Abstract
Healthcare practitioners, patient safety leaders, educators, and researchers increasingly recognize the value of human factors/ergonomics and make use of the discipline’s person-centered models of sociotechnical systems. This paper first reviews one of the most widely used healthcare human factors systems models, the Systems Engineering Initiative for Patient Safety (SEIPS) model, and then introduces an extended model, “SEIPS 2.0.” SEIPS 2.0 incorporates three novel concepts into the original model: configuration, engagement, and adaptation. The concept of configuration highlights the dynamic, hierarchical, and interactive properties of sociotechnical systems, making it possible to depict how health-related performance is shaped at “a moment in time.” Engagement conveys that various individuals and teams can perform health-related activities separately and collaboratively. Engaged individuals often include patients, family caregivers, and other non-professionals. Adaptation is introduced as a feedback mechanism that explains how dynamic systems evolve in planned and unplanned ways. Key implications and future directions for human factors research in healthcare are discussed.
Keywords: healthcare, work system, patient-centered care, patient and family engagement, SEIPS model
1. Introduction
Human factors/ergonomics is a discipline increasingly recognized, promoted, and applied by healthcare leaders and stakeholders, including practitioners, patient safety leaders, educators, and researchers (Gurses, Ozok, & Pronovost, 2012; Norris, 2012; Russ et al., 2013; World Health Organization, 2009). At the same time, the science and practice of human factors in the healthcare domain continue to evolve (Carayon, 2012). Within the healthcare industry, major system redesign efforts and paradigm shifts are also evident worldwide (de Savigny & Adam, 2009; Institute of Medicine, 2005; Magnussen, Vrangbæk, & Saltman, 2009). For example, the “doctor-knows-best” philosophy in the American Medical Association’s (AMA) original Code of Medical Ethics is being replaced by a paradigm of doctor-patient partnership and actively engaged patients, as illustrated below:
AMA Code of Medical Ethics, 1847 (original): “The obedience of a patient to the prescriptions of his physician should be prompt and implicit. He should never permit his own crude opinions … to influence his attention to them.”
AMA Code of Medical Ethics, 2012–13: “Physician and patient are bound in a partnership that requires both individuals to take an active role in the healing process.”
Recognizing that both the human factors discipline and healthcare domain are evolving, this article introduces a next-generation healthcare human factors model, “SEIPS 2.0,” which incorporates contemporary human factors concepts – configuration, engagement, and adaptation. These new concepts were chosen for inclusion for two reasons. First, they have been championed in recent theoretical and empirical work in several areas of human factors (e.g., macroergonomics, cognitive systems engineering, resilience engineering, safety science) (Carayon, 2012; Dekker, Hancock, & Wilkin, 2013; Hollnagel, Woods, & Leveson, 2006; Russ, et al., 2013; Wilson, 2013). Second, these new concepts can address emerging healthcare industry initiatives and needs such as the focus on multi-level interactions in ecological models of health behavior (Sallis, Owen, & Fisher, 2008), the need for resilience in patient safety (Patterson et al., 2006), and the central role of patients and families in health and healthcare (Berwick, 2009; National Research Council, 2011; Wachter, 2009).
1.1. The SEIPS Model: A prevalent healthcare human factors framework
While healthcare has benefited from human factors in many ways, it has particularly embraced these core human factors principles (Dul et al., 2012):
Principle 1, Systems orientation. Performance results from the interaction of a sociotechnical system in which the person is but one embedded component (this has motivated healthcare to replace a blame-the-person culture with a more holistic system-based approach).
Principle 2, Person-centeredness. The person, or group of people, is central in a healthcare work system, meaning that efforts must be taken to support people through the design of work systems that fit their capabilities, limitations, performance needs, and other characteristics, not the other way around.
Principle 3, Design-driven improvements. Person-centered design of work structures and processes, when grounded in sound human factors science and practice, can improve myriad important patient, provider, and organizational outcomes.
Some or all of these principles are depicted in highly recognized human factors models, including Reason’s “Swiss Cheese Model” (Reason, 2000) and Vincent and colleagues’ framework, based on Reason’s work (Vincent, Taylor-Adams, & Stanhope, 1998).
In the US, a prevalent healthcare human factors model of person-centered sociotechnical systems is the framework introduced by Carayon and colleagues in the University of Wisconsin’s Systems Engineering Initiative for Patient Safety (SEIPS) (Carayon et al., 2006; Carayon et al., 2013). The SEIPS model has appeared in national reports such as Making Health Care Safer II (Shekelle, Wachter, Pronovost, & al., 2013), adopted by patient safety leaders (Gurses et al., 2010; Pronovost et al., 2009; Sittig & Singh, 2009), and used in patient safety education (Karsh et al., 2005). The SEIPS model has also been used to frame the design and analysis of research. The original SEIPS model formulation paper accumulated 197 citations in Google Scholar and 127 in Scopus between 2006 and 2013. Research applications of the SEIPS model have spanned multiple healthcare delivery settings including intensive care units (ICUs), pediatric hospitals, cardiac operating rooms, outpatient surgery centers, primary care clinics, and home health nursing. A large body of research applies the model to evaluate various health information technologies such as bar coded medication administration, smart infusion pumps, electronic health records, computerized provider order entry, and virtual ICU technology. The SEIPS model has also influenced other system-based models used in healthcare research and practice, most notably Karsh and colleagues’ human factors paradigm for patient safety (Holden, 2011a; Holden, Brown, et al., 2011; Karsh, Holden, Alper, & Or, 2006). Table 1 cites some of the projects using or adapting the SEIPS model. Readers wishing to learn more about the model and its use can find thorough discussion of the model, its origin, and applications in several recent reviews (Carayon, 2009; Carayon, et al., 2006; Carayon, et al., 2013).
Table 1.
Projects using the SEIPS model.
| Overall safety and quality of care delivery | References |
|---|---|
| Understanding patient safety | (Karsh, et al., 2006; Shekelle, et al., 2013) |
| Improving safety in outpatient surgery | (Carayon, Hundt, et al., 2005) |
| Cardiac surgical care | (Gurses et al., 2012; Martinez et al., 2011; D. Wiegmann, A. Eggman, A. ElBardissi, S. Parker, & T. Sundt, 2010) |
| Patient safety in radio-therapy | (Rivera & Karsh, 2008) |
| Patient safety in the intensive care unit (ICU) | (Faye et al., 2010) |
| Medication safety in community pharmacies | (Chui, Mott, & Maxwell, 2012) |
| Patient safety in nursing homes | (Scandrett et al., 2012) |
| Patient safety climate | (Ausserhofer et al., 2013) |
| Clinical work and workflow evaluation and design | References |
| Workflow modeling | (Carayon, Cartmill, et al., 2012; Carayon et al., 2010) |
| Improving nursing processes | (Boston-Fleischhauer, 2008a, 2008b) |
| Analysis of critical care work systems | (Catchpole & McCulloch, 2010) |
| Timeliness of follow-up of abnormal tests in outpatient settings | (Singh et al., 2009) |
| Workload and performance obstacles among ICU nurses | (Carayon & Gurses, 2008; Gürses & Carayon, 2007; Holden, Scanlon, et al., 2011; Karsh, et al., 2005) |
| Evaluation of ways to improve electronic communication and alerts | (Hysong et al., 2009) |
| Evaluation of lean in healthcare | (Holden, 2011b) |
| Health information technology and medical devices | References |
| Technology acceptance and implementation | (Holden & Karsh, 2009; Karsh & Holden, 2007) |
| Electronic health record (EHR) implementation in a small clinic | (Carayon, Smith, Hundt, Kuruchittham, & Li, 2009; Carayon & Smith, 2001) |
| Examining the safety of EHR technology | (Holden, 2011a; Sittig & Singh, 2009) |
| Computerized provider order entry (CPOE) implementation in 4 ICUs | (Carayon, Cartmill, et al., 2011; Hoonakker & Carayon, 2010; P. L. T. Hoonakker, P. Carayon, R. L. Brown, et al., 2013; Hoonakker, Carayon, Walker, Brown, & Cartmill, 2013; Hoonakker, Wetterneck, Carayon, Cartmill, & Walker, 2011; Hundt A.S. et al., 2013; Wetterneck et al., 2011) |
| Health information technology-supported care management in community setting | (Carayon, Alyousef, et al., 2012; Hundt et al., 2012) |
| Health information technology in home care nursing | (Johnson et al., 2008) |
| Bar-coded medication administration systems | (Carayon et al., 2007; Holden, Brown, et al., 2011) |
| Smart infusion pumps | (Carayon, Wetterneck, et al., 2005; Schroeder, Carayon, & Li, 2005; Wetterneck et al., 2005) |
| Tele-ICU | (Hoonakker, Carayon, Khunlertkit, Mcguire, & Wiegmann, 2011; P. L. T. Hoonakker, P. Carayon, K. McGuire, et al., 2013; Hoonakker et al., 2011) |
| Computer decision support in primary care | (Hoonakker, Khunlertkit, Tattersall, Keevil, & Smith, 2012) |
| Patient and family engagement | References |
| Human factors in home care | (T. Zayas-Cabán & P. T. Brennan, 2007; Zayas-Cabán & Valdez, 2012) |
| Patient and family self-care “work” | (Holden & Mickelson, 2013) |
| Engaging families in Bedside Rounds to Promote Pediatric Patient Safety | (Carayon, DuBenske, et al., 2011) |
After several years of use, the SEIPS model has evolved through its use and requires clarification and expansion. It is especially important to incorporate contemporary thinking in human factors science and practice and to ensure that the model is attentive to emerging issues and priorities in the healthcare domain, such as the involvement of patients and families and the importance of temporal phenomena such as adaptation. This is the intent of presenting “SEIPS 2.0”.
2. SEIPS 2.0: The next-generation healthcare human factors framework
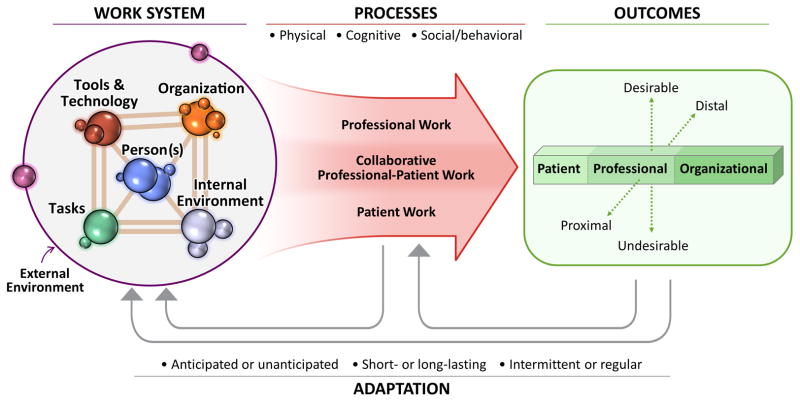
SEIPS 2.0 is graphically depicted in Figure 1. It retains many key properties of the original model and includes several clarifications and additions. The general structure of the model is that the sociotechnical work system (left) produces work processes (middle), which shape outcomes (right). This structure is familiar to healthcare audiences because it parallels Donabedian’s (1988) structure-process-outcome model of healthcare quality and also conforms to the input-transformation-output framework in systems theory (Karsh, et al., 2006). Systems theory also supports the inclusion of feedback loops, which represent adjustments over time (Katz & Kahn, 1966).
Figure 1.
SEIPS 2.0 model.
2.1. The work system in SEIPS 2.0
The left side of the model depicts a sociotechnical work system with six interacting components: person(s), tasks, tools and technologies, organization, internal environment, and external environment. This aspect of the model was introduced in the late 1980s (Carayon, 2009; M. J. Smith & Sainfort-Carayon, 1989). “Person(s)” in this model is one of several components in, and therefore not separable from, the sociotechnical system. The deliberate placement of person(s) in the center of the sociotechnical system fits with the human factors approach (Principle 2, above) and emphasizes that design should support – not replace or compensate for – people (Karsh, et al., 2006). In the healthcare domain, the “person(s)” can be an individual professional such as a clinician or social worker as well as a non-professional individual such as the patient or family caregiver.* The “person(s)” component can also be collectives or teams of individuals such as surgical teams, family units, faith communities, or the distributed patient-professional network managing a chronic medical condition. Person(s) factors therefore describe individual characteristics such as age and expertise as well as collective-level characteristics such as team cohesiveness or the similarity of knowledge among group members (for fuller treatment of key team characteristics, see, e.g., (Salas, Burke, & Cannon-Bowers, 2000; Salas & Fiore, 2004)).
As a new concept, we propose that both patients and healthcare professionals – and also other individuals and groups – should be simultaneously represented under the “person(s)” component of the model.† Including the patient and patient attributes in the center conveys two points. First, systems design and analysis must take into account patient characteristics including preferences, goals, and needs (Institute of Medicine, 2001). Second, sometimes the patient, family caregiver, or other non-professionals are actually the ones who do the “work” (Strauss, Fagerhaugh, Suczek, & Wiener, 1982; Unruh & Pratt, 2007), which may include “maintenance of physical and social well-being, managing health information, and carrying out therapeutics as needed for the care and treatment of illnesses and injuries” (T. Zayas-Cabán & P. F. Brennan, 2007, p. 884), practical, cognitive, and socio-emotional tasks (Hinder & Greenhalgh, 2012), or illness-related (e.g., symptom management), everyday life (e.g., household management), and biographical (e.g., “coming to grips with things”) work (Corbin & Strauss, 1985). Hence, the relevant attributes of these individuals, such as their knowledge or physical strength, must be taken into account, just as with those of any other workers.
The components “tasks,” “tools and technologies,” “organization,” and “internal environment” are included in SEIPS 2.0, as in the original SEIPS model. Tasks are the specific actions within larger work processes. Task factors in SEIPS 2.0 are attributes or characteristics of the task such as difficulty, complexity, variety, ambiguity, and sequence. Tools and technologies are the objects that people use to do work or that assist people in doing work. In the healthcare domain there are many tools and technologies, including many information technologies and medical devices, as well as physical tools and equipment. Tool and technology factors in SEIPS 2.0 can be characteristics such as usability, accessibility, familiarity, level of automation, portability, and functionality. “Organization” broadly refers to the structures external to a person (but often put in place by people) that organize time, space, resources, and activity. Within institutions, organization factors can be characteristics of work schedules and assignments, management and incentive systems, organizational culture, training, policies, and resource availability. In other settings, such as the patient’s home or community, organization factors can be the communication infrastructure, living arrangements, family roles and responsibilities, work and life schedules, interpersonal relationships, culture, social norms and rules, and financial and health-related resources. It is noteworthy that organization factors have both social (e.g., culture) and technical (e.g., technical infrastructure) as well as sociotechnical (e.g., chain of command) characteristics (Pasmore, 1988). Internal environment in SEIPS 2.0 – called simply “environment” in the original SEIPS model – refers to the physical environment. Internal environment factors include characteristics of lighting, noise, vibration, temperature, physical layout and available space, and air quality (Alvarado, 2012). Although it is commonplace in other disciplines (e.g., sociology) to talk about “social environments” (Yen & Syme, 1999), social factors are typically assigned elsewhere in the work system model, for example, under “organization.”
Consistent with the most recent work of Carayon and colleagues (2013; Kelly et al., 2013) as well as other sociotechnical systems models (Karsh, et al., 2006; Kleiner, 2006; Moray, 2000), SEIPS 2.0 includes an “external environment,” which incorporates macro-level societal, economic, ecological, and policy factors outside an organization. This can be seen as a critical addition to human factors and related sub-disciplines such as macroergonomics, cultural ergonomics, and community ergonomics (Aykin, Quaet-Faslem, & Milewski, 2006; Bradley, 2006; Moray, 2000; J. H. Smith et al., 2002). Furthermore, it is necessary to understand the external environment in order to study and intervene on various healthcare phenomena. This is a fundamental precept in ecological models of health promotion, which have been popularized in the past few decades (Richard, Gauvin, & Raine, 2011). Furthermore, recent human factors analyses in healthcare have found it necessary to account for the national workforce and regulatory issues that impact healthcare worker fatigue such as residents (Ulmer, Wolman, & Johns, 2008); the regulatory and professional forces that impact the adoption and use of new health information technology (Holden, 2012); federal government, regulatory group, and local governance influence on an outbreak of hospital-based infections (Waterson, 2010); and the insurance or welfare policy factors that affect a patient’s ability to receive appropriate home care (Henriksen, Joseph, & Zayas-Cabán, 2009).
The SEIPS 2.0 model posits a hierarchical arrangement of the work system by distinguishing between individuals and teams under the person(s) component, between people and organization factors, and between the internal and external environments. The notion of hierarchy is important in human factors research and practice (Hendrick, 2002; Rasmussen, 1997). Additionally, there is growing recognition that healthcare phenomena at one level, for example, in a clinical unit, operating room, or patient home, are influenced by phenomena at levels above (e.g., the culture of the larger organization, the hospital’s surgical enterprise, or community) and below (e.g., the skills or behaviors of individuals or teams) (Hackman, 2003; Karsh, 2006). Recent scholarly works argue that if healthcare human factors has taken the first step of recognizing multiple level interactions and cross-level effects, then the next step is to develop and test specific hypotheses using theories and methods designed for this express purpose (Karsh & Brown, 2010; Karsh, Waterson, & Holden, 2013; Waterson, 2009). Some healthcare human factors models have taken steps in this direction (Carayon & Gurses, 2005; Holden & Karsh, 2009; Holden, Scanlon, et al., 2011; Karsh & Brown, 2010; Karsh, et al., 2006; Karsh, et al., 2013). For example, Karsh and colleagues (2013) illustrated a mesoergonomic approach to multiple-level human factors research using the case of hospital-acquired infection outbreaks in the UK National Health Service (NHS). The analysis not only identified contributory factors at many levels of hierarchy – government, regulatory, the governing board of the NHS trust, hospital management, clinical management, equipment and buildings – but also theorized cross-level and multilevel effects such as an “alignment” of latent failures across all levels, promoting patterns of risky behavior (Waterson, 2010).
2.1.1. The concept of configuration
According to SEIPS 2.0, any number of work system components can interact simultaneously, at “a moment in time,” to shape performance processes and outcomes. This assumes that all of the components and their elements (e.g., the many potential people, tasks, tools, organizations, and environments involved) are networked, that each can interact with any other, and that often multiple components are interacting at once. This is challenging to depict in a two-dimensional figure, so some of the interactions, especially those between three or more components, cannot be directly shown. The focus on interactions is a fundamental and unique characteristic of the human factors discipline (International Ergonomics Association, 2000; Waterson, 2009; Wilson, 2000) and is central to the novel SEIPS 2.0 concept, configuration.
The idea of configuration is that while all components of the work system potentially interact, only a subset of all possible interactions is actually relevant in a given work process or situation. What is “relevant” is based on the strength of influence of the interactions on work process performance. Thus, for a particular process or situation, one can distinguish a configuration of a finite number of relevant elements that interact to strongly shape the performance of that process. There will also be an infinite set of networked elements that are present but not relevant because they weakly shape performance. For a different process, sub-process, set of processes, or a different situation, the configuration of relevant interactions will likely differ, with a new set of elements affecting performance, some strongly and some weakly. In a network analogy, this is akin to a subset of nodes in a network being active above a threshold level, while countless nodes may have nonzero levels of activation.‡ In Figure 1, the above ideas are represented by showing a finite number of relevant elements (spheres) under each work system component. Varying sphere sizes in the figure reflect that even among elements that strongly influence performance, there are varying degrees of influence.
Under the configural view, the performance of a process is the emergent property of the whole interacting system, not of its separate parts (Dekker, et al., 2013; Wilson, 2013). Furthermore, the set of relevant interactions is dynamic and situation-specific, meaning that at different times and for different processes, different work system configurations must be described.
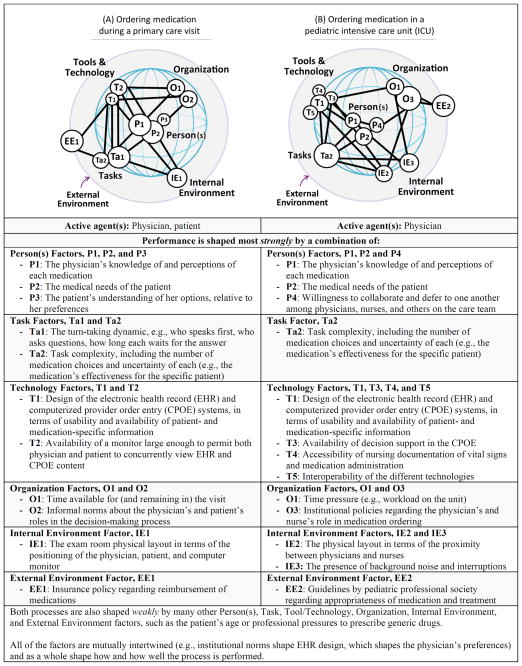
2.1.2. Applying the SEIPS 2.0 configural work system concept
Several uses of the concept of configuration are possible. One is to diagram the active and interacting work system factors for two processes. This is illustrated in Figure 2, which depicts the relevant work system configuration for two hypothetical healthcare work processes: “ordering medication during a primary care visit” (A) and “ordering medication in a pediatric intensive care unit” (B). The two processes were chosen to show how both common and unique work system factors interact to form two different configurations that shape the performance of two variants of the same type of activity or work process (i.e., medication ordering). The comparison of work system configurations for two processes, as in Figure 2, might be used by a designer or decision maker to implement solutions such as computerized order entry systems that can address system factors common to both processes, as well as process-specific system factors and interactions. Note that to construct Figure 2, we selected a non-comprehensive set of work system factors for illustration purposes. The set was derived from our accumulated research experience with these two processes. In practice, a configural diagram can be built through expert input, literature review, a voluntary reporting system, observations, interviews, surveys, and other methods.
Figure 2.
Illustration of the configural work system concept and configural diagrams.
It will also be possible to use this diagramming approach to assess differences in systems that may account for different performance outcomes (e.g., success vs. failure). Similarly, one could use the configural diagram to assess the work system configurations in incident or accident investigations (Lawton et al., 2012). This might result in identifying common factors and, more importantly, common interactions and configurations across multiple safety events (Wiegmann & Shappell, 2003). Diagramming configurations could also serve as a means for conveying safety science principles to healthcare stakeholders. For example, configural diagrams could show that accidents result from a “perfect storm” of chance combinations or that the same work system factors and interactions active in accidents are also present and may be necessary for successful performance (Woods, Dekker, Johannessen, & Sarter, 2010).
By using the configural work system diagram for safety event analysis, it will also be possible to investigate the accidents that occurred when a particular work system factor (e.g., excessive workload) or combination of factors (e.g., workload and worker fatigue) were an active ingredient of the configuration. The diagram can also be used to compare how two or more units or organizations have configured their work system, by design or otherwise, for the same process or processes. Beyond this, one might identify ideal types of configurations (Miller, 1996) exhibited by successful units or organizations, or identify how units or organizations configure for efficiency versus safety versus resilience. The diagram can also be used for planning and redesign purposes. For example, a planning team can create and compare several possible future configurations using the configural work system model. Doing so should stimulate systems-oriented considerations such as “If we introduce technology A versus technology B, which new interactions will become relevant between each of those technologies and the work system’s people, task, other tool and technology, organization, internal environment and external environment factors?”
A final suggested use of the configural diagram is to examine phenomena that evolve over time and therefore may be best analyzed by comparing the change in work system configurations, or lack thereof. An analysis of safety-related system factors and outcomes might, for example, illustrate how major work system changes at one point had a gradual or delayed (e.g., latent, accumulated) effect on outcomes later on (Reason, 1995) or uncover migrations towards higher levels of risk, tighter coupling, or the normalization of deviance (Cook & Rasmussen, 2005).
2.2. Work processes in SEIPS 2.0
The middle of Figure 1 depicts work processes. Based on the work of Karsh and Holden (Holden, 2011a; Karsh, et al., 2006), SEIPS 2.0 posits that these can be decomposed into physical, cognitive, and social/behavioral performance processes. Performance processes can be further decomposed into specific activities – paid or unpaid, core or peripheral to care, etc. – that result in accomplishing some goal or outcome. “Workflow” is a construct isomorphic to process that has particular relevance to and traction in the healthcare industry, especially in the context of health information technology (Carayon, et al., 2010; Unertl, Novak, Johnson, & Lorenzi, 2010).
2.2.1. The concept of engagement
A novel way to decompose work processes in SEIPS 2.0 is to differentiate work activities based on who is actively engaged in performing them. To be engaged is to be an active agent who performs some or all of a health-related work activity. Indirect or passive contributors are called “co-agents” in recognition of their presence but also their relative inactivity. Note that agency is an assignment, not an enduring property of a person. Thus, multiple individuals can be agents at a given time or for a given process, including healthcare professionals, patients, family or community members, and countless others. In an outpatient office visit attended by a primary care physician, elderly patient with dementia, and the patient’s daughter, perhaps the physician and daughter are the agents who do most of the “work” of talking, planning, and remembering. Nevertheless, the patient remains a co-agent by being materially present, participating even minimally, and having previously articulated his wishes to his daughter. (These wishes may be accounted for as one “person(s) factor” in the work system configuration, in addition to other person(s) factors such as the physician’s knowledge and the daughter’s attitude.) Just as there are infinite configurations of a work system, there are infinite combinations of agents and co-agents. However, for simplification, SEIPS 2.0 plots three ideal-type categories along the continuum of engagement: professional, patient, and collaborative work.
2.2.2. Professional work (Table 2)
Table 2.
Example of professional work: replacing a heart valve on a sedated patient.
|
Professional work – Work in which a healthcare professional or team of professionals are the primary agents, with minimal active involvement of patients, family caregivers, and other non-professionals Example: Surgery team replacing the aortic valve on a sedated patient |
|
Agent(s): Cardiac surgeon, fellow surgeon, physician assistant, anesthesia attending, perfusionist, scrub nurse, circulating nurse Co-agent(s): Anesthesia fellow, anesthesia resident, supply technician, patient |
| Work system factors. Person(s) factors include skill levels of all of the involved parties, experience with the procedure, and professionals’ personal preferences concerning the procedure (e.g., preferences for tools and supplies, use of time-outs, and patient transfer processes). Task factors include the difficulty of the surgical case and the familiarity of work tasks for various team members. Tool/technology factors include the availability or usability of patient monitoring technologies and patient checklists, various other medical devices (anesthesia machine, perfusion machine), supplies, whiteboard, and various checklists (e,g, surgical equipment count checklist). Organization factors include the number of hours or surgeries worked per day by the team members, whether work-arounds need to be used due to lack of personnel, whether all team members can work in unison and can speak up, and the availability of appropriate detailed procedures for emergency situations. Internal environment factors include operating room hygiene, lighting, air quality, noise, workspace design and layout, and operating room size. External environment factors may be the impact of budget and cost on the quality of the tools/technologies used, market-influenced pay levels for personnel, and societal expectations for patient and family preferences. These factors interact to shape surgical performance. |
| Process. The process of surgically replacing the aortic valve of a patient includes applying the anesthetics to the patient, surgical skin preparation to prevent infections, inserting central line(s), opening the patient, connecting the patient to the perfusion machine, aortic cross clamp, delivering cardioplegia to stop the heart and the cardiopulmonary bypass, replacing the aortic valve, restarting the heart, disconnecting the patient from the perfusion machine, placing pacing wires and drainage tubes, and closing the patient. Performance of each may be shaped by unique configurations of work system factors. |
| Outcomes. Proximal outcomes include successful completion of the surgery, minimal errors and adverse events (such as intraoperative aortic dissection), and surgical team member stress and fatigue. Distal outcomes include full recovery of the patient, patient satisfaction with their care and trust in the healthcare delivery system, no downstream complications (e.g., healthcare-associated infections), job satisfaction of surgical team members, and long-term profits for the institution. |
In professional work, the primary agent is a professional or team of professionals, with minimal active patient, family caregiver, or other non-professional involvement. Professionals may be physicians, nurses, pharmacists, technicians, medical assistants, social workers, hospital clergy, physical therapists, secretaries, and others. Not all provide medical care but to be agents they must engage in some form of health-related work. One example of professional work, described in Table 2, is the replacement of an aortic valve on a sedated patient. In the example, the agents are members of a surgical team working together. The patient and family are co-agents because they are not able to participate in the surgery, even if they may have had active engagements earlier, for example, in deciding about, communicating about, and preparing for the surgery.
2.2.3. Patient work (Table 3)
Table 3.
Example of patient work: home-based management of heart failure medications.
|
Patient work – Work in which the patient (and/or family caregiver) is the primary agent, with minimal active healthcare professional involvement. Example: Patient managing heart failure medications at home with the help of a spouse. |
|
Agent(s): Patient, patient’s spouse.a Co-agent(s): Physicians, nurses, pharmacists, clergy, other family members (e.g., son visiting his mother). |
| Work system factors. Person(s) factors include the age, cognitive function, and attitudes of the patient and spouse toward medications. Task factors include the number of medications, the complexity of the medication regimen, and the real or perceived side effects of medications. Tool/technology factors include the presence and design of a pillbox system, the clarity of written notes and instructions, and access to telehealth and telemonitoring systems that connect patients to remote healthcare professionals. Organization factors include whether the patient or spouse works during the day, the affordability of medications, and the social influence imposed on the patient to adhere to the medication regimen. Internal environment factors might include lighting, clutter, and noise in the area where medications are managed. External environment factors include the financial, motivational, and spiritual support offered by the patient’s local community. These factors interact to shape the performance of medication management. |
| Process. The process of home-based medication management could be decomposed into tasks such as learning the medication regimen, procuring and refilling medications, planning doses, adjusting the regimen, preparing to take the medication (e.g., obtaining water, meal), taking the medication, documenting medication taking, and communicating about the medication to healthcare professionals. Performance of each may be shaped by unique configurations of work system factors. |
| Outcomes. From a clinical perspective, the main outcomes may be accurate and timely (i.e., adherent) medication taking (proximal) and resultant health or disease control (distal). Whether the patient is readmitted for heart failure exacerbation affects hospital (organizational) outcomes, both proximal (e.g., patient census) and distal (e.g., penalties for exceeding average national heart failure readmission rates). For the patient and spouse, the outcomes may be clinical, functional, or personal, including feeling better or being symptom-free (proximal), hiking with friends, living to a certain age (distal), and satisfaction with specific clinical encounters (proximal) and with their course of care (distal). Other outcomes may include financial ones, including continuing to work and avoiding hospitalization. |
Note that the work may become collaborative if, for example, a home health nurse or case manager is assigned to assist with medications. Additionally, co-agents may become agents when their roles becomes more direct, as when the patient’s son moves home to help his mother, which may include preparing and reminding her about medications.
Patient work involves the active engagement of a patient, family caregiver, and other non-professional (the term “patient work” is used for simplification). Healthcare professionals are minimally involved in this type of work. There is growing recognition that many patients – and even potential patients currently free from illness – are engaged in health-related activities and are not passive recipients of professional care (Unruh & Pratt, 2007). Indeed, patient and family engagement in health-related activities has been referred to as “the blockbuster drug of the century” (Dentzer, 2013, p. 202) and a “key component in the redesign of health care processes” (Longtin et al., 2010, p. 53). Various models are emerging that conceptualize and promote patient, family, and citizen engagement (Carman et al., 2013; Health Canada, 2000; Hibbard, Stockard, Mahoney, & Tusler, 2004). Likewise, there are national and global efforts, such as Stage 3 of Meaningful Use and the Blue Button Pledge in the US, which attempt to leverage health information technology to increase patient and family engagement (National eHealth Collaborative, 2012; Westat, 2013). It is therefore important that human factors models and methods take into account the idea that patients, families, and others can be engaged in “work” and that this work be appropriately supported (Holden & Mickelson, 2013; Unruh & Pratt, 2007; T. Zayas-Cabán & P. F. Brennan, 2007).
Patient work activities can be clinically recommended (e.g., medication taking and symptom monitoring) or logistical and coordination activities (e.g., scheduling appointments, consuming information about health, and communicating with healthcare professionals). Other activities that influence health such as nutrition, exercise, and hygiene can also be included in this type of work. Another classification of patient work distinguishes between “maintenance of physical and social well-being, managing health information, and carrying out therapeutics as needed for the care and treatment of illnesses and injuries” (T. Zayas-Cabán & P. F. Brennan, 2007, p. 884). Table 2 describes one example of patient work: patient management of heart failure medications.
2.2.4. Collaborative professional-patient work (Table 4)
Table 4.
Example of collaborative work: Family-centered rounds in a pediatric hospital.
|
Collaborative work – Work in which both healthcare professionals and patients (and/or family) are jointly and actively involved. Example: Family-centered rounds in a pediatric hospital. |
|
Agent(s): Child, parents, physician, nurse, pharmacist, social worker. Co-agent(s): Unit clerk, pharmacist, and imaging technicians. |
| Work system factors. Person(s) factors include age and health status of child, attitudes and perceptions of parents toward rounds, and communication style of physicians and other healthcare professionals. Task factors include the characteristics of the assessment and plan for the day; the order of the review of orders; the timeline of the discharge plan; and the quality of interactions/Q&A between child, parent and healthcare professionals. Tool/technology factors might be the availability of a computer-on-wheel with access to electronic health records for placing orders during rounds and the presence of a (digital or analog) whiteboard to display information to all involved. Organization factors include roles of the healthcare professionals (e.g., who presents, who is in charge) and the scheduling of rounds. Internal environment factors include the location of rounds (e.g., in patient room, in hallway) and the physical proximity of each agent. External environment factors might be availability of community resources for post-discharge support to the family and policies related to the privacy of health information. These factors interact to shape the performance of rounds. |
| Process. The process of family-centered rounds could be decomposed in phases, such as pre-rounding performed by nurses and physicians to gather information from family (e.g., questions), the actual rounds, and post-round follow-up with family. Performance of each process and sub-process (e.g., assessment, discharge planning) may be shaped by unique configurations of work system factors. |
| Outcomes. Key proximal clinical outcomes may be timely processing of orders and shared understanding of the care plan as well as distal consequences (e.g., delay in discharge, medical errors). For the child and parents, proximal outcomes include the perception of participation in care decisions, a feeling of being informed about the next steps, and global satisfaction with the clinical encounter. These proximal outcomes can affect distal outcomes, such as long-term trust, satisfaction, and post-discharge behavior. |
Collaborative work is work in which both professionals and non-professionals (e.g., patients) are actively engaged agents. Many processes in healthcare involve collaboration between professionals and non-professionals. For example, in a specialty care clinic visit, both clinicians and patients (or family members) must provide and process information. Other processes can be, but are not always, collaborative. A nurse might treat a pediatric patient’s wound alone, in which case this is professional work, or the nurse might engage in collaborative work by treating the wound with a family member in order to provide education. As another example, patients may self-diagnose or self-medicate without involving professionals (patient work) or contact a healthcare professional for advice via a patient portal’s messaging system (collaborative work). Table 4 provides another illustration of collaborative work: family-centered rounds in a pediatric hospital. (Note that for present purposes, work done by teams of professionals without patient or family involvement would be categorized as “professional work,” even though elsewhere it is referred to as “collaborative” (e.g., Reddy, Gorman, & Bardram, 2011; Salas, Wilson, Murphy, King, & Salisbury, 2008).)
2.3. Work outcomes in SEIPS 2.0
The rightmost side of the model depicts work outcomes for patients, professionals, and organizations. Outcomes are defined as states or conditions resulting from the work process. Outcomes are important indicators of performance, but are not the only indicators. For example, process indicators such as timeliness or efficiency can also be important indicators of quality and safety (Donabedian, 1988; Holden, Brown, et al., 2011).
Patient, professional, and organizational outcomes are ostensibly related (e.g., Fogarty & Mckeon, 2006), but more research is needed to support this contention. Proximal and distal outcomes can be distinguished given that some outcomes may be the immediate result of work processes while others are further down the causal chain and may only emerge over time (Karsh, et al., 2006). Outcomes can be desirable or undesirable. The specific outcomes considered in an analysis may reflect the goals of different stakeholders such as clinicians, organizational leaders, regulators, payors and, perhaps most importantly, patients (Reuben & Tinetti, 2012). Table 5 provides some examples of outcomes.
Table 5.
Examples of work outcomes.
| Patient outcomes | Professional outcomes | Organizational outcomes | |
|---|---|---|---|
| Proximal |
|
|
|
| Distal |
|
|
|
2.3.1. The concept of adaptation
SEIPS 2.0 depicts feedback loops, representing intended and unintended adaptations. In dynamic systems, processes and their outcomes are monitored; then, adaptations are made in an attempt to decrease the gap between actual versus ideal performance (Hollnagel & Woods, 2005).
Some recent models inspired by the SEIPS model have been especially attentive to the idea that the work system is not static and that systems are frequently perturbed and transformed by the introduction of new technology (Holden, Brown, et al., 2011), improvement programs such as lean thinking (Holden, 2011b), and planned redesign efforts in general (Karsh, et al., 2006). The transition to hospice care is an example of a planned adaptation of patient work. These planned adaptations are often anticipated, staged, and long-lasting, although their specific consequences may not be (Campbell, Sittig, Ash, Guappone, & Dykstra, 2006).
Adaptations can also be reactive, intermittent, and short-lasting, such as the first-order problem-solving behaviors of nurses who encounter day-to-day operational problems (e.g., lacking supplies or medications) (Tucker & Spear, 2006) or patients experimenting with a new diet. Some adaptations can involve a combination of anticipatory control and reactive adjustments, for example, the blood glucose control achieved by expert diabetics (Altman Klein & Lippa, 2008). Wilson (2013) writes that the systems principle of emergence states that not all adaptations are easily predictable or beneficial. However, as seen in the ubiquity of workarounds in healthcare settings (Halbesleben, Wakefield, & Wakefield, 2008), and specifically workarounds of health information technology (Gurses, Xiao, & Hu, 2009; Holden, Rivera-Rodriguez, Faye, Scanlon, & Karsh, in press; Novak, Holden, Anders, Hong, & Karsh, in press) and medical devices (Gurses, Kim, et al., 2012; Pennathur et al., 2013), adaptations are an inevitability of complex sociotechnical systems (Wilson, 2013). The workarounds or ad-hoc adaptations seen in healthcare may be one way that healthcare professionals “balance” their work system when one of its components (e.g., a policy or technology) is relatively fixed (Carayon, et al., 2013). The same may be true of patients or patient-professional teams, as exemplified by studies reporting that chronically ill patients come to rely on new technologies or other people to compensate for irresolvable physical, cognitive, and motivational challenges (Riegel & Carlson, 2002).
3. Key implications and future directions
Healthcare is a complex sociotechnical system (Carayon, 2006). It involves multiple agents with different goals as well as complex evolving technologies, processes, and external forces. The original SEIPS model offered a conceptual framework that captured healthcare’s complexity and was easy to use by diverse stakeholders, especially those not trained in human factors. SEIPS 2.0 extends the original model by introducing contemporary human factors concepts and retains its ability to capture complexity while being easy to use. The extensions in SEIPS 2.0 are necessary for this human factors framework to be relevant in light of the contemporary view that healthcare work systems are dynamic, collaborative, multilevel, adaptive, and include patients and families as actual or potential agents. Certainly, the core issues and values in healthcare will change with time, and human factors as a discipline as well as its models and methods must evolve to continue to be useful and relevant. Accordingly, future considerations for the SEIPS model may include adding components from other system-based models (Carayon, 2006; Karsh, et al., 2006) or unpacking the model’s current components, for example, by distinguishing between physical vs. information and communication tools and technologies. Another future pursuit may be to expand the person(s) component to more fully depict the complexity of teams and other collectives, including team composition and structure, team-related technical and nontechnical skills, intra-team communication options, and interpersonal and social dynamics. These and any other expansions, however, should be made with care because the five original components of the model plus the external environment are a manageable number to remember and present while being fairly inclusive.
As highlighted by Waterson (2009), human factors research in healthcare needs to give serious consideration to system interactions. This is a key concept in SEIPS 2.0, which introduces the notion that various configurations or networks of work system components contribute to various processes and outcomes. More research needs to be done using the configural approach. Additionally, there needs to be more work looking at multiple levels, including beyond the single organization, to capture the multi-level nature of healthcare phenomena such as patient safety (Schutz, Counte, & Meurer, 2007). Future work can draw on concepts from the ‘meso’ paradigm (House, Rousseau, & Thomas-Hunt, 1995; Karsh, et al., 2013) and from the literature on levels in general (Rousseau, 1985) including specifying causal relationships across levels (“cross-level effects,” e.g., how do a work system’s organization-level factors affect individual and team factors, and vice versa?) and causal patterns replicated across levels (“multilevel effects,” e.g., does the relationship between clinical team situation awareness and clinical team performance parallel that of individual situation awareness and individual performance?).
Health and healthcare work are increasingly viewed as collaborative activities that can include teams of professionals, non-professionals, or, increasingly, a combination of both. To date, a vast majority of human factors studies and applications have focused on single professionals or co-located professional teams. For example, prior applications of the original SEIPS model include using its work system categories to identify and describe critical care nurses’ performance obstacles (Gurses & Carayon, 2007; Gurses, Carayon, & Wall, 2008), physicians’ barriers and facilitators to health information technology use (Holden, 2011c), factors affecting the motivation and satisfaction of tele-ICU nurses (P. L. Hoonakker et al., 2013), key work system factors in cardiac surgery (Gurses, Kim, et al., 2012; D. A. Wiegmann, A. A. Eggman, A. W. ElBardissi, S. H. Parker, & T. M. Sundt, 2010), and factors shaping community pharmacists’ implementation of medication therapy management (Chui, et al., 2012). In addition to human factors approaches to professional healthcare work, Holden and Mickelson (2013) argue for more patient-engaged human factors:
Patient-engaged human factors is the application of human factors theories and principles, methods and tools, analyses, and interventions to study and improve work done by patients and families, alone or in concert with healthcare professionals.
The relative lack of patient-engaged human factors research and application is a gap worth addressing, as various studies, including ones of chronic diseases such as heart failure and diabetes, argue that patients’ health-related activities can be and are often viewed as work that takes place within sociotechnical systems (Gallacher, May, Montori, & Mair, 2011; Granger, Sandelowski, Tahshjain, Swedberg, & Ekman, 2009; Strauss, et al., 1982). The concept of patient work implies the importance of applying human factors techniques and frameworks such as cognitive task analysis and control theory (Altman Klein & Meininger, 2004; Lippa, Altman Klein, & Shalin, 2008) or user-centered design of tools, technologies, and equipment (Fisk, Rogers, Charness, Czaja, & Sharit, 2009; Mayhorn, Lanzolla, Wogalter, & Watson, 2005; Morrow et al., 2005; Ward, Buckle, & Clarkson, 2010) to study and improve work done by patients. Similarly, conceptual models such as SEIPS 2.0 could be fruitfully applied to patient work. For instance, Zayas Cabán and Brennan (2007) used the SEIPS work system model to characterize person(s), task, tool/technology, organization, and environment factors from the perspective of a home-based patient. Additionally, human factors scholars and practitioners should more thoroughly consider collaborative work that involves both professionals and patients (and their families). In one recent example, Carayon and colleagues (2011) used the SEIPS work system model to identify barriers and facilitators to family engagement in bedside rounds. Data were collected from parents and children, and various healthcare team members (physician, nurse, pharmacist) by using the stimulated recall methodology. Henriksen and colleagues proposed a human factors model of home healthcare that mirrored the SEIPS model and considered quality and safety as the joint product of patient and professional factors as well as a broad array of systems-based factors (Henriksen, et al., 2009). Several groups have also developed tools and processes for patients and family members to identify patient safety events and participate in quality improvement efforts (Coulter & Ellins, 2007; Giles, Lawton, Din, & McEachan, 2013; Unruh & Pratt, 2007; Weingart et al., 2005; Weingart et al., 2011). Apart from those and several other human factors projects on patient work, there are also multiple emerging streams of research on patient and collaborative patient-professional work that might benefit from partnership with human factors researchers. These includes work on concepts of patient workload and complexity (Shippee, Shah, May, Mair, & Montori, 2012) and self-management behavior “in the wild” (Hinder & Greenhalgh, 2012). In summary, more is needed in the area of patient-engaged human factors, consistent with the recognized need for patients to play an active role in their health, safety, and quality improvement (Berwick, 2009; Toussaint, 2009; Vincent & Coulter, 2002; Wagner et al., 2001).
With respect to work outcomes and adaptations, it is important for human factors studies to take into account multiple outcomes: from safety and worker well-being to productivity, efficiency, and organizational performance (Dul, et al., 2012). More research is needed to show how these outcomes are interrelated. Furthermore, as adaptations are being identified in healthcare work, it will be important to study work over time and to identify how work systems are being adjusted in planned and unplanned ways. Some of the adaptations constitute violations of protocol or take workers into zones of unfamiliar performance and may therefore have safety consequences (Alper et al., 2012; Holden, et al., in press). Other adaptations may be safe and effective and therefore should be studied as useful, potentially replicable strategies. Adaptations related to technologies, in particular, could be an area of future research, as significant evidence exists demonstrating that when technologies are introduced, various worker- and management-driven adaptations emerge, for better or for worse (Koppel, Wetterneck, Telles, & Karsh, 2008; Novak, Brooks, Anders, Gadd, & Lorenzi, 2012; Novak, et al., in press; Pennathur, et al., 2013). A useful framework for future research on adaptations might consider whether – or under which conditions – adaptations can “balance” a work system to create fit between work system components (e.g., between new technology and task characteristics) as well as compensate for less than desirable attributes of difficult-to-change work system components (e.g., federal regulations). The earlier discussion about assessing configurations over time to understand longitudinal outcomes also applies to the need to consider how work system configurations change over time as a result of feedback and adaptation.
A final major future direction is to develop a practical toolkit to accompany the SEIPS 2.0 conceptual framework. The toolkit would build on prior applications of the SEIPS model (see Table 1) and the methods already established in those applications, such as the identification of barriers across the work system or the evaluation of relationships between work systems, processes, and outcomes. Established tools and methods should be supplemented by new ones, including the configural diagram and its various uses, described above. New tools and methods should support a range of activities including planning and organizational decision making, training and education, analysis, design and redesign, evaluation, or a combination of these. They should also be either broadly applicable or tailored to multiple areas, including patient and employee safety; health information technology, medical devices, and other tools; care coordination and transition management; patient and family engagement; system and process (workflow) improvement; job design and workload; cognition, decision making, and expertise; and teamwork, communication, and interruptions. Application domains to be considered should include the hospital, primary and specialty care, long-term care facilities, the patient home and community, and anywhere else where health- and healthcare-related work occurs.
4. Conclusion
One of the greatest contributions of human factors to the healthcare domain is the discipline’s focus on work systems and its various sociotechnical system models (Norris, 2012). Both human factors and healthcare are evolving, requiring continual updating of sociotechnical systems models to accommodate new science and practice as well as new domain-specific concerns and needs. SEIPS 2.0 updates a widely used human factors framework that will no doubt require future updating. In the meantime, we offer SEIPS 2.0 as a useful conceptual model and analytic tool for the use of anyone interested in studying and improving work done by healthcare professionals, patients, family caregivers, and mixed professional-patient teams.
Practitioner summary.
SEIPS 2.0 is a new human factors/ergonomics framework for studying and improving health and healthcare. It describes how sociotechnical systems shape health-related work done by professionals and non-professionals, independently and collaboratively. Work processes, in turn, shape patient, professional, and organizational outcomes. Work systems and processes undergo planned and unplanned adaptations.
Acknowledgments
We thank Russ Beebe for his support in developing the figures and the anonymous reviewers for their feedback. The manuscript was partially supported by the Clinical and Translational Science Award (CTSA) program, previously through the National Institutes of Health (NIH) National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. Dr. Holden was supported by NCATS grant 2KL2TR000446-06 through the Vanderbilt CTSA. Dr. Gurses was supported in part by an Agency for Healthcare Research and Quality K01 grant (HS018762) for her work on this paper. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
We note here: (1) while patients or caregivers can have professions, they are “non-professionals” to the extent that their involvement in care is not a function of those professions and (2) the term “family caregiver” here refers to individuals providing informal care but does not imply that only family members provide informal care or that family members’ health-related roles are confined to caregiving.
In the original formulation, the “person” could be either a healthcare professional or a patient (Carayon, et al., 2006)
Another analogy is of different atomic elements combining through strong or weak bonds to form different molecules. The varying strength of bonds could be depicted in the model by changing the line color or thickness between the elements.
Contributor Information
Richard J. Holden, Assistant Professor, Department of Medicine, Division of General Internal Medicine & Public Health, Department of Biomedical Informatics Vanderbilt University School of Medicine, Phone: +1-615-936-4343, Fax: +1-615-936-7373, Center for Research and Innovation in Systems Safety, 719 Medical Arts Building, 1211 21st Avenue S, Nashville, TN, 37212.
Pascale Carayon, Email: carayon@engr.wisc.edu, Procter & Gamble Bascom Professor in Total Quality, Department of Industrial and Systems Engineering, Director of the Center for Quality and Productivity Improvement, University of Wisconsin-Madison, 3126 Engineering Centers Building, 1550 Engineering Drive, Madison, WI 53706 - USA, tel: +1-608-265-0503 or +1-608-263-2520, fax: +1-608-263-1425
Ayse P. Gurses, Email: agurses1@jhmi.edu, Associate Professor, Armstrong Institute for Patient Safety and Quality, Department of Anesthesiology and Critical Care Medicine, Division of Health Sciences Informatics, School of Medicine, Department of Health Policy and Management, Bloomberg School of Public Health, Department of Civil Engineering, Whiting School of Engineering, The Johns Hopkins University, 750 E. Pratt St. 15thFloor, Baltimore, MD 21202, Phone: +1-410-637-4387
Peter Hoonakker, Email: PHoonakker@cqpi.engr.wisc.edu, Research Scientist and Associate Director of Research, Center for Quality and Productivity Improvement, University of Wisconsin-Madison, 3132 Engineering Centers Building, 1550 Engineering Drive, Madison, WI 53706 – USA, Phone: +1-608-658 0837, Fax: +1-608-263-1425
Ann Schoofs Hundt, Email: hundt@cqpi.engr.wisc.edu, Associate Scientist and Associate Director of Education, Center for Quality and Productivity Improvement, University of Wisconsin-Madison, 3132 Engineering Centers Building, 1550 Engineering Drive, Madison, WI 53706 – USA, Phone: +1-608-262-9100, Fax: +1-608-263-1425
A. Ant Ozok, Email: ozok@umbc.edu, Associate Professor, Department of Information Systems, UMBC, Adjunct Associate Professor, Department of Anesthesiology, Visiting Associate Professor, The Armstrong Institute of Patient Safety and Quality, School of Medicine, The Johns Hopkins University, 1000 Hilltop Circle, Baltimore, MD 21250, Phone : +1-410-455-8627, Fax : +1-410-455-1073
A. Joy Rivera-Rodriguez, Email: rodrig7@clemson.edu, Assistant Professor, Department of Industrial Engineering, Clemson University, Phone: +1-864-656-3114, Fax: +1-864-656-0795, 130-C Freeman Hall, Box 340920 Clemson, SC 29631
References
- Alper SJ, Holden RJ, Scanlon MC, Patel NR, Kaushal R, Skibinski K, Karsh B. Self-reported violations during medication administration in two pediatric hospitals. BMJ Quality & Safety. 2012;21:408–415. doi: 10.1136/bmjqs-2011-000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman Klein H, Lippa KD. Type 2 diabetes self-management: Controlling a dynamic system. Journal of Cognitive Engineering and Decision Making. 2008;2:48–62. [Google Scholar]
- Altman Klein H, Meininger AR. Self management of medication and diabetes: Cognitive control. IEEE Transactions on Systems, Man and Cybernetics. 2004;34:718–725. [Google Scholar]
- Alvarado CJ. The physical environment in health care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2. Boca Raton, FL: CRC Press; 2012. pp. 215–234. [Google Scholar]
- Ausserhofer D, Schubert M, Desmedt M, Blegen MA, De Geest S, Schwendimann R. The association of patient safety climate and nurse-related organizational factors with selected patient outcomes: a cross-sectional survey. International Journal of Nursing Studies. 2013;50:240–252. doi: 10.1016/j.ijnurstu.2012.04.007. [DOI] [PubMed] [Google Scholar]
- Aykin N, Quaet-Faslem PH, Milewski AE. Cultural ergonomics. In: Salvendy G, editor. Handbook of Human Factors and Ergonomics. Hoboken, NJ: Wiley; 2006. pp. 177–190. [Google Scholar]
- Berwick DM. What ‘patient-centered’ should mean: Confessions of an extremist. Health Affairs. 2009;28:w555–w565. doi: 10.1377/hlthaff.28.4.w555. [DOI] [PubMed] [Google Scholar]
- Boston-Fleischhauer C. Enhancing healthcare processes with human factors engineering and reliability science, Part 2: Applying tne knowledge to clinical documentation systems. Journal of Nursing Administration. 2008a;38(2):84–89. doi: 10.1097/01.NNA.0000295637.03216.26. [DOI] [PubMed] [Google Scholar]
- Boston-Fleischhauer C. Enhancing healthcare processes with human factors engineering and reliability science: Part 1: Setting the context. Journal of Nursing Administration. 2008b;38(1):27–32. doi: 10.1097/01.NNA.0000295632.80345.3d. [DOI] [PubMed] [Google Scholar]
- Bradley G. Social and Community Informatics: Humans on the Net. New York: Routledge; 2006. [Google Scholar]
- Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. Journal of the American Medical Informatics Association. 2006;13:547–556. doi: 10.1197/jamia.M2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P. Human factors of complex sociotechnical systems. Applied Ergonomics. 2006;37:525–535. doi: 10.1016/j.apergo.2006.04.011. [DOI] [PubMed] [Google Scholar]
- Carayon P. The Balance Theory and the work system model... Twenty years later. International Journal of Human-Computer Interaction. 2009;25:313–327. [Google Scholar]
- Carayon P, editor. Handbook of Human Factors and Ergonomics in Patient Safety. 2. Mahwah, NJ: Lawrence Erlbaum; 2012. [Google Scholar]
- Carayon P, Alyousef B, Hoonakker P, Schoofs Hundt A, Cartmill R, Tomcavage J, Walker J. Challenges to care coordination posed by the use of multiple health IT applications. Work. 2012;41(2):4468–4473. doi: 10.3233/WOR-2012-0746-4468. [DOI] [PubMed] [Google Scholar]
- Carayon P, Cartmill R, Blosky MA, Brown R, Hackenberg M, Hoonakker PLT, Walker JM. ICU Nurses’ Acceptance of electronic health records. JAMIA. 2011;18(6):812–819. doi: 10.1136/amiajnl-2010-000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Cartmill R, Hoonakker P, Schoofs Hundt A, Karsh B, Krueger D, Wetterneck TB. Human factors analysis of workflow in health information technology implementation. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Patient Safety. 2. Mahwah, NJ: Lawrence Erlbaum; 2012. pp. 507–521. [Google Scholar]
- Carayon P, DuBenske LL, McCabe BC, Shaw B, Gaines ME, Kelly MM, Cox ED. Work system barriers and facilitators to family engagement in rounds in a pediatric hospital. In: Albolino S, Bagnara S, Bellandi T, editors. Healthcare Systems Ergonomics and Patient Safety. Boca Raton, FL: CRC Press; 2011. pp. 81–85. [Google Scholar]
- Carayon P, Gurses AP. A human factors engineering conceptual framework of nursing workload and patient safety in intensive care units. Intensive and Critical Care Nursing. 2005;21:284–301. doi: 10.1016/j.iccn.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Carayon P, Gurses AP. Nursing workload and patient safety-a human factors engineering perspective. In: Quality AfHRa., editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: AHRQ; 2008. [Google Scholar]
- Carayon P, Hundt AS, Alvarado CJ, Springman S, Borgsdorf A, Jenkins L. Implementing a systems engineering intervention for improving safety in outpatient surgeries. Advances in Patient Safety: From Research to Implementation. 2005;3:305–321. [PubMed] [Google Scholar]
- Carayon P, Karsh B, Cartmill R, Hoonakker P, Hundt AS, Krueger D, Wetterneck TB. Incorporating Health IT Into Workflow Redesign - Summary Report. Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- Carayon P, Schoofs Hundt A, Karsh B, Gurses AP, Alvarado CJ, Smith M, Brennan PF. Work system design for patient safety: the SEIPS model. Quality & Safety in Health Care. 2006;15:i50–i58. doi: 10.1136/qshc.2005.015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Smith P, Hundt AS, Kuruchittham V, Li Q. Implementation of an electronic health records system in a small clinic. Behaviour and Information Technology. 2009;28(1):5–20. [Google Scholar]
- Carayon P, Smith PD. Evaluating the human and organizational aspects of information technology implementation in a small clinic. In: Smith MJ, Salvendy G, editors. Systems, Social and Internationalization Design Aspects of Human-Computer Interaction. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. pp. 903–907. [Google Scholar]
- Carayon P, Wetterneck TB, Hundt AS, Ozkaynak M, DeSilvey J, Ludwig B, Rough SS. Evaluation of nurse interaction with bar code medication administration technology in the work environment. Journal of Patient Safety. 2007;3(1):34–42. [Google Scholar]
- Carayon P, Wetterneck TB, Hundt AS, Ozkaynak M, Ram P, DeSilvey J, Sobande S. Observing nurse interaction with infusion pump technologies. Advances in Patient Safety: From Research to Implementation. 2005;2:349–364. [PubMed] [Google Scholar]
- Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden RJ, Gurses AP. Human factors systems approach to healthcare quality and patient safety. Applied Ergonomics. 2013 doi: 10.1016/j.apergo.2013.04.023. forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, Sweeney J. Patient and family engagement: A framework for understanding the elements and developing interventions and policies. Health Affairs. 2013;32:223–231. doi: 10.1377/hlthaff.2012.1133. [DOI] [PubMed] [Google Scholar]
- Catchpole K, McCulloch P. Human factors in critical care: Towards standardized integrated human-centered systems of work. Current Opinion in Critical Care. 2010;16(6):618–622. doi: 10.1097/MCC.0b013e32833e9b4b. [DOI] [PubMed] [Google Scholar]
- Chui MA, Mott DA, Maxwell L. A qualitative assessment of a community pharmacy cognitive pharmaceutical services program, using a work system approach. Research in Social & Administrative Pharmacy. 2012;8:206–216. doi: 10.1016/j.sapharm.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook RI, Rasmussen J. “Going solid”: A model of system dynamics and consequences for patient safety. Quality & Safety in Health Care. 2005;14:130–134. doi: 10.1136/qshc.2003.009530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbin J, Strauss A. Managing chronic illness at home: Three lines of work. Qualitative Sociology. 1985;8:224–247. [Google Scholar]
- Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. British Medical Journal. 2007;335:24–27. doi: 10.1136/bmj.39246.581169.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Savigny D, Adam T, editors. Systems Thinking for Health Systems Strengthening. Geneva, Switzerland: Alliance for Health Policy and Systems Research, World Health Organization; 2009. [Google Scholar]
- Dekker SWA, Hancock PA, Wilkin P. Ergonomics and sustainability: Towards an embrace of complexity and emergence. Ergonomics. 2013;56(3):357–364. doi: 10.1080/00140139.2012.718799. [DOI] [PubMed] [Google Scholar]
- Dentzer S. Rx for the ‘blockbuster drug’ of patient engagement. Health Affairs. 2013;32:202. doi: 10.1377/hlthaff.2013.0037. [DOI] [PubMed] [Google Scholar]
- Donabedian A. The quality of care. How can it be assessed? Journal of the American Medical Asssociation. 1988;260:1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- Dul J, Bruder R, Buckle P, Carayon P, Falzon P, Marras WS, van der Doelen B. A strategy for human factors/ergonomics: Developing the discipline and profession. Ergonomics. 2012;55:377–395. doi: 10.1080/00140139.2012.661087. [DOI] [PubMed] [Google Scholar]
- Faye H, Rivera-Rodriguez AJ, Karsh BT, Hundt Schoofs A, Baker C, Carayon P. Involving ICU Nurses in a Proactive Risk Assessment of the Medication Management Process. The Joint Commission Journal on Quality and Patient Safety. 2010;36(8):376–384. doi: 10.1016/s1553-7250(10)36056-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisk AD, Rogers WA, Charness N, Czaja SJ, Sharit J. Designing for Older Adults: Principles and Creative Human Factors Approaches. 2. Boca Raton, FL: CRC Press; 2009. [Google Scholar]
- Fogarty GJ, Mckeon CM. Patient safety during medication administration: The influence of organizational and individual variables on unsafe work practices and medication errors. Ergonomics. 2006;49:444–456. doi: 10.1080/00140130600568410. [DOI] [PubMed] [Google Scholar]
- Gallacher K, May CR, Montori VM, Mair FS. Understanding patients’ experiences of treatment burden in chronic heart failure using Normalization Process Theory. Annals of Family Medicine. 2011;9:235–243. doi: 10.1370/afm.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giles SJ, Lawton RJ, Din I, McEachan RR. Developing a patient measure of safety (PMOS) BMJ Quality & Safety. 2013;22:554–562. doi: 10.1136/bmjqs-2012-000843. [DOI] [PubMed] [Google Scholar]
- Granger BB, Sandelowski M, Tahshjain H, Swedberg K, Ekman I. A qualitative descriptive study of the work of adherence to a chronic heart failure regimen: Patient and physician perspectives. Journal of Cardiovascular Nursing. 2009;24(4):308–315. doi: 10.1097/JCN.0b013e3181a4be30. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Carayon P. Performance obstacles of intensive care nurses. Nursing Research. 2007;56:185–194. doi: 10.1097/01.NNR.0000270028.75112.00. [DOI] [PubMed] [Google Scholar]
- Gürses AP, Carayon P. Performance obstacles of intensive care nurses. Nursing Research. 2007;56(3):185–194. doi: 10.1097/01.NNR.0000270028.75112.00. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Carayon P, Wall M. Impact of performance obstacles on intensive care nurses’ workload, perceived quality and safety of care, and quality of working life. Health Services Research. 2008;44:422–443. doi: 10.1111/j.1475-6773.2008.00934.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurses AP, Kim G, Martinez E, Marsteller J, Bauer L, Lubomski L, Thompson D. Identifying and categorizing patient safety hazards in cardiovascular operating rooms using an interdisciplinary approach: A multisite study. BMJ Quality & Safety. 2012;21:810–818. doi: 10.1136/bmjqs-2011-000625. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Marsteller JA, Ozok AA, Xiao Y, Owens S, Pronovost PJ. Using an interdisciplinary approach to identify factors that affect clinicians’ compliance with evidence-based guidelines. Critical Care Medicine. 2010;38:S282–S291. doi: 10.1097/CCM.0b013e3181e69e02. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Ozok AA, Pronovost PJ. Time to accelerate integration of human factors and ergonomics in patient safety. BMJ Quality & Safety. 2012;21:347–351. doi: 10.1136/bmjqs-2011-000421. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Xiao Y, Hu P. User-designed information tools to support communication and care coordination in a trauma hospital. Journal of Biomedical Informatics. 2009;42:667–677. doi: 10.1016/j.jbi.2009.03.007. [DOI] [PubMed] [Google Scholar]
- Hackman JR. Learning more by crossing levels: Evidence from airplanes, hospitals, and orchestras. Journal of Organizational Behavior. 2003;25:905–922. [Google Scholar]
- Halbesleben JRB, Wakefield DS, Wakefield BJ. Work-arounds in health care settings: Literature review and research agenda. Health Care Management Review. 2008;33:2–12. doi: 10.1097/01.HMR.0000304495.95522.ca. [DOI] [PubMed] [Google Scholar]
- Health Canada. Health Canada Policy Toolkit for Public Involvement in Decision Making. Ottawa, Ontario: 2000. [Google Scholar]
- Hendrick HW. An overview of macroergonomics. In: Hendrick HW, Kleiner BM, editors. Macroergonomics: Theory, methods and applications. Mahwah, NJ: Lawrence Erlbaum Associates; 2002. pp. 1–23. [Google Scholar]
- Henriksen K, Joseph A, Zayas-Cabán T. The human factors of home health care: A conceptual model for examining safety and quality concerns. Journal of Patient Safety. 2009;5:229–236. doi: 10.1097/PTS.0b013e3181bd1c2a. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research. 2004;39:1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinder S, Greenhalgh T. “This does my head in”. Ethnographic study of self-management by people with diabetes. BMC Health Services Research. 2012;12 doi: 10.1186/1472-6963-12-83. http://www.biomedcentral.com/1472-6963/12/83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ. Cognitive performance-altering effects of electronic medical records: An application of the human factors paradigm for patient safety. Cognition, Technology & Work. 2011a;13:11–29. doi: 10.1007/s10111-010-0141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ. Lean thinking in emergency departments: A critical review. Annals of Emergency Medicine. 2011b;57:265–278. doi: 10.1016/j.annemergmed.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ. What stands in the way of technology-mediated patient safety improvements? A study of facilitators and barriers to physicians’ use of electronic health records. Journal of Patient Safety. 2011c;7:193–203. doi: 10.1097/PTS.0b013e3182388cfa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ. Social and personal normative influences on healthcare professionals to use information technology: Towards a more robust social ergonomics. Theoretical Issues in Ergonomics Science. 2012;13:546–569. doi: 10.1080/1463922X.2010.549249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ, Brown RL, Alper SJ, Scanlon MC, Patel NR, Karsh B. That’s nice, but what does IT do? Evaluating the impact of bar coded medication administration by measuring changes in the process of care. International Journal of Industrial Ergonomics. 2011;41:370–379. doi: 10.1016/j.ergon.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ, Karsh B. A theoretical model of health information technology usage behaviour with implications for patient safety. Behaviour & Information Technology. 2009;28:21–38. [Google Scholar]
- Holden RJ, Mickelson RS. Performance barriers among elderly chronic heart failure patients: An application of patient-engaged human factors and ergonomics. Proceedings of the Human Factors and Ergonomics Society 2013 [Google Scholar]
- Holden RJ, Rivera-Rodriguez AJ, Faye H, Scanlon MC, Karsh B. Automation and adaptation: Nurses’ problem-solving behavior following the implementation of bar coded medication administration technology. Cognition, Technology & Work. doi: 10.1007/s10111-10012-10229-10114. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ, Scanlon MC, Patel NR, Kaushal R, Escoto KH, Brown RL, Karsh B. A human factors framework and study of the effect of nursing workload on patient safety and employee quality of working life. BMJ Quality & Safety. 2011;20:15–24. doi: 10.1136/bmjqs.2008.028381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollnagel E, Woods DD. Joint Cognitive Systems: Foundations of Cognitive Systems Engineering. New York: CRC Press; 2005. [Google Scholar]
- Hollnagel E, Woods DD, Leveson N, editors. Resilience Engineering: Concepts and Precepts. Aldershot, UK: Ashgate; 2006. [Google Scholar]
- Hoonakker PL, Carayon P, McGuire K, Khunlertkit A, Wiegmann DA, Alyousef B, Wood KE. Motivation and job satisfaction of Tele-ICU nurses. Journal of Critical Care. 2013;28:315, e313–321. doi: 10.1016/j.jcrc.2012.10.001. [DOI] [PubMed] [Google Scholar]
- Hoonakker PLT, Carayon P. The Impact of Health Information Technology on Workload of ICU Nurses. Paper presented at the ICOH WOPS Conference; Amsterdam, The Netherlands. 2010. [Google Scholar]
- Hoonakker PLT, Carayon P, Brown RL, Cartmill RS, Wetterneck TB, Walker JM. Changes in end-user satisfaction with CPOE over time among nurses and providers in Intensive Care Units. JAMIA. 2013;20:252–259. doi: 10.1136/amiajnl-2012-001114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoonakker PLT, Carayon P, Khunlertkit A, Mcguire K, Wiegmann D. Case Study Research: An example from the tele-ICU. In: Goebel M, Christie CJ, Zschernack S, Todd AI, Mattison M, editors. Organizational Design And Management (ODAM) X. I. Grahamstown, South Africa: IEA Press; 2011. pp. 121–127. [Google Scholar]
- Hoonakker PLT, Carayon P, McGuire K, Khunlertkit A, Wiegmann D, Alyousef B, Wood K. Motivation and Job Satisfaction of Tele-ICU Nurses. Journal of Critical Care. 2013 doi: 10.1016/j.jcrc.2012.10.001. [DOI] [PubMed] [Google Scholar]
- Hoonakker PLT, Carayon P, Walker JM, Brown RL, Cartmill RS. The effects of Computerized Provider Order Entry implementation on communication in Intensive Care Units. International Journal of Medical Informatics (IJMI) 2013;82(5):e107–e117. doi: 10.1016/j.ijmedinf.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoonakker PLT, Khunlertkit A, Mcguire K, Wiegmann D, Carayon P, Wood K. A day in life of a tele-Intensive Care Unit nurse. Paper presented at the Healthcare Systems Ergonomics and Patient Safety (HEPS) 2011 Conference Oviedo; Spain. 2011. [Google Scholar]
- Hoonakker PLT, Khunlertkit A, Tattersall M, Keevil J, Smith PD. Computer decision support tools in primary care. Work. 2012;41(2):4474–4478. doi: 10.3233/WOR-2012-0747-4474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoonakker PLT, Wetterneck TB, Carayon P, Cartmill RS, Walker JM. Drug Safety Alerts Override from a Human factors Perspective. Paper presented at the Healthcare Systems Ergonomics and Patient Safety (HEPS) 2011 Conference Oviedo; Spain. 2011. [Google Scholar]
- House R, Rousseau DM, Thomas-Hunt M. The meso paradigm: A framework for the integration of micro and macro organizational behavior. Research in Organizational Behavior. 1995;17:71–114. [Google Scholar]
- Hundt AS, Adams JA, Schmid JA, Musser LM, Walker JM, Wetterneck TB, Carayon P. Conducting an efficient proactive risk assessment prior to CPOE implementation in an intensive care unit. Int J Med Inform. 2013;82(1):25–38. doi: 10.1016/j.ijmedinf.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hundt AS, Hoonakker P, Carayon P, Den Herder R, Cartmill R, Walker J, Topper J. Organizational learning in a large-scale complex health IT project. Paper presented at the Human Factors and Ergonomics Society 56th Annual Meeting; 2012; Boston, MA. 2012. [Google Scholar]
- Hysong S, Sawhney M, Wilson L, Sittig DF, Esquivel A, Watford M, Singh H. Improving outpatient safety through effective electronic communication: a study protocol. Implementation Science. 2009;4(1):62. doi: 10.1186/1748-5908-4-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- Institute of Medicine. Building a Better Delivery System: A New Engineering/Health Care Partnership. Washington, DC: National Academies Press; 2005. [Google Scholar]
- International Ergonomics Association. The Discipline of Ergonomics. 2000 from http://www.iea.cc/01_what/What%20is%20Ergonomics.html.
- Johnson K, Valdez RS, Casper GR, Kossman SP, Carayon P, Or CK, Brennan PF. Experiences of technology integration in home care nursing. AMIA Annu Symp Proc. 2008;6:389–393. [PMC free article] [PubMed] [Google Scholar]
- Karsh B. Meso-ergonomics: A new paradigm for macroergonomics research. Paper presented at the International Ergonomics Association; Maastricht, Netherlands. 2006. [Google Scholar]
- Karsh B, Brown R. The impact of levels on theory, measurement, analysis, and intervention in medical error research: the case of patient safety health information technology. Applied Ergonomics. 2010;41:674–681. doi: 10.1016/j.apergo.2009.12.007. [DOI] [PubMed] [Google Scholar]
- Karsh B, Carayon P, Smith M, Skibinski K, Thomadsen B, Brennan P, Murray ME. The University of Wisconsin-Madison multidisciplinary graduate certificate in patient safety. In: Henriksen K, Battles J, Marks EE, Lewis DI, editors. Advances in Patient Safety: From Resarch to Implementation. Vol. 4. Rockville, MD: 2005. pp. 269–281. [PubMed] [Google Scholar]
- Karsh B, Holden RJ. New technology implementation in health care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Patient Safety. Mahwah, NJ: Lawrence Erlbaum; 2007. pp. 393–410. [Google Scholar]
- Karsh B, Holden RJ, Alper SJ, Or CKL. A human factors engineering paradigm for patient safety – designing to support the performance of the health care professional. Quality & Safety in Health Care. 2006;15:i59–i65. doi: 10.1136/qshc.2005.015974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karsh B, Waterson PE, Holden RJ. Crossing levels in systems ergonomics: Outlining a framework for ‘mesoergonomics’. Applied Ergonomics. 2013 doi: 10.1016/j.apergo.2013.04.021. in press http://dx.doi.org/10.1016/j.apergo.2013.1004.1021. [DOI] [PMC free article] [PubMed]
- Katz D, Kahn RL. Common characteristics of open systems. In: Katz D, Kahn RL, editors. The Social Psychology of Organizations. New York: John Wiley & Sons; 1966. pp. 14–29. [Google Scholar]
- Kelly MM, Xie A, Carayon P, DuBenske LL, Ehlenbach ML, Cox ED. Strategies for improving family engagement during family-centered rounds. Journal of Hospital Medicine. 2013;8:201–207. doi: 10.1002/jhm.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiner BM. Macroergonomics: Analysis and design of work systems. Applied Ergonomics. 2006;37:81–89. doi: 10.1016/j.apergo.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Koppel R, Wetterneck TB, Telles JL, Karsh B. Workarounds to barcode medication administration systems: Their occurrences, causes, and threats to patient safety. Journal of the American Medical Informatics Association. 2008;15:408–423. doi: 10.1197/jamia.M2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton R, McEachan RRC, Giles SJ, Sirriyeh R, Watt IS, Wright J. Development of an evidence-based framework of factors contributing to patient safety incidents in hospital settings: A systematic review. BMJ Quality & Safety. 2012;21:369–380. doi: 10.1136/bmjqs-2011-000443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippa KD, Altman Klein H, Shalin VL. Everyday expertise: Cognitive demands in diabetes self-management. Human Factors. 2008;50:112–120. doi: 10.1518/001872008X250601. [DOI] [PubMed] [Google Scholar]
- Longtin Y, Sax H, Leape LL, Sheridan SE, Donaldson L, Pittet D. Patient participation: current knowledge and applicability to patient safety. Mayo Clinic Proceedings. 2010;85:53–62. doi: 10.4065/mcp.2009.0248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnussen J, Vrangbæk K, Saltman RB, editors. Nordic Health Care Systems: Recent Reforms and Current Policy Challenges. Berkshire, England: Open University Press; 2009. [Google Scholar]
- Martinez EA, Thompson DA, Errett NA, Kim GR, Bauer L, Lubomski LH, Pronovost PJ. Review article: high stakes and high risk: a focused qualitative review of hazards during cardiac surgery. Anesthesia & Analgesia. 2011;112:1061–1074. doi: 10.1213/ANE.0b013e31820bfe8e. [DOI] [PubMed] [Google Scholar]
- Mayhorn CB, Lanzolla VR, Wogalter MS, Watson AM. Personal digital assistants (PDAs) as medication reminding tools: Exploring age differences in usability. Gerontechnology. 2005;4:128–140. [Google Scholar]
- Miller D. Configurations revisited. Strategic Management Journal. 1996;17:502–512. [Google Scholar]
- Moray N. Culture, politics and ergonomics. Ergonomics. 2000;43:858–868. doi: 10.1080/001401300409062. [DOI] [PubMed] [Google Scholar]
- Morrow DG, Weiner M, Young J, Steinley D, Deer M, Murray MD. Improving medication knowledge among older adults with heart failure: A patient-centered approach to instruction design. The Gerontologist. 2005;45:545–552. doi: 10.1093/geront/45.4.545. [DOI] [PubMed] [Google Scholar]
- National eHealth Collaborative. The Patient Engagement Framework. 2012 Retrieved May 2, 2013, from http://www.nationalehealth.org/patient-engagement-framework.
- National Research Council. Health Care Comes Home: The Human Factors. Washington, DC: National Academies Press. Committee on the Role of Human Factors in Home Health Care, Board on Human-Systems Integration, Division of Behavioral and Social Sciences and Education; 2011. [Google Scholar]
- Norris BJ. Systems human factors: How far have we come? BMJ Quality & Safety. 2012;21:713–714. doi: 10.1136/bmjqs-2011-000476. [DOI] [PubMed] [Google Scholar]
- Novak LL, Brooks J, Anders S, Gadd CS, Lorenzi NM. Mediating the intersections of organizational routines during the introduction of health IT systems. European Journal of Information Systems. 2012 doi: 10.1057/ejis.2012.2. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak LL, Holden RJ, Anders SH, Hong JY, Karsh B. Using a sociotechnical framework to understand adaptations in health IT. International Journal of Medical Informatics. doi: 10.1016/j.ijmedinf.2013.01.009. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasmore WA. Designing Effective Organizations: The Sociotechnical Systems Perspective. New York, NY: Wiley; 1988. [Google Scholar]
- Patterson ES, Woods DD, Roth EM, Cook RI, Wears RL, Render ML. Three key levers for achieving resilience in medication delivery with information technology. Journal of Patient Safety. 2006;2:33–38. [Google Scholar]
- Pennathur PR, Thompson DA, Abernathy JH, Martinez EA, Pronovost PJ, Kim GR, Gurses AP. Technologies in the wild (TiW): Human factors implications for patient safety in the cardiovascular operating room. Ergonomics. 2013 doi: 10.1080/00140139.2012.757655. in press. [DOI] [PubMed] [Google Scholar]
- Pronovost PJ, Goeschel CA, Marsteller JA, Sexton JB, Pham JC, Berenholz SM. Framework for patient safety research and improvement. Circulation. 2009;119:330–337. doi: 10.1161/CIRCULATIONAHA.107.729848. [DOI] [PubMed] [Google Scholar]
- Rasmussen J. Risk management in a dynamic society: A modelling problem. Safety Science. 1997;27:183–213. [Google Scholar]
- Reason J. A systems-approach to organizational error. Ergonomics. 1995;38:1708–1721. [Google Scholar]
- Reason J. Human error: Models and management. British Medical Journal. 2000;320:768–770. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy MC, Gorman P, Bardram J. Special issue on Supporting collaboration in healthcare settings: the role of informatics. International Journal of Medical Informatics. 2011;80:541–543. doi: 10.1016/j.ijmedinf.2011.05.001. [DOI] [PubMed] [Google Scholar]
- Reuben DB, Tinetti ME. Goal-oriented patient care: An alternative health outcomes paradigm. New England Journal of Medicine. 2012;366:777–779. doi: 10.1056/NEJMp1113631. [DOI] [PubMed] [Google Scholar]
- Richard L, Gauvin L, Raine K. Ecological models revisited: Their uses and evolution in health promotion over two decades. Annual Review of Public Health. 2011;32:307–326. doi: 10.1146/annurev-publhealth-031210-101141. [DOI] [PubMed] [Google Scholar]
- Riegel B, Carlson B. Facilitators and barriers to heart failure self-care. Patient Education and Counseling. 2002;46(4):287–295. doi: 10.1016/s0738-3991(01)00165-3. [DOI] [PubMed] [Google Scholar]
- Rivera AJ, Karsh BT. Human Factors and Systems Engineering Approach to Patient Safety for Radiotherapy. Int J Radiation Oncology Biol Phys. 2008;71(1):S174–S177. doi: 10.1016/j.ijrobp.2007.06.088. [DOI] [PubMed] [Google Scholar]
- Rousseau DM. Issues of level in organizational research: Multilevel and cross level perpectives. Research in Organizational Behavior. 1985;7:1–37. [Google Scholar]
- Russ AL, Fairbanks RJ, Karsh B, Militello LG, Saleem JJ, Wears RL. The science of human factors: Separating fact from fiction. BMJ Quality & Safety. 2013 doi: 10.1136/bmjqs-2012-001450. forthcoming, http://dx.doi.org/10.1136/bmjqs-2012-002036. [DOI] [PMC free article] [PubMed]
- Salas E, Burke CS, Cannon-Bowers JA. Teamwork: Emerging principles. International Journal of Management Reviews. 2000;2:339–356. [Google Scholar]
- Salas E, Fiore SM. Team Cognition: Understanding the Factors that Drive Process and Performance. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- Salas E, Wilson KA, Murphy CE, King H, Salisbury M. Communicating, coordinating, and cooperating when lives depend on it: Tips for teamwork. Joint Commission Journal on Quality and Patient Safety. 2008;34:333–341. doi: 10.1016/s1553-7250(08)34042-2. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer BK, Vishwanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: Jossey-Bass; 2008. pp. 465–485. [Google Scholar]
- Scandrett KG, Anichini MA, Berdes C, Estabrook S, Boockvar K, Saliba D, Taylor SL. Patient safety in the nursing home: how nursing staff assess and communicate about change in condition. Journal of Gerontological Nursing. 2012;38:28–37. doi: 10.3928/00989134-20121003-03. [DOI] [PubMed] [Google Scholar]
- Schroeder M, Carayon P, Li Q. Anesthesia providers’ perceptions of smart infusion pump; Paper presented at the ASA’ 2005 Conference..2005. Oct 22–26, [Google Scholar]
- Schutz AL, Counte MA, Meurer S. Assessment of patient safety research from an organizational ergonomics and structural perspective. Ergonomics. 2007;50:1451–1484. doi: 10.1080/00140130701346765. [DOI] [PubMed] [Google Scholar]
- Shekelle PG, Wachter RM, Pronovost PJ, et al. RE-bP Center, editor. Making Helath Care Safer II: An Updated Critical Analysis of the Evidence for Patient Safety Practices. Comparative Effectiveness Review No. 211. Rockville, MD: 2013. Vol. Publicatin No. 13-E001-EF. [PMC free article] [PubMed] [Google Scholar]
- Shippee ND, Shah ND, May CR, Mair FS, Montori VM. Cumulative complexity: A functional, patient-centered model of patient complexity can improve research and practice. Journal of Clinical Epidemiology. 2012;65:1041–1051. doi: 10.1016/j.jclinepi.2012.05.005. [DOI] [PubMed] [Google Scholar]
- Singh H, Thomas EJ, Mani S, Sittig DF, Arora H, Espadas H, Petersen LA. Tinely follow-up of abnormal disgnostic imaging test results in an outpatient setting: Are electronic medical records achieving their potential. Archives of Internal Medicine. 2009;169(17):1578–1586. doi: 10.1001/archinternmed.2009.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sittig DF, Singh H. Eight rights of safe electronic health record use. Journal of the American Medical Association. 2009;302(10):1111–1113. doi: 10.1001/jama.2009.1311. [DOI] [PubMed] [Google Scholar]
- Smith JH, Cohen WJ, Conway FT, Carayon P, Derjani-Bayeh A, Smith MJ. Community ergonomics. In: Hendrick HW, Kleiner BM, editors. Macroergonomics: Theory, Methods, and Applications. Mahwah, NJ: Lawrence Erlbaum; 2002. pp. 289–309. [Google Scholar]
- Smith MJ, Sainfort-Carayon P. Balance theory of job design for stress reduction. International Journal of Industrial Ergonomics. 1989;4:67–79. [Google Scholar]
- Strauss A, Fagerhaugh S, Suczek B, Wiener C. The work of hospitalized patients. Social Science & Medicine. 1982;16:977–986. doi: 10.1016/0277-9536(82)90366-5. [DOI] [PubMed] [Google Scholar]
- Toussaint J. Writing the new playbook for U.S. health care: Lessons from Wisconsin. Health Affairs. 2009;28:1343–1350. doi: 10.1377/hlthaff.28.5.1343. [DOI] [PubMed] [Google Scholar]
- Tucker AL, Spear SJ. Operational failures and interruptions in hospital nursing. HSR: Health Services Research. 2006;41:643–662. doi: 10.1111/j.1475-6773.2006.00502.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulmer C, Wolman DW, Johns ME, editors. Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- Unertl KM, Novak LL, Johnson KB, Lorenzi NM. Traversing the many paths of workflow research: Developing a conceptual framework of workflow terminology through a systematic literature review. Journal of the American Medical Informatics Association. 2010;17:265–273. doi: 10.1136/jamia.2010.004333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unruh KT, Pratt W. Patients as actors: the patient’s role in detecting, preventing, and recovering from medical errors. International Journal of Medical Informatics. 2007;76:S236–S244. doi: 10.1016/j.ijmedinf.2006.05.021. [DOI] [PubMed] [Google Scholar]
- Vincent C, Coulter A. Patient safety: What about the patient? Quality & Safety in Health Care. 2002;11:76–80. doi: 10.1136/qhc.11.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. British Medical Journal. 1998;316:1154–1157. doi: 10.1136/bmj.316.7138.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wachter RM. Patient safety at ten: Unmistakable progress, troubling gaps. Health Affairs. 2009;29:165–173. doi: 10.1377/hlthaff.2009.0785. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: Translating evidence into action. Health Affairs. 2001;20:64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- Ward J, Buckle P, Clarkson PJ. Designing packaging to support the safe use of medicines at home. Applied Ergonomics. 2010;41:682–694. doi: 10.1016/j.apergo.2009.12.005. [DOI] [PubMed] [Google Scholar]
- Waterson PE. A critical review of the systems approach within patient safety research. Ergonomics. 2009;52:1185–1195. doi: 10.1080/00140130903042782. [DOI] [PubMed] [Google Scholar]
- Waterson PE. A systems ergonomics analysis of the Maidstone and Tunbridge Wells infection outbreaks. Ergonomics. 2010;52:1196–1205. doi: 10.1080/00140130903045629. [DOI] [PubMed] [Google Scholar]
- Weingart SN, Pagovich O, Sands DZ, Li JM, Aronson MD, Davis RB, Phillips RS. What can hospitalized patients tell us about adverse events? Learning from patient-reported incidents. Journal of General Internal Medicine. 2005;20:830–836. doi: 10.1111/j.1525-1497.2005.0180.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weingart SN, Zhu J, Chiappetta L, Stuver SO, Schneider EC, Epstein AM, Weissman JS. Hospitalized patients’ participation and its impact on quality of care and patient safety. International Journal for Quality in Health Care. 2011;23:269–277. doi: 10.1093/intqhc/mzr002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westat. Findings and Lessons From the Enabling Patient-Centered Care Through Health IT Grant Initiative. Rockville, MD: Agency for Healthcare Research and Quality; 2013. (AHRQ Publication No. 13-0011-EF) [Google Scholar]
- Wetterneck TB, Brown RL, Carayon P, Kleppin SM, Hundt AS, Ozkaynak M. End-user response to intravenous infusion pump medication dosing alerts: An analysis of user-interface events. In: Tartaglia R, Bagnara S, Bellandi T, Albolino S, editors. Healthcare Systems Ergonomics and Patient Safety. Florence, Italy: Taylor & Francis; 2005. pp. 235–238. [Google Scholar]
- Wetterneck TB, Walker JM, Blosky MA, Cartmill RS, Hoonakker PLT, Johnson MA, Carayon P. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. JAMIA. 2011;18(6):774–782. doi: 10.1136/amiajnl-2011-000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiegmann D, Eggman A, ElBardissi A, Parker S, Sundt T. Improving cardiac surgical care: A work systems approach. Applied Ergonomics. 2010;41(5):701–712. doi: 10.1016/j.apergo.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiegmann DA, Eggman AA, ElBardissi AW, Parker SH, Sundt TM. Improving cardiac surgical care: A work systems approach. Applied Ergonomics. 2010;41:701–712. doi: 10.1016/j.apergo.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiegmann DA, Shappell SA. Human Error Approach to Aviation Accident Analysis: The Human Factors Analysis and Classification System. Aldershot, UK: Ashgate; 2003. [Google Scholar]
- Wilson JR. Fundamentals of ergonomics in theory and practice. Applied Ergonomics. 2000;31:557–567. doi: 10.1016/s0003-6870(00)00034-x. [DOI] [PubMed] [Google Scholar]
- Wilson JR. Fundamentals of systems ergonomics/human factors. Applied Ergonomics. 2013 forthcoming http://dx.doi.org/10.1016/j.apergo.2013.1003.1021.
- Woods DD, Dekker SCRI, Johannessen LK, Sarter N. Behind Human Error. 2. Aldershot, UK: Ashgate; 2010. [Google Scholar]
- World Health Organization. WHO Patient Safety Retrieved October. 2009;30:2009. from http://www.who.int/patientsafety/en/ [Google Scholar]
- Yen IH, Syme SL. The social environment and health: A discussion of the epidemiologic literature. Annual Review of Public Health. 1999;20:287–308. doi: 10.1146/annurev.publhealth.20.1.287. [DOI] [PubMed] [Google Scholar]
- Zayas-Cabán T, Brennan PF. Human factors in home care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. Mahwah, NJ: Erlbaum; 2007. pp. 883–897. [Google Scholar]
- Zayas-Cabán T, Brennan PT. Human factors in home care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. Mahwah, NJ: Lawrence Erlbaum Associates; 2007. pp. 883–897. [Google Scholar]
- Zayas-Cabán T, Valdez RS. Human Factors and Ergonomics in Home Care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2. Boca Raton, FL: CRC Press; 2012. pp. 743–762. [Google Scholar]