Abstract
Background
Limiting dietary sodium consumption is a core lifestyle recommendation for the prevention of hypertension. There is increasing evidence that low potassium consumption also increases hypertension risk. We estimated sex‐specific 22‐year trends in sodium and potassium consumption.
Methods and Results
We used data from the Minnesota Heart Survey, which performs surveillance of risk factors for cardiovascular disease in the Minneapolis–St. Paul metropolitan area. The Minnesota Heart Survey is a random population‐based sample of free‐living adults aged 25 to 74. Surveys were conducted in 1985–1987 (n=2273), 1990–1992 (n=2487), 1995–1997 (n=1842), 2000–2002 (n=2759), and 2007–2009 (n=1502). Dietary intake of sodium and potassium was estimated from one 24‐hour dietary recall. Over 22 years, age‐adjusted sodium and potassium intake among men remained relatively stable in 1985–1987 and 2007–2009 (Ptrend=0.41 and 0.29, respectively); sodium ranged from 3820 mg/day (1995–1997) to 3968 mg/day (2007–2009) and potassium from 3111 mg/day (2000–2002) to 3249 mg/day (1995–1997). Sodium and potassium intake increased among women, from 2531 mg/day in 1985–1987 to 2854 mg/day in 2007–2009 (Ptrend=0.001) for sodium and from 2285 to 2533 mg/day (Ptrend<0.0001) for potassium. We observed stable or increasing sodium and potassium intake within some strata of age, education, and body mass index.
Conclusions
Despite long‐standing public health recommendations to limit sodium intake to <2300 mg/day, high sodium intake levels have persisted over the past 22 years. Furthermore, although potassium consumption increased in some subgroups over the study period, mean consumption remained significantly lower than the recommended 4700 mg/day in all groups.
Keywords: diet, population, potassium, prevention, risk factors, sodium
Introduction
Studies support a role for both sodium and potassium consumption in the development of hypertension and cardiovascular disease.1–3 Current national survey data indicate that most Americans consume far more sodium and less potassium than the recommended4 maximum of 2300 mg/day of sodium and minimum of 4700 mg/day of potassium, with lower sodium recommendations for certain high‐risk groups.5 Sodium restriction has been a component of the Dietary Guidelines for Americans since its introduction in 1980,6 and national health organizations have encouraged individuals to use less salt, read labels for sodium content, and request low‐salt options and have urged industry to lower the sodium content of commercially prepared food products. In contrast, little attention has been directed at increasing potassium consumption in the population.
Data available to evaluate long‐term trends in sodium and potassium intake in the United States population over the last several decades are limited, and findings across studies are inconsistent.7–10 Furthermore, population‐representative data are scant, and dietary assessment from national surveillance has not been completely consistent. To contribute to the limited number of studies of trends in the consumption of these nutrients, this article describes trends in sodium and potassium consumption from 1985–1987 through 2007–2009, using data from the Minnesota Heart Survey (MHS). Since its survey in 1985–1987, the MHS has employed rigorous and consistent methods for dietary assessment and nutrient coding, offering an opportunity to examine long‐term sodium and potassium trends. We hypothesized that sodium consumption has not declined over the 22‐year study period and that potassium consumption has been lower than the recommended 4700 mg/day over the 22 years.
Methods
Minnesota Heart Survey
The Minnesota Heart Survey (MHS) is a population‐based surveillance study of trends in cardiovascular disease risk factors in the Minneapolis–St. Paul, Minnesota, 7‐county metropolitan area.11–12 The MHS selected a probability sample of noninstitutionalized adults at each of 5 cross‐sectional surveys conducted in 1985–1987, 1990–1992, 1995–1997, 2000–2002, and 2007–2009. Data were also collected in 1980–1982, but we restricted the present analysis to data from 1985–1987 onward because of changes in sodium assessment (described in the Dietary Intake Assessment section).
The MHS employed a 2‐stage cluster sampling design. Clusters (n=704) of ≈1000 households each were derived from census maps, among which 40 clusters were randomly selected to represent the study area. At each survey, population growth was calculated in all 704 clusters, with new clusters selected to account for population growth. The 40 original clusters were used until 1995, when urban growth merited the addition of household clusters to ensure representation of the region. In 1995–1997 and 2000–2002, 4 new clusters, for a total of 44 clusters, were randomly selected from 10 clusters that were identified as high‐growth areas that exhibited an increase of ≥250% in the number of households from the 1980 to the 1990 census. In 2007–2009, based on the same population growth methodology, 3 clusters were added to account for growth in suburban areas for a total of 47 clusters. Within each cluster, household addresses were randomly sampled without replacement, meaning that households were not eligible to be sampled in >1 MHS study period.
Individuals were eligible to participate if they were aged 25 to 74 years for study periods through 1985–1987, after which eligibility was extended to 84 years of age. In 2000–2002, youth aged 8 to 17 were also included. The current analysis was restricted to those aged 25 to 74.
Trained in standardized procedures, a study interviewer visited selected households to administer a 15‐ to 45‐minute home interview that assessed participant sociodemographic characteristics, medical history, smoking status, and health knowledge, attitudes, and beliefs. Study participants were also asked to attend a local clinic visit for physical measures and collection of a 24‐hour dietary recall. Study staff measured participant height and weight using standard protocols. Body mass index (BMI) was calculated as weight (in kilograms) divided by height (meters squared). Response rates ranged from 64% to 69% across the 6 study periods. MHS survey respondents were slightly more likely to be married, employed, better educated, and nonsmokers, as compared with nonrespondents.
Written consent was obtained from all study participants. Consent and data collection procedures for each survey were approved by the University of Minnesota Research Subjects' Protection Programs Institutional Review Board.
Dietary Intake Assessment
A 24‐hour dietary recall was obtained from a random 50% sample of participants who completed the clinic survey, with the exception of study period 2000–2002, during which all clinic participants were asked to complete the dietary recall.
Interviewers who collected 24‐hour dietary recall data were trained and certified by the University of Minnesota Nutrition Coordinating Center. Dietary recall data were collected in‐person using a multiple‐pass approach. A listing of all foods and beverages consumed in the previous 24 hours was obtained, followed by detailed information about each reported food and beverage, including the amount consumed and method of preparation. Three‐dimensional food models along with visual aids (eg, household measuring cups and spoons, rulers) were available to assist in reporting portion size.
Several sodium‐specific questions were included in MHS dietary assessments, beginning in 1985–1987. Participants were asked if a food item was reduced in sodium or low sodium when applicable and whether salt was added in the preparation of foods in which salt may be added in cooking. This information was used in coding foods for calculating sodium intake. Salt added to food at the table was not assessed.
For all surveys, the University of Minnesota Nutrition Coordinating Center Food and Nutrient Database was used to calculate sodium and potassium intake from foods.13 To keep pace with changes in the marketplace, this database was expanded and updated on an ongoing basis with a new version released annually. In 1984 the database underwent a major sodium update that included the addition of a number of low‐sodium products such as unsalted butter, margarine, and potato chips. The update also included expanding entries for food items that vary in sodium and potassium content. As an example, separate entries were created for fresh, frozen, and canned vegetables to account for the generally higher sodium content of canned vegetables (before the update, nutrient values for fresh and frozen vegetables were used for all cooked vegetables).
The 24‐hour dietary recall information was collected manually (paper and pencil) until 1995, when computerized direct data entry was introduced (Nutrition Data System for Research software) and used in the 1995–1997 and subsequent surveys.14 The 2 approaches (paper and pencil versus Nutrition Data System for Research) did not yield significantly different estimates of nutrient consumption on the basis of a substudy of 100 participants from whom data were collected using both methods. For example, there was a 3.2‐kilocalorie difference in estimated total caloric intake and a 1.1% difference in calories obtained from fat (P>0.05 for both; unpublished data, Donna Arnett, PhD, 1998).
Statistical Analysis
Data analysis was restricted to participants aged 25 to 74 years with a completed 24‐hour dietary recall. After age and diet data restrictions, there were 2273 participants available for analysis from the 1985–1987 survey, 2487 from the 1990–1992 survey, 1842 from the 1995–1997 survey, 2759 from the 2000–2002 survey; and 1502 from the 2007–2009 survey. All analyses were conducted using the SAS software package (SAS Inc, Cary, NC).
Survey‐specific mean intake of sodium and potassium was estimated using a generalized linear mixed model to account for the 2‐stage sample design. The model adjusted variance estimates for correlations among MHS participants that resulted from neighborhood‐based clustered sampling. Sex‐specific trends were calculated because of significant differences in food intake. Furthermore, sex‐specific trends were estimated by 15‐year age groups, educational attainment (<high school or ≥high school), and BMI (normal weight [BMI <25 kg/m2], overweight [25≤BMI<30 kg/m2], and obese [BMI ≥30 kg/m2]). We did not adjust for total energy intake in primary age‐adjusted analysis because we wanted to compare mean intake estimates to recommended intake levels. In separate analyses, we adjusted for total energy to examine the effect of changes in energy intake.
Results
Demographic characteristics of the MHS sample changed over the 5 surveys (Table 1). The Minneapolis–St. Paul metropolitan area has become more ethnically diverse, as reflected in the increase in nonwhite ethnicities. Also apparent was the increase in the prevalence of obesity, mirroring well‐documented national trends, from 20.8% in 1985–1987 to 36.2% in 2007–2009 among men and from 21.6% to 30.8% among women. In the MHS sample, educational attainment increased and the age distribution shifted to older ages over the study period. Among men overall, age‐adjusted mean sodium and potassium intake remained stable from 1985–1987 to 2007–2009 (Table 2). Sodium consumption trends were stable within all strata of age, education, and BMI, except for a statistically significant increase in sodium intake among men 55 to 74 years of age (Ptrend=0.004; Table 2). Potassium intake declined among men aged 25 to 39 (P=0.02) and those aged 40 to 54 (P=0.03), but increased among those aged 55 to 74 (P=0.005; Table 2). Mean nutrient intake did not differ in men across education and BMI categories, except estimated sodium intake was lower among older men compared with younger men (Table 2). Estimated mean sodium intake did not materially change on additional adjustment for total energy, but age‐group‐specific potassium trends were attenuated and no longer statistically significant (Figure 1, Table S1).
Table 1.
Participant Characteristics by Sex and Survey Year, Minnesota Heart Survey, 1985–1987 Through 2007–2009
| 1985–1987 | 1990–1992 | 1995–1997 | 2000–2002 | 2007–2009 | |
|---|---|---|---|---|---|
| Men, n | 1100 | 1141 | 860 | 1272 | 696 |
| Kilocalories, mean (SD) | 2510 (1069) | 2502 (1038) | 2469 (1079) | 2439 (960) | 2378 (887) |
| Age group, n (%) | |||||
| 25 to 39 | 498 (45.3) | 513 (45.0) | 296 (34.4) | 430 (33.8) | 175 (25.1) |
| 40 to 54 | 335 (30.5) | 370 (32.4) | 320 (37.2) | 511 (40.2) | 266 (38.2) |
| 55 to 74 | 267 (24.3) | 258 (22.6) | 244 (28.4) | 331 (26.0) | 255 (36.6) |
| Education level, n (%) | |||||
| >High school | 755 (68.6) | 813 (71.3) | 644 (74.9) | 971 (76.3) | 571 (82.0) |
| ≤High school | 345 (31.4) | 328 (28.8) | 216 (25.) | 301 (23.7) | 125 (18.0) |
| Ethnicity, n (%) | |||||
| White | 1059 (96.3) | 1083 (94.9) | 803 (93.4) | 1136 (89.3) | 632 (90.8) |
| Nonwhite | 41 (3.7) | 58 (5.1) | 57 (6.6) | 136 (10.7) | 64 (9.2) |
| Body mass index, n (%) | |||||
| <25 | 298 (27.1) | 308 (27.0) | 169 (19.7) | 307 (24.1) | 135 (19.4) |
| 25.0 to 29.9 | 573 (52.1) | 559 (49.0) | 418 (48.6) | 540 (42.5) | 309 (44.4) |
| ≥30 | 229 (20.8) | 274 (24.0) | 273 (31.7) | 425 (33.4) | 252 (36.2) |
| Women, n | 1173 | 1346 | 982 | 1487 | 806 |
| Kilocalories, mean (SD) | 1653 (657) | 1661 (680) | 1833 (879) | 1772 (669) | 1773 (632) |
| Age group, n (%) | |||||
| 25 to 39 | 497 (42.4) | 590 (43.8) | 354 (36.1) | 496 (33.4) | 209 (25.9) |
| 40 to 54 | 387 (33.0) | 451 (33.5) | 381 (38.8) | 632 (42.5) | 326 (40.5) |
| 55 to 74 | 289 (24.6) | 305 (22.7) | 247 (25.1) | 359 (24.1) | 271 (33.6) |
| Education level, n (%) | |||||
| >High school | 687 (58.6) | 899 (66.8) | 685 (69.8) | 1107 (74.4) | 672 (83.4) |
| ≤High school | 486 (41.4) | 447 (33.2) | 297 (30.2) | 380 (25.6) | 134 (16.6) |
| Ethnicity, n (%) | |||||
| White | 1122 (95.6) | 1282 (95.3) | 925 (94.2) | 1345 (90.4) | 725 (90.0) |
| Nonwhite | 51 (4.4) | 64 (4.7) | 57 (5.8) | 142 (9.6) | 81 (10.0) |
| Body mass index, n (%) | |||||
| <25 | 579 (49.4) | 650 (48.3) | 400 (40.7) | 579 (39.0) | 313 (38.8) |
| 25.0 to 29.9 | 341 (29.1) | 393 (29.2) | 296 (30.1) | 439 (29.5) | 245 (30.4) |
| ≥30 | 253 (21.6) | 303 (22.5) | 286 (29.1) | 469 (31.5) | 248 (30.8) |
Table 2.
Age‐Adjusted Mean Intake of Sodium and Potassium (mg/day) for Men in the Minneapolis–St. Paul Metropolitan Area Aged 25 to 74: Minnesota Heart Survey, 1985–1987 Through 2007–2009
| Mean (SE) | P Value, Linear Trend | |||||
|---|---|---|---|---|---|---|
| 1985–1987 | 1990–1992 | 1995–1997 | 2000–2002 | 2007–2009 | ||
| Sodium, mg/day | ||||||
| All men | 3896 (58) | 3869 (58) | 3820 (66) | 3889 (55) | 3968 (73) | 0.41 |
| Age | ||||||
| 25 to 39 | 4246 (93) | 4279 (92) | 3934 (121) | 4183 (100) | 4209 (157) | 0.66 |
| 40 to 54 | 4138 (111) | 3766 (107) | 4028 (115) | 3792 (95) | 4021 (123) | 0.56 |
| 55 to 74 | 3148 (94) | 3397 (96) | 3357 (98) | 3580 (85) | 3482 (96) | 0.004 |
| Education level | ||||||
| >High school | 3862 (72) | 3805 (70) | 3783 (65) | 3911 (65) | 3977 (82) | 0.15 |
| ≤High school | 3962 (105) | 4037 (107) | 3956 (132) | 3832 (112) | 3954 (172) | 0.61 |
| Body mass index | ||||||
| <25.0 | 3702 (116) | 3835 (116) | 3936 (150) | 3806 (115) | 3990 (167) | 0.22 |
| 25.0 to 29.9 | 3964 (79) | 3847 (80) | 3770 (92) | 3831 (81) | 3884 (107) | 0.54 |
| ≥30.0 | 3992 (125) | 3953 (115) | 3817 (115) | 4011 (93) | 4055 (119) | 0.62 |
| Potassium, mg/day | ||||||
| All men | 3196 (48) | 3190 (48) | 3249 (54) | 3111 (46) | 3150 (59) | 0.29 |
| Age | ||||||
| 25 to 39 | 3264 (72) | 3317 (72) | 3183 (90) | 3068 (77) | 3037 (112) | 0.02 |
| 40 to 54 | 3408 (88) | 3199 (85) | 3358 (92) | 3092 (76) | 3154 (98) | 0.03 |
| 55 to 74 | 2874 (87) | 3003 (89) | 3170 (91) | 3176 (78) | 3185 (89) | 0.005 |
| Education level | ||||||
| >High school | 3247 (94) | 3213 (96) | 3242 (116) | 3035 (100) | 3175 (62) | 0.13 |
| ≤High school | 3183 (55) | 3186 (63) | 3257 (59) | 3141 (50) | 3050 (149) | 0.73 |
| Body mass index | ||||||
| <25.0 | 3261 (95) | 3177 (99) | 3494 (123) | 3166 (94) | 3170 (137) | 0.59 |
| 25.0 to 29.9 | 3217 (64) | 3219 (65) | 3169 (74) | 3120 (66) | 3166 (85) | 0.32 |
| ≥30.0 | 3074 (90) | 3155 (83) | 3189 (83) | 3058 (68) | 3111 (86) | 0.94 |
Figure 1.
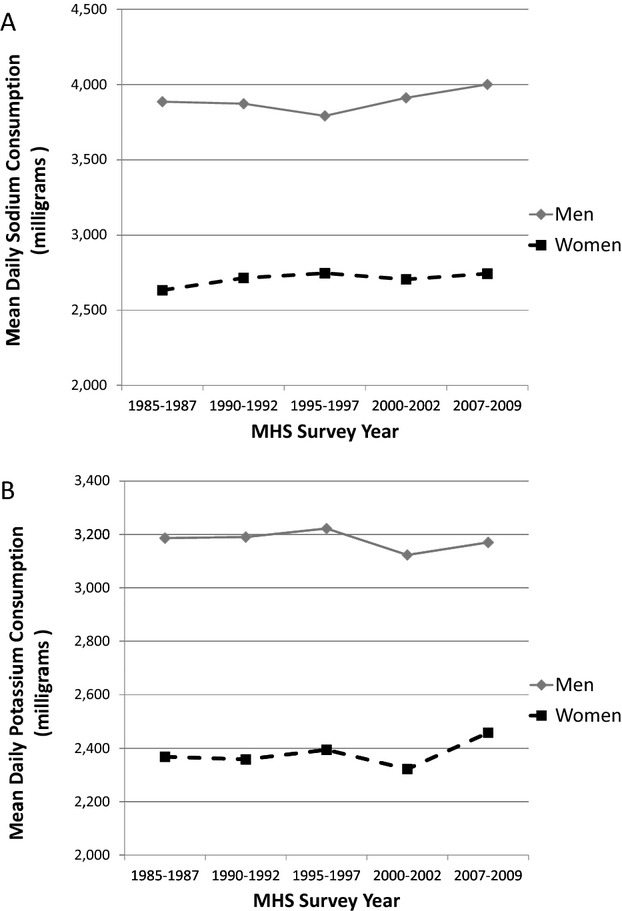
Sex‐specific age‐ and energy‐adjusted mean daily sodium (A) and potassium (B) consumption (mg), Minnesota Heart Survey (MHS), 1985–1987 through 2007–2009.
Among women, sodium intake increased over the study period in both age‐ (Table 3) and age‐ and energy‐adjusted analyses (Ptrend<0.05 for both; Figure 1, Table S2). Age‐adjusted mean sodium intake was lower among older compared with younger women: 2007–2009 age‐adjusted estimates ranged from 2519 among 55‐ to 74‐year‐olds to 3120 among 25‐ to 39‐year‐olds (P=0.003; Table 3). Age‐adjusted potassium intake also increased among women overall and in all subgroups (Table 3). On further adjustment for total energy consumption, however, potassium trends were generally attenuated (Table S2).
Table 3.
Age‐Adjusted Mean Intake of Sodium and Potassium (mg/day) for Women in the Minneapolis–St. Paul Metropolitan Area Aged 25 to 74: Minnesota Heart Survey, 1985–1987 Through 2007–2009
| Mean (SE) | P Value, Linear Trend | |||||
|---|---|---|---|---|---|---|
| 1985–1987 | 1990–1992 | 1995–1997 | 2000–2002 | 2007–2009 | ||
| Sodium, mg/day | ||||||
| All women | 2531 (43) | 2623 (42) | 2917 (47) | 2790 (41) | 2854 (51) | 0.001 |
| Age, y | ||||||
| 25 to 39 | 2695 (61) | 2774 (57) | 3005 (73) | 3056 (62) | 3120 (94) | 0.001 |
| 40 to 54 | 2598 (84) | 2646 (80) | 3040 (86) | 2777 (74) | 2868 (90) | 0.011 |
| 55 to 74 | 2202 (74) | 2334 (74) | 2603 (80) | 2450 (70) | 2519 (80) | 0.002 |
| Education level | ||||||
| >High school | 2575 (53) | 2632 (48) | 2885 (54) | 2793 (44) | 2908 (54) | 0.001 |
| ≤High school | 2447 (68) | 2588 (72) | 2971 (85) | 2802 (77) | 2687 (120) | 0.02 |
| Body mass index | ||||||
| <25.0 | 2578 (59) | 2659 (57) | 2972 (71) | 2761 (60) | 2770 (79) | 0.02 |
| 25.0 to 29.9 | 2486 (66) | 2542 (62) | 2800 (71) | 2721 (59) | 2915 (78) | 0.001 |
| ≥30.0 | 2494 (85) | 2637 (78) | 2909 (71) | 2854 (64) | 2892 (87) | 0.001 |
| Potassium, mg/day | ||||||
| All women | 2285 (36) | 2282 (35) | 2501 (39) | 2374 (35) | 2533 (42) | <0.0001 |
| Age, y | ||||||
| 25 to 39 | 2304 (48) | 2306 (45) | 2435 (57) | 2301 (49) | 2483 (74) | 0.06 |
| 40 to 54 | 2337 (60) | 2326 (56) | 2565 (61) | 2443 (50) | 2545 (65) | 0.004 |
| 55 to 74 | 2191 (60) | 2188 (60) | 2519 (65) | 2389 (56) | 2595 (64) | <0.0001 |
| Education level | ||||||
| >High school | 2371 (43) | 2352 (38) | 2517 (43) | 2422 (36) | 2562 (44) | 0.0007 |
| ≤High school | 2202 (60) | 2171 (62) | 2472 (72) | 2259 (66) | 2394 (97) | 0.05 |
| Body mass index | ||||||
| <25.0 | 2372 (51) | 2389 (50) | 2603 (60) | 2426 (52) | 2626 (67) | 0.003 |
| 25.0 to 29.9 | 2265 (54) | 2232 (51) | 2391 (59) | 2352 (49) | 2595 (64) | <0.0001 |
| ≥30.0 | 2169 (70) | 2174 (66) | 2485 (69) | 2334 (57) | 2345 (73) | 0.02 |
Over the 5 study periods, mean age‐adjusted intake of sodium and potassium among women was appreciably lower than men, a difference that appeared to be largely attributable to differences in energy intake. Estimates of sodium and potassium (in milligrams) per 1000 kilocalories were similar in men and women (Figure 2; Tables S3 and S4).
Figure 2.
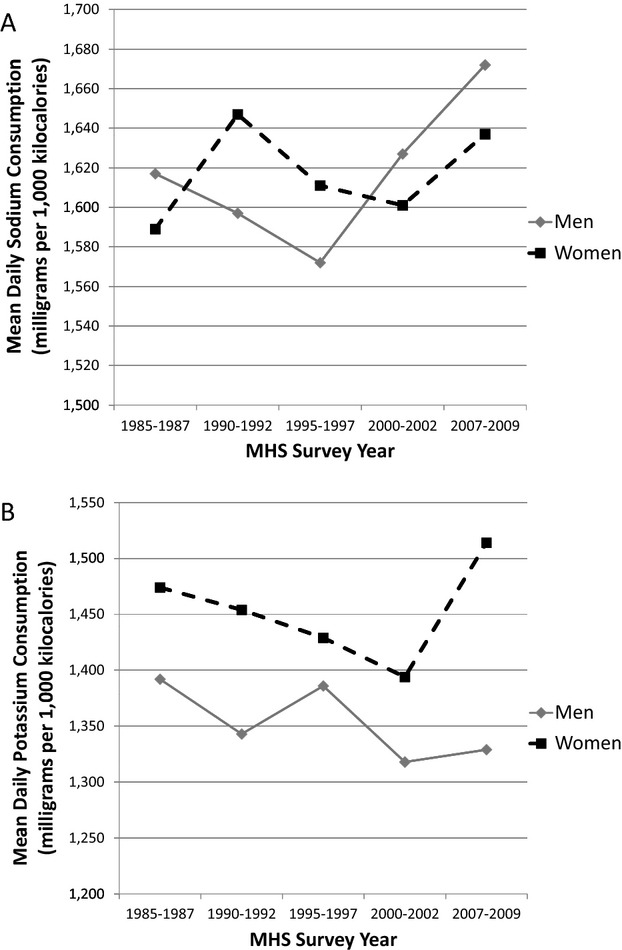
Sex‐specific mean daily sodium (A) and potassium (B) consumption (mg) per 1000 kilocalories, Minnesota Heart Survey (MHS), 1985–1987 through 2007–2009.
Discussion
We quantified long‐term trends in sodium and potassium consumption in a population‐based sample of adults. Over 22 years, mean dietary sodium intake was either stable or increased, depending on demographic subgroup, despite decades‐long public health efforts aimed at reducing sodium. In both men and women and within all subgroups of age, educational attainment, and BMI, current mean sodium intake exceeded the maximum recommended amount of 2300 mg/day for individuals, which has also been established as the upper limit for safe consumption.15 In all subgroups, potassium intake remained lower than the 4700 mg/day recommendation, with stable or increasing consumption over the 22‐year study period.
Few population‐based data exist to assess long‐term trends in sodium and potassium consumption. Among available studies, inconsistencies in dietary assessment, study samples, and analytic approaches may limit comparisons. A strength of the MHS data is the rigor and consistency of dietary assessment over the study period, particularly with respect to sodium. In comparison, the National Health and Nutrition Examination Survey (NHANES), which also assessed intake from 24‐hour dietary recall, instituted several changes that could affect estimates of consumption trends, including using different nutrient databases for different survey cycles and adding aids to improve participant recall.8
The most recent sodium consumption estimates from MHS and NHANES are remarkably similar, but there are apparent differences in subgroup trends. In the 2007–2008 NHANES, mean daily sodium consumption estimates were 4043 and 2884 mg/day for men and women ≥20 years of age, respectively,16 compared with 3968 and 2854 mg/day in the 2007–2009 MHS adult sample. However, in a recent NHANES study, sodium consumption declined between 1988–1994 and 2003–2008 in some age‐ and sex‐specific subgroups,4 whereas MHS showed increases for women and for some age groups among men. NHANES potassium consumption declined in all age and sex subgroups4; in MHS, potassium intake declined only among young men. Aside from changes in NHANES dietary assessment, there are several possible explanations for these differences. A notable difference is that NHANES includes a greater representation of nonwhite racial/ethnic groups than does MHS. Direct comparisons are also complicated by differences in survey administration years, age‐group cut points, and statistical adjustment. However, despite these differences, both MHS and NHANES show that population consumption of sodium has been and remains too high, whereas potassium consumption remains too low.
Several other US‐based studies of sodium, but not potassium, trends have been published. A national dietary survey conducted by General Mills suggested a small decline in overall mean sodium consumption between 1980–1982 and 1990–1992 because of estimated decreases in discretionary sodium consumption from salt added in cooking and at the table, whereas sodium from foods increased over the same period, particularly among women.9 As in MHS and NHANES data, mean daily sodium intake exceeded recommended levels, decreasing from 4047 to 3174 mg in 1990–1992. Sodium estimates in the General Mills study were derived from 14‐day food diaries of specific foods consumed that lacked information on food quantity. This assignment may not have accurately reflected sodium consumption. In addition, food and nutrient databases were changed in the last of 4 rounds of data collection.
A recent meta‐analysis of 24‐hour urinary sodium excretion estimates from studies published between 1957 and 2003 supported a small, statistically nonsignificant increase in sodium consumption over time.10 The use of urinary sodium excretion data provides a more precise estimate of sodium consumption compared with dietary reports, but study participants included in the meta‐analysis may not have been representative of the US population.
Much policy work has been directed at sodium consumption, but potassium has received little attention. Evidence indicates that dietary recommendations have not yielded desired changes in sodium and potassium intake levels, and the extensive public health efforts with respect to sodium reduction specifically have not been successful over the past 22 years. Other countries have achieved population reductions in sodium through a combination of public education, government regulations, and working with food production and preparation professionals.17–18 Between 75% and 80% of sodium consumed in the United States is estimated to derive from food that is commercially produced or prepared in restaurants,17,19–20 illustrating the importance of working with these industries in sodium‐reduction efforts. Importantly, evidence suggests that the removal of a substantial amount of salt from prepared foods can be acceptable to the population and need not result in compensatory intake.21–23
The prospects for universal sodium reduction strategies to yield substantial improvements in population health are supported by clinical and population data. A recent meta‐analysis of trial supported significant declines in blood pressure among both hypertensives (−7.1/3.9 mm Hg) and normotensives (−3.6/1.7 mm Hg) from 6 g lower salt consumption (2358 mg sodium).24 A simulation study estimated that sodium declines of 1200 mg/day would have large impacts on the incidence of coronary heart disease (annual reduction of between 60 000 and 120 000 cases), stroke (reduced by between 32 000 and 66 000), and deaths from any cause (between 44 000 and 92 000).25 In Finland, population‐level declines in sodium consumption have corresponded with temporal declines in blood pressure and mortality due to stroke and coronary heart disease.26
Although potassium has received less attention, studies show that achieving an adequate intake (AI) of potassium (4.7 g [120 mmol]/day for adults) may yield important health benefits.15 In a meta‐analysis of randomized trials, Geleijnse and colleagues27 found that a median increase in potassium intake of 44 mmol/day was associated with a 2.42 mm Hg lower (−3.75, −1.08) systolic and 1.57 mm Hg lower (−2.65, −0.50) diastolic blood pressure. A shift away from high‐sodium processed foods toward a diet rich in fruits and vegetables would have positive effects on both sodium and potassium consumption in the population. Furthermore, requiring potassium content be added to food labels would enable consumers to make informed choices.
Our study has strengths and limitations. The MHS employed consistent methods of dietary assessment and specifically probed for sodium‐containing foods throughout the 22‐year study period, along with regular updates of the nutrient database, including the sodium and potassium content of foods. It is possible that the Nutrition Coordinating Center database does not represent all changes in the food supply, but to our knowledge it stands as the most complete and consistent source of dietary nutrient data. In contrast, NHANES has undergone meaningful changes in dietary assessment over the same period, particularly during early data collection periods.
Limitations related to dietary assessment using the 24‐hour recall apply to both MHS and NHANES. In both, nutrient intake is likely underestimated because of underreporting of food intake—a well‐known shortcoming of self‐report dietary assessment methods, including the 24‐hour dietary recall methodology28—and the lack of data on salt added at the table, estimated to account for 5% of all sodium consumed.17,19–20 Underestimated intakes should not affect trends if the degree of bias does not change over time. We could not assess whether this bias has changed over time in either NHANES or MHS. However, it is possible that we were unable to detect true declines in table salt use. In addition, it could be speculated that the magnitude of underreporting has increased over time because BMI increased over time, and it is well known that overweight and obese people underreport consumption to a greater extent than healthy‐weight people.28 We note that in MHS energy intake appeared to increase among women, but not among men, mirroring our findings for nutrient consumption. National data support increased energy consumption,29 consistent with increases in BMI in the MHS sample.
Although day‐to‐day intraindividual variability in dietary intake is a concern when collecting a single 24‐hour recall, one 24‐hour recall is a valid measure of group mean nutrient intake.30 However, one 24‐hour recall will not enable us to distinguish within‐ and between‐person variability in consumption. Because within‐person variability is such a large component of variability in nutrient consumption, we cannot derive valid estimates of the overall population distribution.31 We were thus unable to present data on the percentage of the MHS sample who complied with sodium and potassium recommendations.
Participants in this study were predominantly white adults living in the Minneapolis–St. Paul metropolitan area, and it is possible that our estimates of absolute nutrient consumption or trends in intake may not represent those of other populations. However, as discussed, our estimates were very similar to those from national surveillance data (NHANES).
In summary, despite decades of dietary recommendations to limit intake, our data suggest that sodium intake has not declined over the past 22 years. Mean levels of sodium consumption exceeded the recommended upper limit for individuals of 2300 mg/day in all population subgroups examined. Furthermore, potassium consumption remains lower than the recommended 4700 mg/day. These data underscore the need for population‐based interventions, such as consumer education, improved product labeling, changes in food production and restaurant offerings, and increased incorporation of potassium‐related interventions.
Sources of Funding
Funding for this research was provided by award number 6R01‐HL‐23727 from the National Heart, Lung, and Blood Institute, NIH and award number T32‐HL‐07779 (PI: Aaron Folsom) from the National Heart, Lung, and Blood Institute, NIH.
Disclosures
None.
References
- 1.Adrogue HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med. 2007; 356:1966-1978 [DOI] [PubMed] [Google Scholar]
- 2.Cook NR, Obarzanek E, Cutler JA, Buring JA, Rexrode KM, Kumanyika SK, Appel LJ, Whelton PK. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: the Trials of Hypertension Prevention follow‐up study. Arch Intern Med. 2009; 169:32-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang Q, Liu T, Kuklina EV, Flanders WD, Hong Y, Gillespie C, Chang MH, Gwinn M, Dowling N, Khoury MJ, Hu FB. Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2011; 171:1183-1191 [DOI] [PubMed] [Google Scholar]
- 4.Cogswell ME, Zhang Z, Carriquiry AL, Gunn JP, Kuklina EV, Saydah SH, Yang Q, Moshfegh AJ. Sodium and potassium intakes among US adults: NHANES 2003–2008. Am J Clin Nutr. 2012; 96:647-657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 20107th edWashington, DC: U.S. Government Printing Office; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.U.S. Department of Agriculture and U.S. Department of Health and Human Services Dietary Guidelines for Americans, 1980. 19801st edWashington, DC: U.S. Government Printing Office [Google Scholar]
- 7.IOM Strategies to Reduce Sodium Intake in the United States. 2010Washington, DC: IOM; [PubMed] [Google Scholar]
- 8.Briefel RR, Johnson CL. Secular trends in dietary intake in the United States. Annu Rev Nutr. 2004; 24:401-431 [DOI] [PubMed] [Google Scholar]
- 9.Engstrom A, Tobelmann RC, Albertson AM. Sodium intake trends and food choices. Am J Clin Nutr. 1997; 652 suppl:704S-707S [DOI] [PubMed] [Google Scholar]
- 10.Bernstein AM, Willett WC. Trends in 24‐h urinary sodium excretion in the United States, 1957–2003: a systematic review. Am J Clin Nutr. 2010; 92:1172-1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luepker RV, Jacobs DR, Gillum RF, Folsom AR, Prineas RJ, Blackburn H. Population risk of cardiovascular disease: the Minnesota Heart Survey. J Chronic Dis. 1985; 38:671-682 [DOI] [PubMed] [Google Scholar]
- 12.Luepker RV, Jacobs DR, Jr, Folsom AR, Gillum RF, Frantz ID, Jr, Gomez O, Blackburn H. Cardiovascular risk factor change—1973–74 to 1980–82: the Minnesota Heart Survey. J Clin Epidemiol. 1988; 41:825-833 [DOI] [PubMed] [Google Scholar]
- 13.Schakel SF, Sievert YA, Buzzard IM. Sources of data for developing and maintaining a nutrient database. J Am Diet Assoc. 1988; 88:1268-1271 [PubMed] [Google Scholar]
- 14.Feskanich D, Sielaff BH, Chong K, Buzzard IM. Computerized collection and analysis of dietary intake information. Comput Methods Programs Biomed. 1989; 30:47-57 [DOI] [PubMed] [Google Scholar]
- 15.IOM (Institute of Medicine) Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. 2004Washington, DC: The National Academies Press [Google Scholar]
- 16.U.S. Department of Agriculture, Agricultural Research Service, Beltsville Human Nutrition Research Center, Food Surveys Research Group (Beltsville, MD) and U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics (Hyattsville, MD) Sodium Intake of the U.S. Population: What We Eat In America, NHANES 2007–2008. Food Surveys Research Group, Dietary Data Brief No. 8; 2011, October. Available at: http://ars.usda.gov/Services/docs.htm?docid=19476 Accessed January 14, 2012.
- 17.He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009; 23:363-384 [DOI] [PubMed] [Google Scholar]
- 18.Reinivuo H, Valsta LM, Laatikainen T, Tuomilehto J, Pietinen P. Sodium in the Finnish diet: II trends in dietary sodium intake and comparison between intake and 24‐h excretion of sodium. Eur J Clin Nutr. 2006; 60:1160-1167 [DOI] [PubMed] [Google Scholar]
- 19.Mattes RD, Donnelly D. Relative contributions of dietary sodium sources. J Am Coll Nutr. 1991; 10:383-393 [DOI] [PubMed] [Google Scholar]
- 20.Havas S, Roccella EJ, Lenfant C. Reducing the public health burden from elevated blood pressure levels in the United States by lowering intake of dietary sodium. Am J Public Health. 2004; 94:19-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beauchamp GK, Bertino M, Engelman K. Failure to compensate decreased dietary sodium with increased table salt usage. JAMA. 1987; 258:3275-3278 [PubMed] [Google Scholar]
- 22.Adams SO, Maller O, Cardello AV. Consumer acceptance of foods lower in sodium. J Am Diet Assoc. 1995; 95:447-453 [DOI] [PubMed] [Google Scholar]
- 23.Bolhuis DP, Temme EH, Koeman FT, Noort MW, Kremer S, Janssen AM. A salt reduction of 50% in bread does not decrease bread consumption or increase sodium intake by the choice of sandwich fillings. J Nutr. 2011; 141:2249-2255 [DOI] [PubMed] [Google Scholar]
- 24.He FJ, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta‐analysis of randomized trials. Implications for public health. J Hum Hypertens. 2002; 16:761-770 [DOI] [PubMed] [Google Scholar]
- 25.Bibbins‐Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, Goldman L. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010; 362:590-599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karppanen H, Mervaala E. Sodium intake and hypertension. Prog Cardiovasc Dis. 2006; 49:59-75 [DOI] [PubMed] [Google Scholar]
- 27.Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomized trials. J Hum Hypertens. 2003; 17:471-480 [DOI] [PubMed] [Google Scholar]
- 28.Johnson RK, Soultanakis RP, Matthews DE. Literacy and body fatness are associated with underreporting of energy intake in US low‐income women using the multiple‐pass 24‐hour recall: a doubly labeled water study. J Am Diet Assoc. 1998; 98:1136-1140 [DOI] [PubMed] [Google Scholar]
- 29.Nielsen SJ, Siega‐Riz AM, Popkin BM. Trends in energy intake in U.S. between 1977 and 1996: similar shifts seen across age groups. Obes Res. 2002; 10:370-378 [DOI] [PubMed] [Google Scholar]
- 30.Bingham SA, Gill C, Welch A, Day K, Cassidy A, Khaw KT, Sneyd MJ, Key TJ, Roe L, Day NE. Comparison of dietary assessment methods in nutritional epidemiology: weighed records v. 24 h recalls, food‐frequency questionnaires and estimated‐diet records. Br J Nutr. 1994; 72:619-643 [DOI] [PubMed] [Google Scholar]
- 31.Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, Guenther PM, Krebs‐Smith SM, Subar AF, Dodd KW. A mixed‐effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med. 2010; 29:2857-2868 [DOI] [PMC free article] [PubMed] [Google Scholar]


