Abstract
Interventional radiologists are often consulted for acute management of hemorrhagic complications in obstetric and gynecologic patients. The aim of this article is to review the common indications for vascular embolization in obstetric and gynecologic emergencies, specifically in the setting of primary postpartum hemorrhage, and to discuss the technique and outcomes of endovascular treatment.
Keywords: postpartum hemorrhage, endovascular, embolization, balloon occlusion catheter
Objectives: Upon completion of this article, the reader will be able to identify the etiology of primary postpartum hemorrhage, define existing endovascular treatment techniques, and describe the outcomes of endovascular therapy.
Accreditation: This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of Tufts University School of Medicine (TUSM) and Thieme Medical Publishers, New York. TUSM is accredited by the ACCME to provide continuing medical education for physicians.
Credit: Tufts University School of Medicine designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Approximately 500,000 women die annually worldwide from causes related to pregnancy and childbirth and one-quarter of these deaths are caused by bleeding complications within the first 24 hours of delivery. In the developing world, the risk of maternal death from postpartum hemorrhage (PPH) is approximately 1 in 1,000 deliveries.1 PPH has been defined as an estimated blood loss (EBL) of 500 mL or more after vaginal delivery or 1,000 mL or more after cesarean delivery and PPH can be classified as primary (early) or secondary (delayed), with primary occurring within 24 hours after delivery and secondary occurring anywhere between 24 hours to 12 weeks postpartum.2
PPH has multiple causes, with uterine atony being the most common. Placentation abnormalities are an unusual but particularly morbid etiology for PPH. Failure of the placenta to separate normally from the uterus after delivery is accompanied by severe PPH and attempts to remove the adherent tissue can provoke further bleeding and a cascade of ongoing hemorrhage, shock, and coagulopathy.3 Standard management of placenta accreta is cesarean delivery followed by hysterectomy. The incidence of abnormal placentation is on the rise, mostly attributed to the increased numbers of cesarean deliveries.3 Placenta accreta is defined as an abnormal adherence of the placenta to the uterine wall and traditionally, abnormal placental adherence has been classified into placenta accreta, placenta increta, and placenta percreta based on depth of invasion into the myometrium: superficial, deep, and through to serosa and adjacent structures, respectively (Fig. 1).
Figure 1.
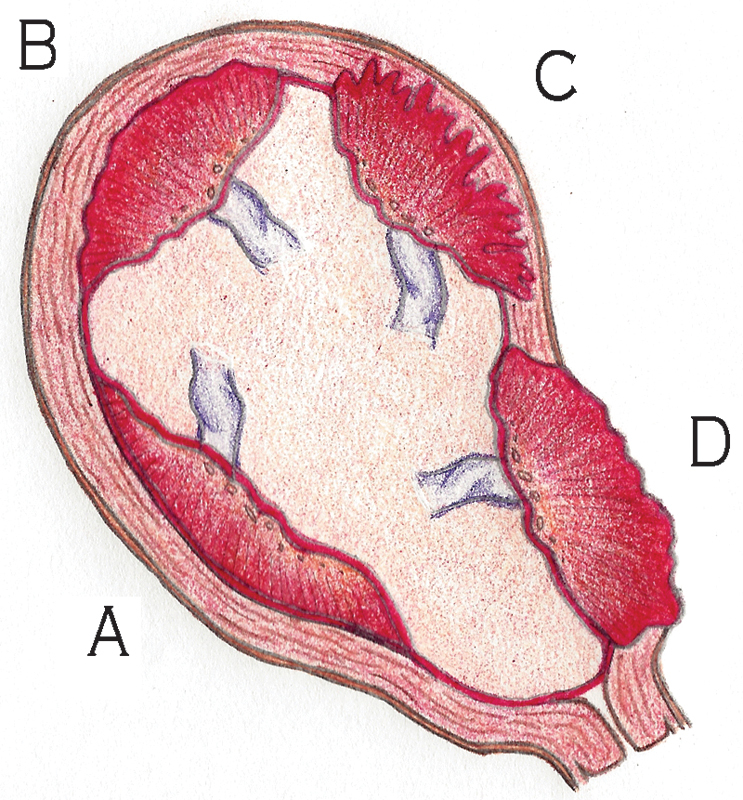
Types of placenta accreta. (A) Normal, (B) accreta, (C) increta, and (D) percreta.
This article describes percutaneous techniques applicable to PPH including vascular embolization in the setting of uterine atony and prophylactic balloon occlusion of the hypogastric arteries in patients with placenta accreta with a discussion of recent technical and clinical outcomes.
Postpartum Hemorrhage
The most common cause of PPH is uterine atony which complicates 1 in 20 births and is responsible for at least 80% of cases of PPH. Table 1 lists additional etiologies of primary and secondary PPH.2 Relying on vital signs to initiate treatment could be misleading and may delay appropriate care as a healthy woman may lose approximately 20% blood volume without a change in blood pressure or vital signs.2 Conservative measures aimed at preventing uterine atony include bimanual exam with uterine massage, administration of uterotonics (oxytocin, ergot alkaloids, and prostaglandins), and if bleeding persists, a search for undiagnosed lower genital lacerations or retained products of conception. Uterine tamponade techniques and exploratory laparotomy with possible hysterectomy are used in the setting of ongoing and uncontrollable bleeding. Women with persistent PPH despite conservative treatment modalities may benefit from transcatheter embolization.
Table 1. Etiologies of primary and secondary postpartum hemorrhage.
| Primary |
| Uterine atony |
| Genital tract lacerations |
| Retained placenta (placenta accreta) |
| Uterine rupture |
| Coagulation defects |
| Secondary |
| Subinvolution of placental site |
| Retained products of conception |
| Infection |
| Inherited coagulation defects |
Patient Assessment
The interventional radiologist is often consulted after more conservative measures have failed and in urgent or emergent fashion; however, informed consent with detailed discussion of the potential risks should be discussed with the patient and family when clinically feasible. It is important to discuss with the obstetrical team the details of the delivery, to determine any predelivery conditions, the likelihood of an iatrogenic injury, and any attempted instrumentation. Failed attempts at uterine ligation might also influence approach, particularly when intervention is being performed after hysterectomy. It is common that the interventional radiologist has arrived before the patient is transferred to the angiography suite; this is a good time to gather important information.
Physical exam including a peripheral vascular examination and review of recent laboratory and imaging studies should be performed. Coagulation parameters and serum chemistry levels should be reviewed before any arterial intervention and optimal laboratory values include a serum creatinine < 1.5 mg/dL with an estimated glomerular filtration rate > 60, an international normalized ratio < 1.5, and a platelet count > 50,000/dL.4 Average blood loss after vaginal and cesarean delivery is approximately 500 and 1,000 mL, respectively.5 Volume expansion with crystalloid and colloids may have started before angiography and blood products need to be readily available perioperatively. Prophylactic intravenous antibiotics (1 g cefazolin) should be administered before the procedure.
Postpartum Hemorrhage Embolization: Technique
Common femoral artery access is achieved using Seldinger technique either with fluoroscopy/palpation or by ultrasound guidance. The latter is particularly useful in women with small caliber blood vessels secondary to hypotension and/or shock. At our institution, we prefer arterial access with a 21-gauge micropuncture introducer set (Cook Inc., Bloomington, IN) and advance a 0.035-inch guidewire (Bentson; Cook Inc.) into the abdominal aorta. Over wire, a 5-French side arm vascular sheath (Cordis Corp, Bridgewater, NJ) is placed and connected to heparinized saline infusion. The decision to use unilateral or bilateral retrograde common femoral artery access depends on the availability of multiple operators and the overall clinical scenario. A nonselective aortogram with a standard flush pigtail angiographic catheter, to include the vasculature of the pelvic floor, can be helpful to quickly assess for a vascular injury when a laceration is anticipated from the delivery history and the location is unclear. Angiographic catheter injection rates and volumes should be increased to aid in visualizing the location of vascular injury. A 5-French Cobra catheter (Cook Inc.) is used to place a guidewire into the contralateral common femoral artery and a Roberts Uterine Catheter (RUC) (Cook Inc.) is formed in the abdominal aorta and can be used to select either the contralateral or ipsilateral hypogastric artery. First, the contralateral hypogastric artery is cannulated and angiography in the opposite obliquity (approximately 30 degrees) is undertaken to delineate the location of the anterior division of the hypogastric artery and uterine artery.
Uterine artery catheterization is desirable. Commonly, the uterine artery can be cannulated with the 5-French RUC as the artery is almost always hypertrophied given the enlarged uterus and recent postpartum state. A microcatheter (Renegade HI-FLO; Boston Scientific Corp, Quincy, MA) can be placed in coaxial fashion through the RUC if vascular spasm precludes placement of the 5-French catheter into the uterine artery. Road map technique can be particularly helpful to selectively cannulate the smaller, more terminal branches of the hypogastric or uterine artery when a laceration or focal injury is discovered. The position of the catheter before embolization will depend on the underlying vascular injury and hemodynamic status of the patient. It is often necessary to sacrifice careful technique for speed in the setting of rapid hemorrhage and blood loss and nonselective embolization of the anterior division of the hypogastric artery maybe necessary.
The most commonly used and preferred embolic agent when bleeding appears to be nonfocal or secondary to atony is absorbable gelatin sponge (Gelfoam; Pfizer Inc., New York, NY). Gelfoam can be cut into small pledgets and individually delivered hydrostatically through the catheter or cut into small 2 to 3 mm cubes and used to make slurry. The slurry can be prepared by rapidly mixing the gelfoam cubes between two 10 mL syringes connected with a three-way stop cock. Dilute the mixture in a 1:1 ratio of iodinated contrast and normal saline; the consistency of “cake frosting” is desired. The advantages of gelfoam include inexpensive cost, quick delivery, and rapid embolization result. Medium to large sized particles (500–1000 µm), such as polyvinyl alcohol (PVA; Cook Inc.) can also be used for embolization (complications from ischemia may be higher with smaller sized particles). With either embolic agent, a larger inner-diameter catheter will make the delivery of the material faster and more uniform. The embolization end point is a stagnant column of contrast—complete stasis (Fig. 2). When injuries are traumatic, selective embolization can be performed as elsewhere in the body. Pseudoaneurysms and arteriovenous fistulas are treated selectively with either coils or vascular plugs when possible (Fig. 3).4
Figure 2.
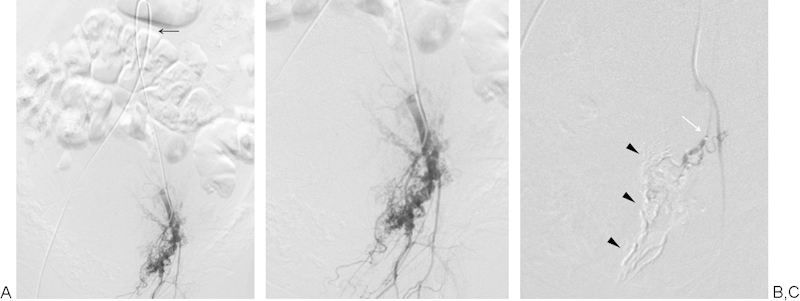
A 32-year-old woman (G1P0) with recalcitrant blood loss after vaginal delivery. Left-sided anterior division hypogastric arteriography (A, B) demonstrates no angiographic findings of active hemorrhage (Roberts uterine catheter is formed in distal abdominal aorta [black arrow]). (C) Uterine artery angiogram through microcatheter (white arrow) demonstrates pruning of the uterine artery with occlusion of distal branches with gelfoam slurry cast (arrowheads).
Figure 3.
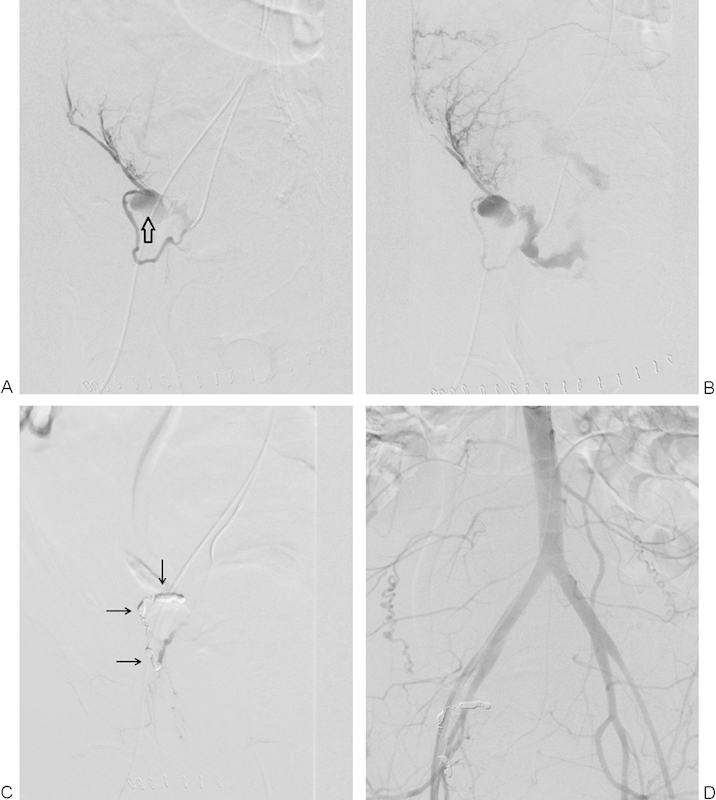
A 38-year-old woman (G1P1) status post primary low cesarean section via Pfannenstiel incision who became tachycardic and hypotensive with rapid onset vaginal bleeding after delivery. Patient failed resuscitation with blood products and trial of lower uterine segment balloon tamponade. (A) Early arterial and (B) late arterial digital subtraction angiography (DSA) demonstrates a pseudoaneurysm (open arrow) arising from the uterine artery with active hemorrhage into the pelvis. (C) DSA of the uterine artery and (D) flush aortogram after transcatheter coiling demonstrates cessation of hemorrhage with coil pack (arrows) in the right hemipelvis.
Postpartum Hemorrhage: Outcomes
Transcatheter arterial embolization in the setting of PPH has been proven to be safe and effective since it was first described in 1979.6 7 8 More recent reports in the medical literature have documented good technical and clinical outcomes. A study by Touboul et al in 2008 described selective arterial embolization in 102 patients with life-threatening PPH and found an overall success rate of 71.5%. In their study, arterial embolization in women with uterine atony was associated with an 88.6% success rate; however, cesarean deliveries and hemodynamic shock were associated with high failure rates.9 In 2009, Kirby et al published a retrospective multicenter study evaluating 43 patients who underwent arterial embolization for primary PPH and found clinical success of approximately 80% and technical success of 100%.10 Lee et al evaluated 251 patients in a recent retrospective, single-center study and found a clinical success rate of 86.5% (217 of 251) and overall bleeding control was achieved in 98.0% (246 of 251) of patients. They found that clinical success was not related to mode of delivery, cause of PPH, transfusion requirements, time from delivery to embolization, or hysterectomy before arterial embolization, and patients with angiographic findings of active extravasation were more likely to require repeat embolization.11 Absorbable gelatin sponge material was the embolic agent of choice for these studies. In 2013, Kim et al published a retrospective study of 257 consecutive patients who underwent pelvic arterial embolization for PPH. Failure to achieve hemostasis was seen in 24 cases (approximately 9%) and this group experienced more major complications. Factors more frequently found in failed embolization included disseminated intravascular coagulation (DIC), hemodynamic instability, hemoglobin level below 8 g/dL, and extravasation detected on angiography. After statistical analysis, DIC was the only significant predictive factor of failure to achieve hemostasis.12
Major complications associated with uterine artery embolization (UAE) in the setting of PPH are rare with an overall complication rate of approximately 9%.13 These include transient fever, transient buttock ischemia, transient foot ischemia, iliac artery perforation, and abscess.14
Abnormal Placentation: Placenta Accreta
The incidence of placenta accreta is increasing, affecting approximately 1 in 533 pregnancies, and the rapid rise of cesarean deliveries over the past 20 years is the strongest contributing factor.15 16 Other risk factors include prior dilatation and curettage, surgical termination, myomectomies, and nonsurgical factors such as the presence of placenta previa, advanced maternal age, grand multiparity, and smoking.15 Management for prenatally diagnosed placenta accreta usually consists of a scheduled cesarean hysterectomy.3 Blood loss with this anticipated procedure can be massive, often exceeding 2 L.17 Although mixed results are described in the literature, the internal iliac arteries may be catheterized preoperatively for prophylactic intraoperative balloon occlusion, first reported by Dubois et al in 1997.18
Prophylactic Hypogastric Balloon Occlusion: Technique
At our institution, if the diagnosis of placenta accreta is diagnosed prenatally, the case is reviewed at a multidisciplinary conference before the scheduled delivery. Specialists from obstetrics, maternal fetal medicine, gynecologic oncology, neonatology, anesthesiology, urology, and interventional radiology are in attendance to discuss the clinical scenario, logistics, and treatment plan. Prophylactic perioperative balloon occlusion and cesarean delivery are performed in our hybrid operating room, which contains equipment and staff that can accommodate both endovascular and surgical procedures.
Ultrasound guidance is used to obtain vascular access in all cases. The gravid abdomen can make it difficult to palpate the femoral artery and ultrasound will provide vascular access amenable for percutaneous closure device (Perclose Proglide Suture-Mediated Closure System; Abbott Laboratories, Abbott Park, IL). Standard Seldinger technique is used to place bilateral 7-French long angled sheaths (Pinnacle Destination Guiding Sheath; Terumo Interventional Systems, Somerset, NJ). Using a 5-French Cobra catheter, 0.035 inch Amplatz (Cook Inc.) guidewires are placed into the contralateral hypogastric arteries. The 7-French guide sheaths are advanced “up and over” the iliac bifurcation and into the contralateral common iliac arteries. Over wire, 80-cm 5.3-French flow-directed balloon catheters (FDB; Cook Inc.) are placed with distal tip in the hypogastric artery. The balloons are briefly insufflated with a 1:1 mixture of dilute contrast and normal saline and digital subtraction angiography is performed through the balloon occlusion catheter to evaluate adequacy of arterial occlusion (Fig. 4). The balloons are deflated and the necessary volume injected into the balloon to create occlusion is not only recorded but marked on the syringes (connected with a stopcock) used to inflate the balloons. Steri-Strips (3M, St. Paul, MN) are placed on the FDB catheters at the junction of the vascular sheaths and the coaxial system is securely taped to the patient. The imaging equipment is moved out from over the abdomen and the surgeons begin preparation for cesarean delivery.
Figure 4.
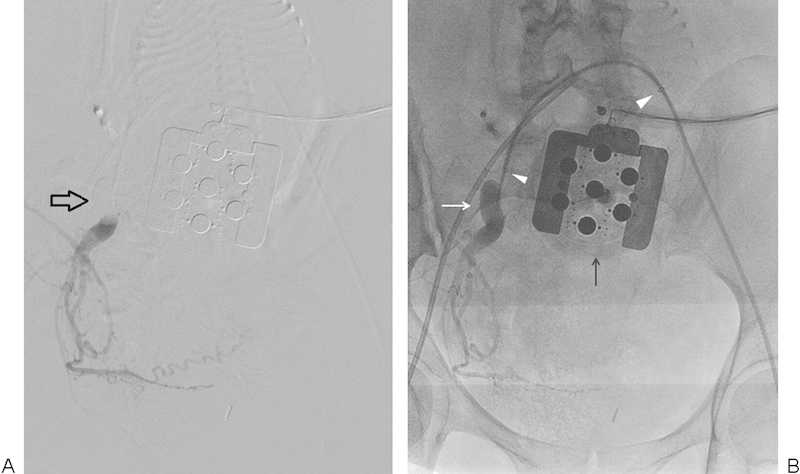
A 34-year-old woman (G3P2) with complete placenta previa and percreta who underwent preoperative balloon catheter placement for scheduled cesarean delivery. (A) Right-sided hypogastric artery digital subtraction angiography (DSA) after balloon catheter inflation demonstrates good position of the occlusion balloon (open arrow) and stasis of forward flow. (B) DSA native image redemonstrates balloon catheter (white arrow) and bilateral 7-French sheath tips (arrowheads). Radio-opaque fetal monitoring equipment overlies the anterior abdomen (black arrow).
After the infant is delivered, the placenta is left in place and the uterus is closed in anticipation of hysterectomy. The occlusion balloons are insufflated if bleeding is evident and not readily controlled. Often hysterectomy is performed by an oncologic gynecologist, a different team who performed delivery.
After the operation is completed, the balloon occlusion catheters are deflated and a search for further bleeding conducted. It is our standard practice to remove the vascular sheaths while the patient is in the hybrid operating room; however, they can remain in place for rapid access in cases were recurrent bleeding is felt to be likely. If the decision is made to keep arterial access, the 7-French long sheaths are exchanged for standard short 7-French side arm vascular sheaths which are secured to the skin and pressurized infusion with heparinized normal saline should continue. Monitoring of distal pulses is mandatory until the sheaths are removed. Femoral artery complications due to vasoconstriction caused by uterotonic medications need to be considered.
Preoperative Balloon Occlusion Catheter Placement: Outcomes
Controversy exists as regarding the safety and efficacy of this technique and remains a topic of debate. Lack of prospective randomized trials, heterogeneous patient populations, and differences in technique attribute to the shortage of data to support its routine use. The two largest series to date evaluating preoperative balloon catheter placement were published in 2007 and 2012. Shrivastava et al published a retrospective case-controlled series of patients with placenta accreta, in which 69 subjects were identified as having hysterectomies at the time of cesarean delivery for abnormal placentation. Nineteen of these patients had preoperative balloon catheter placement into the anterior division of the hypogastric arteries and 50 patients had cesarean hysterectomy alone. At the time of delivery, all 19 patients underwent balloon insufflation and they found no statistical difference between the two groups, including EBL, numbers of units of blood products transfused, duration of surgery, or length of postoperative hospital days. They hypothesized that the failure of occlusive balloons in reducing blood loss may be explained by the extensive collateral blood flow from the cervical, ovarian, rectal, femoral, lumbar, and sacral arteries. Approximately 16% of patients who underwent balloon occlusive measures had complications associated with placement, deployment, or removal of the catheters.19 Ballas et al recently published a retrospective case-controlled study of 117 patients with pathology-proven placenta accreta. Fifty percent of patients underwent preoperative hypogastric artery balloon placement and approximately half of those patients required balloon inflation intraoperatively. They found that placement of balloon catheters decreased the overall surgical morbidity, as measured by decreased mean EBL, fewer cases with EBL of more than 2,500 mL, and fewer massive transfusions despite a higher rate of placenta percreta in the group that received balloon catheters. However, the subgroup that had the balloons inflated intraoperatively secondary to hemorrhage showed significantly higher mean EBL and amount of packed red blood cells transfused. They attributed this outcome as multifactorial in nature, with the major factor being how the balloons are used intraoperatively as they are only insufflated with the onset of significant hemorrhage. Complications related to balloon catheter placement were only 3% in their study.16
Complications associated with the use of balloon catheters include maternal thromboembolic events resulting in acute limb ischemia, need for arterial bypass or surgical thromboembolectomy, arterial pseudoaneurysms, dissection, and arterial rupture.14 19
Abnormal Placentation: Alternative Techniques
An alternative management approach to placentation abnormalities is cesarean delivery, immediate prophylactic transcatheter UAE followed by hysterectomy, or medical management.13 20 21 A proposed cause of UAE failure is vascular spasm in the setting of shock or impending shock due to massive blood loss. As patients are stabilized after delivery and transferred to the radiology department, there can be a long interval between the onset of bleeding and embolization. Vascular spasm, shock, and DIC can frequently occur in this setting and timing of embolization may be an important factor in controlling bleeding.13 Yu et al described a small series of 11 patients who underwent immediate prophylactic bilateral UAE (gelfoam pledgets) in the setting of placenta accreta, increta, or percreta after cesarean delivery. Nine of the 11 patients had a favorable outcome in which the uteri were preserved, blood loss was only between 500 and 2,300 mL, and all fetuses were born with no radiation exposure.13
Conclusion
Interventional radiologists play a key role in the endovascular management of perinatal maternal bleeding and should be familiar with the various embolization techniques. Transcatheter embolization in the setting of primary PPH has been proven to be safe and effective, with absorbable gelatin material (gelfoam) being the most common agent used in cases of atony. In the setting of abnormal placentation, controversy remains and prospective, randomized trails are needed to evaluate the efficacy of pelvic artery balloon catheter usage or prophylactic UAE. The importance of experienced operators and a multidisciplinary approach needs to be emphasized in this setting to improve outcomes.
Acknowledgment
The authors would like to thank Erika Gipson for providing the medical illustration.
References
- 1.Mousa H A Alfirevic Z Treatment for primary postpartum haemorrhage Cochrane Database Syst Rev 2007(1, Issue 1):CD003249. [DOI] [PubMed] [Google Scholar]
- 2.Su C W. Postpartum hemorrhage. Prim Care. 2012;39(1):167–187. doi: 10.1016/j.pop.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Hull A D, Resnik R. Placenta accreta and postpartum hemorrhage. Clin Obstet Gynecol. 2010;53(1):228–236. doi: 10.1097/GRF.0b013e3181ce6aef. [DOI] [PubMed] [Google Scholar]
- 4.Salazar G M, Petrozza J C, Walker T G. Transcatheter endovascular techniques for management of obstetrical and gynecologic emergencies. Tech Vasc Interv Radiol. 2009;12(2):139–147. doi: 10.1053/j.tvir.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 5.Stafford I, Dildy G A, Clark S L, Belfort M A. Visually estimated and calculated blood loss in vaginal and cesarean delivery. Am J Obstet Gynecol. 2008;199(5):e1–e7. doi: 10.1016/j.ajog.2008.04.049. [DOI] [PubMed] [Google Scholar]
- 6.Heaston D K, Mineau D E, Brown B J, Miller F J Jr. Transcatheter arterial embolization for control of persistent massive puerperal hemorrhage after bilateral surgical hypogastric artery ligation. AJR Am J Roentgenol. 1979;133(1):152–154. doi: 10.2214/ajr.133.1.152. [DOI] [PubMed] [Google Scholar]
- 7.Brown B J, Heaston D K, Poulson A M, Gabert H A, Mineau D E, Miller F J Jr. Uncontrollable postpartum bleeding: a new approach to hemostasis through angiographic arterial embolization. Obstet Gynecol. 1979;54(3):361–365. [PubMed] [Google Scholar]
- 8.Pelage J P, Le Dref O, Jacob D, Soyer P, Herbreteau D, Rymer R. Selective arterial embolization of the uterine arteries in the management of intractable post-partum hemorrhage. Acta Obstet Gynecol Scand. 1999;78(8):698–703. [PubMed] [Google Scholar]
- 9.Touboul C, Badiou W, Saada J. et al. Efficacy of selective arterial embolisation for the treatment of life-threatening post-partum haemorrhage in a large population. PLoS ONE. 2008;3(11):e3819. doi: 10.1371/journal.pone.0003819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kirby J M, Kachura J R, Rajan D K. et al. Arterial embolization for primary postpartum hemorrhage. J Vasc Interv Radiol. 2009;20(8):1036–1045. doi: 10.1016/j.jvir.2009.04.070. [DOI] [PubMed] [Google Scholar]
- 11.Lee H Y, Shin J H, Kim J. et al. Primary postpartum hemorrhage: outcome of pelvic arterial embolization in 251 patients at a single institution. Radiology. 2012;264(3):903–909. doi: 10.1148/radiol.12111383. [DOI] [PubMed] [Google Scholar]
- 12.Kim Y J, Yoon C J, Seong N J. et al. Failed pelvic arterial embolization for postpartum hemorrhage: clinical outcomes and predictive factors. J Vasc Interv Radiol. 2013;24(5):703–709. doi: 10.1016/j.jvir.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 13.Yu P C, Ou H Y, Tsang L L, Kung F T, Hsu T Y, Cheng Y F. Prophylactic intraoperative uterine artery embolization to control hemorrhage in abnormal placentation during late gestation. Fertil Steril. 2009;91(5):1951–1955. doi: 10.1016/j.fertnstert.2008.02.170. [DOI] [PubMed] [Google Scholar]
- 14.Dilauro M D, Dason S, Athreya S. Prophylactic balloon occlusion of internal iliac arteries in women with placenta accreta: literature review and analysis. Clin Radiol. 2012;67(6):515–520. doi: 10.1016/j.crad.2011.10.031. [DOI] [PubMed] [Google Scholar]
- 15.Wu S, Kocherginsky M, Hibbard J U. Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol. 2005;192(5):1458–1461. doi: 10.1016/j.ajog.2004.12.074. [DOI] [PubMed] [Google Scholar]
- 16.Ballas J, Hull A D, Saenz C. et al. Preoperative intravascular balloon catheters and surgical outcomes in pregnancies complicated by placenta accreta: a management paradox. Am J Obstet Gynecol. 2012;207(3):e1–e5. doi: 10.1016/j.ajog.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 17.Miller D A, Chollet J A, Goodwin T M. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997;177(1):210–214. doi: 10.1016/s0002-9378(97)70463-0. [DOI] [PubMed] [Google Scholar]
- 18.Dubois J, Garel L, Grignon A, Lemay M, Leduc L. Placenta percreta: balloon occlusion and embolization of the internal iliac arteries to reduce intraoperative blood losses. Am J Obstet Gynecol. 1997;176(3):723–726. doi: 10.1016/s0002-9378(97)70582-9. [DOI] [PubMed] [Google Scholar]
- 19.Shrivastava V, Nageotte M, Major C, Haydon M, Wing D. Case-control comparison of cesarean hysterectomy with and without prophylactic placement of intravascular balloon catheters for placenta accreta. Am J Obstet Gynecol. 2007;197(4):e1–e5. doi: 10.1016/j.ajog.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 20.Timmermans S, van Hof A C, Duvekot J J. Conservative management of abnormally invasive placentation. Obstet Gynecol Surv. 2007;62(8):529–539. doi: 10.1097/01.ogx.0000271133.27011.05. [DOI] [PubMed] [Google Scholar]
- 21.Mitty H A, Sterling K M, Alvarez M, Gendler R. Obstetric hemorrhage: prophylactic and emergency arterial catheterization and embolotherapy. Radiology. 1993;188(1):183–187. doi: 10.1148/radiology.188.1.8511294. [DOI] [PubMed] [Google Scholar]


