Abstract
Background
Transseptal puncture is a critical step in achieving left atrial (LA) access for a variety of cardiac procedures. Although the mechanical Brockenbrough needle has historically been used for this procedure, a needle employing radiofrequency (RF) energy has more recently been approved for clinical use. We sought to investigate the comparative effectiveness of an RF versus conventional needle for transseptal LA access.
Methods and Results
In this prospective, single‐blinded, controlled trial, 72 patients were randomized in a 1:1 fashion to an RF versus conventional (BRK‐1) transseptal needle. In an intention‐to‐treat analysis, the primary outcome was time required for transseptal LA access. Secondary outcomes included failure of the assigned needle, visible plastic dilator shavings from needle introduction, and any procedural complication. The median transseptal puncture time was 68% shorter using the RF needle compared with the conventional needle (2.3 minutes [interquartile range {IQR}, 1.7 to 3.8 minutes] versus 7.3 minutes [IQR, 2.7 to 14.1 minutes], P=0.005). Failure to achieve transseptal LA access with the assigned needle was less common using the RF versus conventional needle (0/36 [0%] versus 10/36 [27.8%], P<0.001). Plastic shavings were grossly visible after needle advancement through the dilator and sheath in 0 (0%) RF needle cases and 12 (33.3%) conventional needle cases (P<0.001). There were no differences in procedural complications (1/36 [2.8%] versus 1/36 [2.8%]).
Conclusions
Use of an RF needle resulted in shorter time to transseptal LA access, less failure in achieving transseptal LA access, and fewer visible plastic shavings.
Clinical Trial Registration
URL: http://www.clinicaltrials.gov. Unique identifier: NCT01209260.
Keywords: Brockenbrough needle, comparative effectiveness, left atrial access, radiofrequency energy needle, randomized controlled trial, transseptal puncture
Introduction
Transseptal puncture is commonly performed to achieve left atrial (LA) access for a variety of common cardiac procedures, including catheter ablation of atrial fibrillation (AF),1 accessory pathways and ventricular tachycardia,2–3 LA appendage closure,4–5 and mitral valve procedures.6–7 Historically, a conventional Brockenbrough needle has been used to mechanically puncture the fossa ovalis, but adoption of a newer transseptal needle using radiofrequency (RF) energy applied to an insulated blunt‐tipped electrode has increased despite a prospective trial comparing the 2 strategies. Although the conventional needle may provide more immediate tactile feedback and has a longer track record of success, the RF needle may be more effective in cases of an elastic, aneurysmal, or thickened interatrial septum.8 In addition, safety concerns have been raised as more plastic particle shavings were observed after introduction of the Brockenbrough versus the RF needle through the dilator and sheath, suggesting that there may be a risk of plastic particle embolization with the conventional needle.9 A large retrospective study found that the RF needle was faster, more effective, and safer in achieving LA access,10 but a randomized prospective comparison to the conventional needle has not been performed.
The purpose of this study was to examine the effectiveness and safety of an RF needle compared with a conventional Brockenbrough needle for transseptal LA access in a prospective, randomized trial.
Methods
Trial Design and Patient Population
The Conventional Transseptal Needle Versus Radiofrequency Energy Needle Puncture for Left Atrial Access (TRAVERSE‐LA) study was a single‐blinded, randomized, controlled trial to compare the effectiveness and safety of transseptal puncture using an RF needle versus a conventional Brockenbrough in patients undergoing catheter ablation procedures requiring LA access.
Between January 2011 and November 2012, 72 patients were randomized in a 1:1, single‐blinded fashion to 1 of 2 transseptal needle groups. Intraprocedural measurements were prospectively obtained at the bedside by study personnel. Patients undergoing catheter ablation procedures involving a planned transseptal puncture were included if they were ≥18 years of age and able to consent to the research study. Patients were excluded from the study if transesophageal echocardiography performed before the procedure revealed a patent foramen ovale large enough to alter the strategy for transseptal LA access (such as the planned use of the ablator to probe the interatrial septum). All patients provided informed, written, and witnessed consent. The study protocol was approved by the Committee on Human Research of the University of California, San Francisco.
Study Protocol and Transseptal Puncture
The transseptal puncture was performed by a cardiac electrophysiology fellow and attending electrophysiologist via right femoral venous access. Intracardiac echocardiography (ICE) using a 9‐F Ultra ICE catheter (Boston Scientific) or an 8‐F AcuNav ultrasound catheter (Biosense Webster) guided the transseptal puncture. Patients randomized to the RF needle group underwent transseptal puncture with a large, preformed curve 71‐cm‐C1 or 98‐cm‐C1 18‐gauge NRG needle (Baylis Medical) through a 63‐cm Fast‐Cath SL1 sheath (St. Jude Medical) or a 71‐cm large curl Agilis NxT Steerable Introducer sheath (St. Jude Medical). Sheaths were selected at the discretion of the operating physician prior to knowledge of treatment assignment. The RF needle diameter was 18 gauge proximally and 21 gauge distally and had a blunt distal uninsulated electrode tip for RF energy transmission. The needle was fully insulated throughout its course, except for the electrode tip. A grounding pad was placed on the left thigh. The RFP 100‐115 RF Puncture Generator (Baylis Medical) was attached to the grounding pad and RF needle using a connector cable and was set to an output power of 10 W for 2 seconds. The generator produced continuous monopolar RF power output at a fixed frequency of ≈500 kHz. Patients randomized to the conventional needle group underwent transseptal puncture with either a large, preformed curve 71‐ or 98‐cm 18‐gauge BRK‐1 needle (St. Jude Medical) through the same sheaths listed above. The BRK‐1 needle had a shoulder 3 mm proximal to the introducer tip, designed to prevent the needle from advancing too far.
In preprocedural ex vivo testing of both needle groups, the transseptal needle and sheath were flushed with heparinized saline before use, and the transseptal needle was placed through the dilator and sheath until the tip of the needle could be visualized. The transseptal needles were not modified or manually shaped prior to placement through the dilator and sheath. In the conventional needle arm, the inner stylet was removed prior to advancement through the dilator and sheath. The transseptal needle was then removed, and the dilator and sheath were flushed again. Operators and study personnel looked for any evidence of grossly visible plastic particles, recorded as yes versus no (a “yes” answer required agreement between the operator and study personnel present).
The transseptal sheath and dilator were then advanced to the superior vena cava over a guidewire under fluoroscopic visualization. The guidewire was removed, and the contents of the dilator were evacuated and then flushed with heparinized saline. The transseptal needle was then flushed with heparinized saline, inserted into the dilator and sheath, and advanced under fluoroscopic guidance until the needle tip was located 2 to 5 mm proximal to the dilator tip. The needle, dilator, and sheath were pulled down as a unit (beginning of the time of measurement for the primary outcome) until tenting of the fossa ovalis was confirmed using ICE. Contrast injection and fluoroscopy were also used to verify the needle location. Holding the dilator and sheath still, the needle was then advanced out of the dilator, and contrast was injected. If LA access was not obtained after initial needle advancement in the conventional needle arm, the entire apparatus was advanced as a unit to puncture the septum with the needle; for the RF needle arm, RF energy was applied at 10 W for 2 seconds. If necessary, additional applications of RF energy were delivered to obtain LA access. LA access was confirmed by the operators on the basis of contrast media visualized in the LA under fluoroscopy and microbubbles observed in the LA with ICE. The dilator and sheath were then advanced over the needle into the LA under fluoroscopic and ICE visualization (end of the time of measurement for the primary outcome).
The initial study protocol allowed application of monopolar RF energy using an electrosurgical pencil (Covidien) or “bovie” set to “cut” at 35 W and applied to the proximal needle handle of the BRK‐1 needle in those who failed transseptal LA access with mechanical attempts.11 However, the protocol was amended after enrollment of the 10th patient to exclude this practice after the publication of a study suggested that application of electrocautery to the BRK‐1 needle may result in coring and embolizaton of septal tissue.12
Data Collection and Study Outcome Measures
The primary outcome was total time required for LA access for the first transseptal puncture, defined as time from the first pull‐down of the needle/sheath/dilator apparatus in the superior vena cava to first entrance of the sheath into the left atrium. Secondary outcome measures included other efficacy measures (failure of the assigned needle type, time from interatrial septum engagement to sheath advancement, and time from needle advancement to sheath advancement) and safety measures (presence of visible plastic dilator shavings from needle introduction and any procedural complication plausibly related to transseptal puncture). Procedural complications plausibly related to transseptal needle puncture included aortic puncture, pericardial effusion, stroke or systemic embolization, and death. The assigned needle type was determined to fail when further attempts to achieve LA access were deemed to be either futile or unsafe per the discretion of the operator. All patients were monitored for both intraprocedural complications and postprocedural complications until discharge.
Statistical Analysis
We targeted a sample size of 72 (36 in each randomization group) in order to achieve 80% power to detect a 5‐minute reduction in total transseptal puncture time (assuming a standard deviation of 7.5 minutes) using a 2‐sided alpha level of 0.05. The primary analysis was performed on an intention‐to‐treat basis. An exploratory per‐protocol analysis restricted to participants who maintained their initial needle assignment (ie, excluding crossover patients) was also performed. Normally distributed continuous variables are expressed as means and standard deviations, whereas continuous variables with skewed distributions are expressed as medians and interquartile ranges (IQRs). Baseline patient characteristics and outcome measures were compared between assigned needle groups using the χ2 test for categorical variables and t tests or the Wilcoxon rank‐sum test for continuous variables, as appropriate. A linear regression analysis using log‐transformed transseptal time (due to right‐skewed data) was used to identify predictors of transseptal time. Covariates were selected for inclusion in multivariable models if their univariate association with the outcome reached P<0.20. Statistical tests were 2‐sided and considered significant if they yielded a P<0.05. Analyses were performed using Stata version 11.1 (College Station, TX).
Results
Baseline Characteristics
We enrolled a total of 72 patients undergoing planned LA access via a transseptal puncture; 36 patients were randomly assigned to the RF needle and 36 to the conventional BRK‐1 needle (Figure 1). There were no significant differences in baseline patient demographic and clinical characteristics between the 2 study arms (Table 1). Twenty‐two patients (30.6%) had a previous transseptal puncture a median of 536 days (IQR, 173 to 1167 days) before the index procedure. Contrary to the protocol, 3 conventional needle patients were initially unsuccessful and ultimately resulted in LA access only after electrocautery energy was applied to the proximal needle handle. These patients were included in all analyses as part of the conventional needle arm and were not considered failures or crossover patients.
Figure 1.
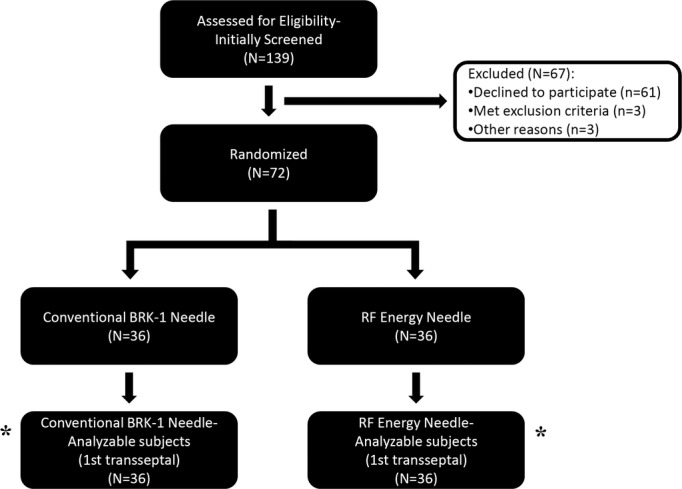
Subject flow in the study. *Patients available for analysis of the primary outcome of time of first transseptal puncture. There were no patients excluded from the analysis. RF indicates radiofrequency.
Table 1.
Baseline Patient, Operator, and Procedural Characteristics
| Characteristic | Conventional Needle Group (n=36) | RF Needle Group (n=36) | P Value |
|---|---|---|---|
| Patient demographic characteristics | |||
| Age, y | 61.1±11.7 | 59.9±11.3 | 0.668 |
| Male sex | 23 (63.9) | 25 (69.4) | 0.617 |
| Race | 0.392 | ||
| White | 33 (91.7) | 33 (91.7) | |
| Black | 1 (2.8) | 0 (0.0) | |
| Asian | 1 (2.8) | 0 (0.0) | |
| Other | 1 (2.8) | 3 (8.3) | |
| Body mass index, kg/m2 | 28.4±4.7 | 28.4±5.9 | 0.995 |
| Hypertension | 20 (55.6) | 20 (55.6) | 1.000 |
| Diabetes | 4 (11.1) | 5 (13.9) | 0.722 |
| Coronary artery disease | 4 (11.1) | 5 (13.9) | 0.722 |
| Congestive heart failure | 3 (8.3) | 3 (8.3) | 1.000 |
| Previous stroke or transient ischemic attack | 3 (8.3) | 2 (5.6) | 0.643 |
| Atrial fibrillation | 35 (97.2) | 35 (97.2) | 1.000 |
| Atrial fibrillation type | 0.563 | ||
| Paroxysmal | 27 (77.1) | 29 (82.9) | |
| Persistent | 7 (20.0) | 6 (17.1) | |
| Long‐standing persistent | 1 (2.9) | 0 (0.0) | |
| History of atrial flutter | 6 (16.7) | 9 (25.0) | 0.384 |
| History of atrial tachycardia | 1 (2.8) | 1 (2.8) | 1.000 |
| Wolff–Parkinson–White syndrome | 1 (2.8) | 1 (2.8) | 1.000 |
| Indication for transseptal puncture | 1.000 | ||
| Atrial fibrillation | 35 (97.2) | 35 (97.2) | |
| Accessory pathway | 1 (2.8) | 1 (2.8) | |
| Previous transseptal puncture | 10 (27.8) | 12 (33.3) | 0.609 |
| Left atrial size* | 0.844 | ||
| Normal | 8 (29.6) | 6 (25.0) | |
| Mildly enlarged | 5 (18.5) | 7 (29.2) | |
| Moderately enlarged | 8 (29.6) | 6 (25.0) | |
| Severely enlarged | 6 (22.2) | 5 (20.8) | |
| Operator‐related characteristics | |||
| Operator experience, days | |||
| Fellow‐in‐training experience | 395.2±169.4 | 433.3±165.4 | 0.337 |
| Attending physician experience | 3389.8±1377.3 | 3553.0±1458.3 | 0.627 |
| Procedural characteristics | |||
| Intracardiac echocardiography | 0.759 | ||
| Phased‐array ultrasound | 30 (83.3) | 29 (80.6) | |
| Radial‐view ultrasound | 6 (16.7) | 7 (19.4) | |
| Biplane fluoroscopy | 33 (91.7) | 31 (86.1) | 0.453 |
| Long sheath for transseptal needle | 0.555 | ||
| SL1 long sheath | 35 (97.2) | 34 (94.4) | |
| Agilis steerable long sheath | 1 (2.8) | 2 (5.6) | |
Values are reported as mean±SD or n (%). RF indicates radiofrequency; SD, standard deviation.
Proportions were calculated on the basis of patients with echocardiographic data available in each arm.
Primary and Secondary Outcomes
As seen in Figure 2, the median transseptal puncture time was 68% shorter using the RF needle compared with the conventional needle (2.3 minutes [IQR, 1.7 to 3.8 minutes] versus 7.3 minutes [IQR, 2.7 to 14.1 minutes], P=0.005). In additional analyses, the mean transseptal puncture time trended toward a shorter overall time using the RF needle compared with the conventional needle (5.2±10.2 versus 9.0±8.2 minutes, P=0.086). Median transseptal puncture times were also shorter in the RF needle arm from engagement of the fossa ovalis to the long sheath in the LA and needle tip out of the long sheath to the long sheath in the LA (Table 2). Of the 36 patients randomized to the RF needle arm, 27 (75.0%) required RF application an average of 1.2±0.6 times to achieve LA access. Per‐protocol analysis (ie, excluding crossovers) showed statistically significantly shorter median transseptal puncture times in the RF needle arm from engagement of the fossa ovalis (1.3 minutes [IQR, 0.7 to 1.9 minutes] versus 2.4 minutes [IQR, 1.2 to 4.7 minutes], P=0.003) and from first advancing the needle out of the long sheath (0.8 minutes [IQR, 0.4 to 1.2 minutes] versus 1.5 minutes [IQR, 0.7 to 2.2 minutes], P=0.012).
Figure 2.
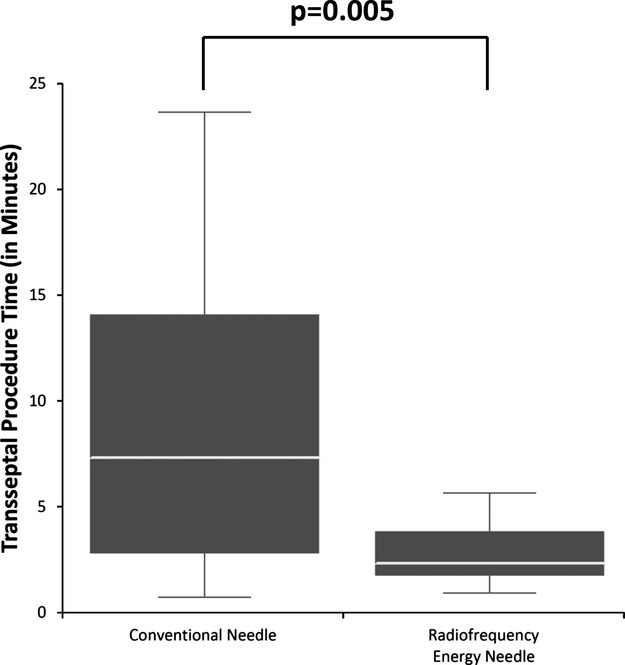
Total transseptal puncture procedure time by assigned transseptal needle. Box plots show the median (white line) and interquartile range (from top to bottom of the box plot). Each whisker represents the most extreme value within 1.5 times the interquartile range. Outlier values are not shown. Times are inclusive of crossover time.
Table 2.
Procedural Outcomes
| Outcome | Conventional Needle Group (n=36) | RF Needle Group (n=36) | P Value |
|---|---|---|---|
| Transseptal‐related procedural outcomes (minutes)* | |||
| Time from pulling down from superior vena cava to sheath in LA | 7.3 (2.7 to 14.1) | 2.3 (1.7 to 7.3) | 0.005 |
| Time from interatrial septum engagement to sheath in LA | 2.8 (1.4 to 8.5) | 1.3 (0.7 to 1.9) | <0.001 |
| Time from needle first out of dilator to sheath in LA | 1.9 (0.8 to 7.6) | 0.8 (0.4 to 1.2) | <0.001 |
| Total procedure‐related outcomes (minutes) | |||
| Total procedure time | 356.5±71.3 | 347.4±82.3 | 0.615 |
| Total fluoroscopy time | 52.6±18.8 | 54.1±21.0 | 0.747 |
Values are reported as median (IQR) or mean±SD. IQR indicates interquartile range; LA, left atrium; RF, radiofrequency; SD, standard deviation.
Times are inclusive of crossover time.
Failure to achieve transseptal LA access with the assigned needle was less common using the RF needle compared with the conventional needle (0/36 [0%] versus 10/36 [27.8%], P<0.001). Although a larger proportion of patients with a previous transseptal puncture failed with the conventional needle, this did not reach statistical significance (4/10 [40%] versus 6/26 [23.1%], P=0.31). In all 10 failures, crossover occurred because of an inability to puncture the interatrial septum despite forward pressure and tenting, leading to concern that further effort might lead to perforation of the free (lateral) LA wall. Of the 7 operators who enrolled patients in the study, 5 operators experienced failure of the assigned conventional needle. The 7 operators differed in their preference of and experience with each type of needle prior to study initiation (Table 3). In the RF needle arm, transseptal LA access was initially unsuccessful in 1 patient despite engagement of the interatrial septum and application of the RF pulse, resulting in crossover to the conventional needle. However, after failure of the conventional needle, the RF needle was attempted again, this time resulting in successful LA access after 1 RF pulse.
Table 3.
Operator Characteristics Before and During Transseptal Needle Study
| Operator ID | Years of Experience With BRK‐1 Needle Before Study | Years of Experience With RF Needle Before Study | Preferred Needle Before Study | Number of Patients in Study Randomized to BRK‐1 Needle | Number of Patients in Study Randomized to RF Needle | Number of Crossover Patients From BRK‐1 to RF Needle |
|---|---|---|---|---|---|---|
| 1 | 18 | 1 | BRK‐1 | 4 | 5 | 3 |
| 2 | 10 | 0 | BRK‐1 | 2 | 6 | 1 |
| 3 | 10 | 0 | BRK‐1 | 4 | 0 | 0 |
| 4 | 8 | 2 | RF | 18 | 17 | 4 |
| 5 | 7 | 2 | BRK‐1 | 2 | 1 | 1 |
| 6 | 5 | 2 | RF | 5 | 7 | 2 |
| 7 | 1 | 1 | RF | 1 | 0 | 0 |
ID indicates identification; RF, radiofrequency.
With ex vivo preprocedural testing involving advancement of the assigned transseptal needle through the plastic dilator and sheath, the RF needle created grossly visible plastic shavings less often than the conventional needle (0 [0%] versus 12/36 [33.3%], P<0.001). An example of plastic dilator shavings seen after introduction of the conventional needle through the dilator and long sheath is shown in Figure 3.
Figure 3.
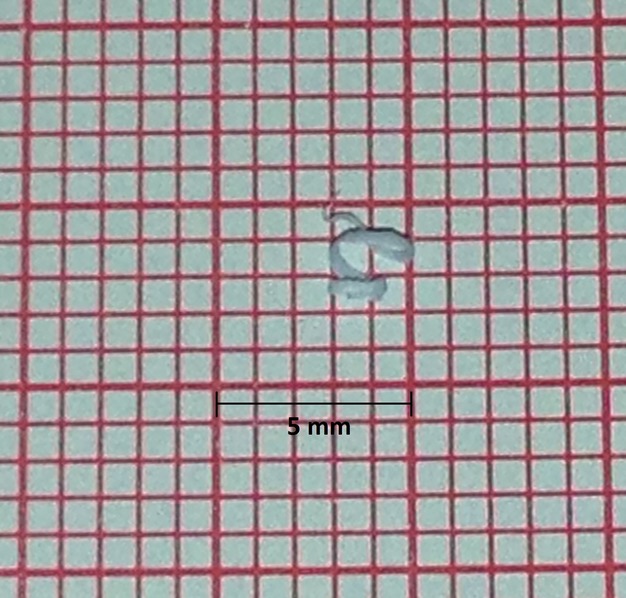
Pictured is an example of grossly visible particles that were produced after the introduction of a conventional needle through the dilator and long sheath. The particles are placed on conventional electrocardiography paper as a size reference.
Procedural complications were no different between the RF and conventional needle groups (1/36 [2.8%] versus 1/36 [2.8%], P=1.000). In the RF needle arm, 1 patient was found to have a pericardial effusion detected by ICE after conclusion of the LA ablation procedure (3 hours after the transseptal puncture). In the conventional needle arm, 1 patient experienced a transient ischemic attack with brain magnetic resonance imaging consistent with embolic etiology.
Predictors of Transseptal Time
Multivariable linear regression analysis revealed that older patient age, increased attending physician experience, use of the conventional needle, and radial‐view ICE were each significantly associated with longer transseptal time (Table 4).
Table 4.
Univariate and Multivariable Analyses of Predictors Associated With Transseptal Time
| Variable | Univariate Analysis | Multivariable Analysis | ||
|---|---|---|---|---|
| Percent Increase in Transseptal Time* (95% CI) | P Value | Percent Increase in Transseptal Time* (95% CI) | P Value | |
| Age (per 10‐year increase) | 15.4% (−5.1 to 35.9) | 0.138 | 18.2% (1.6 to 34.8) | 0.032 |
| Previous transseptal puncture | 34.1% (−16.6 to 84.8) | 0.184 | 31.0% (−10.0 to 72.1) | 0.136 |
| Radial view intracardiac ultrasound | 87.5% (29.6 to 145.3) | 0.004 | 79.6% (29.6 to 129.7) | 0.002 |
| Attending physician experience (per 1‐year increase) | 9.8% (4.1 to 15.5) | 0.001 | 8.3% (3.2 to 13.3) | 0.002 |
| Conventional needle | 67.8% (23.3 to 112.2) | 0.003 | 73.3% (35.8 to 110.9) | <0.001 |
| Male sex | −22.0% (−71.9 to 27.9) | 0.381 | * | — |
| Congestive heart failure | −29.2% (−114.5 to 56.1) | 0.497 | * | — |
| Fellow physician experience (per 1‐year increase) | −5.2% (−57.1 to 46.7) | 0.842 | * | — |
| Biplane fluoroscopy | 34.8% (−39.9 to 109.6) | 0.356 | * | — |
CI indicates confidence interval.
The β coefficient from regression analyses represents the percent increase in transseptal time per unit increase of continuous predictor variables or as associated with individual categorical variables.
Covariates failing to meet criteria for inclusion in the multivariable model (as described in the Methods and Results section).
Discussion
TRAVERSE‐LA is the first randomized comparison of an RF versus conventional needle for transseptal puncture. The RF needle significantly reduced time to transseptal LA access, resulted in less failure of the assigned needle, and produced fewer visible plastic shavings from introduction of the needle through the dilator and sheath. Procedural complications did not differ between needle groups.
Transseptal puncture for LA access is becoming more common because of the growing adaptation of catheter ablation and structural heart procedures involving left‐sided access.1–7 However, the transseptal puncture procedure can be time consuming13–14 and can result in important complications.15–16 Prolonged transseptal procedures may increase total procedure times and ionizing radiation exposure to the patient and operator because of the high‐intensity fluoroscopy that is often employed. Finally, personnel and electrophysiology laboratory time may become both clinically and financially relevant at the extremes of differences in transseptal time, particularly if it means staffing overtime is used or the “next case” is postponed for another day.
An observational study describing the initial experience using the RF needle reported a 97.2% success rate (35 of 36) in achieving transseptal access, but no comparator group was included.17 Subsequently, a larger observational study suggested that the RF needle may result in shorter procedure times, better efficacy of achieving LA access, and decreased complications.10 However, data were analyzed retrospectively, and patients were not randomized to needle therapy. As the RF needle was used more recently and therefore potentially in a more experienced electrophysiology laboratory, the results may have been biased in favor of the RF needle.
We found that RF compared with conventional needle use resulted in a 68% shorter median time to transseptal LA access; this amounted to an absolute 5‐minute median difference and more than a 10‐minute upper quartile difference in transseptal puncture time between the 2 arms. However, the absolute time difference may not be particularly large in light of the whole procedure. Indeed, we observed no difference in total procedure or fluoroscopy time between groups. Of note, the RF application itself was quite short; the 75% of patients who required RF usage for transseptal LA access needed an average of 1.2±0.6 applications, translating into an approximate mean of 2.4±1.2 seconds of total RF application time. Subanalyses examining several points during the first transseptal puncture, including time from fossa ovalis engagement to long sheath across and needle out of the sheath to long sheath across, found that the RF needle consistently resulted in shorter transseptal times in both intention‐to‐treat and per‐protocol analyses. It is interesting to note that the variability of transseptal time appeared to be largest in the conventional group (as can be seen in Figure 2), suggesting that the timing differences were driven primarily by the more difficult cases in the conventional group versus a more uniform experience in the RF group.
To assess predictors of transseptal time, we constructed multivariable models with covariates plausibly associated with the outcome. After adjustment, use of the RF needle was one of the strongest predictors of a shorter transseptal time. Use of radial‐view ICE was associated with longer transseptal times, suggesting that the higher‐resolution view of the fossa ovalis obtained with phased‐array ICE rather than the more global atrial view obtained with the radial‐view system may be particularly useful during these procedures. Older patient age also predicted longer transseptal times, perhaps because of more distorted cardiac anatomy or more interatrial septal fibrosis. Counter to expectations, increased attending physician experience was also associated with longer transseptal times, perhaps related to a more cautious approach taken by experienced operators.
Randomization to the RF needle resulted in success in all patients, whereas randomization to the conventional needle resulted in 10 crossover patients, all of whom were subsequently successful using the RF needle. Because this was a single‐blinded study and the operator made the final decision to crossover based on safety reasons, inadvertent bias may have occurred. However, we found that crossover of patients from the conventional to RF needle was distributed across operators, many of whom personally preferred to use the conventional needle prior to the study (Table 3). Therefore, it is not clear why bias (or lack of blinding) would not have similarly led to more crossovers from the RF to the conventional needle. Although the proportion of patients who failed transseptal puncture with the conventional needle was higher than reported in previous studies, it is noteworthy that all previous studies on the subject have been retrospective.10,16 It is important to emphasize that this is the first study to prospectively enroll and then follow transseptal puncture patients with research personnel in the room before and throughout the case to carefully track successes and failures. It is possible that difficult or failed transseptal puncture attempts in previous retrospective studies were not included or missed. Finally, although not statistically significant, 40% of those who failed with the conventional needle (and succeeded with the RF needle) had a previous transseptal puncture, a previously established predictor of a difficult procedure.13 However, given this large difference and previous evidence that repeat transseptal punctures are more challenging, the RF needle may be particularly preferred in the repeat transseptal puncture population. In fact, we used a conservative estimate when designating “failure” of the assigned transseptal needle: 3 additional patients assigned to the conventional needle had difficulty in achieving LA access despite forward pressure and tenting, and based on operator discretion, application of electrocautery to the conventional needle was performed against protocol, each time resulting in success. Although successful transseptal puncture has been described in the literature based on this technique,11 we changed the study protocol to preclude this practice after the study was already under way based on evidence of tissue coring and the theoretical risk of embolism that can occur with this technique.12
We found that the RF needle was less likely to produce visible plastic shavings after introduction into the dilator and sheath. The most plausible mechanism for this difference is that the conventional needle has a sharp tip, whereas the RF needle tip is blunt. Feld et al9 reported that the production of plastic shavings measured by light microscopy occurred less commonly with RF needles than with conventional needles. Our study is the first prospective, randomized trial to confirm these findings and quantitate the prevalence of this phenomenon in a clinical setting. In the conventional needle arm, we performed ex vivo testing without the stylet in the needle, which is the standard of care at our institution. We performed shaving in this manner to mimic the course of the needle through the dilator/sheath outside the patient's body. In fact, our method of conventional needle introduction without the stylet and with forward flushing is the most common method employed in published reports,10,13,16 and is reflected in the original report of shaved visible particles.9 We acknowledge that the frequency of plastic shavings might be reduced if the stylet is left in place until the needle/stylet tip is close to the dilator tip; however, removing the stylet within the body may increase the risk of air embolism and does not preclude unseen shaving production from the unprepared distal portion of the dilator. Future studies are needed to evaluate whether plastic shavings are dislodged during transseptal procedures, even after the dilator and sheath are prepped in the absence of the stylet, potentially leading to clinical sequelae. Complications did not differ between the RF and conventional needle arms. It is important to emphasize that ICE was used to guide transseptal puncture in all cases in this trial and that risks may be higher if the RF needle is used in the absence of ICE.
Study Limitations
Several limitations should be acknowledged. First, this study included a relatively small number of patients. We calculated the sample size necessary to meet the primary outcome of the study a priori, and a lack of power should not result in spurious false‐positive results. However, lack of power could result in failure to detect certain real relationships, such as important predictors of transseptal time in multivariable models. Second, the reasons for the high rate of LA access failure in the conventional needle study arm are unclear and could represent unique aspects of the patient population studied that may not be generalizable to general practice. Third, we only used the BRK‐1 needle manufactured by St. Jude Medical in the conventional needle arm of this study. Conventional needles manufactured by different companies may have other characteristics that could affect transseptal puncture success. Fourth, our study did not involve other novel protocols in the event of conventional needle failure, such as use of electrocautery applied to a conventional needle or a nitinol guidewire (SafeSept, Pressure Products Inc) through the lumen of the conventional needle.18 Finally, despite finding that use of the RF needle resulted in shorter transseptal puncture time, less failure, and fewer plastic shavings, the RF needle is generally more expensive than the conventional needle, suggesting that a formal cost‐effectiveness study is warranted.
Conclusions
Use of an RF needle resulted in shorter time to transseptal LA access, less failure in achieving transseptal LA access, and fewer visible plastic shavings. There were no differences in clinically recognized complications.
Sources of Funding
This study was funded by the Joseph Drown Foundation (awarded to Dr Marcus) and partially supported by Baylis Medical as an investigator‐initiated grant (to Dr Marcus). The funding sources had no role in the study design, study implementation, statistical analysis, data interpretation, or manuscript preparation. The final manuscript was not submitted to the funding sources for review. Analyses were performed at the University of California, San Francisco, by the study authors.
Disclosures
Dr Marcus is a consultant for InCarda and has received research support from Baylis Medical, Gilead, and SentreHeart Inc.
References
- 1.Calkins H, Kuck KH, Cappato R, Brugada J, Camm AJ, Chen SA, Crijns HJ, Damiano RJ, Jr, Davies DW, DiMarco J, Edgerton J, Ellenbogen K, Ezekowitz MD, Haines DE, Haissaguerre M, Hindricks G, Iesaka Y, Jackman W, Jalife J, Jais P, Kalman J, Keane D, Kim YH, Kirchhof P, Klein G, Kottkamp H, Kumagai K, Lindsay BD, Mansour M, Marchlinski FE, McCarthy PM, Mont JL, Morady F, Nademanee K, Nakagawa H, Natale A, Nattel S, Packer DL, Pappone C, Prystowsky E, Raviele A, Reddy V, Ruskin JN, Shemin RJ, Tsao HM, Wilber D. 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow‐up, definitions, endpoints, and research trial design. J Interv Card Electrophysiol. 2012; 33:171-257 [DOI] [PubMed] [Google Scholar]
- 2.Lesh MD, Van Hare GF, Scheinman MM, Ports TA, Epstein LA. Comparison of the retrograde and transseptal methods for ablation of left free wall accessory pathways. J Am Coll Cardiol. 1993; 22:542-549 [DOI] [PubMed] [Google Scholar]
- 3.Pluta S, Lenarczyk R, Pruszkowska‐Skrzep P, Kowalski O, Sokal A, Sredniawa B, Mazurek M, Kalarus Z. Transseptal versus transaortic approach for radiofrequency ablation in patients with cardioverter‐defibrillator and electrical storm. J Interv Card Electrophysiol. 2010; 28:45-50 [DOI] [PubMed] [Google Scholar]
- 4.Holmes DR, Reddy VY, Turi ZG, Doshi SK, Sievert H, Buchbinder M, Mullin CM, Sick P. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non‐inferiority trial. Lancet. 2009; 374:534-542 [DOI] [PubMed] [Google Scholar]
- 5.Bartus K, Han FT, Bednarek J, Myc J, Kapelak B, Sadowski J, Lelakowski J, Bartus S, Yakubov SJ, Lee RJ. Percutaneous left atrial appendage suture ligation using the lariat device in patients with atrial fibrillation: initial clinical experience. J Am Coll Cardiol. 2013; 62:108-118 [DOI] [PubMed] [Google Scholar]
- 6.Reyes VP, Raju BS, Wynne J, Stephenson LW, Raju R, Fromm BS, Rajagopal P, Mehta P, Singh S, Rao DP, Satyanarayana PV, Turi ZG. Percutaneous balloon valvuloplasty compared with open surgical commissurotomy for mitral stenosis. N Engl J Med. 1994; 331:961-967 [DOI] [PubMed] [Google Scholar]
- 7.Feldman T, Wasserman HS, Herrmann HC, Gray W, Block PC, Whitlow P, St Goar F, Rodriguez L, Silvestry F, Schwartz A, Sanborn TA, Condado JA, Foster E. Percutaneous mitral valve repair using the edge‐to‐edge technique: six‐month results of the EVEREST Phase I Clinical Trial. J Am Coll Cardiol. 2005; 46:2134-2140 [DOI] [PubMed] [Google Scholar]
- 8.Sakata Y, Feldman T. Transcatheter creation of atrial septal perforation using a radiofrequency transseptal system: novel approach as an alternative to transseptal needle puncture. Catheter Cardiovasc Interv. 2005; 64:327-332 [DOI] [PubMed] [Google Scholar]
- 9.Feld GK, Tiongson J, Oshodi G. Particle formation and risk of embolization during transseptal catheterization: comparison of standard transseptal needles and a new radiofrequency transseptal needle. J Interv Card Electrophysiol. 2011; 30:31-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Winkle RA, Mead RH, Engel G, Patrawala RA. The use of a radiofrequency needle improves the safety and efficacy of transseptal puncture for atrial fibrillation ablation. Heart Rhythm. 2011; 8:1411-1415 [DOI] [PubMed] [Google Scholar]
- 11.Knecht S, Jais P, Nault I, Wright M, Matsuo S, Madaffari A, Lellouche N, O'Neill MD, Derval N, Deplagne A, Bordachar P, Sacher F, Hocini M, Clementy J, Haissaguerre M. Radiofrequency puncture of the fossa ovalis for resistant transseptal access. Circ Arrhythm Electrophysiol. 2008; 1:169-174 [DOI] [PubMed] [Google Scholar]
- 12.Greenstein E, Passman R, Lin AC, Knight BP. Incidence of tissue coring during transseptal catheterization when using electrocautery and a standard transseptal needle. Circ Arrhythm Electrophysiol. 2012; 5:341-344 [DOI] [PubMed] [Google Scholar]
- 13.Marcus GM, Ren X, Tseng ZH, Badhwar N, Lee BK, Lee RJ, Foster E, Olgin JE. Repeat transseptal catheterization after ablation for atrial fibrillation. J Cardiovasc Electrophysiol. 2007; 18:55-59 [DOI] [PubMed] [Google Scholar]
- 14.Tomlinson DR, Sabharwal N, Bashir Y, Betts TR. Interatrial septum thickness and difficulty with transseptal puncture during redo catheter ablation of atrial fibrillation. Pacing Clin Electrophysiol. 2008; 31:1606-1611 [DOI] [PubMed] [Google Scholar]
- 15.De Ponti R, Cappato R, Curnis A, Della Bella P, Padeletti L, Raviele A, Santini M, Salerno‐Uriarte JA. Trans‐septal catheterization in the electrophysiology laboratory: data from a multicenter survey spanning 12 years. J Am Coll Cardiol. 2006; 47:1037-1042 [DOI] [PubMed] [Google Scholar]
- 16.Roelke M, Smith AJ, Palacios IF. The technique and safety of transseptal left heart catheterization: the Massachusetts General Hospital experience with 1,279 procedures. Cathet Cardiovasc Diagn. 1994; 32:332-339 [DOI] [PubMed] [Google Scholar]
- 17.Smelley MP, Shah DP, Weisberg I, Kim SS, Lin AC, Beshai JF, Burke MC, Knight BP. Initial experience using a radiofrequency powered transseptal needle. J Cardiovasc Electrophysiol. 2010; 21:423-427 [DOI] [PubMed] [Google Scholar]
- 18.Wadehra V, Buxton AE, Antoniadis AP, McCready JW, Redpath CJ, Segal OR, Rowland E, Lowe MD, Lambiase PD, Chow AW. The use of a novel nitinol guidewire to facilitate transseptal puncture and left atrial catheterization for catheter ablation procedures. Europace. 2011; 13:1401-1405 [DOI] [PubMed] [Google Scholar]


