Abstract
Specific IgE to gliadin was proposed as a marker for wheat dependent exercise induced anaphylaxis, while Tri a 14 was found to induce IgE response in baker's asthma. We evaluated whether these components could be used for discriminating phenotypes of wheat allergy. Twenty-nine patients who were wheat-induced anaphylaxis and/or urticaria (n=21, group I) and baker's asthma (n=8, group II) were enrolled. The prevalence of serum specific IgE to Tri a 14 was higher in group II (25%) than in group I (4.8%), while the serum specific IgE to gliadin was significantly higher in group I (70%) than in group II (12.5%). The cutoff value for predicting the baker's asthma using the ratio of serum specific IgE to Tri a 14 to gliadin was 742.8 optical density×1,000/(kU/L) with high sensitivity and specificity. These findings suggest that Tri a 14/gliadin may be a potential marker for predicting baker's asthma.
Keywords: Baker's Asthma, Gliadin, Lipid Transfer Protein, Wheat
The prevalence of wheat allergy is about 0.5% worldwide (1). The allergic reactions to wheat are variable according to the sensitization route, per os (anaphylaxis, urticaria) and inhalation (baker's asthma) (2, 3). Wheat-related allergens include various components including salt-soluble proteins associated with baker's asthma and salt-insoluble proteins associated with wheat dependent exercise induced anaphylaxis (WDEIA), whereas both protein fractions could induce IgE production in patients with food allergy to wheat (4). Specific IgE to gliadin has been proposed as a useful serologic marker for WDEIA (5), while lipid transfer protein (LTP), Tri a 14, has been found to induce IgE response in patients with baker's asthma in recent studies (6, 7). To the best of our knowledge, this is the first study to evaluate whether the results of serum-specific IgE to wheat, gliadin and Tri a 14 using ELISA could be used for discriminating two major phenotypes of wheat-related allergy, anaphylaxis and/or urticaria and baker's asthma.
Twenty-nine patients with wheat allergy and 30 non-atopic healthy controls were enrolled from Ajou University Hospital, Suwon, Korea. Hypersensitivity reactions to wheat were wheat-induced anaphylaxis and/or urticaria (n=21, group I) and baker's asthma (n=8, group II). Skin-prick tests (SPTs) were performed for 50 common aeroallergens (Bencard, Bretford, UK). Total serum IgE levels and serum-specific IgE levels to wheat and gliadin were measured using the ImmunoCAP system (Pharmacia-Upjohn, Uppsala, Sweden). We measured serum-specific IgE to Tri a 14, which is the recombinant allergen provided by Palacin et al. (8) by ELISA reported previously. The positive cut-off value was determined as the mean plus three standard deviations of absorbance values of healthy controls. The significance of the differences between two groups was evaluated using Pearson's chi-square test or Mann-Whitney test. A receiver operating characteristic (ROC) curve was used to evaluate the diagnostic value of serum specific IgE to Tri a 14 and gliadin for discriminating phenotypes of wheat allergy. All analyses were carried out using the SPSS ver. 16.0 software (SPSS Inc., Chicago, IL, USA). P<0.05 was considered statistically significant.
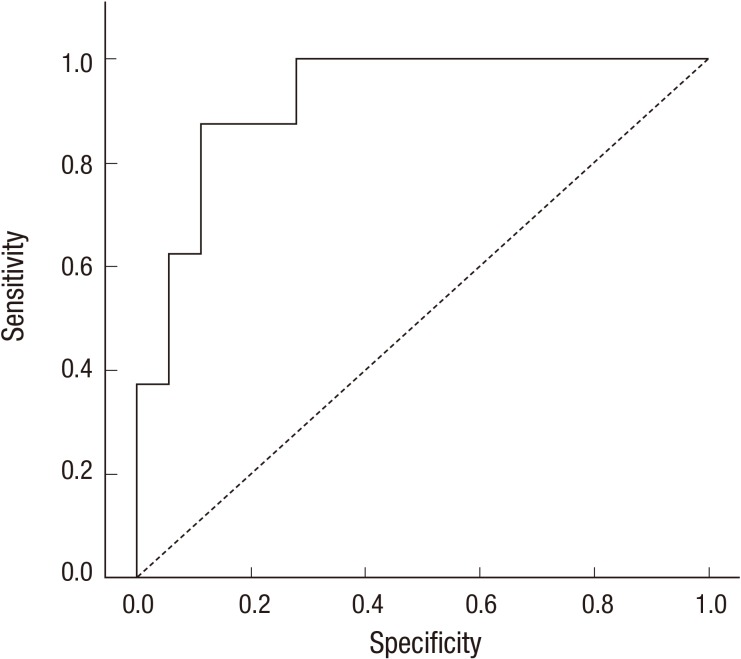
Of the 29 patients with wheat allergy, 50.0% (8/16) were positive to wheat on SPT and its positive rate tended to be higher in group II (75%) than in group I (41.7%). Serum-specific IgE to wheat was found in 71.4% of group I and 87.5% of group II subjects. Moreover, the level of serum specific IgE to wheat was significantly higher in group II than in group I (1.0±1.2 vs 7.2±7.1 kU/L; P=0.001). The serum specific IgE to gliadin was significantly higher in group I (70%) than in group II (12.5%). The serum specific IgE to Tri a 14 tended to be higher in group II (25%) than in group I subjects (4.8%), although statistical significance was not reached (Table 1). The patients with high specific IgE to Tri a 14 showed higher eosinophil cationic protein (49.6±42.5 vs 32.2±25.3 µg/L; P=0.019) than those with lower specific IgE levels, while no significant differences were noted in other clinical parameters. When the ROC curve was composed, the ratio of serum specific IgE to Tri a 14 to gliadin at 742.8 optical density×1,000/(kU/L) can be used for predicting the phenotype of baker's asthma with 87.5% sensitivity and 83.3% specificity (Fig. 1).
Table 1.
Clinical characteristics of study subjects with wheat allergy
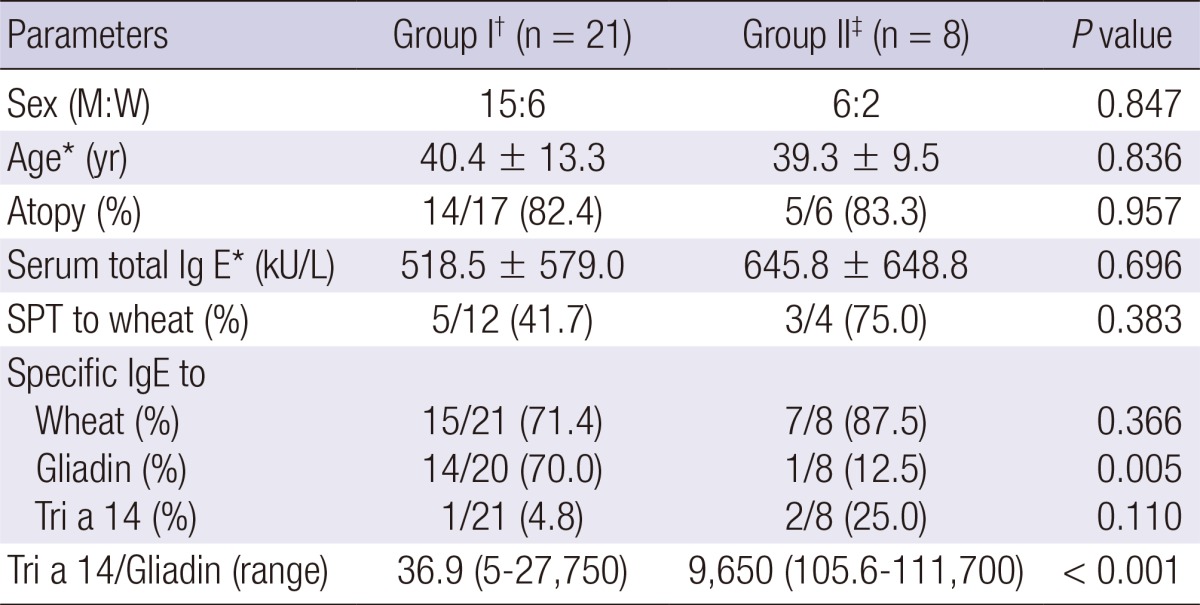
*Data are presented as mean±SD; †Group I, patients with wheat-related anaphylaxis and/or urticaria; ‡Group II, patients with wheat-related baker's asthma. M, men; W, women; SPT, skin prick test.
Fig. 1.
Receiver operating characteristic (ROC) curves for the ratio of serum specific IgE to Tri a 14 to gliadin. The area under ROC curve = 0.924.
SPTs play an important role in the diagnosis of baker's asthma, however, the frequency of sensitization to wheat flour by SPT among bakers varied from 5% to 15% (9). The results of SPTs with wheat flour had been shown wide variability between 45% and 67% according to different producers (10). In the present study, the sensitivity of serum specific IgE to wheat using ImmunoCAP system was higher than that of SPT in both group I and II subjects. These findings suggest that for the diagnosis of wheat allergy, both SPT and serum specific IgE detection to wheat is more sensitive in patients with baker's asthma, which is sensitized via inhalation than in those with anaphylaxis, which was induced by oral ingestion. However, they were detected in both conditions and cannot be used for differentiating between the two different phenotypes of wheat allergy. These findings suggested that more sensitive in vitro or in vivo method is required for differentiating two major phenotypes of wheat allergy.
IgE reactivity has been a high degree of heterogeneity among patients with wheat allergy as well as within groups according to phenotypes (11). A major grain allergen, gliadin, is commonly associated with WDEIA (5), and also useful for diagnosis of wheat-induced anaphylaxis with high sensitivity and specificity (12). In the present study, high serum specific IgE to gliadin was significantly higher in anaphylaxis group compared to baker's asthma group.
LTPs have been identified as major allergens in many plant foods, mainly Rosaceae fruits, and pollens, which showed various geographical distribution in Europe, with a high prevalence in the Mediterranean area, but lower prevalence in northern and central regions (13, 14). Wheat LTP, Tri a 14, as a major allergen in baker's asthma was supported by in vivo and in vitro assays. SPT and serum specific IgE to Tri a 14 was detected in 62% and 60% of the Spanish patients with baker's asthma (7). In addition, Tri a 14 was also a major allergen in wheat IgE-mediated food allergy in Italian patients in which 40.9% were detected (15). However, these findings suggest that Tri a 14 could be a useful tool for diagnosis of wheat allergy in the limited Mediterranean population. Most of the recombinant allergen preparations showed biological equivalence with the corresponding natural allergens, therefore they have been used for diagnosis and immunotherapy (10). On the other hand, the CREATE project showed only 2 recombinant allergens of the 9 recombinant molecules would be suitable for international reference in which recombinant allergens were compared with purified natural allergens for physico-chemical and immunological characteristics (16). Recombinant Tri a 14 showed similar IgE-binding capacity with natural Tri a 14 confirmed by ELISA and basophil activation test. It had high thermal stability and resistance to proteolysis (7), which might induce severe symptoms as like other food allergens (13). In this study, the prevalence rates of serum-specific IgE to Tri a 14 was very low: 4.8% in group I and 25% in group II subjects both of which was lower compared to previous studies (7, 15). This may be due to differences in the study subjects or ethnic difference derived from different environmental factors.
In conclusion, we report first a very low sensitization rate to Tri a 14 in patients of two major phenotypes of wheat allergy in a Korean population. The findings suggest that the ratio of serum specific IgE to Tri a 14 to gliadin may be a potential candidate marker for predicting the phenotype of baker's asthma with higher sensitivity and specificity among the patients with wheat related allergy.
Footnotes
This study was supported by a grant from the Korea Science and Engineering Foundation (KOSEF) funded by the Korean government (MEST, 2013-003341).
There are no financial or other issues that might lead to conflict of interests.
References
- 1.Zuidmeer L, Goldhahn K, Rona RJ, Gislason D, Madsen C, Summers C, Sodergren E, Dahlstrom J, Lindner T, Sigurdardottir ST, et al. The prevalence of plant food allergies: a systematic review. J Allergy Clin Immunol. 2008;121:1210–1218.e4. doi: 10.1016/j.jaci.2008.02.019. [DOI] [PubMed] [Google Scholar]
- 2.Bock SA. Prospective appraisal of complaints of adverse reactions to foods in children during the first 3 years of life. Pediatrics. 1987;79:683–688. [PubMed] [Google Scholar]
- 3.Wang J, Sampson HA. Food allergy: recent advances in pathophysiology and treatment. Allergy Asthma Immunol Res. 2009;1:19–29. doi: 10.4168/aair.2009.1.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salcedo G, Quirce S, Diaz-Perales A. Wheat allergens associated with Baker's asthma. J Investig Allergol Clin Immunol. 2011;21:81–92. [PubMed] [Google Scholar]
- 5.Matsuo H, Dahlström J, Tanaka A, Kohno K, Takahashi H, Furumura M, Morita E. Sensitivity and specificity of recombinant omega-5 gliadin-specific IgE measurement for the diagnosis of wheat-dependent exercise-induced anaphylaxis. Allergy. 2008;63:233–236. doi: 10.1111/j.1398-9995.2007.01504.x. [DOI] [PubMed] [Google Scholar]
- 6.Bittner C, Grassau B, Frenzel K, Baur X. Identification of wheat gliadins as an allergen family related to baker's asthma. J Allergy Clin Immunol. 2008;121:744–749. doi: 10.1016/j.jaci.2007.09.051. [DOI] [PubMed] [Google Scholar]
- 7.Palacin A, Quirce S, Armentia A, Fernández-Nieto M, Pacios LF, Asensio T, Sastre J, Diaz-Perales A, Salcedo G. Wheat lipid transfer protein is a major allergen associated with baker's asthma. J Allergy Clin Immunol. 2007;120:1132–1138. doi: 10.1016/j.jaci.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Palacin A, Varela J, Quirce S, del Pozo V, Tordesillas L, Barranco P, Fernandez-Nieto M, Sastre J, Diaz-Perales A, Salcedo G. Recombinant lipid transfer protein Tri a 14: a novel heat and proteolytic resistant tool for the diagnosis of baker's asthma. Clin Exp Allergy. 2009;39:1267–1276. doi: 10.1111/j.1365-2222.2009.03280.x. [DOI] [PubMed] [Google Scholar]
- 9.Houba R, Doekes G, Heederik D. Occupational respiratory allergy in bakery workers: a review of the literature. Am J Ind Med. 1998;34:529–546. doi: 10.1002/(sici)1097-0274(199812)34:6<529::aid-ajim1>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 10.Sander I, Merget R, Degens PO, Goldscheid N, Brüning T, Raulf-Heimsoth M. Comparison of wheat and rye flour skin prick test solutions for diagnosis of baker's asthma. Allergy. 2004;59:95–98. doi: 10.1046/j.1398-9995.2003.00349.x. [DOI] [PubMed] [Google Scholar]
- 11.Mittag D, Niggemann B, Sander I, Reese I, Fiedler EM, Worm M, Vieths S, Reese G. Immunoglobulin E-reactivity of wheat-allergic subjects (baker's asthma, food allergy, wheat-dependent, exercise-induced anaphylaxis) to wheat protein fractions with different solubility and digestibility. Mol Nutr Food Res. 2004;48:380–389. doi: 10.1002/mnfr.200400016. [DOI] [PubMed] [Google Scholar]
- 12.Park HJ, Kim JH, Kim JE, Jin HJ, Choi GS, Ye YM, Park HS. Diagnostic value of the serum-specific IgE ratio of ω-5 gliadin to wheat in adult patients with wheat-induced anaphylaxis. Int Arch Allergy Immunol. 2012;157:147–150. doi: 10.1159/000327549. [DOI] [PubMed] [Google Scholar]
- 13.Salcedo G, Sanchez-Monge R, Diaz-Perales A, Garcia-Casado G, Barber D. Plant non-specific lipid transfer proteins as food and pollen allergens. Clin Exp Allergy. 2004;34:1336–1341. doi: 10.1111/j.1365-2222.2004.02018.x. [DOI] [PubMed] [Google Scholar]
- 14.Van Ree R. Clinical importance of non-specific lipid transfer proteins as food allergens. Biochem Soc Trans. 2002;30:910–913. doi: 10.1042/bst0300910. [DOI] [PubMed] [Google Scholar]
- 15.Pastorello EA, Farioli L, Conti A, Pravettoni V, Bonomi S, Iametti S, Fortunato D, Scibilia J, Bindslev-Jensen C, Ballmer-Weber B, et al. Wheat IgE-mediated food allergy in European patients: alpha-amylase inhibitors, lipid transfer proteins and low-molecular-weight glutenins: allergenic molecules recognized by double-blind, placebo-controlled food challenge. Int Arch Allergy Immunol. 2007;144:10–22. doi: 10.1159/000102609. [DOI] [PubMed] [Google Scholar]
- 16.Van Ree R, Chapman MD, Ferreira F, Vieths S, Bryan D, Cromwell O, Villalba M, Durham SR, Becker WM, Aalbers M, et al. The CREATE project: development of certified reference materials for allergenic products and validation of methods for their quantification. Allergy. 2008;63:310–326. doi: 10.1111/j.1398-9995.2007.01612.x. [DOI] [PubMed] [Google Scholar]