. Treatment sessions were video recorded, and a clinical trials researcher with extensive familiarity with MBSR (LC) evaluated approximately half (45/112) for treatment fidelity and adherence to the treatment manuals. Using a scale of 1 to 5 with higher ratings indicating greater adherence, MBSR sessions received an average rating of 4.4 (range = 4.2 to 4.7); PMR sessions received an average rating of 4.3 (range = 4.1 to 4.7).
Clinic Blood Pressure
MBSR resulted in substantial and statistically significant reductions in the primary outcomes of clinic SBP and DBP (see Figure 3). Hierarchical multiple linear regression analyses were performed to evaluate the effect of the two treatments on changes in clinic SBP and DBP. The first step regressed change in BP on pretest BP. For clinic SBP, the equation containing these variables accounted for less than 2% of the variability in SBP change, F(1,54) = 0.96, p = 0.331. Adding treatment condition to the model explained an additional 10.3% of the variance in change in SBP, F(1,53) = 6.23, p = 0.016. Thus, the 4.9 mm Hg reduction in clinic SBP observed in the MBSR treatment condition exceeded the 0.7 mm Hg reduction observed in the PMR group. The interaction term from the group by time ANOVA was similar, F(1,54) = 6.77, p = 0.012, although simple main effects revealed that posttreatment SBP for the MBSR group (M = 128.1, SD = 9.1) was not lower than SBP for the PMR group (M = 125.3, SD = 7.4), p = .208. When regression analyses were repeated with completers, treatment condition accounted for 12.4% of the variability in SBP change after controlling for pretreatment clinic SBP, F(1,35) = 5.2, p = 0.029. The 6.5 mm Hg reduction in clinic SBP observed in the MBSR treatment condition exceeded the 1.1 mm Hg reduction observed in the PMR group.
Figure 3. Change in clinic Blood Pressure by Treatment (Intent-to-treat).
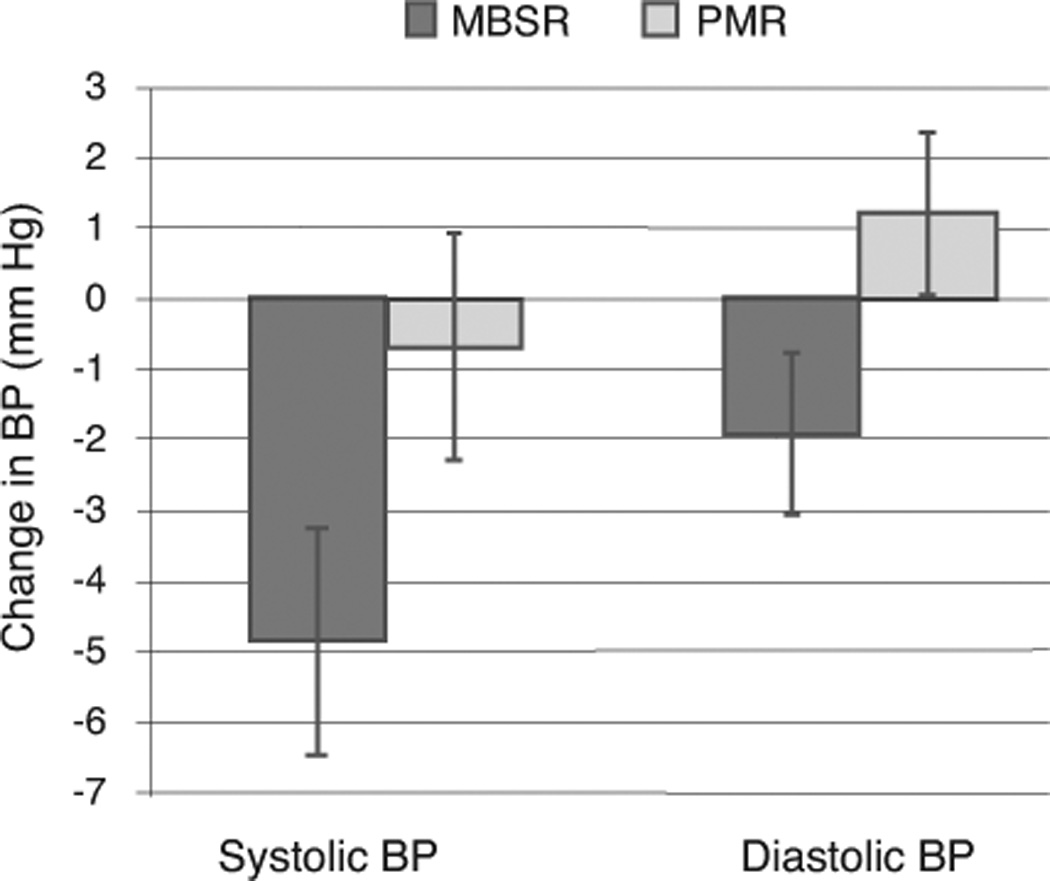
Mean change in clinic systolic and diastolic blood pressure from pretreatment to posttreatment. Error bars represent the standard error of the mean. PMR = progressive muscle relaxation. MBSR = mindfulness-based stress reduction.
For clinic DBP, pretest values and gender accounted for less than 1% of the variance in change in DBP, F(1,54) = 0.15, p = 0.702. Adding treatment condition to the model explained an additional 12.5% of the variance in change in DBP, F(1,53) = 7.58, p = 0.008. Thus, the 1.9 mm Hg reduction in clinic DBP observed in the MBSR treatment condition was a larger reduction in DBP than the 1.2 mm Hg increase observed in the PMR group. The interaction term from the group by time ANOVA was similar, F(1,54) = 7.38, p = 0.009, and simple main-effects revealed that posttreatment DBP for the MBSR group (M = 75.4, SD = 5.1) was lower than SBP for the PMR group (M = 79.4, SD = 8.0), p = .023. When regression analyses were repeated with completers, treatment condition accounted for 18.5% of the variability in DBP change after controlling for pretreatment clinic DBP, F(1,35) = 8.0, p = 0.008. The 2.6 mm Hg reduction in clinic DBP observed in the MBSR treatment condition exceeded the 2.0 mm Hg increase observed in the PMR group.
The consistency of the effects was examined for exploratory purposes. In the MBSR group, 18 of 21 completers (86%) experienced at least a 1 mm Hg reduction in SBP compared to 7 of 17 in the PMR group (41%). For DBP, 13 of 21 completers exhibited at least a 1 mm Hg reduction in BP (61%) compared to 7 of 17 (41%) in the PMR group.
Ambulatory Blood Pressure
Hierarchical multiple linear regression analyses were performed to evaluate the effect of the two treatments on changes in daytime and sleeping ambulatory SBP and DBP, which were secondary outcomes. The first step regressed change in BP on pretest BP. The second step added treatment condition. For change in daytime ambulatory SBP, pretest SBP accounted for 12.2% of the variability in SBP change, F(1,53) = 7.33, p = 0.009. Adding treatment condition to the model did not explain additional variance in change in daytime ambulatory SBP, ΔR2 = .03, F(1,52) = 2.06, p = 0.157. The 3.1 mm Hg drop in daytime ambulatory SBP in the MBSR treatment condition was not appreciably larger than the 1.5 mm Hg decrease observed for the PMR group. For sleeping ambulatory SBP, pretest ambulatory BP explained 7.5% of the variance in change in SBP, F(1,53) = 4.31, p = 0.043. Adding treatment group to the model did not explain additional variance in sleeping ambulatory SBP, ΔR2 = .04, F(1,51) = 2.38, p = 0.129. The 2.3 mm Hg decrease in sleeping ambulatory SBP observed in the MBSR treatment group did not exceed the 0.8 mm Hg decrease in the PMR group. For ambulatory SBP, completers analyses were not appreciably different from intent-to-treat analyses.
For change in daytime ambulatory DBP, pretest BP accounted for 1% of the variability in DBP change, F(1,53) = 0.52, p = 0.476. No additional variance was explained by adding treatment condition to the model, ΔR2 < .001, F(1,52) = 0.07, p = 0.795. The 1.4 mm Hg drop in daytime ambulatory DBP in the MBSR treatment condition was not smaller than the 2.2 mm Hg decrease observed for participants randomized to PMR. For sleeping ambulatory DBP, pretest BP explained 2% of the variance in change in DBP, F(1,53) = 1.16, p = 0.286. Adding treatment group explain no additional variance in sleeping ambulatory DSBP, ΔR2 = .03, F(1,52) = 1.55, p = 0.218. The 1.7 mm Hg decrease in sleeping ambulatory DBP among patients treated with MBSR was not larger than the 0.6 mm Hg decrease observed in the PMR group. For ambulatory DBP, completers analyses were not appreciably different from intent-to-treat analyses.
Discussion
MBSR is a popular practice used by the public and is claimed to treat stress-related high BP. The primary finding from this randomized trial is that MBSR is effective in lowering elevated BP compared to an active control, and results show decreases in clinic SBP and DBP in prehypertensive individuals. The magnitude of reduction in BP was similar to those reported in a recent meta-analysis of TM (13), and similar to the difference in BP reductions between the active and control treatment groups in the PREMIER trial of comprehensive lifestyle modification for high BP (23). BP changes of this magnitude have been shown to be of public health importance and, if sustained, may lead to reductions in MI, stroke, and CV death (24). Exploratory examinations of the consistency of BP changes suggested that a few outliers did not account for clinic BP differences between groups. However, effects were limited to clinic BP and were not found for ambulatory BP. Interestingly, the HARMONY trial also reported null results for ambulatory BP (25), so our results are consistent with their findings. Whether null results for ambulatory BP were due to white-coat hypertension (26), the contribution of behavioral factors to ambulatory BP (e.g., activity patterns), or other influences cannot be derived from this study. One intriguing possibility is that patients were more able to apply the principles learned in the intervention during seated resting BP assessments in a controlled room than they were when going about their daily lives. Although patients were not coached to meditate or relax during the assessments, they were instructed to apply the principles of relaxation and mindfulness meditation broadly to their lives. It would also have been possible for patients to use relaxation by recall and mindfulness meditation during the waking ambulatory BP measurements, so this may not fully explain why the results for clinic and ambulatory BP were discrepant.
Our results provide evidence that MBSR, when added to lifestyle modification advice, may be an appropriate complementary treatment for BP in the prehypertensive range. Given that patients who desire to avoid or delay antihypertensive medication use may prefer controlling elevated BP with non-pharmacologic interventions, such as lifestyle changes and stress-management approaches, MBSR was shown to hold promise in this regard. When used with otherwise healthy patients with BP in the prehypertensive range, employing MBSR does not contradict treatment recommendations and could prove useful for this highly prevalent condition that is often poorly controlled. Patients with hypertension often require multiple pharmacologic agents and even then frequently do not achieve goal BP levels (2). MBSR could potentially be an important nonpharmacologic adjunctive treatment for these individuals as well, decreasing polypharmacy and/or improving BP control; these hypotheses require additional study.
Strengths and Limitations
Despite much talk in the lay press, prospective and randomized controlled trials of complementary medicine techniques are scarce. To our knowledge, this and the HARMONY trial (25) were the first randomized controlled trials of MBSR in individuals with elevated BP. This trial employed an active (vs. wait list) control, which provided a stringent test of the MBSR intervention. A recent systematic review of clinical trials of mindfulness-based treatments (27) argued that the lack of an active control group is a limitation of much MBSR research suggested that evaluations of MBSR use an active treatment as a comparison condition. Since the completion of this study, an active control intervention has been created and validated for comparison with MBSR (28). For this trial, the PMR control intervention was chosen because, although it is not considered an effective treatment for high BP, it was a very credible placebo. That is, to the patients PMR appeared to be a bona-fide treatment for high BP. Furthermore, PMR could be matched with the MBSR treatment for therapist contact hours and homework. Both MBSR and PMR were well-tolerated by patients. Treatment fidelity and self-reported compliance were high. Thus, PMR and MBSR were procedurally similar on a superficial level, although there are differences in the treatments. PMR is designed to achieve a relaxation response, which is a state that may not persist beyond the relaxation exercises. PMR does not specifically address adopting a way of life that may improve adherence to health behavior changes, whereas MBSR does (e.g., mindful eating). These speculations cannot be confirmed in the current study, but future research may be able to identify the mechanistic differences that affect blood pressure.
Limitations of this intervention include the modest sample size, high dropout rates, questionable validity of the homework measures, the inclusion of non-protocol participants, and the current lack of long term follow up. With respect to the dropout rates, 75% of the patients in the MBSR condition finished the post-treatment assessment, which is at the low end of reported completion rates (although a couple studies with 40%+ dropout have been reported) (27). Future studies may be more feasible if conducted at centers with more clinical capacity, as scheduling treatment groups at mutually convenient times was a challenge. With respect to the homework measures, not all participants consistently remembered to turn in their homework, and self-report logs are not necessarily valid. Future studies may benefit from including experience sampling methodologies that measure homework completion on an ongoing basis. With respect to non-protocol participants, a desire to have larger and ecologically valid treatment groups was balanced against the possibility that including participants who were not enrolled or randomized and who did not complete the study BP assessments may have changed the character of the groups in some way. Finally, the lack of a follow-up precludes any conclusions about sustained effects of MBSR on BP. Future trials should investigate more long-term effects of MBSR on BP.
No conclusions about the ability of meditation to prevent hypertension can be drawn from this design, as firm conclusion would require prevention trials with incident hypertension as the primary outcome. In addition, the mechanism whereby MBSR reduced BP was not determined. MBSR may reduce BP by reducing stress, altering sympathetic nervous system activity, altering hemodynamic regulation of BP, or improving compliance with lifestyle modification advice. For example, to the extent that patients cultivated a mindful approach to daily living, they may have been more able to monitor and control their food and alcohol intake and their exercise habits. This is an important possibility, and evidence that meditation reduces BP should not be taken as a recommendation to neglect needed health behavior changes (e.g., exercise, diet). However, these limitations were consistent with the pilot-and-feasibility nature of the study, which should be followed by larger trials addressing these concerns.
The MBSR program was initially developed and applied in behavioral medicine settings as an adjunctive therapy for patients with a wide range of chronic pain and stress-related disorders (29). Our patients were broadly representative of individuals in the community and recruited via a variety of methods. Thus, they were not recruited from a hospital setting and were enrolled on the basis of being otherwise “healthy” (i.e., by self-report) adults with unmedicated prehypertension. An attempt was made to implement MBSR as it was designed, with the exception of the all-day (8-hour) intensive mindfulness retreat that typically occurs in the sixth week of treatment. The 2.5-hour weekly group sessions included instruction and practice in mindfulness meditation skills along with discussion of stress, coping, and homework assignments. Whether this duration of treatment is necessary for BP reduction is not known, and for comparison, the trial of meditation conducted with adolescents required only 10 minutes of daily meditation in school and at home to achieve BP reductions. Thus, it is possible that a shortened protocol could prove effective, while improving feasibility of larger trials by reducing patient burden.
It was only possible to able to evaluate what happens to BP after patients were taught MBSR. Although patients in both the MBSR and PMR conditions were taught to use their stress management skills to cope with daily life, the extent to which these skills and practices were adopted by patients as lasting lifestyle changes was not evaluated. The possible effects on BP of longer-term personal meditation practices could not be evaluated. That is, MBSR may be more likely to reduce BP for those patients who effectively integrate it into their lives over a long period of time.
Conclusions
The primary finding from this small randomized trial is that MBSR is more effective in lowering elevated BP than an active control and resulted in significant decreases in SBP and DBP in prehypertensive individuals, but for clinic BP only. If sustained, reductions in BP could prove important for health outcomes, but future research is necessary to evaluate these questions. The magnitude of change in BP is similar to that reported in meta-analyses of TM. This was one of the first prospective randomized trials of MBSR as a nonpharmacologic treatment for elevated BP. MBSR could prove to be an adjunct to individuals with poorly controlled BP and could potentially decrease polypharmacy and/or improve BP control, a possibility which merits additional study. Future research should also focus on whether MBSR-related BP reductions can be sustained.
Acknowledgments
Source of Funding:
This research was supported by 1R21AT002698-01A2 from the National Center for Complementary and Alternative Medicine, NIH.
Glossary
Abbreviations
- AHA
American Heart Association
- AHRQ
agency for healthcare and research quality
- BP
blood pressure
- DASH
dietary approaches to stop hypertension
- DBP
diastolic blood pressure
- MBSR
mindfulness-based stress reduction
- PMR
progressive muscle relaxation training
- SBP
systolic blood pressure
- TM
transcendental meditation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: None declared.
Author contributions:
Drs. Hughes and Fresco served as co-principal investigators of this trial, had full access to all of the data, and take responsibility for the integrity of the data and the accuracy of the data analyses. They were responsible for study concept and design, acquisition of data, analysis of data, and drafting of the manuscript.
Rodney Myerscough served as the trial therapist, delivering both group treatments, and also aided in study concept and design and critical revision of the manuscript.
Manfred van Dulmen served as the statistical consultant for this trial, and was involved in study design including power analyses and the data analytic strategy.
Linda E. Carlson served as a consultant on this study and contributed to study concept and design, as well as treatment fidelity ratings and critical revision of the manuscript.
Richard Josephson was the medical director of this clinical trial and was involved in study concept and design, study supervision, and critical revision of the manuscript.
Additional contributions:
We wish to thank the Data Safety and Monitoring Board chaired by Patrick Palmieri, and the following individuals who made significant contributions to the work but who are not authors: Lawrence J. Appel, MD, Kate Guerini, BA, James Rosneck, RN, MS, Andrea Vest, BA, and Donna Waechter, Ph.D.
Reference List
- 1.American Heart Association. Heart Disease and Stroke Statistics - 2004 Update. Dallas, TX: American Heart Association; 2003. [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JLJ, Jones DW, Materson BJ, Oparil S, Wright JTJ, Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA : the journal of the American Medical Association. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 3.Barnes VA, Davis HC, Murzynowski JB, Treiber FA. Impact of Meditation on Resting and Ambulatory Blood Pressure and Heart Rate in Youth. Psychosom Med. 2004;66(6):909–914. doi: 10.1097/01.psy.0000145902.91749.35. [DOI] [PubMed] [Google Scholar]
- 4.Brook RD, Appel LJ, Rubenfire M, Ogedegbe G, Bisognano JD, Elliott WJ, Fuchs FD, Hughes JW, Lackland DT, Staffileno BA, Townsend RR, Rajagopalan S. Beyond Medications and Diet: Alternative Approaches to Lowering Blood Pressure: A Scientific Statement From the American Heart Association. Hypertension. 2013 doi: 10.1161/HYP.0b013e318293645f. [DOI] [PubMed] [Google Scholar]
- 5.Linden W, Lenz JW, Con AH. Individualized stress management for primary hypertension: a randomized trial. Arch Intern Med. 2001;161(8):1071–1080. doi: 10.1001/archinte.161.8.1071. [DOI] [PubMed] [Google Scholar]
- 6.Patel C, Marmot MG, Terry DJ, Carruthers M, Hunt B, Patel M. Trial of relaxation in reducing coronary risk: four year follow up. British medical journal (Clinical research ed) 1985;290(6475):1103–1106. doi: 10.1136/bmj.290.6475.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel C, Marmot MG, Terry DJ. Controlled trial of biofeedback-aided behavioural methods in reducing mild hypertension. British medical journal (Clinical research ed) 1981;282(6281):2005–2008. doi: 10.1136/bmj.282.6281.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schneider R, Alexander CN, Staggers F, Orme-Johnson D, Rainforth M, Salerno J, Castillo-Richmond A, Barnes V, Nidich S. Effects of Stress Reduction on Hypertension in African Americans: A Randomized Controlled Trial over One Year. Circulation. 2003;108(Supplement IV):IV-722. [Google Scholar]
- 9.Spence JD, Barnett PA, Linden W, Ramsden V, Taenzer P. Lifestyle modifications to prevent and control hypertension. 7. Recommendations on stress management. Canadian Hypertension Society, Canadian Coalition for High Blood Pressure Prevention and Control, Laboratory Centre for Disease Control at Health Canada, Heart and Stroke Foundation of Canada. CMAJ : Canadian Medical Association journal = journal de lAssociation medicale canadienne. 1999;160(9 Suppl):S46–S50. [PMC free article] [PubMed] [Google Scholar]
- 10.Schneider RH, Staggers F, Alxander CN, Sheppard W, Rainforth M, Kondwani K, Smith S, King CG. A randomised controlled trial of stress reduction for hypertension in older African Americans. Hypertension. 1995;26(5):820–827. doi: 10.1161/01.hyp.26.5.820. [DOI] [PubMed] [Google Scholar]
- 11.Eisenberg DM, Delbanco TL, Berkey CS, Kaptchuk TJ, Kupelnick B, Kuhl J, Chalmers TC. Cognitive behavioral techniques for hypertension: are they effective? Annals of internal medicine. 1993;118(12):964–972. doi: 10.7326/0003-4819-118-12-199306150-00009. [DOI] [PubMed] [Google Scholar]
- 12.Linden W, Chambers L. Clinical effectiveness of non-drug treatment for hypertension: A meta-analysis. Annals of Behavioral Medicine. 1994;16(1):35–45. [Google Scholar]
- 13.Rainforth MV, Schneider RH, Nidich SI, Gaylord-King C, Salerno JW, Anderson JW. Stress reduction programs in patients with elevated blood pressure: a systematic review and meta-analysis. Curr Hypertens Rep. 2007;9(6):520–528. doi: 10.1007/s11906-007-0094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaufmann PG, Jacob RG, Ewart CK, Chesney MA, Muenz LR, Doub N, Mercer W. Hypertension Intervention Pooling Project. Health psychology : official journal of the Division of Health Psychology American Psychological Association. 1988;7(Suppl):209–224. doi: 10.1037/0278-6133.7.Suppl.209. [DOI] [PubMed] [Google Scholar]
- 15.Ospina MB, Bond TK, Karkahah M, Tjosvold L, Vandermeer B, Liang Y, Bialy L, Hooton N, Buscemi N, Dryden DM, Klassen TP. AHRQ Publication No. 07-E010. Rockville, MD: Agency for Healthcare Research and Quality; 2007. Meditation Practices for Health: State of the Research. Evidence Report/Technology Assessment No. 155. [PMC free article] [PubMed] [Google Scholar]
- 16.Julius S. Treatment of Borderline (Nonsustained) Hypertension. In: Izzo JLJ, Black HR, editors. Hypertension Primer. 3rd ed. Dallas: American Heart Association; 2003. pp. 449–452. [Google Scholar]
- 17.Julius S. The blood pressure seeking properties of the central nervous system. Journal of hypertension. 1988;6(3):177–185. doi: 10.1097/00004872-198803000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Bernstein DA, Borkovec TD, Hazlett-Stevens H. New Directions in Progressive Relaxation Training: A Guidebook for Helping Professionals. Westport, CT: Praeger Publishers; 2000. [Google Scholar]
- 19.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves JW, Hill MN, Jones DH, Kurtz T, Sheps SG, Roccella EJ. Recommendations for blood pressure measurement in humans: an AHA scientific statement from the Council on High Blood Pressure Research Professional and Public Education Subcommittee. Journal Of Clinical Hypertension (Greenwich, Conn) 2005;7(2):102–109. doi: 10.1111/j.1524-6175.2005.04377.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O'Brien E. Demise of the mercury sphygmomanometer and the dawning of a new era in blood pressure measurement. Blood Pressure Monitoring. 2003;8(1):19–21. doi: 10.1097/01.mbp.0000057012.67622.de. [DOI] [PubMed] [Google Scholar]
- 21.O'Brien E, Waeber B, Parati G, Staessen J, Myers MG. Blood pressure measuring devices: recommendations of the European Society of Hypertension. BMJ (Clinical Research Ed ) 2001;322(7285):531–536. doi: 10.1136/bmj.322.7285.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Winnicki M, Canali C, Mormino P, Palatini P. Ambulatory blood pressure monitoring editing criteria: is standardization needed? Hypertension and Ambulatory Recording Venetia Study (HARVEST) Group, Italy. American journal of hypertension : journal of the American Society of Hypertension. 1997;10(4 Pt 1):419–427. [PubMed] [Google Scholar]
- 23.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin PH, Svetkey LP, Stedman SW, Young DR. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA : the journal of the American Medical Association. 2003;289(16):2083–2093. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 24.Whelton PK, He J, Appel LJ, Cutler JA, Havas S, Kotchen TA, Roccella EJ, Stout R, Vallbona C, Winston MC, Karimbakas J. Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA: The Journal Of The American Medical Association. 2002;288(15):1882–1888. doi: 10.1001/jama.288.15.1882. [DOI] [PubMed] [Google Scholar]
- 25.Blom K, How M, Dai M, Baker B, Irvine J, Abbey S, Abramson BL, Myers M, Perkins N, Tobe SW. Hypertension Analysis of stress Reduction using Mindfulness meditatiON and Yoga (The HARMONY Study): study protocol of a randomised control trial. BMJ Open. 2012;2(2):e000848. doi: 10.1136/bmjopen-2012-000848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pickering TG. White coat hypertension. Current opinion in nephrology and hypertension. 1996;5(2):192–198. doi: 10.1097/00041552-199603000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Fjorback LO, Arendt M, Ornbol E, Fink P, Walach H. Mindfulness-based stress reduction and mindfulness-based cognitive therapy: a systematic review of randomized controlled trials. Acta Psychiatrica Scandinavica. 2011;124(2):102–119. doi: 10.1111/j.1600-0447.2011.01704.x. [DOI] [PubMed] [Google Scholar]
- 28.MacCoon DG, Imel ZE, Rosenkranz MA, Sheftel JG, Weng HY, Sullivan JC, Bonus KA, Stoney CM, Salomons TV, Davidson RJ, Lutz A. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behav Res Ther. 2012;50(1):3–12. doi: 10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. General Hospital Psychiatry. 1982;4(1):33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]


