Abstract
Objective
We evaluated potential explanations for advantaged mental health status among immigrant Asian American women compared to U.S. born Asian American women.
Method
In a nationally representative sample of 1030 women (185 U.S. born, 368 early-life immigrants [arrived before age 25], 477 late-life immigrants), we examined the hypothesis that increased exposure to social risk factors mediate nativity-based differences in lifetime prevalence of depression and anxiety disorders. Indicators of social class were also examined as protective factors enjoyed by U.S. born women that may suppress observed nativity-based disparities. We also examined whether there were group differences in reactivity to stress in predicting disorder.
Results
U.S. born women were twice as likely as late-life immigrants to report lifetime history of depression (O.R. = 2.03, 95% C.I [1.35, 4.54]) and anxiety (O.R. = 2.12, 95% C.I [1.34, 5.19]). Nativity differences in perceived discrimination, family conflict, and cultural conflict explained disparities in rates of disorder. There was no support for the contention that immigrant women were more psychologically hardy or resilient to social stress.
Conclusion
Findings suggested that the gap in mental health status between U.S. and foreign born Asian American women would be indeed be magnified if differences in social status were accounted for, but also that ready explanations for the so-called immigrant paradox are found in differential levels of reported stress exposure.
Keywords: Asian American, immigrant paradox, nativity, disparities, anxiety and depression
Epidemiologic data indicate that immigrants have lower prevalence of psychiatric disorders relative to their U.S.-born counterparts (e.g., Grant et al., 2004; Vega et al., 1998). This occurs despite the fact that foreign nativity is generally thought to be associated with increased burdens of stress, poverty, and low social status (Burnham et al., 1987). Thus, this pattern of findings has been referred to as the ‘immigrant paradox’ and extends across a range of health disparities, such as reproductive health (Cervantes, Keith, & Wyshak, 1999), preventable disease (e.g., Jasso et al., 2004), and psychiatric disorders (e.g., Ortega et al., 2000; Vega et al., 2003). These data largely focus on U.S. Latinos, with recent findings suggesting the pattern may be most apparent in specific national origin groups (i.e., Mexican Americans) and certain psychiatric disorders, such as substance abuse (Alegria et al., 2008).
More limited evidence reveals this pattern among Asian Americans, in terms of both physical (Bates et al., 2008; Popkin & Udry, 1998) and mental health (Breslau & Chang, 2006). In a nationally representative sample of Asian Americans, Takeuchi et al. (2007) reported that U.S.-born women experienced a two-fold risk of anxiety disorder and depression compared to foreign-born women, but no nativity differences were reported among Asian American men. The current study examined possible explanations for this nativity-based disparity in anxiety and depression among Asian American women.
Two general classes of explanations have been advanced to explain nativity effects on health and mental health (Avecedo-Garcia & Bates, 2007; Escobar, Nervi & Gara, 2000). One class contends that the paradox merely reflects artifacts in the data. The apparent differences may be explained by underreporting of health problems by immigrants (Franzini, Ribble, & Keddie, 2001; Palloni & Morenoff, 2001). However, any differential veracity of self-reports between U.S.-born and immigrant respondents has yet to be demonstrated, and documented disparities have emerged from objective measures of health status (e.g., body mass index, mortality).
More often, nativity-based disparities are attributed to selection, whereby only exceptionally healthy individuals undertake migration. If selection is operative, one would expect lower morbidity among immigrants compared to compatriots remaining in the country of origin. The evidence for the ‘healthy immigrant hypothesis’ is mixed. On the one hand, Latino and Asian American immigrants have higher life expectancy compared to their U.S.-born counterparts and people in their home countries (Jasso et al., 2004). While suggestive, these comparisons cannot establish that immigrant health advantages are driven by selection (Avecedo-Garcia & Bates, 2007). Moreover, previous research has refuted assumptions of selection hypotheses, though prospective studies are lacking (Abraido-Lanza et al., 1999). In fact, recent data indicates that risk of first-onset anxiety and depressive disorders is higher among representative samples of Mexican American immigrants than among nonmigrants in Mexico, highlighting possible adverse effects of migration rather than healthy selection processes (Breslau et al., 2011).
The second class of explanations interprets the data as reflecting bona fide differences in health status explained by differential risk exposure. U.S.-born ethnic minorities may face chronic stressors associated with growing up in the context of minority stress (Alegria, Pescosolido, Williams, & Canino, 2011). For example, U.S.- born African Americans, Asian Americans, and Latinos report more experiences of discrimination compared to their immigrant counterparts (Finch, Kolody & Vega, 2000; Krieger et al., 2011; Perez, Fortuna, Alegria, 2008). Compared to immigrants, U.S.-born minorities may be more attuned to issues of race and class, feel more entitled to fair treatment, and thus may be more vigilant to signs of discrimination which are robustly related to both physical health problems and psychiatric disorder (Schwartz & Meyer, 2010).
In addition, U.S.-born ethnic minorities may be more likely than immigrants to experience the tensions of intrafamilial cultural conflict that can elevate psychiatric risk. Dissonant acculturation and acculturative family distancing that result in family conflict and estrangement may be more risky for U.S.-born Asian Americans where there are intergenerational differences in nativity, cultural values and experience (Hwang, Wood & Fujimoto, 2010). Among Latinos, the relationship between length of residence in the U.S. and risk of past year psychiatric disorder is explained in part by increases in family cultural conflict (e.g., perceived family interference with personal goals, arguments prompted by value conflicts) (Cook, Alegria, Lin & Guo, 2009). Thus, nativity differences in psychiatric morbidity may be attributable to differential risk experiences concerning family cultural conflict and perceived discrimination.
A related explanation of the immigrant paradox concerns the loss of culturally-mediated protective social resources in the second generation. Compared to immigrants, U.S.-born ethnic minorities may be less likely to reap the benefits of social conditions that stem from traditional values and family structures (Escobar, 1998). For example, immigrants are more likely to reside in enclaves conferring the benefits of a co-ethnic community and collective sense of identity (Stafford, Becares & Nazroo, 2010). Immigrant Asian Americans report greater extended family support and more cohesive family climates than their U.S born counterparts (Walton & Takeuchi, 2010). These psychological resources may shield immigrants from anxiety and depression, but may erode across generations and with increased length of residence in the U.S. (Alegria et al., 2008; Escobar et al., 2000).
Explanations concerning differential exposure to risk and protective factors can be tested with formal tests of mediation, yet few studies subject these explanations of nativity-based differences to empirical test. Mediation models can evaluate social stress explanations of mental health disparities, but are largely not used (Schwartz & Meyer, 2010). For example, in a review of the role of discrimination stress in mental health disparities, only five (3%) of 148 studies conducted mediation analyses (Paradies, 2006). To the extent that nativity differences in psychiatric risk can be attributed to heightened stress exposure (e.g., perceived discrimination, family/cultural conflict) and fewer traditional culture supports (e.g., low family cohesion) among U.S.-born ethnic minorities, the ‘immigrant paradox’ is explicable rather than enigmatic.
It is possible, however, that there is indeed a paradox in effect, that immigrants enjoy better mental health status than would be expected on the basis on their risk profiles relative to U.S.-born minorities. Rather than showing mediation, such analyses could reveal support for suppression effects (MacKinnon, Krull, & Lockwood, 2000), such that predicted estimates of the differences in disorder risk between nativity groups would be even greater when taking into account the heightened risk profiles of immigrants. For example, U.S.-born Asian Americans have greater social mobility than their parent’s immigrant generation on many indices of educational and occupational status, with gains most pronounced among women (Park & Meyers, 2010). Thus, because high social status and mobility are generally protective against mental disorder (Adler, Epel, Castellazzo & Ickovics, 2000), higher rates of psychiatric morbidity among Asian American women in the second generation may reflect an epidemiologic paradox. As such, we undertake both mediation and suppression analyses, as appropriate, to evaluate the immigrant paradox in risk for depression and anxiety in a nationally representative sample of Asian American women.
Finally, a third explanation of the immigrant advantage in mental health requires attention. Rather than differential risk exposure, immigrant and U.S.-born Asian Americans may evince differential reactivity to environmental stressors. U.S.-born Asian Americans may be more vulnerable to the effects of stress than their immigrant counterparts, who have been described as hardy. Hardiness is a term used to describe individuals who perceive fewer situations as stressful and whose reactions to stressors tend to be less intense, helping them resist stress-related illnesses (Funk, 1992). Hardy individuals view stressors as changeable and as challenges that provide opportunities for growth.
Immigrant Asians have been described as hardy, exhibiting high internal locus of control, reporting mastery over previous stressors, and exhibiting lower reactivity to subsequent stressful experiences (Kuo & Tsai, 1986; Noh & Avison, 1996). Immigrant hardiness may stem from the appraisal of their stress context relative to their country of origin experiences, where social disadvantage may have been both profound and normative (Alegria et al., 2008). These expectancies may protect immigrants from demoralization that sets the stage for depression and anxiety. For example, a strong monotonic increase in risk of depression in response to negative life events has been shown for highly acculturated Chinese Americans, but not among those less acculturated (Hwang & Myers, 2007). Thus, we examined nativity-based differences in the associations between perceived stressors (e.g., family/cultural conflict, discrimination) and risk of depressive and anxiety disorders among Asian American women.
In addition to examining nativity differences, we also incorporated age of immigration in our analyses because age of immigration profoundly shapes the context of the immigration experience, such as ease of adapting to English, exposure to diverse social networks, and occupational/ educational opportunities (Leu et al., 2008). Age of immigration itself predicts differential rates of disorder, although there isn’t necessarily a linear relationship with disorder risk among Asian American women (Gong et al., 2011). We contrasted U.S.-born Asian Americans with early life immigrants who migrated during childhood, adolescence or young adulthood versus later life immigrants who arrived in middle or late adulthood. Age 25 was used to demarcate immigration during formative years prior to social and cognitive maturation, completion of education and/or initiation of adult economic and family roles (Giedd, 2004; Gogtay et al., 2004).
The Current Study
We examined nativity-based differences in prevalence of lifetime depressive and anxiety disorders among Asian American women and examined explanations for observed differences. First, mediation analyses were employed to determine whether differential risk of disorder could be explained by greater stress exposure (i.e., discrimination, family/cultural conflict) among U.S.-born compared to early and later immigrant women. However, U.S.-born women may actually be exposed to less risk in some respects (i.e., subjective social status) compared to immigrants. Thus, our mediation models also considered potential suppression effects that could illustrate the paradoxical nature of an immigrant advantage in mental health. Second, we examined the differential reactivity hypothesis which asserts that U.S.-born Asian American women are more highly reactive to risk factors for disorder, such that there may be stronger associations between stress and disorder for this group. We conducted subgroup analyses and formal moderation analyses to examine this possibility.
Method
Data for the current study were obtained from the National Latino and Asian American Survey (NLAAS). The NLAAS used a multi-frame, stratified probability sampling scheme resulting in a nationally representative household sample of Latino and Asian Americans. For detailed documentation of sampling procedures, please see Alegria et al. (2004) and Heeringa et al. (2004). The interviews were offered in English, Mandarin, Cantonese, Tagalog, and Vietnamese. In generating point estimates and standard errors, weighting corrections were applied to control for differences in selection probability.
Among the surveyed Asian American females (N = 1030), 185 (18%) were US-born, and 845 (82%) were foreign-born. Consistent with previous studies using the NLAAS sample (e.g., Leu et al., 2008; Takeuchi et al., 2007) age at immigration was dichotomized at age 25 years to examine within-group differences in foreign-born immigrants. We designated those who immigrated before age 25 as early immigrants (n=368), and those who immigrated after age 25 as later life immigrants (n = 477). The three largest ethnic groups represented were Chinese (28.80%), Filipino (24.70%), and Vietnamese (25.00%). In terms of educational attainment, 766 (29.1%) had 11 or fewer years of education (less than high school graduate), 556 (21.1%) had 12 years of education (high school graduate), 660 (25.1%) had 13 to 15 years of education (some college), and 652 (24.8%) had 16 or more years of education (college graduate). In terms of annual household income, 174 (16.9%) reported less than $15,000, 131 (12.7%) reported between $15,000 and $34,999, 217 (21.1%) between $35,000 and $74,999, and 345 (33.5%) reported income greater than $75,000.
Measures
Lifetime Depressive & Anxiety Diagnoses
The World Health Organization Composite International Diagnostic Interview (World Mental Health Survey Consortium, 2004) was used to assess lifetime prevalence of psychiatric disorders with criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Any depressive disorder in the present study included diagnoses of either Major Depressive Disorder or Dysthymia. Any anxiety disorder included the following diagnoses: Generalized Anxiety Disorder, Social Phobia, Panic Disorder, Agoraphobia, Agoraphobia without Panic Disorder, and Post-Traumatic Stress Disorder.
Cultural Conflict
Cultural Conflict was assessed with 5 items asking respondents to indicate the extent to which their own personal goals and preferences conflicted with her family’s goals and customs (e.g., “Because you have different customs, you have had arguments with other members of your family.”). Items were rated on a 3-point Likert scale ranging from 1 (Often) to 3 (Hardly ever or never). Given our interpretation of cultural conflict as a risk factor, we reversed scored the scale such that higher scores indicating greater perceived cultural conflict. Internal consistency was satisfactory (Cronbach’s α= .77 to .78) across nativity groups.
Family Cohesion
Family Cohesion was assessed by 10 items asking respondents to rate their agreement with statements such as, “Family members feel loyal to the family”, and “Family members respect one another.” Responses were on a 4-point Likert scale ranging from 1 (Strongly Disagree) to 4 (Strongly Agree) with higher scores indicating perceptions of greater family closeness, loyalty, trust, and respect. Internal consistency was satisfactory (Cronbach’s α =.92 to .93) across the nativity groups.
Family Conflict
Family Conflict was assessed by 2 items on the frequency of conflict with relatives and children. Respondents were asked “Not including your (husband/wife/partner), how often do your relatives or children make too many demands on you” and “How often do your family or relatives argue with you?” Responses were made on a 4-point Likert scale ranging from 1 (Never) to 4 (Often), with higher scores indicating more conflict. Given only 2 items, internal consistency was adequate for this composite (α = .52 to .64) across the nativity groups.
Family Support
Family Support was assessed by 3 questions asking respondents to rate the frequency and extent to which they rely on family and relatives for support (e.g., “Not including your husband/wife/partner, how often do you talk on the phone or get together with family or relatives who do not live with you?”, “How much can you rely on relatives who do not live with you for help if you have a serious problem?”). Internal consistency was satisfactory (Cronbach’s α=.74 to .75) across the nativity groups. Confirmatory factor analysis supported using separate scales for Family Support and Family Conflict, as opposed to single scale to indicate family functioning.
Discrimination
Discrimination was assessed by 9 items on the perceived frequency of experiences of unfair treatment, discrimination and prejudice (e.g., “You are treated with less respect than other people” and “People act as if you are not as good as they are.”). Items were rated on a 6-point Likert scale ranging from 1 (Never) to 6 (Almost every day), with higher scores indicating greater perceived discrimination. Internal consistency was satisfactory (Cronbach’s α= .90) across the nativity groups.
Subjective Social Status
The MacArthur Scale of subjective social status (often referred to as the MacArthur ladder) is a widely used single item measure of social standing that is robustly related to health outcomes (Operario, Adler & Williams, 2004). Two dimensions of status were assessed: perceived social position in the U.S. and in the community (Adler et al., 2000). Respondents were shown a symbolic ladder with 10 rungs and were told: “Think of this ladder as representing where people stand in the United States [in your community]. At the top of the ladder are the people who are the best off, those who have the most money, most education, and best jobs. At the bottom are people who are the worst off, those who have the least money, least education, and worst jobs or no job. What is the number to the right of the rung where you think you stand at this time in your life, relative to other people in the United States [your community]?” The measure is designed allow participants to mentally summate across multiple indicators of SES, weighting each component as they see fit to arrive at their perceived social standing.
Covariates
Social desirability, age, annual household income, and education level were examined as covariates. Social desirability was assessed by 10 true/false items that assess the respondent’s motivation to appear socially appropriate and desirable. Sample items include “I have always told the truth” and “I never met a person I did not like.” Annual household income was treated as a four level categorical variable with 1) less than $15,000, 2) $15,000 – $35,000, 3) $35,000 – $75,000, and 4) $75,000+. Likewise, education level was coded as a four level categorical variable with 1) 11 years or less of education, 2) high school education, 3) college education, and 4) graduate school education. Although we have included ethnicity in our sample descriptives, we did not include it as a covariate in our multivariate analyses, Ethnicity was a sampling stratification variable, but was not a significant predictor of disorder risk (p > .05); its inclusion in the models did not produce a significant increase R2 variance explained and resulted in an artificial increase in weighted standard errors.
Results
Table 1 displays nativity subgroup differences on study variables including demographic characteristics, lifetime prevalence rates for any depressive and anxiety disorders, and reported exposure to risk and protective factors among the Asian American women in our sample.
Table 1.
Nativity differences in sociodemographics, disorder prevalence, and risk and protective factors.
| Age ≥ 25 Immigrant n = 477 |
Age ≤ 24 Immigrant n = 368 |
US-Born n = 185 |
F statistic | |
|---|---|---|---|---|
| Weighted Percentage/Mean (Standard Error)
| ||||
| Age | 49.91a (0.92) | 35.00b (0.93) | 38.30b (2.40) | F (2,45) = 66.78** |
| Education Level | F (4.27, 196.51) = 11.05** | |||
| 11 years or less | 30.65%a (2.45) | 7.45b (2.14) | 6.85b (2.81) | |
| High School | 16.71%a (1.96) | 17.19a (2.35) | 18.53a (4.27) | |
| College | 17.65%a (1.99) | 18.53a (4.27) | 37.25b (3.67) | |
| Post-graduate | 35%a (2.97) | 42.66b (1.74) | 37.36a (4.46) | |
| Annual Household Income | F (4.68, 210.59) = 2.62* | |||
| <$15,000 | 24.93a (2.37) | 15.39b (2.44) | 22.80a (1.90) | |
| $15,000–$35,000 | 16.97a (2.09) | 11.27b (2.68) | 14.48a.b (2.84) | |
| $35,000–75,000 | 22.87a (2.41) | 32.53b (4.30) | 18.19a,c (3.59) | |
| $75,000+ | 35.22a (3.21) | 40.81a,c (3.60) | 44.53c (5.59) | |
| Ethnicity | F (4.21, 193.45) = 10.35** | |||
| Vietnamese | 19.17a (0.03) | 12.14b (0.02) | 2.85c (0.01) | |
| Filipino | 21.55a (0.03) | 21.52a (0.03) | 28.75b (0.04) | |
| Chinese | 37.00a (0.04) | 25.39b (0.03) | 19.02c (0.03) | |
| Other Asian | 22.28a (0.03) | 40.96b (0.05) | 49.38c(0.05) | |
| Disorder Prevalence | ||||
| Depressive Disorder | 5.53%a (1.43) | 10.75%b (1.73) | 17.89%c (3.34) | F (1.90,87.46) = 8.98** |
| Anxiety Disorder | 7.02%a (1.39) | 10.46%a (1.74) | 12.13%b (2.39) | F (1.99, 91.61) = 2.37* |
| Risk Factors | ||||
| High Cultural Conflict | 50.47%a (2.51) | 67.68%b (3.09) | 64.03%,b (3.58) | F (2, 45) = 14.14** |
| Low Family Cohesion | 23.59%a (2.26) | 36.38%b (2.66) | 43.10%c (3.71) | F (2, 45) = 17** |
| High Family Conflict | 25.57%a (2.17) | 39.13%b (3.71) | 39.79%b (3.56) | F (2, 45) = 6.66** |
| High Discrimination | 22.07%a (2.29) | 30.60%a (3.41) | 43.78%b (4.05) | F (2, 45) = 14.79** |
| Protective Factors† | ||||
| Family Support | −0.39a (0.05) | 0.03b (0.08) | 0.36c (0.06) | F (2, 45) = 52.89** |
| Social Position US | −0.09a (0.07) | 0.05b (0.07) | 0.26c (0.08) | F (2, 45) = 7.06** |
| Social Position Comm | −0.11a (0.06) | 0.10b (0.05) | 0.16b,c (0.06) | F (2, 45) = 4.97* |
Note.
p ≤ .05.
p ≤ .01.
Values with different superscripts are significantly different ( p < .05) from one another.
Protective factors are grand mean centered standardized values. Design-corrected df are calculated as the number of clusters (PSUs) minus the number of strata. Some dfs are non-integers because of additional corrections are made including the transformation to an F test.
The three nativity groups differed significantly in age, with early life immigrants (M = 35.00 years, SD = 0.93) and the U.S.-born sample (M = 38.30 years, SD = 2.40) being younger than the later life immigrants (M = 49.91 years, SD = 0.92). In educational attainment, later life immigrants were significantly more likely to not have completed high school (30.65%) compared to U.S.-born (6.85%) and early life immigrant women (7.45%). In terms of college education, U.S.-born women were more likely (37.25%) to have a college education than early (18.53%) and later life immigrants (17.65%). With regard to income, U.S.-born women and early life immigrants were more likely than later life immigrants to report income over $75K (44.53% and 40.81% vs. 35.22%, respectively). Early life immigrants were less likely to report income below $15K than later life immigrants and U.S.-born women (15.39% vs 24.93% and 22.80%, respectively).
As expected, US-born women showed higher lifetime prevalence of depressive and anxiety disorders (17.89% and 12.13%, respectively) than women who immigrated before age 25 (10.75% and 10.46%) and those who immigrant after age 25 (5.53% and 7.02%). The difference between early and later life immigrants in anxiety disorder prevalence was not significant, but later life immigrants had a higher prevalence of depressive disorder than early life immigrants (10.75% and 5.53%, respectively).
Weighted logistic regression analyses controlling for age, income, education, and social desirability confirmed that US-born females were more likely to have any lifetime depressive (OR = 2.03; 95% CI = 1.35, 4.54) or anxiety (OR = 2.12; 95% CI = 1.34, 5.19) disorders compared to women who immigrated after the age of 25. Women who immigrated before age of 25 were not more likely to have any lifetime depressive or anxiety disorders than respondents who immigrated after age of 25. (See Table 2, block 1).
Table 2.
Simultaneous Analysis of Risk and Protective Factors
| Any Depressive Disorder | Any Anxiety Disorder | ||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Block 1 | B | SE (B) | O.R. (95% CI) | B | SE (B) | O.R. (95% CI) | |
|
|
|||||||
| Covariates | Age | 0.002 | 0.01 | 1.00 (0.98, 1.05) | 0.01 | 0.01 | 1.01 (0.99, 1.05) |
| Social Desirability | −0.19 | 0.11 | 0.83 (0.66, 1.29) | −0.31** | 0.05 | 0.73 (0.66, 0.90) | |
| <15,000 incomea | 0.39 | 0.24 | 1.48 (0.92, 3.74) | 0.48 | 0.27 | 1.62 (0.95, 4.58) | |
| 15,000–35,000 incomea | −0.02 | 0.33 | 0.98 (0.51, 3.53) | 0.11 | 0.19 | 1.11 (0.77, 2.31) | |
| 35,000 – 75,000 incomea | −0.14 | 0.16 | 0.87 (0.63, 1.63) | 0.21 | 0.22 | 1.23 (0.79, 2.96) | |
| HS graduateb | −0.34 | 0.17 | 0.71 (0.51, 1.37) | −0.43 | 0.30 | 0.65 (0.36, 2.07) | |
| College graduateb | −0.52* | 0.13 | 0.59* (0.46, 0.98) | −0.21 | 0.24 | 0.81 (0.50, 2.09) | |
| Post-College Graduateb | 0.11 | 0.26 | 1.12 (0.66, 3.13) | 0.2 | 0.29 | 1.22 (0.68, 3.85) | |
| Nativity | Early-life Immigrant c | 0.41 | 0.24 | 1.51 (0.94, 3.80) | 0.36 | 0.26 | 1.43 (0.86, 3.90) |
| US-Born c | 0.71** | 0.20 | 2.03** (1.35, 4.54) | 0.75** | 0.23 | 2.12** (1.34, 5.19) | |
|
| |||||||
| Block 2 | |||||||
| Nativity | Early-life Immigrant c | 0.48* | 0.23 | 1.62* (1.03, 3.91) | 0.41 | 0.23 | 1.51 (0.95, 3.72) |
| US-Born c | 0.85** | 0.20 | 2.34** (1.57, 5.11) | 0.92** | 0.17 | 2.51** (1.77, 4.97) | |
| Protective Factors | Family Support | −0.16* | 0.07 | 0.85* (0.64, 0.99) | −0.23* | 0.10 | 0.79* (0.53, 0.98) |
| Subjective Status US | −0.21* | 0.10 | 0.81* (0.55, 0.99) | −0.11 | 0.13 | 0.89 (0.69, 1.49) | |
| Subjective Status Comm | −0.02 | 0.09 | 0.98 (0.82, 1.39) | −0.09 | 0.08 | 0.91 (0.78, 1.25) | |
|
| |||||||
| Block 3 | |||||||
| Nativity | Early–life Immigrant c | 0.34 | 0.19 | 1.40 (0.96, 2.96) | 0.31 | 0.21 | 1.36 (0.89, 3.15) |
| US-Born c | 0.30 | 0.20 | 1.35 (0.90, 2.99) | 0.39 | 0.21 | 1.48(0.97, 3.37) | |
| Protective Factors | Family Support | −0.07 | 0.11 | 0.93 (0.75, 1.43) | −0.13 | 0.08 | 0.87 (0.75, 1.20) |
| Subjective Status US | −0.08 | 0.09 | 0.92 (0.77, 1.32) | −0.09 | 0.10 | 0.91 (0.75, 1.35) | |
| Subjective Status Comm | −0.03 | 0.09 | 0.97 (0.81, 1.38) | −0.08 | 0.09 | 0.92 (0.77, 1.32) | |
| Risk Factors † | High Cultural Conflict | 0.71* | 0.24 | 2.03* (1.25, 5.28) | 0.31 | 0.22 | 1.36 (0.87, 3.29) |
| Low Family Cohesion | 0.18 | 0.17 | 1.20 (0.85, 2.34) | 0.28 | 0.19 | 1.32 (0.90, 2.82) | |
| High Family Conflict | 0.34* | 0.15 | 1.40* (1.04, 2.53) | 0.64* | 0.29 | 1.90* (1.06, 5.93) | |
| Moderate Family Conflict | −0.21 | 0.24 | 0.81 (0.50, 2.09) | 0.12 | 0.12 | 1.13 (0.64, 3.42) | |
| High Discrimination | 0.71** | 0.20 | 2.03** (1.36, 4.48) | 0.87** | 0.18 | 2.39** (1.65, 4.92) | |
| Moderate Discrimination | 0.33 | 0.17 | 1.39 (0.99, 2.71) | 0.53 | 0.28 | 1.70 (0.97, 5.10) | |
Note.
p ≤ .05.
p ≤ .01.
Referent groups:
greater than $75,000 income,
11 years or less of education,
later-life immigrants.
Referent group is Low Risk group (e.g., low cultural conflict, high family cohesion).
Differential Exposure to Risk and Protective Factors
Data handling for risk and protective factor variables depended on the observed distribution of scores in our sample. For cultural conflict and family cohesion, a large proportion of respondents reported no risk exposure (e.g., 48% reported no cultural conflict and 64.5% reported maximum value on family cohesion), thus these variables were treated as dichotomous with individuals reporting no risk contrasted against those who reported any risk in that domain. The distribution of scores on family conflict and discrimination followed a bimodal distribution, with sizable proportions reporting no risk and moderate-to-high levels of risk. As such, responses were coded into tertiles (e.g., 0 = Low family conflict, 1 = Moderate family conflict, 2 = High family conflict). Finally, the protective factors of family support, and subjective social status in the U.S. and in the community approximated a normal distribution and were treated as continuous variables.
Approach to Testing Mediation and Suppression
To demonstrate that nativity differences in rates of disorder are due to greater risk exposure for the U.S.-born group (mediation), we conducted a series of analyses following the steps outlined by Baron and Kenny’s (1986) for testing mediation. The first step is to demonstrate the nativity effect on rates of disorder. In all analyses, nativity was entered using two dummy coded variables to denote late-life immigrants and U.S. born women, with early-life immigrants as the reference group. The second step is to demonstrate nativity differences in risk factors with U.S.-born women being at higher risk. The third step is to demonstrate that the proposed risk factors are associated with disorder. The fourth step is to demonstrate that when controlling for the effects of heightened risk factor, the effect of nativity on disorder prevalence is weakened. Sobel’s (1982) test is conducted to demonstrate that the reduction in the nativity effect between steps 1 and 4 is statistically significant.
To demonstrate that nativity differences in rates of depression and anxiety are smaller than would be expected based on higher levels of protective factors among the immigrant groups (suppression), we conducted the same steps outlined above but predicted suppression patterns (MacKinnon, Krull, & Lockwood, 2000). The first step is to demonstrate that there is indeed a nativity effect on rates of psychological disorders with U.S.-born women at greater risk. The second step is to demonstrate nativity differences in protective factors with U.S.-born women experiencing higher levels of protection. The third step is to demonstrate that the protective factors are associated with lower risk for disorder. The fourth step is to demonstrate that when controlling for the effects of the protective factor, U.S.-born women’s risk for disorder is increased. Sobel’s (1982) test is conducted to demonstrate that the increase in the effect of nativity between steps 1 and 4 is statistically significant.
Tests of Mediated Risk
The first step of both mediation and suppression analyses is to examine nativity differences in disorder risk, which was demonstrated in earlier analyses. Table 1 displays levels of reported exposure to risk factors by nativity subgroup, which addresses the second step in Baron and Kenny’s (1986) test of mediation. Compared to later life immigrants, U.S.-born women were significantly more likely to report family conflict (39.79% vs. 25.57%, respectively), cultural conflict (64.03% vs. 50.47%, respectively, low family cohesion (43.10% vs. 23.59%, respectively), and perceived discriminatory treatment (43.78% vs. 22.07%, respectively)1. Compared to later life immigrants, early life immigrants were more likely to report cultural conflict (67.68% vs. 50.47%, respectively), low family cohesion (36.38% vs. 23.59%, respectively), high family conflict (39.13% vs. 25.57%, respectively), but not perceived discrimination (30.60% vs. 22.07%). Overall, the direction of the differences is consistent with the notion that nativity differences in psychiatric disorder may be attributable to differential risk exposure. More specifically, cultural conflict, low family cohesion, family conflict, and perceived discrimination remain as possible mediators for nativity differences in disorder.
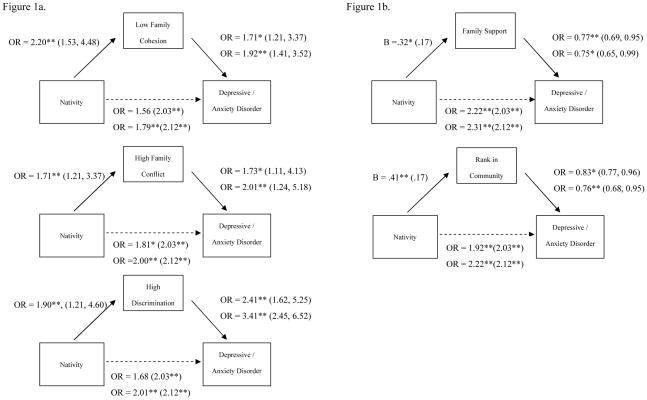
To test the third step of the mediation model, a series of weighted logistic regression analyses controlling for age, income, education, and social desirability estimated the associations between risk factors and lifetime depressive or anxiety disorder. As expected, cultural conflict (OR = 2.39 ; 95% CI = 1.40, 4.08; and OR = 5.72; 95% CI = 3.22, 10.14, for any lifetime depressive and any lifetime anxiety disorder, respectively), low family cohesion (OR = 1.71; 95% CI = 1.21, 3.37 and OR = 1.92,; 95% CI = 1.41, 3.52), family conflict (OR = 1.73; 95% CI = 1.11, 4.13 and OR = 2.01; 95% CI = 1.24, 5.18), and perceived discrimination (OR = 2.41; 95% = 1.62, 5.25 and OR = 3.41; 95% = 2.45, 6.52) were associated with lifetime depressive and lifetime anxiety disorder. As such, these four risk factors continue to be viable mediators of observed nativity differences in depression and anxiety.
Sobel (1982) tests were conducted to test the significance of the reduction in the nativity effect in psychological disorder risk as shown in Figure 1a. Analyses revealed that cultural conflict did not mediate the association between nativity and risk of depressive and anxiety disorder (Sobel Z = 1.59, p > .05 & Z = 1.67, p > .05, respectively). Family conflict attenuated the relationship between nativity and any anxiety disorder (Z = 1.99, p < .05), but the Sobel test was marginal for depressive disorder (Z= 1.74, p > .05). Lack of family cohesion mediated the effect of nativity on anxiety disorder (Z= 2.11, p < .05) with the mediation effect being marginal for depressive disorder (Z= 1.89, p = .06). Lastly, perceived discrimination mediated the relationship between nativity and any depressive disorder (Z= 3.22, p < .01) and any anxiety disorder (Z = 2.10, p < .05).
Figure 1.
Panel A shows results of mediation analyses examining risk factors as mediators of the effect of Nativity (U.S. born versus Adults Immigrants) on disorder. Panel B shows results of suppression analyses examining protective factors as suppressors of the relationship between Nativity and disorder. Numbers within parentheses show O.R. in predicting disorder from U.S. born nativity before controlling for risk and protective factors. ORs and B coefficients in the second row predict anxiety disorders. *p ≤ .05. **p ≤ .01.
Tests of Suppression
Several factors were potential suppressors of the nativity differences in depression and anxiety. As shown in Table 1, U.S.-born women reported higher level of a protective factor (family support, higher social standing in the U.S., higher social standing in the community) compared to immigrant women. Analyses were conducted to examine whether without the suppression effects of these protective factors, the nativity differences in disorder would have been even larger. Step 3 of the mediation analysis used weighted logistic regression analyses to examine the relationship between these protective factors and risk for lifetime disorders. As expected, family support (B = −0.18, p < .05 and B = −0.19, p < .05) and subjective social status in the U.S. (B = −0.24, p < .05 and B = −0.25, p < .05) and subjective social status in the community (B = −0.19, p < .05 and B = −0.23, p < .05) were inversely related to risk of depressive and anxiety disorders, respectively. To test whether these protective factors served as suppressors of the relationship between nativity and disorder, nativity effects on lifetime disorder risk was calculated controlling for the effect of the protective factor. Results of suppression analyses are shown in Figure 1b. For all three protective factors, nativity differences for lifetime disorder risk were increased when the model controlled for the effect of the protective factor. Sobel tests demonstrated a suppression effect of family support in lifetime depressive disorder risk (Z = 2.31, p < .05 and Z = 2.01, p < .05, respectively), for perceived social standing in the community (Z = 2.31, p < .001 and Z = 2.21, p < .05). However, subjective social status in the U.S. did not significantly suppress the associations between nativity and disorder (Z = 1.63, p > .05 and Z = 1.66, p > .05).
Simultaneous Examination of Risk and Protective Factors
The foregoing analyses examined individual risk and protective factors as potential mediators or suppressors of nativity differences in lifetime disorder. We then conducted weighted hierarchical logistic regression models to examine the independent contribution of each factor in predicting risk of disorder. Nativity and sociodemographic covariates were entered in the first block, the candidate suppressor variables in the second, and the potential risk factor mediators in the third block. As shown in Table 2, Block 1, only education was a significant predictor of depression risk with women holding a college degree (OR = 0.59; 95% CI = 0.46, 0.98) being at lower risk than those with less than high school education. In predicting lifetime anxiety disorders, only social desirability (B = −0.31, p < .05) was a significant predictor. As shown in Block 2, adding the protective factors of family support (B = −0.16, p < .05 depressive disorders and B = −0.23, p < .05 anxiety disorders) and subjective status within the U.S. (B = −0.21, p < .05 depressive disorders) disattenuated the O.R. for U.S. nativity predicting depression (OR = 2.34; 95% CI = 1.57, 5.11) and anxiety (OR = 2.51; 95% CI = 1.77, 4.97). In Block 3, however, the associations between nativity and lifetime depressive disorder were no longer significant (OR = 1.35; 95% CI = 0.90, 2.99) after accounting for cultural conflict (OR = 2.03, 95% CI = 1.25, 5.28), family conflict (OR = 1.40; 95% CI = 1.04, 2.53), and perceived discrimination (OR = 2.03; 95% CI = 1.36, 4.48). Similarly, in Block 3, the associations between nativity and lifetime anxiety disorder were no longer significant (OR = 1.48; 95% CI = 0.97, 3.37) after accounting for family conflict (OR = 1.90; 95% CI = 1.06, 5.93) and discrimination (OR = 1.65, 95% CI = 1.65, 4.92).
Differential Stress Reactivity
In Table 3, weighted logistic regression analyses were conducted separately by nativity group to examine the associations between risk/protective factors and any lifetime depressive or anxiety disorder. Contrary to our hypotheses that US-born women may be more reactive to stress, immigrant women who immigrated after the age of 25 showed robust associations between cultural conflict (OR = 3.22; 95% CI = 2.21, 6.73 and OR = 4.01; 95% CI = 2.91, 7.52 for lifetime depressive and anxiety disorders, respectively), family cohesion (OR = 2.99; 95% CI = 2.23, 5.31 and OR = 1.98; 95% CI = 1.13, 5.94), and perceived discrimination (OR = 1.91; 95% CI = 1.01, 6.66 and OR = 3.41; 95% CI = 2.35, 7.07) and lifetime depressive and anxiety disorders, but none of these factors were significant predictors of disorder for U.S.-born women except for discrimination (OR = 3.74; 95% CI = 2.61, 7.57 and OR = 1.98; 95% CI = 1.08, 6.50) Among women who immigrated before age 25, cultural conflict (OR = 4.42; 95% CI = 3.36, 7.57 and OR = 3.21; 95% CI = 2.11, 7.31) and family conflict (OR = 3.31; 95% CI = 2.61, 5.27 and OR = 2.57; 95% CI = 1.34, 9.21) predicted both depressive and anxiety disorders, but lack of family cohesion and discrimination did not. On the other hand, US-born women showed significant and robust protection from disorder from family support (B = −0.23, p < .05 and B = −0.31, p < .05 for depressive and anxiety disorders, respectively) and from subjective social status in the U.S. (B = −0.56, p < .05 and B = −0.46, p < .05), and the community (B = −0.39, p < .05 and B = −.31, p < .05), whereas these protective factors were only inconsistently related to disorder risk among the two groups of immigrant women. Despite these patterns in subgroup analyses, formal tests of moderation failed to reveal significant interactions between nativity and risk/protective factors in predicting lifetime anxiety or depressive disorders.
Table 3.
Odd Ratios (OR) /Regression Coefficients (B) of Risk/Protective Factors Predicting Disorder by Nativity
| Risk/Protective Factors | Nativity | Depressive Disorder | Anxiety Disorder |
|---|---|---|---|
| Cultural Conflict a | Later-life Immigrant | OR= 3.22* (2.21, 6.73) | OR = 4.01** (2.91,7.52) |
| Early–life Immigrant | OR= 4.42** (3.36, 7.57) | OR= 3.21** (2.11, 7.31) | |
| US-Born | OR= 1.63 (0.94, 4.79) | OR= 1.91 (0.99, 6.92) | |
|
| |||
| Low Family Cohesion a | Later-life Immigrant | OR= 2.99** (2.23, 5.31) | OR = 1.98* (1.13, 5.94) |
| Early–life Immigrant | OR= 1.18 (0.41, 9.37) | OR = 1.69 (0.84, 6.65) | |
| US-Born | OR= 1.31 (0.71, 4.35) | OR = 1.74 (0.98, 5.36) | |
|
| |||
| High Family Conflict a | Later-life Immigrant | OR= 1.80 (0.91, 6.85) | OR= 2.32* (1.21, 8.31) |
|
| |||
| Early–life Immigrant | OR= 3.31** (2.61, 5.27) | OR= 2.57** (1.34, 9.21) | |
|
| |||
| US-Born | OR= 2.02 (1.13, 6.31) | OR= 1.02* (1.02, 7.37) | |
|
| |||
| High Discrimination a | Later-life Immigrant | OR= 1.91* (1.01, 6.66) | OR= 3.41** (2.35, 7.07) |
|
| |||
| Early–life Immigrant | OR= 1.53 (0.92, 4.15) | OR= 2.00 (0.98, 8.10) | |
| US-Born | OR= 3.74** (2.61, 7.57) | OR= 1.98** (1.08, 6.50) | |
|
| |||
| Family Support | Later-life Immigrant | B= −0.02 (−0.38, 0.40) | B= −0.00 (−0.79, 0.78) |
| Early–life Immigrant | B= −0.12 (−0.23, 0.47) | B= −0.29* (−0.68, −0.12) | |
| US-Born | B= −0.23* (−0.45, −0.01) | B= −0.31** (−0.49, −0.13) | |
|
| |||
| Social Position in US | Later-life Immigrant | B = −0.11* (−0.22, −0.01) | B = −0.31* (−0.61, −0.01) |
| Early–life Immigrant | B = −0.02 (−0.53, 0.49) | B = −0.13 (−0.50, 0.24) | |
| US-Born | B = −0.56** (−0.95, −0.15) | B = −0.46* (−0.81, −0.11) | |
|
| |||
| Social Position in Community | Later-life Immigrant | B = −.05 (−0.45, 0.35) | B = −0.32* (−0.78, −0.06) |
| Early–life Immigrant | B = −0.14 (−0.54, 0.34) | B = −0.21 (−0.52, 0.12) | |
| US-Born | B = −0.39** (−0.67, −0.11) | B = −0.31* (−0.61, −0.01) | |
Note.
p = .05.
p = .01.
Odds ratios/Regression Coefficients inside parentheses are 95% confidence intervals.
Referent group is Low Risk group (e.g., High cultural conflict, Low family cohesion).
Covariates include household income, age, education level, and social desirability
Discussion
As first reported in Takeuchi et al. (2007), support for the immigrant paradox was found, as U.S.-born Asian American women showed higher life-time prevalence of depressive and anxiety disorders compared to their counterparts who immigrated before age 25, as well as those who immigrated after age 25. It appeared that part of the elevated risk for depressive and anxiety disorders among U.S.-born Asian American women could be explained by differential exposure to stressors. U.S.-born Asian American women were more likely than their immigrant counterparts to report experiences of discrimination, higher levels of family conflict, and lower levels of family cohesion, which in turn were associated with increased risk for depression and anxiety. Considered individually, differential exposure to these risk factors partially mediated the effect of nativity on disorder. Consistent with a social stress hypothesis, these findings suggest that the so-called immigrant paradox is readily explicable because U.S.-born Asian American women are more likely to experience chronic stress associated with minority status and negative family climate.
However, U.S.-born women were also exposed to less risk compared to immigrant women in some respects. In particular, U.S.-born women reported more favorable conditions with respect to higher levels of subjective social status and family support, which in turn are associated with lower risk of depressive and anxiety disorders. The findings concerning higher social standing among U.S. born women are consistent with previous findings that successive generations of immigrants tend to have higher levels of social mobility and human capital, which are generally protective against mental disorders (Adler et al, 2000; Park & Myers, 2010). However, the findings concerning greater perceived family support among U.S. born women compared to immigrants was not aligned with our predictions. The direction of difference for family support was the opposite of that found for family cohesion, which was higher among immigrant groups as predicted. Rather than feelings of closeness, our family support scale assesses frequent, proximal contact and reliance on immediate and extended family members. Research suggests that U.S. born generations tend to enjoy more proximity to multi-generational extended family support networks than immigrant generations, who are more likely to leave behind extended family support in their country of origin (Glick, 1999). As such, it is important to differentiate the aspects of family climate that may favor or disfavor distinct generations of immigrant groups. When social mobility and family support protective factors were examined in the regression analyses, they produced suppression effects, which lent some credence to the notion that the immigrant advantage in mental health can be viewed as paradoxical because U.S.-born women are at greater risk for lifetime anxiety and depressive diagnoses, despite experiencing some more favorable conditions than immigrant women.
Thus, U.S.-born Asian American women are at greater risk of exposure to certain chronic stressors (e.g. discrimination, family conflict, less family cohesion) while also benefitting more from some protective factors (e.g. higher perceived status and family support) compared to immigrant Asian women. We examined whether nativity differences in depression and anxiety disorders could be explained by the risk and protective factors when considered together. It appeared that the net effect of the risk factors explained the nativity differences in lifetime disorder. The heightened stress that U.S.-born Asian American women experienced in family climate and perceived discrimination explained the elevated risk for disorder, even after accounting for suppression effects. It is also notable that the protective factors were no longer significantly associated with depressive or anxiety disorders after controlling for the effect of stressors. This might suggest that any mental health advantage conferred to U.S.-born women by perceived social standing and family support are outweighed by exposure to risk factors.
Our findings did not support the differential reactivity hypothesis as an explanation for nativity differences in risk of anxiety and depression. U.S.-born Asian American women did not appear more reactive to stress than immigrant Asian women. Contrary to the notion of immigrant hardiness, subgroup analyses revealed more consistent significant associations between the four risk factors under consideration (i.e., family conflict, cultural conflict, low family cohesion, and perceived discrimination) and lifetime disorder risk, particularly among later life immigrant women. It is possible that immigrant women may in some respects be more susceptible to these types of stress given their relatively low social standing in the community. Individuals from low status groups tend to report greater impact of stressful events in their lives than individuals from higher status groups (Grzywacz, Almeida, Neupert, & Ettner, 2004). However, it is also possible that our reliance on self-report data presents a potentially weak test of the immigrant hardiness hypothesis, as respondents were asked to report on their stress context. Psychological hardiness among Asian American immigrants may manifest in a higher threshold for perceiving events and conditions as stressful and reporting them as such in the interview. Future studies should therefore incorporate methodologies that better separate objective circumstances and events from respondents’ appraisals of stress to better evaluate potential group differences in stress reactivity. This could be better accomplished with experimental methods and objective threat stress interview procedures.
There are additional limitations of the study that should be considered in interpreting our results. First, the study pertained to Asian American women, so results may not be generalizable to other ethnic minority and immigrant women or Asian American men. Nevertheless, these nativity disparities in depression and anxiety were not previously shown among Asian American men (Takeuchi et al., 2007). This may be due to the fact that women tend to manifest distress through internalizing symptoms (as evidenced by higher prevalence rates for depression and anxiety disorders) whereas men tend to manifest distress with more externalizing presentations (e.g. Kessler et al., 2005). Indeed, there is some evidence to suggest that U.S.-born Asian American men exhibit higher prevalence of substance use disorders compared to their immigrant Asian counterparts (Takeuchi et. al., 2007). As such, there are opportunities to examine explanations of nativity-based disparities in psychiatric disorders most likely to be revealed among ethnic minority men versus women.
Second, the NLAAS and other major psychiatric epidemiologic surveys yield cross-sectional analyses. We assessed exposure to risk and protective factors and their relation to the lifetime occurrence of psychiatric disorder. This precludes conclusions concerning the directionality of the associations examined. Taking the reverse causality argument through its conclusion, our mediation analyses may be interpreted to suggest that generational differences in depression and anxiety may explain group differences in perceptions of discrimination, family conflict and cohesion. However, as applied to the suppression analyses, reverse causality interpretations are less plausible. Elevated rates of depression and anxiety would be unlikely to result in more favorable appraisals of social status among U.S.-born women compared to immigrants. Prospective data are needed to clarify the directionality of these relationships.
Third, this study relied on self-reports of stressors, protective factors, and mental health problems. We have already discussed this limitation in providing a test of group differences in stress reactivity. Self-report measures of stress represent abstracted estimates of the frequency of events coupled with an appraisal of those events as significant and distressing. The measurement of experiences of discrimination and unfair treatment are particularly subject to frame of reference effects. Future research should capitalize on real-time event sampling, experimental and laboratory manipulations, and objective measures of health status to examine the role of risk and protective factors in explaining nativity based disparities in mental health.
Despite these limitations, the study focused on a large nationally representative sample of Asian American women, and shed new light on how we might best understand nativity differences in psychiatric disorders by examining differential exposure to risk and protective factors in U.S.-born versus immigrant groups. In particular, subjecting psychiatric epidemiologic data to mediation and suppression analyses presents a novel approach to examining the so-called immigrant paradox. Our findings suggest that increased rates of depression and anxiety among later generation Asian American women are explicable based on differential experiences of psychosocial stress in the domains of family and discrimination reported by women.
Acknowledgments
The National Latino and Asian American Study was supported by the National Institute of Mental Health (grants U01 MH62209 and U01 MH62207), with additional support from the Office of Behavioral and Social Science Research at the National Institutes of Health and the Substance Abuse and Mental Health Services Administration.
Footnotes
We tested whether the prevalence differences in lifetime depressive disorder between the early and later life immigrants were mediated by the risk and protective factors. Cultural conflict attenuated the relationship between nativity (i.e., early life vs. later life immigrants) and any depressive disorder (Z = 3.25, p < .05).
Contributor Information
Anna S. Lau, University of California, Los Angeles
William Tsai, University of California, Los Angeles.
Josephine Shih, St. Joseph’s University.
Lisa L. Liu, University of California, Los Angeles
Wei-Chin Hwang, Claremont McKenna University.
David T. Takeuchi, University of Washington
References
- Abraido-Lanza A, Dohrenwend B, Ng-Mak D, Turner J. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. American Journal of Public Health. 1999;89:1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Bates L. Latino health paradoxes: empirical evidence, explanations, future research, and implications. In: Rodríguez H, Saenz R, Menjivar C, editors. Latino/as in the United States: Changing the Face of America. New York, NY: Springer US; 2007. [Google Scholar]
- Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy, white women. Health Psychology. 2000;19:586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Alegría M, Chatterji P, Wells K, Cao Z, Chen C, Takeuchi D, Meng X, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Services. 2008;59:1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Pescosolido B, Williams S, Canino G. Culture, race/ethnicity and disparities: fleshing out the socio-cultural framework for health services disparities. In: Pescosolido BA, Martin JK, McLeod JD, Rogers A, editors. Handbook of the Sociology of Health, Illness and Healing: A Blueprint for the 21st Century. New York, NY: Springer; 2010. pp. 363–382. [Google Scholar]
- Alegria M, Takeuchi D, Canino G, Duan N, Shrout P, Meng X, Gong F. Considering context, place and culture: The National Latino and Asian American Study. International Journal of Methods in Psychiatric Research. 2004;13:208–220. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates L, Acevedo-Garcia D, Alegria M, Krieger N. Immigration and Generational Trends in Body Mass Index and Obesity in the United States: Results of the National Latino and Asian American Survey, 2002–2003. American Journal of Public Health. 2008;98:70–77. doi: 10.2105/AJPH.2006.102814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau JA, Chang DF. Psychiatric disorders among foreign-born and U.S.-born Asian and Pacific Islanders in a U.S. national survey. Social Psychiatry and Psychiatric Epidemiology. 2006;4:27–44. doi: 10.1007/s00127-006-0119-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Borges G, Saito N, Tancredi D, Benjet C, Hinton L, Kendler K, Kravitz R, Vega W, Aguilar-Gaxiola S, Medina-Mora M. Migration from Mexico to the United States and Conduct Disorder: A Cross-National Study. Archives of General Psychiatry. 2011;68:1284–1293. doi: 10.1001/archgenpsychiatry.2011.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnham MA, Hough RL, Karno M, Escobar JI, Telles CA. Acculturation and lifetime prevalence of psychiatric disorders among Mexican Americans in Los Angeles. Journal of Health and Social Behavior. 1987;28:89–102. [PubMed] [Google Scholar]
- Cervantes A, Keith L, Wyshak G. Adverse birth outcomes among native-born and immigrant women: replicating national evidence regarding Mexicans at the local level. Maternal and Child Health Journal. 1999;3:99–109. doi: 10.1023/a:1021805427469. [DOI] [PubMed] [Google Scholar]
- Cobas JA, Balcazar H, Benin MB, Keith VM, Chong Y. Acculturation and low-birthweight infants among Latino women: a reanalysis of HHANES data with structural equation models. American Journal of Public Health. 1996;86:394–396. doi: 10.2105/ajph.86.3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook B, Alegría M, Lin JY, Guo J. Pathways and correlates connecting latinos’ mental health with exposure to the united states. American Journal of Public Health. 2009;99:2247–2254. doi: 10.2105/AJPH.2008.137091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Escobar JI. Immigration and mental health: Why are immigrants better off? Archives of General Psychiatry. 1998;55:781–782. doi: 10.1001/archpsyc.55.9.781. [DOI] [PubMed] [Google Scholar]
- Escobar JI, Nervi CH, Gara MA. Immigration and mental health: Mexican americans in the united states. Harvard Review of Psychiatry. 2000;8:64–72. [PubMed] [Google Scholar]
- Franzini L, Ribble J, Keddie A. Understanding the Hispanic Paradox. Ethnicity and Disease. 2001;11:496–518. [PubMed] [Google Scholar]
- Finch B, Kolody B, Vega W. Perceived Discrimination and Depression among Mexican-Origin Adults in California. Journal of Health and Social Behavior. 2000;41:295–313. [PubMed] [Google Scholar]
- Frisbie W, Cho Y, Hummer R. Immigration and the Health of Asian and Pacific Islander Adults in the United States. American Journal of Epidemiology. 2001;153:372–380. doi: 10.1093/aje/153.4.372. [DOI] [PubMed] [Google Scholar]
- Fuentes-Afflick E, Hessol N, Perez-Stable E. Maternal Birthplace, Ethnicity, and Low Birth Weight in California. Archives of Pediatrics & Adolescent Medicine. 1998;152:1105–1112. doi: 10.1001/archpedi.152.11.1105. [DOI] [PubMed] [Google Scholar]
- Funk SC. Hardiness: A review of theory and research. Health Psychology. 1992;11:335–345. doi: 10.1037//0278-6133.11.5.335. [DOI] [PubMed] [Google Scholar]
- Giedd JN. Structural magnetic resonance imaging of the adolescent brain. In: Dahl RE, Spear LP, Dahl RE, Spear LP, editors. Adolescent Brain Development: Vulnerabilities and Opportunities. New York, NY, US: New York Academy of Sciences; 2004. pp. 77–85. [Google Scholar]
- Glick JE. Economic Support from and to Extended Kin: A Comparison of Mexican Americans and Mexican Immigrants. International Migration Review. 1999;33:745–765. [Google Scholar]
- Gordon-Larsen P, Harris KM, Ward DS, Popkin BM. Acculturation and overweight-related behaviors among Hispanic immigrants to the US: The National Longitudinal Study of Adolescent Health. Social Science & Medicine. 2003;57:2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- Gogtay N, Sporn A, Clasen LS, Nugent TF, Greenstein D, Nicolson R, Rapoport JL. Comparison of progressive cortical gray matter loss in childhood-onset schizophrenia with that in childhood-onset atypical psychoses. Archives of General Psychiatry. 2004;61:17–22. doi: 10.1001/archpsyc.61.1.17. [DOI] [PubMed] [Google Scholar]
- Gong F, Xu J, Fujishiro K, Takeuchi DT. A life course perspective on migration and mental health among Asian immigrants: The role of human agency. Social Science & Medicine. 2011;73:1618–1626. doi: 10.1016/j.socscimed.2011.09.014. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:1226–1233. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- Grzywacz JG, Almeida DM, Neupert SD, Ettner SL. Socioeconomic status and health: A micro-level analysis of exposure and vulnerability to daily stressors. Journal of Health and Social Behavior. 2004;45:1–16. doi: 10.1177/002214650404500101. [DOI] [PubMed] [Google Scholar]
- Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) International Journal of Methods in Psychiatric Research. 2004;13:221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang W, Myers HF. Major depression in chinese americans: The roles of stress, vulnerability, and acculturation. Social Psychiatry and Psychiatric Epidemiology. 2007;42:189–197. doi: 10.1007/s00127-006-0152-1. [DOI] [PubMed] [Google Scholar]
- Hwang W, Wood JJ, Fujimoto K. Acculturative family distancing (AFD) and depression in Chinese American families. Journal of Consulting and Clinical Psychology. 2010;78:655–667. doi: 10.1037/a0020542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasso-Aguilar R, Waitzkin H, Landwehr A. Multinational corporations and health care in the United States and Latin America: Strategies, actions, and effects. Journal of Health and Social Behavior. 2004;45:136–157. [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Waterman PD, Kosheleva A, Chen JT, Carney DR, Smith KW, Samuel L. Exposing racial discrimination: Implicit & explicit measures—The study of 1005 US-born black & white community health center members. PLoS ONE. 2011:6. doi: 10.1371/journal.pone.0027636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo WH, Tsai Y. Social networking, hardiness and immigrant’s mental health. Journal of Health and Social Behavior. 1986;27:133–149. [PubMed] [Google Scholar]
- Leu J, Yen I, Gansky S, Walton E, Adler N, Takeuchi D. The Association between Subjective Social Status and Mental Health among Asian Immigrants: Investigating the Influence of Age at Immigration. Social Science and Medicine. 2008;66:1152–1164. doi: 10.1016/j.socscimed.2007.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prevention Science. 2000;1:173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noh S, Avison WR. Asian immigrants and the stress process: A study of koreans in canada. Journal of Health and Social Behavior. 1996;37:192–206. [PubMed] [Google Scholar]
- Ortega AN, Rosenheck R, Alegría M, Desai RA. Acculturation and the lifetime risk of psychiatric and substance use disorders among Hispanics. Journal of Nervous and Mental Disease. 2000;188:728–735. doi: 10.1097/00005053-200011000-00002. [DOI] [PubMed] [Google Scholar]
- Operario D, Adler NE, Williams DR. Subjective social status: Reliability and predictive utility for global health. Psychology & Health. 2004;19(2):237–246. [Google Scholar]
- Paradies YC. Defining, conceptualizing and characterizing racism in health research. Critical Public Health. 2006;16:143–157. [Google Scholar]
- Palloni A, Morenoff J. Interpreting the paradoxical in the Hispanic Paradox: Demographic and Epidemiologic Approaches. Annals of the New York Academy of Sciences. 2001;954:140–174. doi: 10.1111/j.1749-6632.2001.tb02751.x. [DOI] [PubMed] [Google Scholar]
- Park J, Myers D. Intergenerational mobility in the post-1965 immigration era: Estimates by an immigrant generation cohort method. Demography. 2010;47:369–392. doi: 10.1353/dem.0.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez DJ, Fortuna L, Alegría M. Prevalence and correlates of everyday discrimination among U.S. Latinos. Journal of Community Psychology. 2008;36:421–433. doi: 10.1002/jcop.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Escamilla R, Putnik P. The Role of Acculturation in Nutrition, Lifestyle, and Incidence of Type 2 Diabetes among Latinos. Journal of Nutrition. 2007;137:860–870. doi: 10.1093/jn/137.4.860. [DOI] [PubMed] [Google Scholar]
- Popkin B, Udry J. Adolescent obesity increases significantly in second and third generation U.S. immigrants: the National Longitudinal Study of Adolescent Health. Journal of Nutrition. 1998;128:701–706. doi: 10.1093/jn/128.4.701. [DOI] [PubMed] [Google Scholar]
- Sabogal F, Pérez-Stable EJ, Otero-Sabogal R, Hiatt RA. Gender, ethnic, and acculturation differences in sexual behaviors: Hispanic and non-Hispanic White adults. Hispanic Journal of Behavioral Sciences. 1995;17:139–159. [Google Scholar]
- Schwartz S, Meyer IH. Mental health disparities research: The impact of within and between group analyses on tests of social stress hypotheses. Social Science & Medicine. 2010;70:1111–1118. doi: 10.1016/j.socscimed.2009.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological Methodology. San Francisco: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- Stafford M, Bécares L, Nazroo J. Racial discrimination and health: exploring the possible protective effects of ethnic density. In: Stillwell J, editor. Understanding Population Trends and Processes. Vol. 3. Dordrecht, The Netherlands: Springer; 2010. [Google Scholar]
- Takeuchi DT, Zane N, Hong S, Chae DH, Gong F, Gee GC, Alegría M. Immigration-related factors and mental disorders among Asian Americans. American Journal of Public Health. 2007;97:84–90. doi: 10.2105/AJPH.2006.088401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega WA, Alderete E, Kolody B, Aguilar-Gaxiola S. Illicit drug use among Mexicans and Mexican Americans in California: the effects of gender and acculturation. Addiction. 1998;93:1839–1850. doi: 10.1046/j.1360-0443.1998.931218399.x. [DOI] [PubMed] [Google Scholar]
- Vega WA, Sribney WM, Achara-Abrahams I. Co-occurring alcohol, drug, and other psychiatric disorders among Mexican-origin people in the United States. American Journal of Public Health. 2003;93:1057–1064. doi: 10.2105/ajph.93.7.1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton E, Takeuchi DT. Family structure, family processes, and well-being among Asian Americans: Considering gender and nativity. Journal of Family Issues. 2010;31:301–332. [Google Scholar]
- World Mental Health Survey Consortium. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. Journal of American Medical Association. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]