Abstract
Background
The measure of unmet need relies on women’s reported fertility desires; previous research has demonstrated that fertility desires may be fluid and not firm.
Study design
Our study uses recently collected longitudinal data from four cities in Uttar Pradesh India to examine whether women’s fertility desires and family planning (FP) use at baseline predict pregnancy/birth experience in the two-year follow-up period.
Results
Multivariate models demonstrate that women who were using any method of FP and reported an intention to stop childbearing were the least likely to experience a pregnancy/birth in the two-year follow-up period. The stated desire to delay childbearing, whether or not the woman was using FP did not distinguish pregnancy/birth experience. Ninety- two percent of pregnancies/births over the follow-up period were considered “wanted then” suggesting post hoc rationalization of the pregnancy/birth even among those women who reported a desire to stop childbearing two years earlier.
Conclusions
More nuanced assessments of fertility intentions may be needed to adequately gauge latent family planning needs. Non-users of FP may be ambivalent about future childbearing and the timing of future births; these women may not have an unmet need for FP as typically defined.
Introduction
A common indicator used to measure a population’s need for family planning (FP) services is “unmet need.” This indicator has been defined in the global FP world to be the percentage of sexually active, fecund women who say they want to delay or stop childbearing and are not using any form of FP. Recent estimates of unmet need demonstrate that the proportion of women with an unmet need varies cross-nationally with the highest unmet need in sub-Saharan Africa and slightly lower unmet need in Asia where current FP use is higher.1 Family planning offers a number of health benefits through reduction of unintended (mistimed and unwanted) pregnancies.2–4 These benefits include reduced spread of HIV to newborns;5 reduced maternal mortality and morbidity;6,7 reduced neonatal, infant, and child mortality;8,9 reduced recourse to often unsafe abortion;6,10 and improved education and employment opportunities for women (and men) who are able to delay initiation of childbearing.6
Although unmet need is a useful measure at the policy level, it is less useful at the individual level because it relies on reported fertility desires that have been found to often be fluid, fluctuating in response to changing individual, relationship, and community influences.3,11,12 The fluidity of fertility intentions could partially explain documented inconsistencies between women’s stated pregnancy intentions and subsequent childbearing experiences.13 For example, a 1970s French study demonstrated that among women who intended a birth in the future, 73% had a birth in the five-year follow-up period.12 More notably, among those women who did not intend to have any more children, about 20% had a birth in the five-year follow-up period. Similarly, longitudinal studies from Nigeria and Morocco demonstrated that 16% and 29%, respectively, of women who reported that they did not want any more children had a birth in the two-year follow-up period.11,14 Likewise, a study from Bangladesh found that 17% of couples that did not want any more children had a child in the five-year follow-up period.15 Furthermore, a study from India, the site of the current study, showed that 61% of fecund women who reported that they did not want any more children experienced a child in the 6–7 year follow-up period; this high percentage may reflect the longer follow-up period or fatalistic views about childbearing in the study context.16 These observed inconsistencies between fertility intentions and childbearing experiences raise questions about the measurement of unmet need.
The gap between reported fertility intentions to avoid or delay pregnancy and actual FP use may reflect the host of well documented cost, access, and cultural barriers impeding uptake and sustained use of effective FP.9,17–19 In addition to these barriers to FP use, ambivalent fertility desires must also be considered as part of discussions around measuring unmet FP needs.20,21 A recent study from Indonesia demonstrated that women who were ambivalent about future childbearing, that is, they reported that they did not know whether they desired another child, had birth experiences in the four-year follow-up period similar to women who reported that they did not want any more children.22 In particular, 33% of ambivalent women had a birth in the four-year follow-up compared to 29% among women who did not want a child and 57% among women who wanted more children. Conversely, in terms of FP use, ambivalent women were more similar to the women who wanted more children; FP use was not predictive of ambivalent women’s subsequent birth outcomes.22 Where pregnancy ambivalence is common, measurement of unmet need may be over (or under) estimated given that it relies on fertility desires as a key component of its calculation.
Our study contributes to prior discussions of the measurement of unmet need by examining fertility desires and subsequent childbearing behaviors using novel data from a two-year follow-up study among urban women from Uttar Pradesh, India. Our focus on urban women in India contributes to prior longitudinal research from India that included women from rural areas.16,23 The objectives of the study are twofold. First, we determine whether baseline fertility intentions and FP use are associated with women’s pregnancy experience over the two-year follow-up period. Second, we determine the intentionality of pregnancies at follow-up to determine whether baseline fertility intentions are associated with the reported intentionality of pregnancies experienced in the two-year follow-up period. The hypothesis is that if fertility desires are firm, those women who reported at baseline that they did not want any more children would be more likely to report the pregnancy/birth during the follow-up period as unintended (wanted later or did not want) than those women who reported that they wanted more children at baseline. Moreover, we expect that those women who were using FP at baseline would be more likely to report the pregnancy as unintended. The results provide insights for measuring unmet need through examination of the reliability of stated fertility desires and the relationship between fertility intentions, FP use, and pregnancy experience.
Materials and Methods
Data for this study come from four cities (Agra, Aligarh, Allahabad, and Gorakhpur) in Uttar Pradesh, India. The data were collected by the Measurement, Learning & Evaluation project as part of mid-term data collection for the evaluation of the Urban Health Initiative, implemented by FHI360 with funding from the Bill & Melinda Gates Foundation. Baseline data were collected in early 2010 from a representative sample of 17,643 married women from six cities; the baseline survey has been described previously.24 In 2012, mid-term data were only collected from half of the baseline sample of women from the four initial intervention cities where multi-faceted interventions were introduced starting in March, 2010. To include a representative sample at mid-term, we randomly selected a sample of baseline primary sampling units (PSU) and sought to interview all baseline women in selected PSU. Weights were used to adjust for non-response and oversampling of slums. At mid-term, all eligible women were approached and asked to provide consent to be interviewed; interviews took place in or around the women’s homes or in another location when the woman was identified outside her home. Female interviewers asked women questions about their fertility and FP experiences since the baseline survey. All study procedures were approved by the Institutional Review Boards of the Futures Group in India and by the University of North Carolina at Chapel Hill. A total of 6,752 women were eligible for interview at mid-term; 5,790 of these women were successfully interviewed at mid-term (85·8% response rate).
The study sample is limited to participants who were fecund and non-sterilized at baseline. Infecundability was self-reported either as “can’t get pregnant”, hysterectomy, or menopausal. Sterilization included that the woman or her husband was sterilized. We also excluded women who were pregnant at the time of the baseline interview because it is not clear that their future fertility desires reflect a subsequent pregnancy and all of these women were non-users of FP at baseline. The final analysis sample includes 3,551 women (weighted n=3,808) with complete information on the variables of interest (see Table 1).
Table 1.
Percentage distribution of respondents who were selected for interviewed in 2012, by selected background characteristics according to interview status
| Percent interviewed | Not interviewed* | Interviewed* | Analysis sample** | |
|---|---|---|---|---|
|
| ||||
| City | ||||
| Agra | 83·9 | 34·6 | 34·1 | 33·6 |
| Aligarh | 84·3 | 18·3 | 16·4 | 18·9 |
| Allahabad | 87·9 | 26·9 | 28·7 | 27·6 |
| Gorakhpur | 87·3 | 20·2 | 20·8 | 19·9 |
| Age Group | ||||
| 15–24 | 80·6 | 20·3 | 15·7 | 19·9 |
| 25–29 | 82·9 | 26·1 | 18·6 | 24·0 |
| 30–34 | 86·8 | 18·2 | 19·9 | 23·6 |
| 35–39 | 86·6 | 18·0 | 18·5 | 16·5 |
| 40+ | 90·3 | 17·4 | 27·3 | 15·9 |
| Education | ||||
| None | 84·7 | 34·4 | 31·1 | 26·1 |
| 1–11 years | 87·8 | 28·1 | 35·0 | 32·3 |
| 12+ years | 84·7 | 37·5 | 33·9 | 41·6 |
| Missing | 100·0 | 0·0 | 0·1 | excluded |
| Religion | ||||
| Hindu/othera | 86·0 | 82·5 | 84·3 | 82·7 |
| Muslim | 84·9 | 17·5 | 15·7 | 17·3 |
| Wealth group | ||||
| Poorest | 84·6 | 24·1 | 22·2 | 22·2 |
| Poor | 86·5 | 20·1 | 21·4 | 21·5 |
| Medium | 85·3 | 21·6 | 20·0 | 19·5 |
| Rich | 86·6 | 19·6 | 19·1 | 18·5 |
| Richest | 86·0 | 14·7 | 17·3 | 18·3 |
| Baseline fertility intentions | ||||
| Wants now/wants, DK when/DK | 79·4 | 13·0 | 8·8 | 14·3 |
| Wants in 2+ years | 82·3 | 11·0 | 10·1 | 16·5 |
| Does not want | 87·2 | 40·6 | 42·3 | 69·1 |
| Sterilized | 87·5 | 19·5 | 23·8 | excluded |
| Infecund | 89·6 | 6·6 | 9·1 | excluded |
| Pregnant | 80·4 | 9·3 | 5·9 | excluded |
| Family planning use at baseline | ||||
| No | 83·2 | 43·0 | 33·9 | 30·9 |
| Yes | 87·3 | 57·0 | 66·1 | 69·1 |
|
| ||||
| Total | 85·8 | 100·0 | 100·0 | 100·0 |
| (Unweighted N) | 6752 | 962 | 5790 | 3551 |
Notes: DK – don’t know;
percentages are weighted;
Excludes women that were sterilized, infecund or pregnant at baseline;
Other religions constitute less than 1% of the population, and therefore are grouped with Hindu.
The primary outcome is whether the woman was currently pregnant at mid-term or had experienced a birth since January, 2010 (i.e., the baseline survey). At mid-term, all women who were currently pregnant or who had a birth were asked whether the pregnancy/birth came at the right time, earlier than desired, or was not wanted at all. This question was used to categorize the intentionality of the pregnancy/birth as: wanted then, wanted later, and not wanted. For women who had two births or pregnancies since baseline (n=50), we focused on the most recent event for this analysis.
Key independent variables are the baseline fertility intentions and baseline FP use. All women were asked at baseline if they wanted any more children. Women reporting ‘yes’ were asked when they wanted the next child. Using these two questions, women were classified as: wants now/wants, but not sure when/don’t know; wants in 2+ years; and does not want. The 11 women who were undecided about future childbearing and the three women who had missing information on future desires at baseline were grouped with ‘wants now’, per convention.3 At baseline, women were also asked about current FP use. We classified women into two groups: using any FP method (includes: oral contraceptive pills, intrauterine device, injections, condoms, emergency contraception, spermicide and traditional methods) and not using any method. This is the standard approach used to determine unmet need – i.e., “using any method”.1
The analysis controls for demographic variables associated with fertility experience and FP use including age, education, religion, wealth, and city. Multivariate models included interaction terms between FP use and fertility intentions. To help interpret interactions, we present the predicted probability of a pregnancy/birth for women using and not using any FP method by baseline fertility intentions. Predicted probabilities are calculated by determining the percentage of women who would experience a pregnancy/birth based on the model results under various scenarios holding all other variables constant. All analyses use baseline weights and adjust for the clustering in the data using Stata version 12 svy commands.
Results
Table 1 presents the percent distribution of background characteristics by interview status of the 6,752 women that were selected for re-interview in 2012. At mid-term, data were collected from 85·8% of the eligible mid-term sample. Across the demographic characteristics, more than 80% of the sample was re-interviewed. Notably, we were able to interview a higher percentage of the older women than the younger women; this might reflect greater mobility of younger women/couples. Correspondingly, comparison of the interviewed and not-interviewed samples demonstrates that the re-interviewed sample of women is more likely to be sterilized, infecund, and using FP, all factors associated with older age.24 A smaller percentage of interviewed women reported at baseline that they wanted a child now, wanted another child but don’t know when or didn’t know if they wanted another child; this again corresponds to attrition of the younger women.
Table 1 also presents the demographic and reproductive health indicators of the analysis sample. The majority of the women (69%) reported at baseline that they did not want any more children. There was high concordance between women’s desires and the perceived desires of their partners (data not shown); accordingly, perceived partners’ desires are not included in the analyses reported here. Sixty-nine percent of the analysis sample reported at baseline that they were currently using any FP method.
Table 2a provides the cross-tabulation between women’s baseline FP use and fertility intentions. Among women who wanted a pregnancy soon, only 25% were using any FP method; this percentage was higher among women who wanted to delay childbearing 2+ years (73%) and among women who did not want any more children (77%). Standard calculations of unmet need would classify these married women who report a desire to delay childbearing 2+ years or do not want any more children and are not using FP as having an unmet need; one fifth of the sample (20%) is in these categories and has an unmet need (not shown). Notably, a third (32·2%) of the sample reporting a desire for no more children at baseline was using traditional methods and a similar percentage (30·3%) was using condoms (not shown). Table 2b presents cross tabulations of pregnancy/birth experience between baseline and mid-term by baseline FP use and fertility intentions. Overall, about one-fifth (22%) of the sample experienced a pregnancy/birth; this percentage is significantly higher among non-users of FP at baseline (36%) as compared to users of any method of FP (16%). Among women who wanted a child soon, about 46% had a pregnancy/birth between baseline and mid-term. Among women who wanted to delay childbearing, a slightly higher percentage (51%) experienced a pregnancy/birth. As expected, a lower percentage (10%) of women who said they did not want any more children experienced a pregnancy/birth between baseline and mid-term.
Table 2a.
Cross tabulation between women’s fertility desires and family planning use at baseline among women not sterilized, infecund or pregnant at baseline, Uttar Pradesh, India
| Baseline any method family planning use | ||||
|---|---|---|---|---|
|
| ||||
| Non-user | User | Total | Weighted N | |
|
| ||||
| Baseline fertility intentions | ||||
| Wants now/wants don’t know when/don’t know | 74·6% | 25·4% | 100% | 546 |
| Wants in 2+ years | 26·8% | 73·2% | 100% | 630 |
| Does not want | 22·8% | 77·2%*** | 100% | 2632 |
|
| ||||
| Total | 30·9% | 69·1% | 100% | 3808 |
p ≤ 0·001
Table 2b.
Cross tabulation between women’s pregnancy experience between baseline and midterm and baseline fertility intentions and baseline family planning use among women not sterilized, infecund or pregnant at baseline, Uttar Pradesh, India
| Experienced Pregnancy/ birth between baseline and midterm | No pregnancy/ birth between baseline and midterm | Total | Weighted N | |
|---|---|---|---|---|
|
| ||||
| Family planning use at baseline | ||||
| No | 36·1% | 63·9% | 100% | 1177 |
| Yes | 15·9% | 84·1%*** | 100% | 2631 |
|
| ||||
| Baseline fertility intentions | ||||
| Wants now/wants don’t know when/don’t know | 45·9% | 54·1% | 100% | 546 |
| Wants in 2+ years | 50·6% | 49·4% | 100% | 630 |
| Does not want | 10·4% | 89·6%*** | 100% | 2632 |
|
| ||||
| Total | 22·2% | 77·8% | 100% | 3808 |
p ≤ 0·001
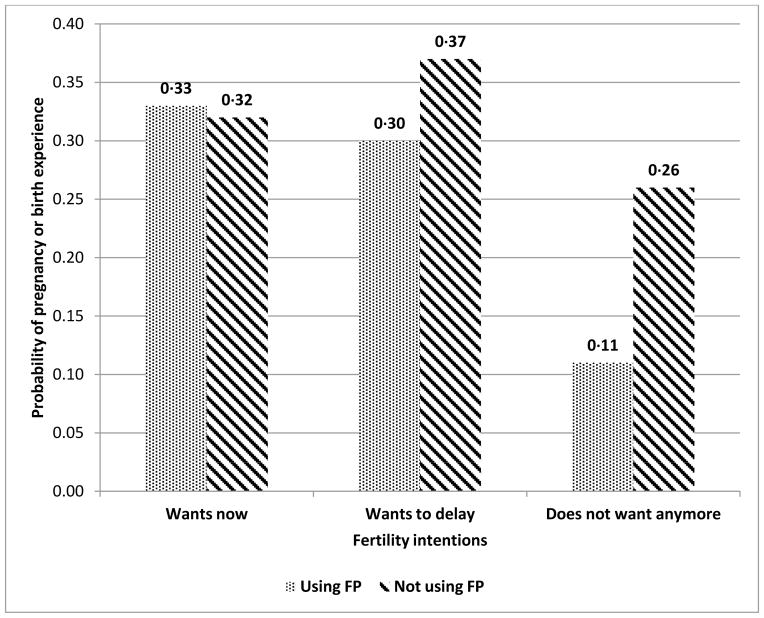
Table 3 presents the multivariate odds ratios and 95% confidence intervals of whether a woman experienced a pregnancy/birth between baseline and mid-term based on two models: Model 1 without interactions and Model 2 including interactions between FP use and fertility intentions. Model 1 demonstrates that women who do not want any(more) children at baseline were significantly less likely to have experienced a pregnancy/birth between baseline and follow-up, controlling for demographic factors. In addition, women who were using FP were significantly less likely to have a pregnancy/birth between baseline and mid-term. Model 2 shows that the main effect of FP use is not significant, and the interaction between FP use and a desire to stop childbearing is significant. Figure 1 presents predicted probabilities of pregnancy/birth experience by FP use and fertility intentions. Table 3 and Figure 1 show that, holding all other variables constant, there is little difference in pregnancy/birth experience among women who want a child now by whether or not they are using FP (predicted probability about 0·33). Among women who want to delay childbearing, those women not using FP at baseline are slightly more likely to become pregnant than women who were using FP. The important difference is for women who do not want any(more) children. Among women who want to avoid childbearing and are using FP, the predicted probability of a pregnancy/birth is 0·11 whereas among women who want to limit childbearing and are not using FP, the predicted probability of a pregnancy/birth is 0·26. Also presented in Table 3 are the demographic factors; all factors showed the expected associations with pregnancy/birth experience.
Table 3.
Multivariate regression of association between baseline family planning use and baseline fertility intentions on pregnancy/birth experience between baseline and midterm among women not sterilized, infecund or pregnant at baseline, Uttar Pradesh, India (n=3808 - weighted)
| Characteristic | Model 1 Odds Ratio (95% CI) |
Model 2 Odds Ratio (95% CI) |
|---|---|---|
|
| ||
| City | ||
| Agra | 1·23 (0·85–1·78) | 1·22 (0·84–1·76) |
| Aligarh | 1·15 (0·77–1·72) | 1·13 (0·76–1·69) |
| Allahabad | 0·71 (0·42–1·20) | 0·70 (0·42–1·19) |
| Gorakhpur (ref) | 1·00 | 1·00 |
|
| ||
| Age Group | ||
| 15–24 | 20·80 (11·95–36·21)*** | 21·62 (12·02–38·89)*** |
| 25–29 | 10·62 (6·17–18·28)*** | 10·93 (6·19–19·28)*** |
| 30–34 | 4·76 (2·61–8·65)*** | 4·82 (2·58–9·01)*** |
| 35+ (ref) | 1·00 | 1·00 |
|
| ||
| Education | ||
| None | 1·39 (0·87–2·23) | 1·37 (0·86–2·20) |
| 1–11 years | 0·87 (0·64–1·19) | 0·90 (0·66–1·23) |
| 12+ years (ref) | 1·00 | 1·00 |
|
| ||
| Religion | ||
| Hindu/other (ref) | 1·00 | 1·00 |
| Muslim | 1·41 (0·97–2·05)+ | 1·41 (0·97–2·05)+ |
|
| ||
| Wealth group | ||
| Poorest | 0·89 (0·57–1·40) | 0·90 (0·57–1·42) |
| Poor | 0·94 (0·58–1·52) | 0·92 (0·57–1·47) |
| Medium | 1·22 (0·75–2·00) | 1·21 (0·74–1·98) |
| Rich | 0·94 (0·60–1·47) | 0·93 (0·59-·1·46) |
| Richest (ref) | 1·00 | 1·00 |
|
| ||
| Residence | ||
| Slum | 1·34 (1·05–1·71)* | 1·36 (1·06–1·74)* |
| Non-slum | 1·00 | 1·00 |
|
| ||
| Baseline fertility intentions | ||
| Wants now/wants DK when/DK (ref) | 1·00 | 1·00 |
| Wants in 2+ years | 1·37 (0·94–2·01) | 1·27 (0·73–2·21) |
| Does not want | 0·39 (0·28–0·56)*** | 0·65 (0·43–0·99)* |
|
| ||
| Family planning use at baseline | ||
| No (ref) | 1·00 | 1·00 |
| Yes | 0·48 (0·36–0·65)*** | 1·02 (0·53–1·94) |
|
| ||
| Interaction between baseline fertility intentions and baseline FP use | ||
| Using FP and wants to delay | NA | 0·66 (0·28–1·54) |
| Using FP and does not want any more | 0·29 (0·13–0·61)*** | |
Notes: DK: Don’t know; NA – not applicable;
p≤0·10;
p≤0·05;
p ≤ 0·01;
p ≤ 0·001
Figure 1.
Predicted probabilities of pregnancy/birth between baseline and midterm among women not sterilized, infecund or pregnant at baseline in urban Uttar Pradesh, demonstrating interaction between baseline fertility intentions and baseline family planning (FP) use
Table 4 presents findings on whether the recent pregnancy/birth was wanted then, wanted later, or not wanted at all; we relate this intentionality to baseline fertility intentions and FP use. Most women (92%) reported the pregnancy/birth as wanted then, only 6% reported the recent pregnancy/birth as mistimed and less than 2% as unwanted; this is lower than expected given that 69% of women at baseline reported that they did not want any(more) children. This may reflect post-hoc rationalization of a pregnancy/birth. Among women who reported that the pregnancy/birth was wanted then, about one-third had baseline intentions to stop childbearing and another third had baseline intentions to delay; among women who wanted to delay at baseline, this pregnancy/birth may be timed appropriately. Among the few women reporting that the pregnancy/birth was mistimed, 29% reported an intention to stop childbearing at baseline. The differences in fertility intentions at baseline are significant by intentionality of the recent pregnancy/birth. Table 4 also shows that among women who had a pregnancy/birth in the two year period, about half were using a FP method at baseline. The percentage using was significantly higher among the small number of women who reported the pregnancy/birth as mistimed or unwanted.
Table 4.
Bivariate comparison of intentionality of pregnancy/birth between baseline and midterm and intentions and family planning use at baseline among women not sterilized, infecund or pregnant at baseline (n= 843 women who had pregnancy/birth weighted)
| Intentionality of pregnancy/birth between baseline and midterm | ||||
|---|---|---|---|---|
|
| ||||
| Wanted then | Wanted later | Did not want | Total | |
|
| ||||
| Total | 92·1% | 6·3% | 1·6% | 100% |
|
| ||||
| (n=776) | (n=53) | (n=14) | (n=843) | |
|
| ||||
| Baseline fertility intentions | ||||
| Wants now/wants don’t know when/don’t know | 31·6 | 9·1 | 3·6 | 29·7 |
| Wants in 2+ years | 36·4 | 62·1 | 22·1 | 37·8 |
| Does not want | 32·0 | 28·9 | 74·3*** | 32·5 |
|
| ||||
| Total | 100% | 100% | 100% | 100% |
|
| ||||
| Family planning use at baseline | ||||
| No | 52·2 | 29·1 | 29·4 | 50·4 |
| Yes | 47·8 | 70·9 | 70·6** | 49·6 |
|
| ||||
| Total | 100% | 100% | 100% | 100% |
p ≤ 0·01;
p ≤ 0·001
Discussion
These findings are important for understanding the use of unmet need to determine gaps in FP program coverage. In our study context, we found that women who do not want any(more) children and are using any FP method are the least likely to experience a pregnancy/birth in the two-year follow-up period. Moreover, women who do not want any(more) children who are non-users of FP were also less likely to experience a pregnancy/birth in the follow-up period. Conversely, the stated desire to delay childbearing, whether or not the woman was using FP, did not distinguish pregnancy/birth experience from women who wanted a child soon. Further, the overwhelming majority of pregnancies/births were reported as “wanted then,” even among women who reported that they wanted to avoid childbearing at baseline.
Given that about a third of women are using traditional FP methods, our findings suggest that the least motivated users may be willing to accept lower FP effectiveness. Therefore, less motivated users may not adopt a more effective method even if it available/affordable. An alternative explanation might be that women who want to space births and are not using a method (or are using a less effective method) may have barriers to use or are ambivalent toward available spacing methods; this would need to be explored in more detail using qualitative research methods.
Using conventional definitions of unmet need, there appear to be important FP needs in our sample; 20% of non-sterilized, fecund, non-pregnant married women reported a desire to delay or stop childbearing and were not using any FP method. Yet many women apparently have ambivalent fertility desires and report a subsequent pregnancy as intended. Our observation of post-hoc rationalization of pregnancies is a similar finding to those found in Morocco and India.14,23 Targeting ambivalent women with FP may be futile as these women still want to have children and perhaps they are just unclear on the timing of the next child.
In the India context, the typical pattern is to marry early, have 2–4 children and then get sterilized.16,23 The women in our sample who are not sterilized or infecund and thus at risk of a pregnancy over the follow-up period are likely still in a childbearing frame of mind. They may not intend to have a child soon but may also not intend to avoid a child. These women may be ambivalent about future childbearing but also may be ambivalent about using FP.25 Family planning ambivalence can be addressed through programs that clarify details of available FP methods and help to clear up misconceptions about side effects and use indications. Programs should also publicize the benefits of child spacing and promote the use of short-acting methods such as pills, injections, and condoms; pills and injections are rarely used in the urban areas studied.24 Family planning program improvements could help women who have firm desires but are not using a method to delay or avoid subsequent childbearing.
This study is not without limitations. First, we rely on births in the follow-up period. Induced abortions also make up some of the pregnancies women experienced; these were not included in this analysis as they are likely to be under-reported. Another limitation is grouping modern and traditional FP methods. Given that the standard definition of unmet need focuses on any method use, we followed that approach. In analyses not presented, we separated traditional method and modern method users and found similar results (users of either method who wanted to avoid childbearing were less likely to have a pregnancy/birth). Finally, the measure of FP used in this analysis is self-reported and thus could be under (or over) reported by included women.
Using the extent of unmet need to gain policy and financial support for family planning programs is strategically important. That said, it is important to recognize that reports of high unmet need for any family planning and even higher unmet need for modern family planning - recently estimated at 222 million women4 - will over-estimate the true latent demand for family planning given that many women may be ambivalent about future childbearing and may be unlikely to adopt a method (or change from a less effective to a more effective method) as illustrated in these analyses. Our findings are consistent with previous studies that challenge accepted approaches to measuring unmet need and raise the need for more nuanced assessments of fertility intentions.3,26–28 “Desiring” versus “not desiring” pregnancy may be a false dichotomy for many women; fertility intentions likely fall more on a continuum.21,29 Furthermore, the fluidity of fertility intentions in response to fluctuations in personal circumstances also contributes to inconsistencies between stated pregnancy desires, FP behaviors, and pregnancy experience.3,13,30 Family planning programs are unlikely to significantly reduce “unmet need” as calculated by program managers and policy makers if a substantial amount of the non-use represents ambivalence toward pregnancy and/or FP. A more accurate and meaningful assessment of FP program coverage should be based on a more nuanced evaluation of women’s fertility desires, the types of methods they are using, and the consistency of method use. Such refined measures will provide greater clarity on where resources should be invested to ensure that all women, men, and couples are able to meet their immediate and longer-term childbearing intentions.
Acknowledgments
Funding for this work comes from the Bill & Melinda Gates Foundation. This research was also supported by grant, 5 R24 HD050924, Carolina Population Center, awarded to the Carolina Population Center at The University of North Carolina at Chapel Hill by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the funders.
References
- 1.Bradley S, Croft TN, Fishel JD, Westoff CF. Revising unmet need for family planning. Calverton, Maryland, USA: ICF International; 2012. (DHS Analytical Studies No. 25). [Google Scholar]
- 2.Cates W. Family Planning: The essential link to achieving all eight Millennium Development Goals. Contraception. 2010;81:460–461. doi: 10.1016/j.contraception.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 3.Tsui AO, McDonald-Mosley R, Burke AE. Family planning and the burden of unintended pregnancies. Epidemiol Rev. 2010;32:152–174. doi: 10.1093/epirev/mxq012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh S, Darroch JE. Adding It Up: Costs and Benefits of Contraceptive Services—Estimates for 2012. New York: Guttmacher Institute and United Nations Population Fund (UNFPA); 2012. [accessed December 20, 2012]. http://www.guttmacher.org/pubs/AIU-2012-estimates.pdf. [Google Scholar]
- 5.Reynolds HW, Janowitz B, Wilcher R, Cates W. Contraception to prevent HIV-positive births: current contribution and potential cost savings in PEPFAR countries. Sex Transm Infect. 2008;84(Suppl II):ii49–ii53. doi: 10.1136/sti.2008.030049. [DOI] [PubMed] [Google Scholar]
- 6.Singh S, Darroch JE, Ashford LS, Vlassoff M. Adding it Up: The Costs and Benefits of Investing in Family Planning and Maternal and Newborn Health. New York: Guttmacher Institute and United Nations Population Fund (UNFPA); 2009. [accessed December 20, 2012]. http://www.guttmacher.org/pubs/AddingItUp2009.pdf. [Google Scholar]
- 7.Cleland J, Conde-Agudelo A, Peterson H, Ross J, Tsui A. Contraception and health. Lancet. 2012;380:149–56. doi: 10.1016/S0140-6736(12)60609-6. [DOI] [PubMed] [Google Scholar]
- 8.Rutstein SO. Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: evidence from the demographic and health surveys. Int J Gynaecol Obstet. 2005;89 (suppl 1):S7–S24. doi: 10.1016/j.ijgo.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 9.Cleland J, Bernstein S, Ezeh A, Faundes A, Glasier A, Innis J. Family planning: the unfinished agenda. Lancet. 2006;368:1810–1827. doi: 10.1016/S0140-6736(06)69480-4. [DOI] [PubMed] [Google Scholar]
- 10.Sedgh G, Singh S, Shah IH, Åhman E, Henshaw SK, Bankole B. Induced abortion: incidence and trends worldwide from 1995 to 2008. Lancet. 2012;379:625–32. doi: 10.1016/S0140-6736(11)61786-8. [DOI] [PubMed] [Google Scholar]
- 11.Bankole A. Desired fertility and fertility behavior among the Yoruba of Nigeria: a study of couple preferences and subsequent fertility. Popul Stud. 1995;49(2):317–328. [Google Scholar]
- 12.Monier A. Fertility intentions and actual behavior. A longitudinal study: 1974, 1976, 1979. Popul. 1989;44(1):237–259. [PubMed] [Google Scholar]
- 13.Speder Z, Kapitany B. How are time-dependent childbearing Intentions realized? Realization, postponement, abandonment, bringing forward. Eur J Population. 2009;25:503–523. [Google Scholar]
- 14.Bankole A, Westoff C. The consistency and validity of reproductive attitudes: evidence from Morocco. J Biosoc Sci. 1998;30:439–455. doi: 10.1017/s0021932098004398. [DOI] [PubMed] [Google Scholar]
- 15.Gipson JD, Hindin MJ. The effect of husbands’ and wives’ fertility preferences on the likelihood of a subsequent pregnancy, Bangladesh 1998–2003. Popul Stud. 2009;63 (2):135–146. doi: 10.1080/00324720902859372. [DOI] [PubMed] [Google Scholar]
- 16.Roy TK, Ram RF, Nangia P, Saha U, Khan N. Can women’s childbearing and contraceptive intentions predict contraceptive demand? Findings from a longitudinal study in central India. Int Fam Plan Perspect. 2003;29(1):25–31. doi: 10.1363/ifpp.29.025.03. [DOI] [PubMed] [Google Scholar]
- 17.Paul VK, Sachdev HS, Mavalankar D, et al. Reproductive health, and child health and nutrition in India: meeting the challenge. Lancet. 2011;377:332–49. doi: 10.1016/S0140-6736(10)61492-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hubacher D, Mavranezouli I, McGinn E. Unintended pregnancy in sub-Saharan Africa: magnitude of the problem and potential role of contraceptive implants to alleviate it. Contraception. 2008;78:73–78. doi: 10.1016/j.contraception.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 19.Ezeh AC, Kodzi I, Emina J. Reaching the urban poor with family planning services. Stud Fam Plann. 2010;41:109–116. doi: 10.1111/j.1728-4465.2010.00231.x. [DOI] [PubMed] [Google Scholar]
- 20.Campo S, Askelson NM, Spies EL, Losch M. Ambivalence, communication and past use: understanding what influences women’s intentions to use contraceptives. Psychol Health Med. 2012;17(3):356–65. doi: 10.1080/13548506.2011.608432. [DOI] [PubMed] [Google Scholar]
- 21.McQuillan J, Greil AL, Shreffler KM. Pregnancy intentions among women who do not try: Focusing on women who are okay either way. [accessed December 20, 2012];Sociology Department, Faculty Publications. Paper 97. 2010 http://digitalcommons.unl.edu/sociologyfacpub/97.
- 22.Withers MH, Tavrow P, Adinata NA. Do ambivalent women have an unmet need for family planning? A longitudinal study from Bali, Indonesia. Womens Health Issues. 2011;21 (6):444–449. doi: 10.1016/j.whi.2011.04.031. [DOI] [PubMed] [Google Scholar]
- 23.Koenig MA, Acharya K, Singh S, Roy TK. Do current measurement approaches underestimate levels of unwanted childbearing? Evidence from rural India. Popul Stud. 2006;60(3):243–256. doi: 10.1080/00324720600895819. [DOI] [PubMed] [Google Scholar]
- 24.Speizer IS, Nanda P, Achyut P, Pillai G, Guilkey D. Family planning use among urban poor women from six cities of Uttar Pradesh, India. J Urban Health. 2012;89:639–658. doi: 10.1007/s11524-011-9667-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zabin LS. Ambivalent feelings about parenthood may lead to inconsistent contraceptive use—and pregnancy. Fam Plann Perspect. 1999;31 (5):250–251. [PubMed] [Google Scholar]
- 26.Dixon-Mueller R, Germain A. Stalking the elusive “unmet need” for family planning. Stud Fam Plann. 1992;23(5):330–5. [PubMed] [Google Scholar]
- 27.Santelli J, Rochat R, Hatfield-Timajchy K, Gilbert BC, Curtis K. The measurement and meaning of unintended pregnancy. Perspect Sex Reprod Health. 2003;35(2):94–101. doi: 10.1363/3509403. [DOI] [PubMed] [Google Scholar]
- 28.Speizer IS. Using strength of fertility motivations to identify family planning program strategies. Int Fam Plan Perspect. 2006;32(4):185–91. doi: 10.1363/3218506. [DOI] [PubMed] [Google Scholar]
- 29.Bachrach CA, Newcomer S. Intended pregnancies and unintended pregnancies: distinct categories or opposite ends of a continuum? Forum: Contraceptive failure and unintended pregnancy. Fam Plann Perspect. 1999;31(5):251–252. [PubMed] [Google Scholar]
- 30.Jain W. Should Eliminating unmet need for contraception continue to be a program priority? Int Fam Plan Perspect. 1999;25(Supplement):S39–S43. S49. [Google Scholar]