Abstract
Purpose
Mentoring is critical for career advancement in academic medicine. However, underrepresented minority (URM) faculty often receive less mentoring than their nonminority peers. The authors conducted a comprehensive review of published mentoring programs designed for URM faculty to identify “promising practices.”
Method
Databases (PubMed, PsycINFO, ERIC, PsychLit, Google Scholar, Dissertations Abstracts International, CINHAL, Sociological Abstracts) were searched for articles describing URM faculty mentoring programs. The RE-AIM framework (Reach, Effectiveness, Adoption, Implementation, and Maintenance) formed the model for analyzing programs.
Results
The search identified 73 citations. Abstract reviews led to retrieval of 38 full-text articles for assessment; 18 articles describing 13 programs were selected for review. The reach of these programs ranged from 7 to 128 participants. Most evaluated programs on the basis of the number of grant applications and manuscripts produced or satisfaction with program content. Programs offered a variety of training experiences, and adoption was relatively high, with minor changes made for implementing the intended content. Barriers included time-restricted funding, inadequate evaluation due to few participants, significant time commitments required from mentors, and difficulty in addressing institutional challenges faced by URM faculty. Program sustainability was a concern because programs were supported through external funds, with minimal institutional support.
Conclusions
Mentoring is an important part of academic medicine, particularly for URM faculty who often experience unique career challenges. Despite this need, relatively few publications exist to document mentoring programs for this population. Institutionally supported mentoring programs for URM faculty are needed, along with detailed plans for program sustainability.
Although numerous definitions of mentoring exist in the professional literature, traditionally it is a process through which a senior, experienced faculty member (mentor) provides guidance and support for a junior or less experienced colleague (mentee). Mentoring is a critical element for faculty career advancement in academic medicine,1–5 and mentors can play a variety of roles in helping mentees delineate and accomplish their career goals.1,6 Ideally, mentors can enable junior faculty to enhance productivity and can provide education about the written and unwritten rules that govern the academic environment.1 Faculty members with mentors express more confidence than their peers,7 report experiencing higher career satisfaction,8,9 are more likely to have productive careers,10,11 and feel greater support for their research careers.12
Unfortunately, many early-career faculty members, particularly those from underrepresented racial and ethnic minority (URM) groups, are often unaware of the significance of mentoring or cannot find mentors committed to their career success.13,14 Ironically, laudable traits such as self-reliance that helped URM early-career faculty to navigate graduate and medical school may actually isolate them and hinder them from achieving further success.15,16
Numerous studies have reported that URM faculty typically receive less mentoring than their nonminority peers.17–19 Mentoring programs designed to address unique challenges faced by URM faculty are critically needed. These challenges include marginalization, overt and covert racism, and a disproportionate share of activities that do not advance careers (e.g., serving on numerous committees; participation in community outreach endeavors; advising minority students, postdoctoral fellows, and residents).17–19 Finally, URM faculty often treat more financially marginalized patients who generate less revenue but whose clinical care requires more time.15,20 Two recent reports provide troubling evidence with regard to reversing these disparities and achieving the goal of enhancing successful career trajectories of URMs in academic health centers (AHCs). A 2010 report from the Association of American Medical Colleges (AAMC)21 indicated that nonwhite faculty are less likely to be promoted than white faculty. Another study, based on National Institutes of Health data (2000–2006), indicated that African American scientists are about 10% less likely than their white peers to obtain R01 grants.22 In a follow-up article that discussed the potential reasons for this disparity, Tabak and Collins23 hypothesized that variability in access to mentoring may be a causal factor.
Leaders of several AHCs in the United States have acknowledged the relative paucity of URM faculty and are attempting to increase the diversity of students, trainees, and faculty.24 The AAMC has stated that enhancing the diversity of AHC faculty is a significant component in the overall strategy to reduce health care disparities in the United States.25 Over the last decade, a few AHCs have designed mentoring programs specifically for URM faculty to address these various disparities24,26; however, the pace of progress has been glacial, and it has yielded mixed results.
We conducted a systematic review of the published literature with a focus on outcomes of mentoring programs designed for URM faculty employed in AHCs. This article extends the descriptive review of mentoring programs by Daley and colleagues26 for URM faculty in AHCs and includes the updated literature with a focus on published programmatic outcomes. We used the RE-AIM framework27 to synthesize and describe the primary components of the programs. From these publications, we gleaned “promising practices” that can be widely disseminated to other AHCs, and we suggest ways to enhance efforts to increase and sustain faculty diversity at AHCs.
Method
Data collection
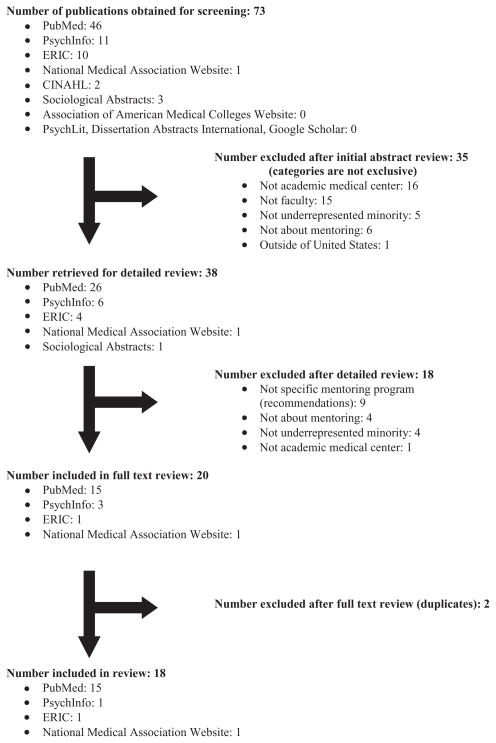
We identified relevant publications by searching the following databases: (1) PubMed, (2) PsycINFO, (3) ERIC, (4) PsychLit, (5) Google Scholar, (6) Dissertations Abstracts International, (7) the AAMC Web site, (8) CINHAL, (9) Sociological Abstracts, and (10) the National Medical Association Web site. Two authors (B.M.B., S.L.) conducted searches during four time periods (May–June 2010; November 2010; May 2011; April 2012) to ensure that we included the most recently published articles. MeSH and other controlled search terms included mentor, mentorship, mentoring, AMCs (academic medical centers), best practices, minority faculty, underrepresented minority faculty, training, and professional development. We used these terms and their combinations to search each database to ensure continuity across sources. We further reviewed the references of identified articles to obtain additional relevant publications; we restricted inclusion to those written in English. Figure 1 outlines the number of publications obtained through each step in the search process, reasons for omitting selected publications, and the final number of publications included in this review. We defined mentorship as a developmental partnership in which knowledge, experience, skills, and information are shared between mentor(s) and mentee(s) to foster the mentee’s professional development and, often, also to enhance the mentor’s perspectives and knowledge.
Figure 1.
Number of publications obtained through each step in the search process, reasons for omission, and the final number included in a systematic review of the published literature with a focus on outcomes of mentoring programs designed for underrepresented minority faculty employed in academic health centers.
Two authors (B.M.B., S.L.) independently reviewed the abstracts of publications obtained through the search process and then selected publications for possible inclusion. We addressed disagreements regarding study inclusion by consulting a third reviewer (J.C.-E.) or through review of the full-text publication until consensus was reached; this process was only required on two occasions.
To be included in the review, publications had to describe mentoring programs based in the United States and identify that their focus was URM faculty. After the initial abstract screening, two reviewers (B.M.B., S.L.) thoroughly reviewed and coded the selected full-text publications. We designed and used a protocol and data collection form to capture from each publication the type of mentoring program; study design, rationale, and goals; location of program and demographics of mentees; enrollment and retention rates; and program outcomes (if reported). Source selection and publication bias was minimized by using multiple types of sources to identify published studies (general source databases, hand-searching of journals, and examining the reference lists of published articles). Further, we maintained a record of articles that were excluded and reasons for their elimination. The quality of selected mentoring programs was assessed by examining study designs, sample sizes, thoroughness of descriptions of the mentoring programs, and program outcomes reported.
Data analysis
We used the RE-AIM framework (Reach, Effectiveness, Adoption, Implementation, Maintenance, described in detail below)27 to conduct our analysis. RE-AIM was originally designed to evaluate health interventions, particularly those focused on changing individual and organizational behaviors.27 However, RE-AIM also is an effective and comprehensive evaluation model for other programs.28,29 Essentially, mentoring programs are a type of intervention designed to positively influence and enhance the career trajectories of early-career faculty (individual level). Ultimately, these programs also affect the academic institutions (organizational level) because mentoring influences faculty satisfaction and retention.10,11 Thus, this framework is a useful tool to comprehensively describe these initiatives.
In the RE-AIM framework, Reach is an individual-level measure of participation and refers to the percentage and characteristics of members of a defined population (e.g., URM early-career faculty members in an AHC) who receive or are affected by a mentoring program. To determine reach, we evaluated the numbers of URM faculty who participated in the mentoring programs.
Effectiveness is an individual-level measure typically used to describe the effect of a program when conducted in a “real-world” setting. We evaluated effectiveness by summarizing the positive and negative outcomes of the faculty mentoring programs and briefly describing program completion rates.
Adoption is an organizational-level measure that refers to the proportion and characteristics of the settings where individuals are willing to participate in a specific program. Because this review focused on the mentoring programs developed in individual AHCs, we defined adoption as characteristics of the program settings and ability of the AHCs to implement the mentoring programs. We combined adoption and implementation to describe both the settings and components of the mentoring programs for URM faculty, as well as levels of participation.
Maintenance, often called “sustainability,” refers to long-term implementation of programming and/or behavior change. We described this metric in terms of subsequent funding sources and the degree of institutionalization of the mentoring programs. Maintenance is critical, particularly with regard to the extent to which programs became part of the culture and norms of the AHCs.
Results
We identified a total of 73 relevant citations. The review of abstracts led to 38 publications for full-text assessment; 20 of these were included in this review (see Figure 1). We excluded two articles because they did not describe programs based in the United States. Original data were available from 13 studies discussed in 18 articles; duplicative references describing the same program(s) are noted.30–34 Appendix 1 lists the 13 published reports of mentoring programs for URM early-career faculty identified through the review process.
Overall, the main objective of each mentoring program was to increase the number of URM faculty who pursue careers in academic medicine and dentistry and to enhance the likelihood of their academic productivity and promotion. The stated goals of the programs were to address numerous barriers disproportionately experienced by URM faculty, including competing academic demands, the historic lack of institutional support and diversity, and the challenge of identifying qualified and interested senior faculty members in specified areas of research. We describe each mentoring program below within the context of the RE-AIM model.
Reach
Structural models for the URM faculty mentoring programs varied. Two mentoring programs included a partnership between two institutions,31,35 and several were housed at one institution but were open to early-career URM faculty from across the United States36–38 or across the United States and Puerto Rico.39 Two programs focused on early-career URM faculty at one institution but included mentors with relevant expertise from across the United States.39,40 Two of the 13 programs were available to all early-career faculty members,31,41 and 3 were specifically designed for only one racial or ethnic minority group (i.e., American Indian/ Alaska Natives;35,38 Hispanics)42; the remaining mentoring programs were available to all URM faculty at their institutions.
Program participation rates varied greatly, as did the amount of detail regarding participation. The number of mentees ranged from 7 to 128 early-career URM faculty participants. Because most publications included in this review did not list the number of URM faculty at each academic institution, the overall rate of participation in the mentoring programs could not be determined.
Four mentoring programs also included activities to increase the number of diverse students/trainees interested in pursuing careers in the health professions.33,34,36,43 These programs included undergraduate students, medical and dental students, students pursuing master’s and PhD degrees, and/ or postgraduates (residents and fellows). One of these six programs43 extended the program to include middle school and high school students.
Effectiveness
Most articles were largely descriptive and provided minimal objective outcomes, but most included some form of program evaluation. When acknowledged, the lack of outcome data was often attributed to the early stage of most programs. Process evaluations of the individual-level outcomes included satisfaction surveys, focus groups, productivity of participants (e.g., numbers of grant applications, peer-reviewed publications, scientific presentations), retention rates, and the number of faculty promotions. In general, participants reported being satisfied with the various mentoring programs, and programs reported early successes regarding faculty retention and productivity. Manson and colleagues38 developed a Likert scale questionnaire and identified high rates of receptivity of key program elements among participants. In one of the few long-term evaluations, Daley and colleagues32 reported a 10-year longitudinal follow-up of 12 of 30 participants in the URM early-career mentoring program at the University of California, San Diego School of Medicine. They reported that 11 of 12 participants (92%) attained promotion to associate professor. When asked what contributed to their success, participants reported critical factors such as support of senior faculty mentors, networking with peers, professional skill development, and better understanding of their institution’s culture.32
Adoption and implementation
Although each mentoring program described unique features, universal aspects included offering training opportunities for early-career URM faculty. Programmatic activities were intended to enhance skills in grant and manuscript writing, the development and delivery of scientific presentations, and didactic teaching. Twelve programs provided one-on-one mentoring with senior faculty, with mentors and mentees carefully selected on the basis of alignment of research interests and disciplines.30,31,33–40,42–45 Senior faculty provided targeted career counseling during regularly scheduled individual meetings. Programs offered tips on stress management, navigating the rigors of academic careers, and time management in monthly group seminars. Two programs41,42 also included interaction with community advisory boards to provide insights regarding the conduct of community-based research.
Six programs were designed to train early-career URM faculty in specific areas of research: health disparities,31 oral health,36 aging,38 HIV disparities,39 addiction,44 and mental health.45 The remaining mentoring programs provided general career development or were designed for research and/or clinical training in an academic department (e.g., family medicine). Several programs provided direct support for research and research-related activities, such as access to experienced biostatisticians and epidemiologists,34,45 funds for mentees to attend national meetings,43 and pilot funding for mentees to gain research experience and generate preliminary data.31,34,44
Overwhelmingly, the mentoring programs appeared to be delivered as intended, with few described modifications or changes made to the original designs. However, common barriers to implementing and sustaining mentoring programs included time-limited funding, few participants (which hampered program evaluation), significant time commitments required from faculty mentors, and difficulty in addressing several institutional challenges faced by early-career URM faculty.
Maintenance
With one exception,41 each mentoring program began via extramural funding, although many also reported some form of institutional support. Several programs explicitly stated that their goal was to transition from time-limited extramural funding to institutional support; two programs accomplished that goal,26,34 with the latter achieving program designation within the Office of Academic Affairs and Vice Chancellor for Health Sciences.
Discussion
The racial and ethnic diversity in the general U.S. population is not reflected in the composition of the health care workforce. African Americans, Hispanic Americans, and American Indians represent nearly 25% of the U.S. population but less than 10% of all physicians. These disparities extend to faculty representation in academic medical institutions. Similar disparities exist for medical school faculty ranks in that the majority of URM faculty are overrepresented at the rank of assistant professor.21
Most mentoring programs arise from a need for experienced guidance vocalized by certain populations; therefore, it is understandable that each institution may have different approaches to address specific interests and needs. Additionally, unique institutional environments and cultures influence program design and implementation. In this review, we sought to identify and assess best practices for mentoring early-career URM faculty by examining published literature describing programs in AHCs. We describe 13 programs that delineated several different approaches to mentoring URM faculty. Good practices included one-on-one mentoring by an experienced investigator, group-based skill-building seminars, access to pilot grants, and support for conducting pilot studies. Institutional components, including the support of key leaders and an allocation of resources, are important for sustaining these programs. These elements are similar to those identified by Palermo and colleagues46 in a descriptive overview of successful mentoring programs for URM faculty in AHCs.
As the field of mentoring in academic medical centers continues to evolve, conducting comprehensive program evaluation and dissemination of findings will be crucial to ultimately determine the most efficacious and acceptable approaches for mentoring URM faculty. Program evaluation has several important roles, including holding stakeholders accountable and highlighting programmatic areas that may need improvement. Evaluations conducted at multiple time points during formal mentoring programs, as well as those conducted with multiple stakeholders (e.g., mentors, mentees, program coordinators, administrators), will permit a “360-degree” perspective that will provide a robust assessment of program processes and outcomes. Measurement tools specifically designed to evaluate formal mentorship programs in academic settings are available in the scientific literature.47
This review was limited by the relative paucity of outcome-driven assessments of mentoring programs for early-career URM faculty. It is essential that outcomes from successful programs be published to further inform best practices for mentoring URM faculty. Our findings are similar to those of Sambunjak and colleagues,48 who conducted a systematic review of all published mentoring programs (N = 39). They reported that although mentoring is perceived as an important component of success in academic medicine, the relationship between participating in such programs and subsequent success is not particularly strong.
In the future, it may be beneficial for organizations like the AAMC and the National Association of Medical Minority Educators to create guidelines for program evaluation that will permit comparisons of mentoring programs across institutions. With this type of centralized evaluation, areas such as cost-effectiveness can be addressed, with the goal of making these programs part of the institutional framework in places of higher learning. This is consistent with the recent call by Nivet49 for AHCs to conduct a “system upgrade,” referred to as Diversity 3.0, to strategically reposition diversity within the framework of these academic institutions.
Previous research has clearly documented both the need for and benefit of dedicated mentoring programs for underrepresented groups.30,40,50 Establishing standardized programmatic guidelines that can be implemented nationally will not only help ensure the success of underrepresented individuals but also strengthen the country’s academic health care workforce.
Acknowledgments
Funding/Support: This work was supported in part by a P60 Center of Excellence grant from the National Institute of Minority Health and Health Disparities (P60MD006917-01).
Appendix 1
Descriptive Characteristics of 13 Mentoring Programs for Underrepresented Minority (URM) Faculty at Academic Medical Centers*
| Citation | Program goal | Reach | Effectiveness | Adoption/implementation | Maintenance |
|---|---|---|---|---|---|
| Buchwald and Dick, 201135; Manson et al, 200638 | Provide intensive mentoring to promising junior American Indian and Alaska Native investigators | 29 Native American investigators who completed at least 1 year of the training program (n = 19), all core and affiliated faculty (n = 10) |
|
|
Not discussed; however, programs have been in existence since 1998 when external funding was obtained |
| Daley et al, 200630; 200931 | Create a cohort of investigators engaged in health disparities research, scholarship, and practice | 19 full-time salaried URM junior faculty and 75 non-URM junior faculty |
|
|
Project EXPORT funding in collaboration with UCSD, San Diego State University, and local agencies |
| Bussey- Jones et al, 200641 | Foster a collaborative environment to develop a junior faculty peer mentoring program | 7 internal medicine faculty who had been at Emory University between 1 and 5 years | Developed “work rules” and established agreement to adhere and hold each other accountable |
|
Institutional funding |
| Johnson et al, 199834; 199933 | Development of a mentoring program to increase the number of minorities entering the faculty development pipeline and enhance faculty retention | 36 Hispanic and African American early-career faculty |
|
|
|
| Kosoko- Lasaki et al, 200643 | Development of a mentoring program to provide junior faculty members with two or more designated mentors | 25–33 URM faculty | Impact after 18 months:
|
|
Extramural funding for the Center of Excellence in Faculty Development |
| Lewellen- Williams et al, 200640 | Development of a multilevel mentoring model (Peer- Onsite-Distance [POD] model) to promote retention and career development among URM medical school faculty | 22 mentees, 9 mentors, and 10 on-site mentors |
|
|
|
| Rabionet et al, 200939 | Development of a multifaceted mentoring model for minority researchers studying HIV health disparities | 15 mentors; number of mentees not explicitly mentioned |
|
|
Funded by National Center for Research Resources and National Institute of Mental Health (NIMH) |
| Rust et al, 200637 | Development, implementation, and evaluation of a faculty development program for faculty in family medicine |
|
|
|
Program initiated with a Health Resources and Services Administration (HRSA) grant, but continued with Title VII grants |
| Sinkford et al, 200936 | Program at a consortium of dental schools to improve the recruitment, retention, and development of URMs in the dental profession |
|
|
|
Funded by W.K. Kellogg Foundation grant |
| Soto-Greene et al, 200542 | Development and implementation of a program dedicated to the advancement of Latino medical faculty | Number of faculty not discussed | Specific outcomes not provided; largely descriptive |
|
Funded by HRSA; Bureau of Health Professions grant |
| Viets et al, 200944 | Development and implementation of a culturally centered mentorship model for ethnic minority faculty at academic health centers | 9 URM faculty (6 Latino; 3 Native Americans); variety of disciplines (medicine, psychiatry, and public health) |
|
|
Funded by National Institute on Alcohol Abuse and Alcoholism |
| Yager et al, 200745 | Development of a program to enhance the research capacity of junior faculty to conduct rigorous mental health research in primary care settings | 14 Native American and Hispanic mentees per cohort |
|
|
|
Information drawn from review of the literature and organized according to the RE-AIM framework.27
Footnotes
Other disclosures: None.
Ethical approval: Not applicable.
Contributor Information
Dr. Bettina M. Beech, Department of Social Sciences and Health Policy, and codirector, Maya Angelou Center for Health Equity, Wake Forest School of Medicine, Winston-Salem, North Carolina.
Dr. Jorge Calles-Escandon, Department of Internal Medicine, Wake Forest School of Medicine, Winston-Salem, North Carolina, and is currently chair, Division of Endocrinology, Metro Health Medical Center, Cleveland, Ohio.
Dr. Kristen G. Hairston, Department of Internal Medicine, Wake Forest School of Medicine, Winston-Salem, North Carolina.
Ms. Sarah E. Langdon, Maya Angelou Center for Health Equity, Wake Forest School of Medicine, Winston-Salem, North Carolina.
Dr. Brenda A. Latham-Sadler, Wake Forest School of Medicine, Winston-Salem, North Carolina.
Dr. Ronny A. Bell, Department of Epidemiology, and codirector, Maya Angelou Center for Health Equity, Wake Forest School of Medicine, Winston-Salem, North Carolina.
References
- 1.White HK, Buhr GT, Pinheiro SO. Mentoring: A key strategy to prepare the next generation of physicians to care for an aging America. J Am Geriatr Soc. 2009;57:1270–1277. doi: 10.1111/j.1532-5415.2009.02300.x. [DOI] [PubMed] [Google Scholar]
- 2.Schrubbe KF. Mentorship: A critical component for professional growth and academic success. J Dent Educ. 2004;68:324–328. [PubMed] [Google Scholar]
- 3.Healy CC, Weichert AJ. Mentoring relations: A definition to advance research and education. Educ Res. 1990;19:17–21. [Google Scholar]
- 4.Benson CA, Morahan PS, Sachdeva AK, Richman RC. Effective faculty preceptoring and mentoring during reorganization of an academic medical center. Med Teach. 2002;24:550–557. doi: 10.1080/0142159021000002612. [DOI] [PubMed] [Google Scholar]
- 5.Jackson VA, Palepu A, Szalacha L, Caswell C, Carr PL, Inui T. “Having the right chemistry”: A qualitative study of mentoring in academic medicine. Acad Med. 2003;78:328–334. doi: 10.1097/00001888-200303000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Fagan M. The term “mentor”: A review of the literature and pragmatic suggestion. Int J Mentoring. 1988;2(2):5–8. [Google Scholar]
- 7.Wingard DL, Garman KA, Reznik V. Facilitating faculty success: Outcomes and cost benefit of the UCSD National Center of Leadership in Academic Medicine. Acad Med. 2004;79(10 suppl):S9–S11. doi: 10.1097/00001888-200410001-00003. [DOI] [PubMed] [Google Scholar]
- 8.Schapira MM, Kalet A, Schwartz MD, Gerrity MS. Mentorship in general internal medicine: Investment in our future. J Gen Intern Med. 1992;7:248–251. doi: 10.1007/BF02598026. [DOI] [PubMed] [Google Scholar]
- 9.Palepu A, Friedman RH, Barnett RC, et al. Medical faculty with mentors are more satisfied. J Gen Intern Med. 1996;11(4 suppl):107. [Google Scholar]
- 10.Illes J, Glover GH, Wexler L, Leung AN, Glazer GM. A model for faculty mentoring in academic radiology. Acad Radiol. 2000;7:717–724. doi: 10.1016/s1076-6332(00)80529-2. [DOI] [PubMed] [Google Scholar]
- 11.Curtis P, Dickinson P, Steiner J, Lanphear B, Vu K. Building capacity for research in family medicine: Is the blueprint faulty? Fam Med. 2003;35:124–130. [PubMed] [Google Scholar]
- 12.Bligh J. Mentoring: An invisible support network. Med Educ. 1999;33:2–3. doi: 10.1046/j.1365-2923.1999.00360.x. [DOI] [PubMed] [Google Scholar]
- 13.Palepu A, Friedman RH, Barnett RC, et al. Junior faculty members’ mentoring relationships and their professional development in U.S. medical schools. Acad Med. 1998;73:318–323. doi: 10.1097/00001888-199803000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Ramanan RA, Phillips RS, Davis RB, Silen W, Reede JY. Mentoring in medicine: Keys to satisfaction. Am J Med. 2002;112:336– 341. doi: 10.1016/s0002-9343(02)01032-x. [DOI] [PubMed] [Google Scholar]
- 15.Carr PL, Bickel J, Inui TS, editors. Taking Root in a Forest Clearing: A Resource Guide for Medical Faculty. Boston, Mass: Boston University School of Medicine; 2004. [Google Scholar]
- 16.Sotello C, Turner V, Gonzales JC, Wood JL. Faculty of color in academe: What 20 years of literature tells us. J Divers High Educ. 2008;1:139–168. [Google Scholar]
- 17.Thomas DA. The truth about mentoring minorities. Race matters. Harv Bus Rev. 2001;79:98–107. 168. [PubMed] [Google Scholar]
- 18.Helm EG, Prieto DO, Parker JE, Russell MC. Minority medical school faculty. J Natl Med Assoc. 2000;92:411–414. [PMC free article] [PubMed] [Google Scholar]
- 19.Morzinski JA, Fisher JC. A nationwide study of the influence of faculty development programs on colleague relationships. Acad Med. 2002;77:402–406. doi: 10.1097/00001888-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Diggs GA, Garrison-Wade DF, Estrada D, Galindo R. Smiling faces and colored spaces: The experiences of faculty of color pursuing tenure in the academy. Urban Rev. 2009;41:312–333. [Google Scholar]
- 21.Liu CQ, Alexander H. AAMC Analysis in Brief. Washington, DC: Association of American Medical Colleges; May, 2010. Promotion rates for first-time assistant and associate professors appointed from 1967 to 1997. [Google Scholar]
- 22.Ginther DK, Schaffer WT, Schnell J, et al. Race, ethnicity, and NIH research awards. Science. 2011;333:1015–1019. doi: 10.1126/science.1196783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tabak LA, Collins FS. Sociology. Weaving a richer tapestry in biomedical science. Science. 2011;333:940–941. doi: 10.1126/science.1211704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nivet MA, Taylor VS, Butts GC, et al. Diversity in academic medicine no. 1 case for minority faculty development today. Mt Sinai J Med. 2008;75:491–498. doi: 10.1002/msj.20079. [DOI] [PubMed] [Google Scholar]
- 25.Association of American Medical Colleges. [Accessed December 14, 2012];The Diversity Research Forum: The Importance and Benefits of Diverse Faculty in Academic Medicine: Implications for Recruitment, Retention, and Promotion. https://members.aamc.org/eweb/DynamicPage.aspx?Action=Add&ObjectKeyFrom=1A83491A-9853-4C87-86A4-F7D95601C2E2&WebCode=PubDetailAdd&DoNotSave=yes&ParentObject=CentralizedOrderEntry&ParentDataObject=Invoice%20Detail&ivd_formkey=69202792-63d7-4ba2-bf4e-a0da41270555&ivd_prc_prd_key=6FD19E7A-D99C-44E6-8DD4-7F2B932FDD48.
- 26.Daley SP, Palermo AG, Nivet M, et al. Diversity in academic medicine no. 6 successful programs in minority faculty development: Ingredients of success. Mt Sinai J Med. 2008;75:533–551. doi: 10.1002/msj.20084. [DOI] [PubMed] [Google Scholar]
- 27.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. Am J Public Health. 1999;89:1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Belza B, Toobert DJ, Glasgow RE. [Accessed December 14, 2012];RE-AIM for Program Planning: Overview and Applications. http://www.prc-han.org/docs/RE-AIM_issue_brief.pdf.
- 29.Planas LG. Intervention design, implementation, and evaluation. Am J Health Syst Pharm. 2008;65:1854–1863. doi: 10.2146/ajhp070366. [DOI] [PubMed] [Google Scholar]
- 30.Daley S, Wingard DL, Reznik V. Improving the retention of underrepresented minority faculty in academic medicine. J Natl Med Assoc. 2006;98:1435–1440. [PMC free article] [PubMed] [Google Scholar]
- 31.Daley SP, Broyles SL, Rivera LM, Reznik VM. Increasing the capacity of health sciences to address health disparities. J Natl Med Assoc. 2009;101:881–885. doi: 10.1016/s0027-9684(15)31034-8. [DOI] [PubMed] [Google Scholar]
- 32.Daley SP, Broyles SL, Rivera LM, Brennan JJ, Lu ER, Reznik V. A conceptual model for faculty development in academic medicine: The underrepresented minority faculty experience. J Natl Med Assoc. 2011;103:816–821. doi: 10.1016/s0027-9684(15)30435-1. [DOI] [PubMed] [Google Scholar]
- 33.Johnson JC, Williams B, Jayadevappa R. Mentoring program for minority faculty at the University of Pennsylvania School of Medicine. Acad Med. 1999;74:376–379. doi: 10.1097/00001888-199904000-00029. [DOI] [PubMed] [Google Scholar]
- 34.Johnson JC, Jayadevappa R, Taylor L, Askew A, Williams B, Johnson B. Extending the pipeline for minority physicians: A comprehensive program for minority faculty development. Acad Med. 1998;73:237–244. doi: 10.1097/00001888-199803000-00011. [DOI] [PubMed] [Google Scholar]
- 35.Buchwald D, Dick RW. Weaving the native web: Using social network analysis to demonstrate the value of a minority career development program. Acad Med. 2011;86:778–786. doi: 10.1097/ACM.0b013e318217e824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sinkford JC, West JF, Weaver RG, Valachovic RW. Modelling mentoring: Early lessons from the W.K. Kellogg/ADEA minority dental faculty development program. J Dent Educ. 2009;73:753–763. [PubMed] [Google Scholar]
- 37.Rust G, Taylor V, Herbert-Carter J, Smith QT, Earles K, Kondwani K. The Morehouse Faculty Development Program: Evolving methods and 10-year outcomes. Fam Med. 2006;38:43–49. [PubMed] [Google Scholar]
- 38.Manson SM, Goins RT, Buchwald DS. The Native Investigator Development Program: Increasing the presence of American Indian and Alaska Native scientists in aging-related research. J Applied Gerontol. 2006;25:105S–130S. [Google Scholar]
- 39.Rabionet SE, Santiago LE, Zorrilla CD. A multifaceted mentoring model for minority researchers to address HIV health disparities. Am J Public Health. 2009;99(suppl 1):S65–S70. doi: 10.2105/AJPH.2008.153635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lewellen-Williams C, Johnson VA, Deloney LA, Thomas BR, Goyol A, Henry-Tillman R. The POD: A new model for mentoring underrepresented minority faculty. Acad Med. 2006;81:275–279. doi: 10.1097/00001888-200603000-00020. [DOI] [PubMed] [Google Scholar]
- 41.Bussey-Jones J, Bernstein L, Higgins S, et al. Repaving the road to academic success: The IMeRGE approach to peer mentoring. Acad Med. 2006;81:674–679. doi: 10.1097/01.ACM.0000232425.27041.88. [DOI] [PubMed] [Google Scholar]
- 42.Soto-Greene ML, Sanchez J, Churrano J, Salas-Lopez D. Latino faculty development in U.S. medical schools: A Hispanic center of excellence perspective. J Hisp Higher Educ. 2005;4:366–376. [Google Scholar]
- 43.Kosoko-Lasaki O, Sonnino RE, Voytko ML. Mentoring for women and underrepresented minority faculty and students: Experience at two institutions of higher education. J Natl Med Assoc. 2006;98:1449–1459. [PMC free article] [PubMed] [Google Scholar]
- 44.Viets VL, Baca C, Verney SP, Venner K, Parker T, Wallerstein N. Reducing health disparities through a culturally centered mentorship program for minority faculty: The Southwest Addictions Research Group (SARG) experience. Acad Med. 2009;84:1118–1126. doi: 10.1097/ACM.0b013e3181ad1cb1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yager J, Waitzkin H, Parker T, Duran B. Educating, training, and mentoring minority faculty and other trainees in mental health services research. Acad Psychiatry. 2007;31:146–151. doi: 10.1176/appi.ap.31.2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Palermo AG, Soto-Greene ML, Taylor VS, et al. Diversity in academic medicine no. 5 successful programs in minority faculty development: Overview. Mt Sinai J Med. 2008;75:523–532. doi: 10.1002/msj.20083. [DOI] [PubMed] [Google Scholar]
- 47.Berk RA, Berg J, Mortimer R, Walton-Moss B, Yeo TP. Measuring the effectiveness of faculty mentoring relationships. Acad Med. 2005;81:66–71. doi: 10.1097/00001888-200501000-00017. [DOI] [PubMed] [Google Scholar]
- 48.Sambunjak D, Straus SE, Marusić A. Mentoring in academic medicine: A systematic review. JAMA. 2006;296:1103–1115. doi: 10.1001/jama.296.9.1103. [DOI] [PubMed] [Google Scholar]
- 49.Nivet MA. Commentary: Diversity 3.0: A necessary systems upgrade. Acad Med. 2011;86:1487–1489. doi: 10.1097/ACM.0b013e3182351f79. [DOI] [PubMed] [Google Scholar]
- 50.Mahoney MR, Wilson E, Odom KL, Flowers L, Adler SR. Minority faculty voices on diversity in academic medicine: Perspectives from one school. Acad Med. 2008;83:781–786. doi: 10.1097/ACM.0b013e31817ec002. [DOI] [PMC free article] [PubMed] [Google Scholar]