Abstract
Importance
Many early life risk factors for childhood obesity are more prevalent among blacks and Hispanics than among whites and may explain the higher prevalence of obesity among racial/ethnic minority children.
Objective
To examine the extent to which racial/ethnic disparities in adiposity and overweight are explained by differences in pregnancy (gestational diabetes and depression), infancy (rapid infant weight gain, non-exclusive breastfeeding, early introduction of solid foods) and early childhood (sleeping less than 12 hours/day, presence of a television in the bedroom, any intake of sugar-sweetened beverages, and any intake of fast food) risk factors.
Design
Prospective, pre-birth cohort study.
Setting
Multi-site group practice in Massachusetts.
Participants
1116 (63% white, 17% black, and 4% Hispanic) mother-child pairs.
Main Exposure
Mother’s report of child’s race/ethnicity.
Main Outcome Measures
Age- and sex-specific body mass index (BMI) z-score, total fat mass index (FMI) from dual-energy X-ray absorptiometry, and overweight/obesity defined as a BMI ≥ 85th percentile at age 7.
Results
Black (0.48 units [95% CI: 0.31, 0.64]) and Hispanic (0.43 [0.12, 0.74]) children had higher BMI z-scores, as well as higher total FMI and overweight/obesity prevalence, than white children. After adjusting for socioeconomic confounders and parental BMI, differences in BMI z-score were attenuated for blacks (0.22 [0.05, 0.40]) and Hispanics (0.22 [−0.08, 0.52]). Adjustment for pregnancy risk factors did not substantially change these estimates. However, after further adjustment for infancy and childhood risk factors, we observed only minimal differences in BMI z-score for whites, blacks (0.07 [−0.11, 0.26]) and Hispanics (0.04 [−0.27, 0.35]). We observed similar attenuation of racial/ethnic differences in adiposity and overweight/obesity prevalence.
Conclusions and Relevance
Racial/ethnic disparities in childhood adiposity and obesity are determined by factors operating in infancy and early childhood. Efforts to reduce obesity disparities should focus on preventing early life risk factors.
Keywords: Obesity, Race/Ethnicity, Pregnancy, Infancy, Childhood, Prevention
INTRODUCTION
In the past three decades, rates of overweight and obesity among children have substantially increased worldwide with all but the poorest countries now struggling with a high prevalence of obesity and its related non-communicable diseases.1 In the United States (US) alone, the prevalence of overweight and obesity in children and adolescents is about one-third.2-4 While childhood overweight and obesity rates may have plateaued in some US population subgroups, such as non-Hispanic whites and those of higher socioeconomic status, overall rates remain high and racial/ethnic and socioeconomic disparities appear to be widening.5-8
There is growing evidence that risk factors in the prenatal period and early childhood are crucial to the development – and thus prevention - of obesity and its consequences. Epidemiologic studies suggest that adverse exposures such as intrauterine exposure to maternal smoking, excessive weight gain or elevated glucose levels, and in early childhood, rapid infant weight gain, poor feeding practices, too much screen time, and short sleep duration, may increase short- and long-term risks for obesity and its sequelae.9-26 For these reasons the 2010 White House Task Force Report, Solving the Problem of Childhood Obesity Within a Generation,27 and two Institute of Medicine (IOM) reports emphasize both the role of early life risk factors in obesity development and the need for interventions in early life to prevent obesity.28,29
Research has shown that racial/ethnic and socioeconomic disparities exist across most known risk factors for childhood obesity from the prenatal period through childhood. In a recent study 30 we found that children from racial/ethnic minority groups had higher prevalence of several early life risk factors for obesity than did their white counterparts. Among blacks and Hispanics during pregnancy, these included higher rates of maternal depression; in infancy more rapid weight gain, lower rates of exclusive breastfeeding, lower proportions sleeping at least 12 hours/day, higher likelihood of introducing solid foods before 4 months of age, and after age 2 years, higher prevalence of having televisions in their bedrooms, higher intake of sugar-sweetened beverages, and higher intake of fast food. These differences may very well explain the observed racial/ethnic disparities in elevated adiposity and prevalence of overweight and obesity as children grow up, but no study has yet explored this hypothesis.
The purpose of this study was to examine the extent to which racial/ethnic disparities in childhood adiposity and overweight and obesity among a cohort of school-age children are explained by differences in pregnancy, infancy, and early childhood risk factors.
METHODS
Subjects/Study Design
Study subjects were participants in Project Viva, a prospective, pre-birth cohort study that recruited women during early pregnancy from Harvard Vanguard Medical Associates, a multi-specialty group practice in eastern Massachusetts.31 Details of recruitment and retention procedures are available elsewhere.31 Of the 2128 women who delivered a live infant, 1579 were eligible for 7-year follow up of whom 1116 attended a 7-year in-person visit.
After obtaining informed consent, we performed in-person study visits with the mother at the end of the first and second trimesters of pregnancy, and with mom and child in the first few days after delivery and at 6 months, 3 and 7 years after birth. Mothers completed mailed questionnaires at 1, 2, 4, 5, and 6 years after birth. Institutional Review Boards of Harvard Pilgrim Health Care, Brigham and Women’s Hospital, and Beth Israel Deaconess Medical Center approved the study protocols.
Measurements
Main Exposure
At the 3-year interview, research assistants asked mothers the question, “Which of the following best describes your child’s race or ethnicity?” Mothers had a choice of 1 or more of the following racial/ethnic groups: Hispanic or Latina, white or Caucasian, black or African American, Asian or Pacific Islander, American Indian or Alaskan Native, and other (please specify). For the participants who chose the “other” race/ethnicity, we compared the specified responses to US census definitions for the other 5 race and ethnicities and reclassified them where appropriate.
Outcome Measures
We measured height and weight of children using a calibrated stadiometer (Shorr Productions, Olney, MD) and scale (Seca model 881, Seca corporation, Hanover, MD). We calculated age- and sex-specific BMI z-scores using US national reference data.32 We defined overweight or obese as a BMI for age and sex ≥ 85th percentile.32 At age 7 years, we also measured total fat using dual-energy X-ray absorptiometry (DXA) and calculated fat mass index (FMI–kg/m2), waist circumference (cm) using a Lefkin woven tape, and subscapular and triceps skinfold thicknesses using Holtain calipers (Holtain LTD, Crosswell, United Kingdom), and calculated the sum (SS+TR) of the two thicknesses. Research assistants performing all measurements followed standardized techniques 33, and participated in in-service training to ensure measurement validity (IJ Shorr, Shorr Productions, Olney, MD). Inter- and intra-rater measurement error were well within published reference ranges for all measurements.34
Intermediates: Early Life Risk Factors
The main intermediates were risk factors during pregnancy, infancy, and early childhood that are associated with childhood obesity in the medical literature and that were significantly more prevalent among black and Hispanic children than their white counterparts in our previous Project Viva analysis of obesity-related risk factors.30
In pregnancy, these risk factors included (1) gestational diabetes, defined as 2 or more abnormal fasting glucose tolerance test results at 26-28 weeks of gestation based on published criteria;35 and (2) maternal depression in the second trimester of gestation defined as a score of 13 or more on the Edinburgh Postpartum Depression Scale.36 We did not include gestational weight gain or smoking during pregnancy because our earlier study did not show racial/ethnic differences in either after adjusting for maternal socioeconomic characteristics.
In infancy, risk factors included (1) rapid infant weight gain defined as being in the highest quartile of change in weight-for-age z-score between birth and 6 months based on US reference data;32 (2) early introduction of solid foods defined as introduction of complementary foods before 4 months of age; and (3) non-exclusive breastfeeding defined as mixed breast and formula feeding, weaned, or formula-feeding only in the first 6 months of life.
Early childhood risk factors (1-3 years of age) included (1) insufficient sleep defined as sleeping < 12 hours/day from 6 months to 2 years of age;9 (2) any sugar sweetened beverage intake at age 2 years defined as intake of soda (other than sugar-free), flavored milks, and fruit drinks (Hi-C, Kool-Aid, lemonade) 37; (3) any intake of fast food 38 at age 3 years; and (4) television in the bedroom defined as mother’s report of a TV in the room where their child sleeps at age 4 years.
Confounding Factors
We also collected information about maternal age, education, parity, and household income. Mothers reported their pre-pregnancy weight and height as well as fathers’ weight and height, from which we calculated their BMIs.
Statistical Analysis
We first examined bivariate relationships between child race/ethnicity and each risk factor, covariate, and our anthropometric outcome. We then used multivariable linear or logistic regression models to examine the association between child’s race/ethnicity and our anthropometric outcomes with and without the inclusion of confounders or early life risk factors. Our first model, Model 1, was adjusted for child age and sex only. We then additionally adjusted the multivariable models for potential confounders including socioeconomic variables (Model 2) and maternal and paternal BMI (Model 3). In subsequent models, we adjusted for risk factors during pregnancy– gestational diabetes and depression (Model 4); during infancy– rapid infant weight gain, non-exclusive breastfeeding, early introduction of solid foods (Model 5), and during early childhood– sleeping less than 12 hours/day, presence of a television in the bedroom, any intake of sugar-sweetened beverages, and any intake of fast food (Model 6).
The confounding and intermediate variables were not observed on all subjects. Using only subjects with all data observed would have resulted in a smaller sample size; most of those lost to analysis would have been missing only one or two values. Reducing the sample in this manner loses information and can result in a selected subset. We therefore used multiple imputation to include the information known about subjects with missing values. 39,40
In the multiple imputation process, a model is used to generate or “impute” a plausible value that might have been observed for each missing datum; this process incorporates known variability in the data. A “completed” data set comprises the observed data and one imputed value for each missing datum. The analysis is then performed using this “completed” data set. Next these initial imputed values are discarded and a new set of imputed values, i.e., a new completed data set, is generated, and the analysis is performed in the new completed data set. After several repetitions of this process, the analysis results–here, parameter estimates–are then combined in a structured fashion that accurately reflects the true amount of information in the observed data. The advantage of this process is that it does not erroneously presume that any of the imputed values are known true values. Instead, the information in partially observed subjects is recovered, relative to discarding those subjects, as is typically performed. Theory about and experience using multiple imputation show that: the results can be unbiased; confidence limits can be narrower; and avoiding the selection bias implied by using complete cases can meaningfully change parameter estimates.41 We generated 50 complete data sets and combined multivariable modeling results (Proc MI ANALYZE) in SAS version 9.3 (SAS Institute, Cary NC).
From these multiple imputation results, we report adjusted differences estimated from regressions and 95% confidence intervals for black and Hispanic compared with non-Hispanic white children as the reference group.
RESULTS
Consistent with national statistics, we found that compared with non-Hispanic white children, black and Hispanic children had substantially higher BMI z-scores, DXA total fat mass index, and prevalence of overweight and obesity at age 7 years (Table 1). Waist circumference and sum of subscapular and triceps skinfold thicknesses were all higher among black and Hispanic children than non-Hispanic white children. Because of the significant heterogeneity among the children of multiracial or other race/ethnicity group and because we did not observe differences in BMI z-score or childhood overweight or obesity prevalence among these children compared to non-Hispanic white children in our study, we only report all subsequent results for black and Hispanic children v. non-Hispanic white children. With the exception of excessive gestational weight gain, we observed that all of the early life risk factors we measured were more prevalent among blacks and Hispanics than among non-Hispanic whites (Table 2).
Table 1.
Selected Parent and Child Characteristics According to Child Race/Ethnicity. Data from 1116 Mother-Child Pairs from Project Viva.
| Maternal, Paternal, and Household Characteristics |
White, non- Hispanic (63%) |
Black, non- Hispanic (17%) |
Hispanic or Latino (4%) |
Other (16%) |
|
|---|---|---|---|---|---|
| % or Mean (SE) | P-value | ||||
| Maternal age, years | 33.4 (0.16) | 28.9 (0.49) | 28.9 (0.93) | 30.8 (0.44) | <.0001 |
| Maternal pre-pregnancy BMI, kg/m2 | 24.0 (0.17) | 27.3 (0.52) | 25.5 (0.81) | 24.6 (0.40) | <.0001 |
| Paternal BMI, kg/m2 | 26.4 (0.14) | 26.9 (0.35) | 27.3 (0.58) | 25.8 (0.33) | 0.05 |
| Education, college graduate or more, % | 80.3 | 38.8 | 21.1 | 60.3 | <.0001 |
| Parity, Nulliparous, % | 49.4 | 42.7 | 35.1 | 48.3 | 0.15 |
| Annual household income > $70,000, % | 73.3 | 25.1 | 23.1 | 56.8 | <.0001 |
| Child Characteristics | |||||
| Girl, % | 51.9 | 45.5 | 36.8 | 50.1 | 0.15 |
|
Anthropometric Characteristics at
Age 7 years |
|||||
| Body mass index z-score | 0.29 (0.04) | 0.79 (0.08) | 0.74 (0.15) | 0.29 (0.08) | |
| Sum of subscapular and triceps skinfold thickness, mm |
18.7 (0.31) | 23.5 (0.98) | 21.9 (1.70) | 20.2 (0.79) | <.0001 |
| Dual-energy X-ray absorptiometry total fat mass index, kg/m2 |
4.26 (0.06) | 5.01 (0.20) | 4.96 (0.33) | 4.41 (0.15) | <.0001 |
| Waist circumference, cm | 59.2 (0.26) | 63.3 (0.84) | 62.1 (1.32) | 59.4 (0.68) | <.0001 |
| BMI ≥ 85th percentile | 21.2 | 39.9 | 39.7 | 24.7 | <.0001 |
| BMI ≥ 95th percentile | 7.2 | 27.3 | 25.4 | 13.0 | <.0001 |
Table 2.
Early Life Risk Factors for Childhood Obesity According to Child Race/Ethnicity. Data from 1116 Mother-Child Pairs from Project Viva.
| Early Life Risk Factors for Childhood Obesity | White, non- Hispanic |
Black, non- Hispanic |
Hispanic or Latino |
P- value |
|---|---|---|---|---|
| Pregnancy exposures | % | |||
| Excessive gestational weight gain | 59.9 | 58.2 | 52.7 | 0.16 |
| Gestational diabetes | 4.6 | 5.2 | 5.2 | 0.99 |
| Mother smoked during early pregnancy | 7.8 | 13.5 | 16.3 | 0.01 |
| Antenatal depression | 6.4 | 15.6 | 20.8 | 0.001 |
| Infancy exposures | ||||
| Highest quartile of change in weight-for-age between birth and 6 months* |
20.5 | 36.8 | 39.7 | 0.0002 |
| Not exclusively breastfed at 6 months | 68.6 | 81.5 | 88.3 | 0.001 |
| Introduction of solids prior to 4 months | 13.1 | 33.9 | 41.2 | <.0001 |
| Early childhood exposures | ||||
| Average daily sleep duration 6m – 2y, < 12 hours (%) | 69.8 | 39.6 | 35.9 | <.0001 |
| Any sugar sweetened beverage intake at 2 years | 46.3 | 84.4 | 81.3 | <.0001 |
| Any fast food intake at 3 years | 64.5 | 80.9 | 83.7 | <.0001 |
| Television in room where child sleeps at 4 years | 6.4 | 52.8 | 61.2 | <.0001 |
Rapid infant weight gain defined as being in the highest quartile of change in weight-for-age z-score between birth and 6 months based on US reference data.
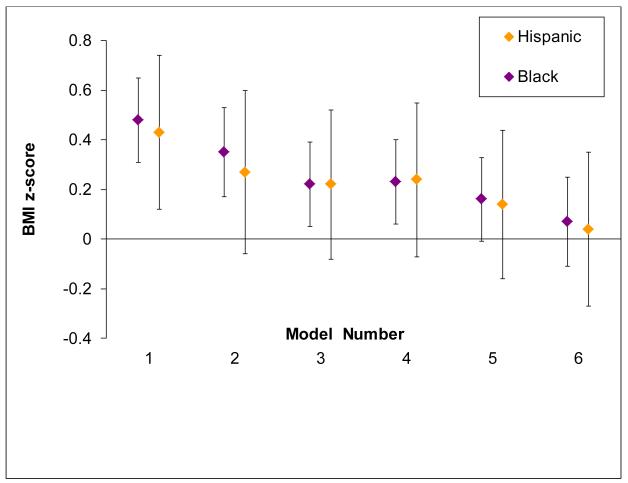
In models adjusted only for child age and sex, BMI z-score was higher among black (0.48 units; 95% CI: 0.31, 0.64) and Hispanic children (0.43 units; 95% CI: 0.12, 0.74) than non-Hispanic white children (Table 3 and Figure). After adjusting for socioeconomic confounders and parental BMI, these differences were attenuated for blacks (0.22 [0.05, 0.40]) and Hispanics (0.22 [−0.08, 0.52]). Adjustment for pregnancy risk factors did not substantially change these estimates among blacks (0.23 [0.06, 0.40]) and Hispanics (0.24 [−0.07, 0.54]). However, after further adjustment for infancy and early childhood risk factors, we observed only minimal differences in BMI z-score for whites, blacks (0.07 [−0.11, 0.26]) or Hispanics (0.04 [−0.27, 0.35]). Each infancy and early childhood risk factor contributed to explaining the observed racial/ethnic differences. The degree of attenuation ranged from 10% after adjustment for having a TV in the bedroom to 23% after adjustment for rapid infant weight gain (Data not shown).
Table 3.
Anthropometric Outcomes at Age 7 According to Child Race/Ethnicity, before and after adjustment for Confounders and Early Life Risk Factors for Obesity
| Multivariable Models*: | White, non-Hispanic |
Black, non-Hispanic |
Hispanic |
|---|---|---|---|
| BMI z-score | Estimated difference (95% Confidence Interval) | ||
| Model 1. Child age and sex | 0.0 (Ref) | 0.48 (0.31, 0.64) | 0.43 (0.12, 0.74) |
| Model 2. Model 1 + Socioeconomic factors | 0.0 (Ref) | 0.35 (0.17, 0.53) | 0.27 (−0.06, 0.59) |
| Model 3. Model 2 + Parental BMI | 0.0 (Ref) | 0.22 (0.05, 0.40) | 0.22 (−0.08, 0.52) |
| Model 4. Model 3 + Pregnancy factors | 0.0 (Ref) | 0.23 (0.06, 0.40) | 0.24 (−0.07, 0.54) |
| Model 5. Model 4 + Infancy factors | 0.0 (Ref) | 0.16 (−0.01, 0.33) | 0.14 (−0.16, 0.44) |
| Model 6. Model 5 + Early childhood factors | 0.0 (Ref) | 0.07 (−0.11, 0.26) | 0.04 (−0.27, 0.35) |
| SS + TR skinfold thickness, mm | |||
| Model 1. Child age and sex | 0.0 (Ref) | 3.95 (2.43, 5.47) | 2.93 (0.02, 5.85) |
| Model 2. Model 1 + Socioeconomic factors | 0.0 (Ref) | 2.64 (0.96, 4.32) | 1.20 (−1.84, 4.24) |
| Model 3. Model 2 + Parental BMI | 0.0 (Ref) | 1.56 (−0.04, 3.16) | 0.81 (−2.07, 3.68) |
| Model 4. Model 3 + Pregnancy factor | 0.0 (Ref) | 1.57 (−0.03, 3.18) | 0.84 (−2.05, 3.74) |
| Model 5. Model 4 + Infancy factor | 0.0 (Ref) | 1.01 (−0.60, 2.61) | −0.01 (−2.89, 2.86) |
| Model 6. Model 5 + Early childhood factors | 0.0 (Ref) | 0.25 (−1.46, 1.97) | −0.86 (−3.83, 2.11) |
| DXA total fat mass index, kg/m 2 | |||
| Model 1. Child age and sex | 0.0 (Ref) | 0.66 (0.35, 0.97) | 0.72 (0.13, 1.30) |
| Model 2. Model 1 + Socioeconomic factors | 0.0 (Ref) | 0.42 (0.07, 0.76) | 0.39 (−0.22, 1.00) |
| Model 3. Model 2 + Parental BMI | 0.0 (Ref) | 0.18 (−0.14, 0.51) | 0.31 (−0.27, 0.89) |
| Model 4. Model 3 + Pregnancy factor | 0.0 (Ref) | 0.19 (−0.14, 0.51) | 0.33 (−0.26, 0.91) |
| Model 5. Model 4 + Infancy factor | 0.0 (Ref) | 0.08 (−0.25, 0.40) | 0.16 (−0.43, 0.74) |
| Model 6. Model 5 + Early childhood factors | 0.0 (Ref) | −0.05 (−0.40, 0.30) | 0.02 (−0.59, 0.62) |
| Waist circumference, cm | |||
| Model 1. Child age and sex | 0.0 (Ref) | 2.85 (1.57, 4.13) | 1.89 (−0.54, 4.31) |
| Model 2. Model 1 + Socioeconomic factors | 0.0 (Ref) | 2.13 (0.71, 3.55) | 0.94 (−1.59, 3.48) |
| Model 3. Model 2 + Parental BMI | 0.0 (Ref) | 1.09 (−0.25, 2.43) | 0.60 (−1.78, 2.99) |
| Model 4. Model 3 + Pregnancy factor | 0.0 (Ref) | 1.11 (−0.23, 2.45) | 0.65 (−1.74, 3.04) |
| Model 5. Model 4 + Infancy factor | 0.0 (Ref) | 0.66 (−0.69, 2.00) | −0.01 (−2.39, 2.38) |
| Model 6. Model 5 + Early childhood factors | 0.0 (Ref) | 0.12 (−1.32, 1.56) | −0.61 (−3.07, 1.85) |
|
Overweight or Obesity (BMI ≥ 85th v. < 85th
percentile) |
Odds Ratio (95% Confidence Interval) | ||
| Model 1. Child age and sex | 1.0 (Ref) | 2.35 (1.69, 3.34) | 2.34 (1.22, 4.51) |
| Model 2. Model 1 + Socioeconomic factors | 1.0 (Ref) | 2.03 (1.36, 3.02) | 1.92 (0.96, 3.84) |
| Model 3. Model 2 + Parental BMI | 1.0 (Ref) | 1.67 (1.09, 2.56) | 1.88 (0.89, 3.94) |
| Model 4. Model 3 + Pregnancy factor | 1.0 (Ref) | 1.71 (1.12, 2.62) | 1.95 (0.92, 4.14) |
| Model 5. Model 4 + Infancy factor | 1.0 (Ref) | 1.54 (1.00, 2.39) | 1.69 (0.78, 3.67) |
| Model 6. Model 5 + Early childhood factors | 1.0 (Ref) | 1.35 (0.84, 2.16) | 1.46 (0.65, 3.28) |
Model 1 is adjusted for child age and sex; Model 2 is further adjusted for maternal age, education, parity, and household income; Model 3 is further adjusted for maternal and paternal BMI; Model 4 is adjusted for gestational diabetes and 2nd trimester depression; Model 5 is further adjusted for highest quartile of change in weight-for-age between birth and 6 months, not exclusively breastfeeding, introduction of solids < 4 months; Model 6 is further adjusted for insufficient sleep, having a TV in the bedroom, sugar sweetened beverage intake, and fast food intake.
Figure. Body Mass Index Z-Score at Age 7 Years among Black and Hispanic Children compared to White Children (Reference Group) before and after adjustment for Confounders and Early Life Risk Factors for Obesity.
Model 1 is adjusted for child age and sex; Model 2 is further adjusted for the confounders maternal age, education, parity, and household income; Model 3 is further adjusted for the confounders maternal and paternal BMI; Model 4 is adjusted for the pregnancy factors gestational diabetes and 2nd trimester depression; Model 5 is further adjusted for the infant factors highest quartile of change in weight-for-age between birth and 6 months, not exclusively breastfeeding, introduction of solids < 4 months; Model 6 is further adjusted for the early childhood factors insufficient sleep, having a TV in the bedroom, sugar sweetened beverage intake, and fast food intake.
We observed similar patterns of attenuation by socioeconomic factors, parental BMI, and infancy and early childhood risk factors for all of our anthropometric outcomes (Table 3). However, the degree of attenuation of racial/ethnic disparities in prevalence of overweight or obesity was less than that observed for BMI z-score. For example, in models adjusted for socioeconomic factors and parental BMI, the odds ratio of overweight or obesity was higher among black (1.67; 95% CI: 1.09, 2.56) and Hispanic children (OR 1.88; 95% CI: 0.89, 3.94) than non-Hispanic white children. After adjustment for infancy and early childhood risk factors, the odds of overweight or obesity was attenuated to 1.35 (95% CI: 0.84, 2.16) among black children and 1.46 (95% CI: 0.65, 3.28) among Hispanic children.
DISCUSSION
In this prospective pre-birth cohort, we found that at age 7 years, overweight and obesity prevalence among black and Hispanic children was almost double the prevalence of white children. The observed racial/ethnic disparities in adiposity and overweight or obesity prevalence were partially but not entirely explained by confounding by socioeconomic factors and parental obesity. While adjustment for obesity risk factors during pregnancy did not substantially change our observed associations, after adjustment for infancy and early childhood risk factors we observed only small differences in BMI z-score among non-Hispanic white, black, and Hispanic children.
Our findings suggest that racial/ethnic disparities in childhood obesity may be explained by factors operating in infancy and early childhood, and that if differences in these factors could be eliminated, so might the disparities in childhood obesity. These factors include differences in modifiable early feeding behaviors such as breastfeeding and timing of introduction of solid foods, accelerated infant weight gain, and early childhood obesity-related risk factors including insufficient sleep, having a TV in a child’s bedroom, and consumption of sugar sweetened beverages and fast food; all of which have been found in previous studies to be more prevalent among blacks and Hispanics than among whites.30,42,43,44,45,46 In our study, adjustment for obesity-related risk factors in infancy and early childhood attenuated the observed differences in BMI z-score between blacks and whites by as much as 69% and between Hispanics and whites by as much as 83%. Perhaps more complete measurement of infancy and childhood risk factors could attenuate the difference still further. Thus, our study implies that interventions to modify early life risk factors may have a large impact on reducing disparities in childhood obesity prevalence.
Substantial evidence suggests that the best times in the lifecourse to prevent obesity are in infancy and early childhood when behaviors are modifiable and/or physiology is plastic.47 The infancy and early childhood periods seem particularly promising and highly sensitive to interventions – there are multiple settings to access parents (e.g. primary care, child care, early education settings, etc), and parents and caregivers are highly sensitized to the child’s needs. Habits and tastes develop early in children and thus establishing the tastes for a variety of foods, enjoying active play, and good sleep habits are all critical for future healthy behavioral patterns. Despite the growing evidence for the potential role of early life interventions for childhood obesity, a recent review of interventions to prevent or treat overweight among children under the age of 2 yielded only ten published studies of poor or fair quality.48 In addition, national funding initiatives continue to exclude children under the age of 2 years, a missed opportunity for both obesity prevention and reduction of related racial/ethnic disparities. For example, in 2011 the Centers for Disease Control and Prevention awarded approximately $18 million to fund the Childhood Obesity Research Demonstration grants to prevent and reduce obesity among children ages 2 to 12 years who are covered by the Children’s Health Insurance Program – a program which provides low cost health insurance to children from working families.
Similar to previous studies, we found that socioeconomic factors confounded the observed associations between race/ethnicity and our anthropometric outcomes. Adjustment for parental and household socioeconomic factors attenuated the observed difference in BMI z-score between blacks and whites by about 27% and between Hispanics and whites by 37%. Previous studies among both children49 and adults50 have examined the extent to which racial/ethnic disparities in obesity are confounded or explained by socioeconomic status. In a study of 8984 children ages 12 to 17 years participating in the National Longitudinal Study of Youth, Powell et al.49 found that although parental income and mother’s education partially explained observed black-white and Hispanic-white differences in BMI, a large portion of the racial/ethnic differences in BMI remained unexplained. In a study of 4,356 US adults from the 1994-1996 Continuing Survey of Food Intakes by Individuals and the Diet and Health Knowledge Survey, Wang et al.50 found that black-white differences in risk of overweight and obesity was reduced by 38% after adjustment for education and income; partially explaining observed black-white differences. Overall, our findings and those in the published literature suggest that social conditions and their effects on children’s environments are important for partially understanding the origins of disparities in childhood obesity.
In this study, we considered maternal and paternal BMI to be confounders of the relationship between race/ethnicity and obesity. It is also possible however, that parental BMI could be an upstream variable in the association between race/ethnicity and obesity. Thus, obesity-related behaviors by overweight or obese parents could influence early life behaviors and physiologic programming in utero or in early childhood which could lead to unhealthy weight trajectories among their offspring.51 In our study, maternal and parental BMI partially explained the observed gaps among blacks, Hispanics, and whites. Our findings emphasize the importance of intergenerational effects on obesity and the need for interventions to interrupt the cycle of obesity in families.
Strengths of our study included having prospectively collected data on a wide range of risk factors extending from pregnancy through early childhood, objectively measured weights, heights, and anthropometry, and the ability to adjust for several important confounding socioeconomic factors. The study also had several potential limitations. First, although we used validated survey items, most of our exposure measures were from self report. These factors could have introduced social desirability bias as participants could exaggerate self-reported behaviors. However, we have no reason to believe that self-report of behaviors would differ by racial/ethnic group. Second, although we studied many risk factors for childhood obesity that had plausible hypotheses, we did not measure others such as lifestyle, cultural, or environmental determinants of dietary and sedentary practices. It is possible that the incomplete measure of other important infancy and early childhood risk factors or incomplete adjustment for residual confounders could have explained why we were not able to entirely explain all of the racial/ethnic disparities in overweight and obesity prevalence. Third, our sample size for Hispanics was small and confidence intervals for some estimates were wide. However, the observed effect estimates of BMI z-score for blacks and Hispanics were almost identical lending support to our conclusions for both groups.
CONCLUSION
Obesity is disproportionately prevalent among racial/ethnic minority children6 and recent trends suggest these disparities are widening.5 Our findings suggest that modifiable risk factors throughout the lifecourse,52 including factors during infancy and early childhood, as well as social conditions in childhood and trans-generational obesity, are critical to understanding how disparities in childhood obesity arise. They also imply that efforts to eliminate racial/ethnic disparities in childhood obesity should focus on preventing these early life risk factors within the socio-environmental context in which they occur.
ACKNOWLEDGEMENTS
Dr. Taveras had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Taveras EM; Acquisition of data: Gillman MW, Rifas-Shiman SL. Analysis and interpretation of data: Taveras EM, Rifas-Shiman SL, Kleinman K, Rich-Edwards J, Gillman MW; Drafting of manuscript: Taveras EM; Critical revision of the manuscript for important intellectual content: Taveras EM, Rifas-Shiman SL, Kleinman K, Rich-Edwards J, Gillman MW; Statistical analysis: Rifas-Shiman SL; Obtained funding: Taveras EM, Gillman MW; Administrative, technical, or material support: Taveras EM, Rifas-Shiman SL; Study supervision: Taveras EM, Gillman MW.
Funding: This study was supported by a grant from the National Institute on Minority Health and Health Disparities (MD 003963).
Footnotes
Conflicts of Interest: None of the authors have any conflicts of interest to disclose.
References
- 1.World Health Organization Global Strategy on Diet, Physical Activity and Health. 2010 http://www.who.int/dietphysicalactivity/en/December.
- 2.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010 Jan 20;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003-2006. JAMA. 2008 May 28;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006 Apr 5;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 5.Olds T, Maher C, Zumin S, et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. International journal of pediatric obesity : IJPO : an official journal of the International Association for the Study of Obesity. 2011 Oct;6(5-6):342–360. doi: 10.3109/17477166.2011.605895. [DOI] [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012 Feb 1;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang YC, Gortmaker SL, Taveras EM. Trends and racial/ethnic disparities in severe obesity among US children and adolescents, 1976-2006. International journal of pediatric obesity : IJPO : an official journal of the International Association for the Study of Obesity. 2010 Mar 17; doi: 10.3109/17477161003587774. [DOI] [PubMed] [Google Scholar]
- 8.Wen X, Gillman MW, Rifas-Shiman SL, Sherry B, Kleinman K, Taveras EM. Decreasing prevalence of obesity among young children in Massachusetts from 2004 to 2008. Pediatrics. 2012 May;129(5):823–831. doi: 10.1542/peds.2011-1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taveras EM, Rifas-Shiman SL, Oken E, Gunderson EP, Gillman MW. Short sleep duration in infancy and risk of childhood overweight. Archives of pediatrics & adolescent medicine. 2008 Apr;162(4):305–311. doi: 10.1001/archpedi.162.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ong KK, Loos RJ. Rapid infancy weight gain and subsequent obesity: systematic reviews and hopeful suggestions. Acta Paediatr. 2006 Aug;95(8):904–908. doi: 10.1080/08035250600719754. [DOI] [PubMed] [Google Scholar]
- 11.Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ. 2005;331(7522):929. doi: 10.1136/bmj.38586.411273.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Monteiro PO, Victora CG. Rapid growth in infancy and childhood and obesity in later life--a systematic review. Obes Rev. 2005 May;6(2):143–154. doi: 10.1111/j.1467-789X.2005.00183.x. [DOI] [PubMed] [Google Scholar]
- 13.Yliharsila H, Kajantie E, Osmond C, Forsen T, Barker DJ, Eriksson JG. Body mass index during childhood and adult body composition in men and women aged 56-70 y. Am J Clin Nutr. 2008 Jun;87(6):1769–1775. doi: 10.1093/ajcn/87.6.1769. [DOI] [PubMed] [Google Scholar]
- 14.Parsons TJ, Power C, Logan S, Summerbell CD. Childhood predictors of adult obesity: a systematic review. Int J Obes Relat Metab Disord. 1999 Nov;23(Suppl 8):S1–107. [PubMed] [Google Scholar]
- 15.Reilly JJ, Armstrong J, Dorosty AR, et al. Early life risk factors for obesity in childhood: cohort study. BMJ. 2005 Jun 11;330(7504):1357. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics. 2005;115(5):1367–1377. doi: 10.1542/peds.2004-1176. [DOI] [PubMed] [Google Scholar]
- 17.Oken E, Levitan EB, Gillman MW. Maternal smoking during pregnancy and child overweight: systematic review and meta-analysis. Int J Obes (Lond) 2008 Feb;32(2):201–210. doi: 10.1038/sj.ijo.0803760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gillman MW, Rifas-Shiman SL, Kleinman K, Oken E, Rich-Edwards JW, Taveras EM. Developmental origins of childhood overweight: potential public health impact. Obesity (Silver Spring) 2008 Jul;16(7):1651–1656. doi: 10.1038/oby.2008.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oken E, Rifas-Shiman SL, Field AE, Frazier AL, Gillman MW. Maternal gestational weight gain and offspring weight in adolescence. Obstet Gynecol. 2008 Nov;112(5):999–1006. doi: 10.1097/AOG.0b013e31818a5d50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oken E, Taveras EM, Kleinman KP, Rich-Edwards JW, Gillman MW. Gestational weight gain and child adiposity at age 3 years. American journal of obstetrics and gynecology. 2007 Apr;196(4):322, e321–328. doi: 10.1016/j.ajog.2006.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wright CS, Rifas-Shiman SL, Rich-Edwards JW, Taveras EM, Gillman MW, Oken E. Intrauterine exposure to gestational diabetes, child adiposity, and blood pressure. American journal of hypertension. 2009 Feb;22(2):215–220. doi: 10.1038/ajh.2008.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gillman MW, Oakey H, Baghurst PA, Volkmer RE, Robinson JS, Crowther CA. Effect of treatment of gestational diabetes mellitus on obesity in the next generation. Diabetes Care. 2010 May;33(5):964–968. doi: 10.2337/dc09-1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taveras EM, Rifas-Shiman SL, Belfort MB, Kleinman KP, Oken E, Gillman MW. Weight status in the first 6 months of life and obesity at 3 years of age. Pediatrics. 2009 Apr;123(4):1177–1183. doi: 10.1542/peds.2008-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Belfort MB, Rifas-Shiman SL, Rich-Edwards J, Kleinman KP, Gillman MW. Size at birth, infant growth, and blood pressure at three years of age. J Pediatr. 2007 Dec;151(6):670–674. doi: 10.1016/j.jpeds.2007.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taveras EM, Rifas-Shiman SL, Scanlon KS, Grummer-Strawn LM, Sherry B, Gillman MW. To what extent is the protective effect of breastfeeding on future overweight explained by decreased maternal feeding restriction? Pediatrics. 2006 Dec;118(6):2341–2348. doi: 10.1542/peds.2006-1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Rossem L, Taveras EM, Gillman MW, et al. Is the association of breastfeeding with child obesity explained by infant weight change? Int J Pediatr Obes. 2010 Oct 28; doi: 10.3109/17477166.2010.524700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White House Task Force . Solving the problem of childhood obesity within a generation: White House Task Force Report on Childhood Obesity Report to The President. Washington, D.C.: 2010. [DOI] [PubMed] [Google Scholar]
- 28.Institute of Medicine . Early Childhood Obesity Prevention Policies. The National Academies Press; Washington, DC: 2011. [Google Scholar]
- 29.Institute of Medicine . Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington DC: 2012. [Google Scholar]
- 30.Taveras EM, Gillman MW, Kleinman K, Rich-Edwards JW, Rifas-Shiman SL. Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics. 2010 Apr;125(4):686–695. doi: 10.1542/peds.2009-2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gillman MW, Rich-Edwards JW, Rifas-Shiman SL, Lieberman ES, Kleinman KP, Lipshultz SE. Maternal age and other predictors of newborn blood pressure. J Pediatr. 2004;144:240–245. doi: 10.1016/j.jpeds.2003.10.064. [DOI] [PubMed] [Google Scholar]
- 32.National Center for Health Statistics CDC Growth Charts, United States. 2000 Available at: http://www.cdc.gov/growthcharts/
- 33.Shorr IJ. How to weigh and measure children. U.N.; New York: 1986. [Google Scholar]
- 34.Mueller WH, Martorell R. Reliability and accuracy of measurement. In: Lohman TG, Roche AF, Martorell R, editors. Anthropometric Standardization Reference Manual. Human Kinetics Books; Champaign, IL: 1988. [Google Scholar]
- 35.Gestational diabetes mellitus. Diabetes Care. 2004 Jan;27(Suppl 1):S88–90. doi: 10.2337/diacare.27.2007.s88. [DOI] [PubMed] [Google Scholar]
- 36.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry. 1987 Jun 1;150(6):782–786. doi: 10.1192/bjp.150.6.782. 1987. [DOI] [PubMed] [Google Scholar]
- 37.Blum RE, Wei EK, Rockett HR, et al. Validation of a food frequency questionnaire in Native American and Caucasian children 1 to 5 years of age. Matern Child Health J. 1999;3:167–172. doi: 10.1023/a:1022350023163. [DOI] [PubMed] [Google Scholar]
- 38.Pereira MA, Kartashov AI, Ebbeling CB, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365(9453):36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- 39.Rubin DB. Multiple Imputation for Nonresponse in Surveys. J. Wiley & Sons; New York: 1987. [Google Scholar]
- 40.Horton NJ, Kleinman KP. Much ado about nothing: A comparison of missing data methods and software to fit incomplete data regression models. Am Stat. 2007 Feb;61(1):79–90. doi: 10.1198/000313007X172556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ertel KA, Kleinman K, van Rossem L, et al. Maternal perinatal depression is not independently associated with child body mass index in the Generation R Study: methods and missing data matter. Journal of clinical epidemiology. 2012 Dec;65(12):1300–1309. doi: 10.1016/j.jclinepi.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 42.Dennison BA, Erb TA, Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics. 2002;109(6):1028–1035. doi: 10.1542/peds.109.6.1028. [DOI] [PubMed] [Google Scholar]
- 43.Welsh JA, Cogswell ME, Rogers S, Rockett H, Mei Z, Grummer-Strawn LM. Overweight among low-income preschool children associated with the consumption of sweet drinks: Missouri, 1999-2002. Pediatrics. 2005 Feb;115(2):e223–229. doi: 10.1542/peds.2004-1148. [DOI] [PubMed] [Google Scholar]
- 44.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988-2004. Pediatrics. 2008 Jun;121(6):e1604–1614. doi: 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 45.Piernas C, Popkin BM. Increased portion sizes from energy-dense foods affect total energy intake at eating occasions in US children and adolescents: patterns and trends by age group and sociodemographic characteristics, 1977-2006. The American journal of clinical nutrition. 2011 Nov;94(5):1324–1332. doi: 10.3945/ajcn.110.008466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nevarez MD, Rifas-Shiman SL, Kleinman KP, Gillman MW, Taveras EM. Associations of early life risk factors with infant sleep duration. Academic pediatrics. 2010 May-Jun;10(3):187–193. doi: 10.1016/j.acap.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gillman MW, Rifas-Shiman SL, Kleinman K, Oken E, Rich-Edwards JW, Taveras EM. Developmental origins of childhood overweight: potential public health impact. Obesity. 2008 Jul;16(7):1651–1656. doi: 10.1038/oby.2008.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ciampa PJ, Kumar D, Barkin SL, et al. Interventions aimed at decreasing obesity in children younger than 2 years: a systematic review. Archives of pediatrics & adolescent medicine. 2010 Dec;164(12):1098–1104. doi: 10.1001/archpediatrics.2010.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Powell LM, Wada R, Krauss RC, Wang Y. Ethnic disparities in adolescent body mass index in the United States: the role of parental socioeconomic status and economic contextual factors. Soc Sci Med. 2012 Aug;75(3):469–476. doi: 10.1016/j.socscimed.2012.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang Y, Chen X. How much of racial/ethnic disparities in dietary intakes, exercise, and weight status can be explained by nutrition- and health-related psychosocial factors and socioeconomic status among US adults? Journal of the American Dietetic Association. 2011 Dec;111(12):1904–1911. doi: 10.1016/j.jada.2011.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nader PR, Huang TT, Gahagan S, Kumanyika S, Hammond RA, Christoffel KK. Next steps in obesity prevention: altering early life systems to support healthy parents, infants, and toddlers. Child Obes. 2012 Jun;8(3):195–204. doi: 10.1089/chi.2012.0004. [DOI] [PubMed] [Google Scholar]
- 52.Dixon B, Pena MM, Taveras EM. Lifecourse approach to racial/ethnic disparities in childhood obesity. Adv Nutr. 2012 Jan;3(1):73–82. doi: 10.3945/an.111.000919. [DOI] [PMC free article] [PubMed] [Google Scholar]